Abstract
Purpose
Intraoperative assessment of tissue perfusion is important to predict wound healing or improvement of symptoms in patients with peripheral arterial disease (PAD) or vascular trauma. There is no widely accepted standard for intraoperative measurement of tissue perfusion. Here, we report the use of indocyanine green (ICG)-based angiography to determine the blood flow in patients with PAD and vascular trauma.
Methods
The SPY fluorescent imaging system was utilized. A dose of 3–5 mL of ICG (2.5 mg/mL) was injected intravenously followed by a 10 mL normal saline flush. The SPY imaging system was used to quantitatively assess perfusion. During the study period, the SPY imaging system was applied in 4 patients with PAD and one patient with vascular trauma.
Results
In 3 patients with PAD associated with an ischemic wound, complete wound healing was achieved with the indication of viable tissue by the SPY system. In one patient with severe claudication in both lower extremities, the ICG angiography was used to determine the increased blood flow after revascularization. In the case of vascular trauma, this imaging system enabled the delineation of viability of the injured tissue.
Conclusion
ICG angiography can determine the surface tissue viability in PAD patients. In cases of severe vascular trauma,the SPY system can be used to determine tissue perfusion. Further study is warranted to define the definite utility of this technology to assess perfusion, response to revascularization, and potentially, to predict the likelihood of wound healing.
Keywords: Indocyanine green, Angiography, Peripheral arterial disease, Perfusion
INTRODUCTION
Peripheral arterial disease (PAD) is not an uncommon vascular disease. The prevalence of PAD has been reported to range from 1.7% to 15.3% in the Korean population [1,2,3]. The clinical manifestations of PAD include intermittent pain produced by varying degrees of walking, resting pain, and ischemic wound. The goal of the PAD treatment is to relieve the ischemic pain and to achieve complete wound healing with and without excision of gangrenous tissue after proper revascularization.
Intraoperative assessment of tissue perfusion is important to predict wound healing or improvement of symptoms in patients with PAD or traumatic injury to the vessel. Therefore,accurate and reliable intraoperative evaluation of tissue perfusion is critical to reduce complications and to improve clinical outcomes. Clinical judgment is the most commonly used method for determining the blood supply [4], but when used alone, is not always completely reliable [5].
Transcutaneous tissue oxygenation has been used to augment the information provided by standard Doppler arterial waveform and pressure measurements [6]. Although these techniques may provide information on regional perfusion, information on the blood supply to the ankle or toe that helps to predict amputation levels is not obtained. Moreover, they also have significant variability, raising some doubts about their overall clinical utility. Currently, there is no widely accepted standard for intraoperative measurement of tissue perfusion.
The indocyanine green (ICG)-based imaging system was introduced to determine real-time arterial blood flow to an ulcerated and/or partially necrotic foot, capillary perfusion within the tissue in doubt, as well as to assess the most current degree of necrosis. Here, we report the clinical use of ICG angiography (ICGA) to determine the blood flow in patients with PAD and vascular trauma.
METHODS
The SPY fluorescent imaging system (Novadaq Corp., Bonita Springs, FL, USA) was utilized to determine arterial blood flow in five consecutive patients. Four patients had PAD and 1 patient had an open wound on the buttock after a traffic accident.
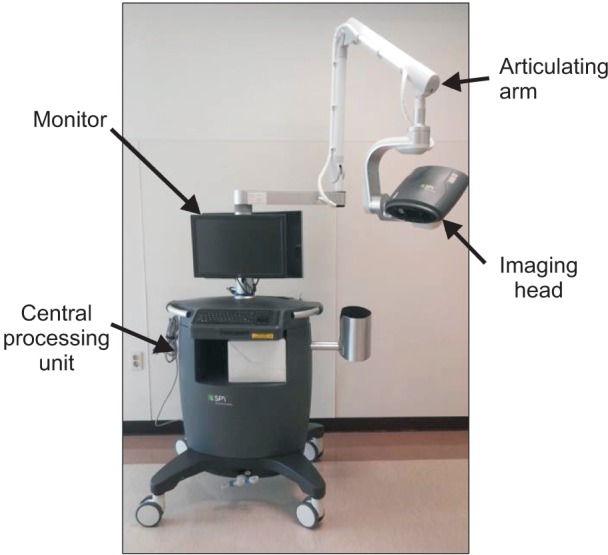
The SPY fluorescent imaging system consists of an imaging head equipped with a charge-coupled device (CCD) camera, a laser light source, and a distance sensor (Fig. 1). We positioned the CCD camera within the distance indicated by the range bar displayed on the monitor. The optimal distance from the tissue to the CCD camera was adjusted with the merging of two laser points.
Fig. 1. The SPY fluorescent imaging system (Novadaq Corp., Bonita Springs, FL, USA). The imaging head is attached to an articulating arm on a mobile cart containing the central processing unit, keyboard, monitor, and mouse.
A dose of 3–5 mL of ICG (2.5 mg/mL) was injected intravenously followed by a 10-mL normal saline flush. The SPY imaging system was used to quantitatively assess perfusion. The objective data on tissue perfusion were obtained before and after revascularization. If the necrotic tissue needed to be excised, tissue excision patterns were based on the tissue perfusion characteristics and the quantitative perfusion gradients.
RESULTS
During the study period, the SPY imaging system was applied in 4 patients with PAD and 1 patient with vascular trauma. Among the 4 PAD patients, 3 patients presented with critical limb ischemia Rutherford category 5 and 1 patient presented with severe claudication. The ICGA was performed before and after revascularization in PAD patients. Also, this imaging was performed before wound closure in the patient with a traumatic wound. We obtained the video image and the objective level of tissue perfusion.
