Abstract
Objective:
To evaluate the clinical and functional outcomes of modular endoprosthetic replacement (EPR) compared to proximal femur intramedullary nailing (IMN) for the treatment of proximal femur metastases.
Methods:
We retrospectively studied the records of patients with proximal femur metastatic lesions treated with surgical stabilization between January 2007 and December 2014 in terms of operation time, blood loss, postoperative score, soreness, Karnofsky performance score (KPS) and survival time.
Results:
There were 34 patients treated with surgical stabilization. The mean follow-up period was 12.1?.6 months (range: 10-47 months). Thirteen were treated with EPR and 21 were stabilized with IMN (20 males, 14 females; mean age: 68.7 years). The median survival time was 11.0 months for both groups (P=0.147). The operation time, blood loss and Harris score of IMN group were lower than those of EPR group (P=0.001, P=0.001, P=0.002, respectively).
Conclusions:
Both EPR and IMN for treating proximal femur metastasis achieved effective clinical outcomes. Therefore, the suitable surgical methods depended on the general conditions and medical requirements of patients, as well as the technical advantages of the doctor.
Keywords: Proximal femur, bone metastasis, intramedullary nailing (IMN), endoprosthetic replacement
Introduction
Bone is the third most common site of metastatic cancer after lung and liver (1). Improvements in oncological treatment over recent years have resulted in an increased life expectancy and hence,a higher incidence of metastases with the skeleton (2). About 10% to 30% of patients will sustain metastasis of long bones as common complications of primary malignant tumors. The breast was the most common site of the primary tumor (60%),followed by the lung,the prostate and the kidney (1). The most frequent site of bone metastatic lesions is located in the femur,specifically in the proximal part of it. Because of its major load-bearing function,the risk of surgical treatment is relatively high. Bone metastasis at the femoral neck (50%) or metastatic lesions of the inter-trochanteric (20%) and sub-trochanteric areas (30%) can be either stabilized with therapeutic or prophylactic fixation or treated with conventional arthroplasty to achieve pain control and early restoration of weight-bearing function (3, 4). This retrospective study described a series of patients with proximal femoral metastases who underwent intramedullary nailing (IMN) or endoprosthetic replacement (EPR),to assess indications,clinical outcomes and complications related to this procedure.
Patients and methods
Patients
Records were reviewed from 34 patients who underwent EPR or IMN for proximal femoral metastases from January 2007 to December 2014 at the Department of Orthopedics,Beijing Friendship Hospital. The inclusion criteria were patients with: 1) intractable pain around hip with or without history of lesions; 2) radiological findings of pathologic fractures; 3) cancer staging of samples conducted to ascertain the presence of bone metastases; and 4) with the history of tumor. The exclusion criteria were patients: 1) without surgical treatment; 2) with primary femoral tumor; or 3) with life expectancy less than 3 months. Preoperative evaluations included cancer staging with total body bone scan to exclude the presence of multiple metastases at other locations. Preoperative blood samples were conducted before surgery and operability depended on the general condition of the patients. The study was approved by the Ethic Committee of Beijing Friendship Hospital,and written informed consent of all patients was obtained.
Treatment methods
In the IMN group,curettage was performed under general or lumbar anesthesia. A proximal femoral antirotation nail was used (PFNA,Johnson and Johnson,USA) and cementation was performed for fixation. In the EPR group,curettage was performed under general or lumbar anesthesia. Patients with resection received a cemented modular proximal femoral or bipolar prosthetic replacement (Smith & Nephew,USA),stabilized by cementation. Corresponding treatments were performed during the perioperative period such as blood transfusion and anti-inflammatory therapy. For primary tumors,chemotherapy and hormone therapy were conducted together with bisphosphonate treatment.
Parameter studies
The data collected included gender,age,operation time,accompanied diseases and blood tests (routine blood,liver and kidney function,electrolyte,blood coagulation function,and blood gas analysis). We selected the value in operation day to analyze Acute Physiology and Chronic Health Evaluation (APACHE) Ⅱ score (5),the blood loss,and Visual Analogue Score of pain (VAS),and also gathered the data of Harris score,Karnofsky scores,and complications during perioperative period [recent complications included infection,thrombosis of lower limbs,etc.; and the long-term complications included dislocation,breakage or loose of internal fixation,fracture around the internal fixation (Vancouver Classification),etc.]. All the parameter data were collected by the same team.
Statistical analysis
Statistical correlation was analyzed with SPSS software version 16.0 (SPSS Inc.,Chicago,IL,USA). The comparisons of measurement data (two groups of operation time,blood loss,Harris score,Karnofsky performance score (KPS) and APACHE Ⅱ scoring system) used independent sample t-test; and VAS score (preoperative and postoperative) used the paired t-test. All the measurement data were expressed as x±s. For patient survival,the Kaplan-Meier analysis was applied,with log-rank Chi-square test. P<0.05 was considered statistically significant.
Results
Clinical and demographic data
There were 34 patients with proximal femoral metastases who underwent surgery treatment (20 males,14 females; age range: 52-89 years old). The mean follow-up period was 12.1±8.6 months (range: 10-47 months). Twenty-one patients received IMN,and 13 patients were treated with EPR. Three patients received total arthroplasty. Hemiarthroplasty as well as total arthroplasty was performed in 10 patients. The mean age of patients in IMN group was 72.6 years old,whereas the mean age of EPR group was 62.2 years old (P=0.03). Primary tumors included 7 cases of bronchogenic carcinoma,6 liver cancer,5 gastric cancer,4 colorectal cancer,3 kidney cancer,3 prostatic cancer,2 breast cancer,2 esophagus cancer,1 bladder cancer and 1 cholangiocarcinoma.
Surgery-related data analysis
As shown in Table 1,the operation time,blood loss and Harris score of IMN group were less than those of EPR group (P=0.001,P=0.001,P=0.002,respectively). There were no statistical differences in VAS,KPS or APACHE Ⅱ between the two groups.
Table 1.
The clinically related data of IMN and EPR groups (x±s)
| Index | IMN | EPR | t value | P |
| *, in IMN group, preoperational vs. postoperational VAS scores, P=0.001; in EPR group, preoperational vs. postoperational VAS scores, P=0.001, which was statistically significant. | ||||
| Case number | 21 | 13 | ||
| Operation time (min) | 59.5±6.1 | 75.4±7.8 | 37.0 | 0.001 |
| Amount of bleeding (mL) | 571.4±96.9 | 753.8±143.6 | 231.0 | 0.001 |
| VAS* | ||||
| Preoperation | 8.7±0.7 | 8.7±0.6 | 27.0 | 0.772 |
| Postoperation | 2.7±0.7 | 2.5±0.6 | 19.0 | 0.363 |
| Harris score | 70.3±4.0 | 76.7±3.4 | 260.0 | 0.002 |
| KPS | 65.7±10.7 | 71.5±10.6 | 324.0 | 0.134 |
| APACHE Ⅱ | 11.2±5.2 | 10.1±4.7 | 221.0 | 0.117 |
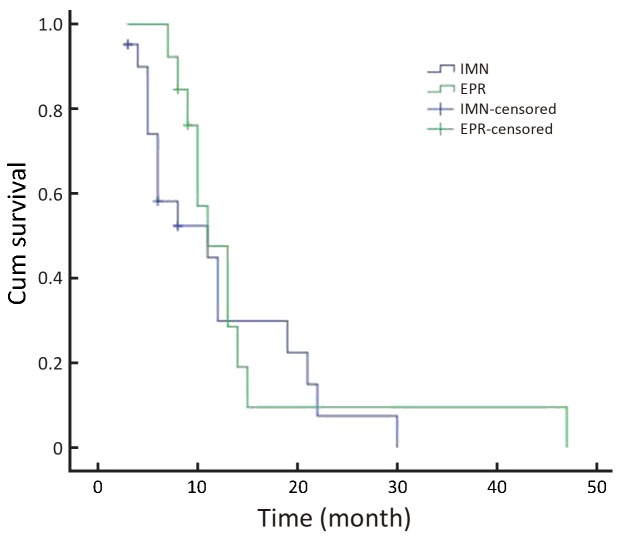
Survival analysis
The Kaplan-Meier survival curves are shown in Figure 1. The survival rate of IMN group was 23.8% with the mean survival time of 12.1±2.0 months (range,8.1-16.0 months). In EPR group,the survival rate was 15.4% with the mean survival time of 14.5±3.4 months (range,7.8-21.3 months). The median survival after operation for patients was 11.0 months for both groups,and there was no statistical deference between two groups (P=0.147).
Figure 1.
The Kaplan–Meier survival rate analysis of IMN and EPR groups. There was no statistical significance between two groups (log-rank P=0.128).
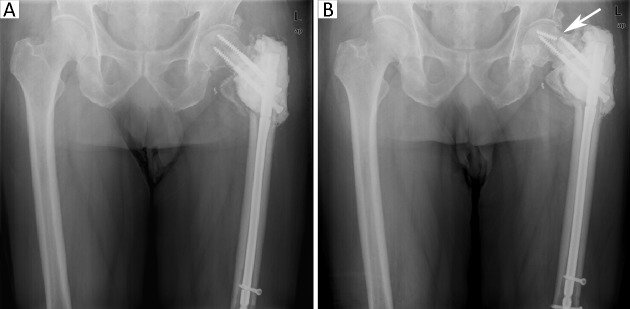
Death and complications
No patients died intra-operatively. There was one breakage of fixation in IMN group (Figure 2). Six patients developed lower extremity arterial thrombosis and 1 patient developed superficial wound infections in IMN group compared with 3 lower extremity arterial thrombosis and 1 superficial wound infection in EPR group. There was no loss of reduction or implant failure in EPR group (Figure 3).
Figure 2.
X-ray showed IMN (A) in a 64-years-old male with bone metastases of liver cancer and one breakage of proximal femoral nail occurred 3 months after operation (B).
Figure 3.
X-ray showed EPR in a 65-years-old male with bone metastases of clear cell carcinoma of kidney.
Discussion
Difficulties still exist in treatments of patients with bone metastasis who also develop pathological fractures. The foremost aim of treatment was to relieve pain,allowing patients acquired better life quality (3). However,for those patients who were estimated with longer life span,fixation was another issue as destructed bones were not able to reunite (6). The method of reconstruction was depending on the level of bone destruction,as well as the clinically related limitations of patients. Studies have shown that IMN and EPR are two major treatments with effective clinical outcomes for proximal femur metastasis. However,some clinically related issues for both methods were still uncertain.
Timing and methods of surgery
Proximal femur metastasis was usually found as pain started. For some patients who were not regularly followed up. Proximal femur metastasis was not found until developing a pathological fracture. Miles score was the most common way of assessment. However,the timing of surgery still remained controversy. In Harrington’s study,he thought the indication of prophylactic fixation was 50% destruction of bones or lesions longer than 2.5 cm (7). However,Arvinius believed that patients would receive advantages from prophylactic fixation at early stage without pointing out the timing of surgery (8). One of the reasons was the limited frequency of follow-up according to patient’s general condition. In addition,interval between bone scans was relatively long for most of the patients,causing difficulties in metastasis diagnose. Although CT was the most accurate assessment for bone destruction evaluation,it was still difficult to predict when the fractures would occur.
According to Yang’s report (9),they suggested EPR as a preferred treatment for Type I and Type Ⅱ proximal femur metastasis,whereas IMN could be performed for Type Ⅱ or Type Ⅲ. The principles of methods to be selected for reconstruction in our study were: 1) depending on the patient’s general condition and levels of destruction. EPR was preferred for patients with metastasis above trochanteric area (without entotrochanter),whereas IMN was favored for metastasis at entotrochanter or calcar femorale; 2) EPR was performed for young patients whereas IMN was preferred for senior patients; and 3) for patients with relatively good conditions,EPR was favored. IMN was performed on the weak ones. Safety was the first issue to consider,meanwhile the assessment of preoperational APACHE Ⅱ score could be the reference for method selection. Generally speaking,the higher the APACHE Ⅱ score,the higher the risk of surgery (10). In our research,the APACHE Ⅱ score was higher in IMN group than EPR group. However,it was not statistically significant,which might arise from the limited cases.
Surgical trauma
In Steensma’s research,they believed that EPR would lead to better fixation and lower failure rate (11). But the clinically related issues and life quality still require a retrospectively review of large scale of reports. Piccioli thought that IMN would also achieve pain control,allowing the patients to regain independency (12). Selection bias will be difficult to eliminate as both methods owned advantages.
In our study,the mean operation time was 59.5±6.1 min with the mean blood loss of 571.4±96.9 mL for IMN group. For EPR group,the mean operation time was 75.4±7.8 min with the mean blood loss of 753.8±143.6 mL. Both the operation time and the blood loss were less in IMN compared with EPR group (P=0.001,P=0.001,respectively). In IMN group,the operation steps were precisely controlled. The location of IMN was confirmed before lesion curettage. Blood loss mainly occurred during lesion curettage,as blood vessels were rich around tumors. Therefore we performed curettage with large curette in order to control the blood loss. Once the amount of bleeding decreased,the main nail was inserted immediately together with placement of supplemental cement for additional structural support. For EPR group,we performed radical resection with the largest possible exposure area,leading to longer operation time and increase in blood loss.
Therefore we chose EPR for young patients with generally good conditions as it may cause more blood loss. On the contrary,for senior and weak patients,IMN approach was favored for shorter operation time and less blood loss.
Some researchers showed different results from this study. Dong’s research (13) showed that the blood loss was less in EPR group. It is might because they took dynamic hip screw (DHS) extramedullary nailing into consideration.
Surgical outcomes and complications
The meta-analysis of Dong believed that EPR between trochanters would achieve higher scores of postoperative functional assessment (13). In our study,the VAS scores of pain showed significant increase,indicating that both treatments would aim to relieve pain effectively. Harris scores were higher in EPR group,as well as the KPS scores. Therefore,for those patients required higher level of functional outcomes and higher quality within expected life span,EPR was the first choice if allowed. From the aspect of scores,EPR group was better than IMN group. The most common complications of proximal femur metastasis were lower extremity deep venous thrombosis (DVT),superficial wound infections and pneumonia. According to Piccioli’s analysis of IMN for proximal femur metastasis,13.75% of patients developed lower extremity arterial thrombosis (12). Harvey’s study found that the complication rate of IMN group was 26% compared to 18% of EPR group (14). In our research,9 patients developed lower extremity arterial thrombosis with occurrence of 26.47%,which might due to the advanced age of patients. Meanwhile,the high coagulation blood state of metastatic patients,long-termed bed period due to pathological fractures,severe pain and surgical trauma would increase the risk of DVT.
Survival rate analysis and surgical methods
Mavrogenis believed that the survival rate of femur metastasis was depending on gender,the type of primary tumor,the amount of lesions,the location of metastasis,the surgical treatment,with or without pathological fractures and many other related factors (15). The bias of treatments would consider all the above elements. In this study,the Kaplan-Meier survival rate was analyzed between two groups,which showed a higher mean survival time in IMN group. However,the median survival time was both 11.0 months for two groups. The early survival rate in EPR group was higher,but it was lower after 11 months compared to IMN group. According to Fakler’s review of proximal femur metastasis reports,it showed that the mean survival time was 4.5 months in EPR group compared with 2.0 months in IMN group. However,it showed no statistical significance due to the limited cases (16). In Chandrasekar’s research,they found that the 1-year and 5-year survival rates were 40% and 15%,respectively,with a mean age of 56.3 years in EPR group (17). Piccioli’s study showed that the 1-year and 3-year survival rates of IMN group were 40% and 15%,respectively,with a mean age of 61.2 years (12). In our study,the mean age of patients in EMR group was 3.3 years younger than that in IMN group (P=0.03). Age was one of the factors,which needed to be considered for selection of surgical methods.
Many factors needed to be considered for surgical treatments: 1) the general conditions of patients including age,the type of tumor,with or without multiple visceral metastases,and the location and the number of bone metastasis; 2) the assessment of surgical risk (18),including the scale of lesion,estimated operation time and blood loss; 3) the estimated life span of patients,requirements of life quality,and the compliance and tolerance level of follow-up treatment; and 4) careful differential diagnosis (19). By considering all the factors above,we performed suitable surgical treatment,allowing patients to regain the maximum quality level and lower incidence of complications.
Conclusions
Both EPR and IMN for treating proximal femur metastasis achieved the same effects of pain control. In terms of surgical trauma,EPR group is bigger than the IMN group. The functional outcome of EPR group was better than IMN group. For survival rate,there was no statistical significance between the two groups. Therefore,the suitable surgical methods depended on the conditions and requirements of patients.
Acknowledgments
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
Contributor Information
Baojun Wang, Email: docwangbaojun@sina.com.
Ai Guo, Email: docguoai@sina.com.
References
- Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am. 2000;31:515–28. doi: 10.1016/s0030-5898(05)70171-1. [Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am 2000;31:515-28.] [DOI] [PubMed] [Google Scholar]
- Bryson DJ, Wicks L, Ashford RU. The investigation and management of suspected malignant pathological fractures: a review for the general orthopaedic surgeon. Injury. 2015;46:1891–9. doi: 10.1016/j.injury.2015.07.028. [Bryson DJ, Wicks L, Ashford RU. The investigation and management of suspected malignant pathological fractures: a review for the general orthopaedic surgeon. Injury 2015;46:1891-9.] [DOI] [PubMed] [Google Scholar]
- Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am. 2009;91:1503–16. doi: 10.2106/JBJS.H.00175. [Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am 2009;91:1503-16.] [DOI] [PubMed] [Google Scholar]
- Nilsson J, Gustafson P. Surgery for metastatic lesions of the femur: good outcome after 245 operations in 216 patients. Injury. 2008;39:404–10. doi: 10.1016/j.injury.2007.07.006. [Nilsson J, Gustafson P. Surgery for metastatic lesions of the femur: good outcome after 245 operations in 216 patients. Injury 2008;39:404-10.] [DOI] [PubMed] [Google Scholar]
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29.] [PubMed] [Google Scholar]
- Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 2003:S4–13. doi: 10.1097/01.blo.0000093045.56370.dd. [Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 2003:S4-13.] [DOI] [PubMed] [Google Scholar]
- Harrington KD. New trends in the management of lower extremity metastases. Clin Orthop Relat Res. 1982:53–61. [Harrington KD. New trends in the management of lower extremity metastases. Clin Orthop Relat Res 1982:53-61.] [PubMed] [Google Scholar]
- Arvinius C, Parra JL, Mateo LS, et al. Benefits of early intramedullary nailing in femoral metastases. Int Orthop. 2014;38:129–32. doi: 10.1007/s00264-013-2108-x. [Arvinius C, Parra JL, Mateo LS, et al. Benefits of early intramedullary nailing in femoral metastases. Int Orthop 2014;38:129-32.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Guo W, Yang RL, et al. Surgical classification and therapeutic strategy for metastases of proximal femur. Zhonghua Wai Ke Za Zhi (in Chinese) 2013;51:407–12. [Yang Y, Guo W, Yang RL, et al. Surgical classification and therapeutic strategy for metastases of proximal femur. Zhonghua Wai Ke Za Zhi (in Chinese) 2013;51:407-12.] [PubMed] [Google Scholar]
- Gao H, Wang B, Zhao L, et al. Analysis of the causes of complications and death of the femoral intertrochanteric fracture during perioperative period. Zhonghua Gu Ke Za Zhi (in Chinese) 2015;35:819–24. [Gao H, Wang B, Zhao L, et al. Analysis of the causes of complications and death of the femoral intertrochanteric fracture during perioperative period. Zhonghua Gu Ke Za Zhi (in Chinese) 2015;35:819-24.] [Google Scholar]
- Steensma M, Boland PJ, Morris CD, et al. Endoprosthetic treatment is more durable for pathologic proximal femur fractures. Clin Orthop Relat Res. 2012;470:920–6. doi: 10.1007/s11999-011-2047-z. [Steensma M, Boland PJ, Morris CD, et al. Endoprosthetic treatment is more durable for pathologic proximal femur fractures. Clin Orthop Relat Res 2012;470:920-6.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccioli A, Rossi B, Scaramuzzo L, et al. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury. 2014;45:412–7. doi: 10.1016/j.injury.2013.09.025. [Piccioli A, Rossi B, Scaramuzzo L, et al. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014;45:412-7.] [DOI] [PubMed] [Google Scholar]
- Dong JB, Wang ZY, Lu H, et al. Meta-analysis of internal fixation versus hip replacement in the treatment of trochanteric fractures. Zhongguo Gu Shang (in Chinese) 2015;28:245–51. [Dong JB, Wang ZY, Lu H, et al. Meta-analysis of internal fixation versus hip replacement in the treatment of trochanteric fractures. Zhongguo Gu Shang (in Chinese) 2015;28:245-51.] [PubMed] [Google Scholar]
- Harvey N, Ahlmann ER, Allison DC, et al. Endoprostheses last longer than intramedullary devices in proximal femur metastases. Clin Orthop Relat Res. 2012;470:684–91. doi: 10.1007/s11999-011-2038-0. [Harvey N, Ahlmann ER, Allison DC, et al. Endoprostheses last longer than intramedullary devices in proximal femur metastases. Clin Orthop Relat Res 2012;470:684-91.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavrogenis AF, Pala E, Romagnoli C, et al. Survival analysis of patients with femoral metastases. J Surg Oncol. 2012;105:135–41. doi: 10.1002/jso.22061. [Mavrogenis AF, Pala E, Romagnoli C, et al. Survival analysis of patients with femoral metastases. J Surg Oncol 2012;105:135-41. ] [DOI] [PubMed] [Google Scholar]
- Fakler JK, Hase F, Böhme J, et al. Safety aspects in surgical treatment of pathological fractures of the proximal femur-modular endoprosthetic replacement vs. intramedullary nailing. Patient Saf Surg. 2013;7:37. doi: 10.1186/1754-9493-7-37. [Fakler JK, Hase F, Böhme J, et al. Safety aspects in surgical treatment of pathological fractures of the proximal femur-modular endoprosthetic replacement vs. intramedullary nailing. Patient Saf Surg 2013;7:37. ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekar CR, Grimer RJ, Carter SR, et al. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108–12. doi: 10.1302/0301-620X.91B1.20448. [Chandrasekar CR, Grimer RJ, Carter SR, et al. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br 2009;91:108-12.] [DOI] [PubMed] [Google Scholar]
- Tao T, Chen S, Xu B, et al. Association between hsa-miR-34b/c rs4938723 T>C promoter polymorphism and cancer risk: a meta-analysis based on 6,036 cases and 6,204 controls. Chin J Cancer Res. 2014;26:315–22. doi: 10.3978/j.issn.1000-9604.2014.06.18. [Tao T, Chen S, Xu B, et al. Association between hsa-miR-34b/c rs4938723 T>C promoter polymorphism and cancer risk: a meta-analysis based on 6,036 cases and 6,204 controls. Chin J Cancer Res 2014;26:315-22.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao H, Wang B, Zhang X, et al. Maffucci syndrome with unilateral limb: a case report and review of the literature. Chin J Cancer Res. 2013;25:254–8. doi: 10.3978/j.issn.1000-9604.2013.03.05. [Gao H, Wang B, Zhang X, et al. Maffucci syndrome with unilateral limb: a case report and review of the literature. Chin J Cancer Res 2013;25:254-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]