Patient 1
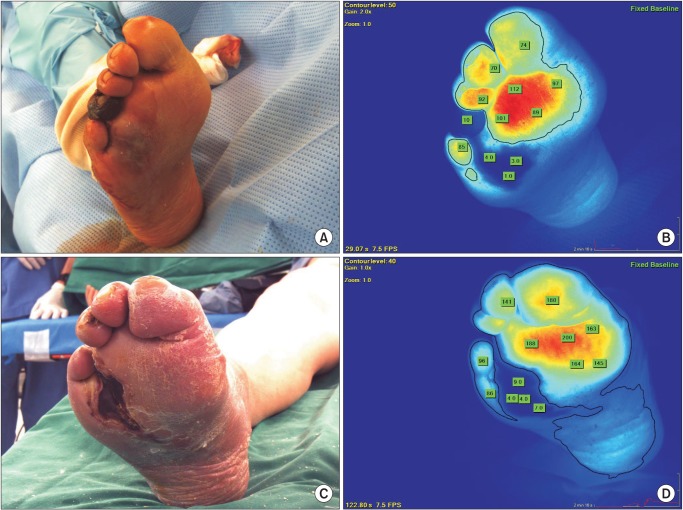
A 78-year-old male patient with a history of type 2 diabetes presented with gangrene of the right 4th toe, which was present since 2 months. The patient had a history of hypertension and loss of protective sensation (particularly in the right foot). Preoperative CT angiography showed a severe stenotic lesion in bilateral iliac arteries and diffuse atherosclerotic changes in the right superficial femoral artery. For the revascularization procedure, stent placement in bilateral iliac arteries and transluminal atherectomy using a directional atherectomy device were performed. After the revascularization procedure, excision of the necrotic tissue including the right 4th toe was planned. ICGA was used to determine tissue perfusion in the right foot, especially in the plantar region. It was impossible to determine the location of the viable margin in the right foot (Fig. 2A). However, preoperative ICGA showed clear demarcation of the ischemic area and perfusion state of the surrounding tissue (Fig. 2B). Three days after excision of the necrotic portion including the right 4th toe, clinical judgment revealed complete removal of the necrotic tissue and good perfusion in the surrounding tissue (Fig. 2C). With the use of postoperative ICGA, we could confirm adequate perfusion in the surrounding tissue (Fig. 2D). The wound was completely healed with closure of the surrounding viable tissue.
Fig. 2. Indocyanine green angiography (ICG) before and after amputation. (A) Before the operation, it was impossible to delineate the viable margin. (B) Preoperative ICG angiogram shows clear demarcation between the viable and ischemic regions. (C) Three days after excision of the necrotic portion including the right 4th toe, clinical judgment revealed viable tissue around the excised area. (D) Postoperative ICG angiogram confirmed the presence of viable tissue in this region.
Patient 2
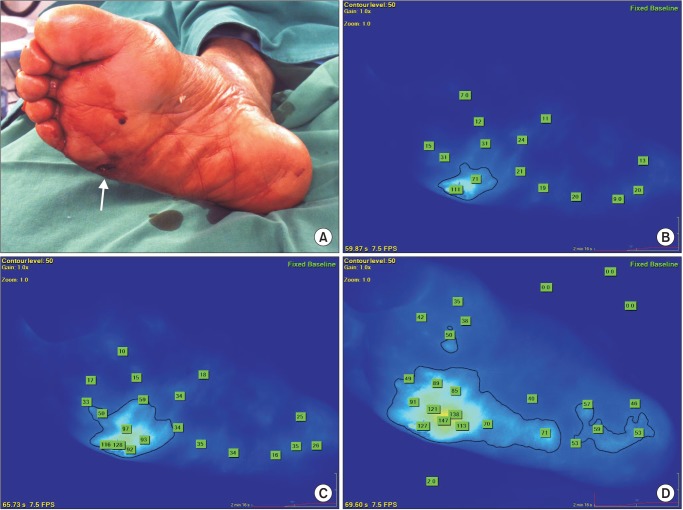
A 68-year-old male patient with a history of diabetes presented with an ulcerative lesion in the right foot. The patient had a history of coronary artery disease and chronic renal disease. Preoperative CT angiography showed a severe steno-occlusive lesion in the right superficial femoral, popliteal, and tibial arteries. Revascularization was planned with balloon angioplasty and selective stent placement for the residual stenosis or flow-limiting dissection after angioplasty. The ICGA was used to measure the perfusion after angioplasty. Fig. 3A and B show the initial picture of the right foot and ICGA before revascularization. After balloon angioplasty, the perfusion was increased (Fig. 3C). But the arteriogram after balloon angioplasty showed residual stenosis greater than 50% in the right superficial femoral artery. Therefore, we performed stent placement in the right superficial femoral artery. After stent placement, ICGA showed significantly increased perfusion in the right foot (Fig. 3D).
Fig. 3. Indocyanine green angiography (ICG) before and after revascularization. (A) Initial picture of the right foot shows ulceration over the plantar area (arrow). (B) Prerevascularization ICG angiogram shows decreased global perfusion in the right foot. (C) After balloon angioplasty, ICG angiogram shows slightly increased perfusion. (D) After stent placement in the region of the residual stenosis, ICG angiogram shows markedly increased perfusion.
Patient 3
A 73-year-old male patient presented with gangrene on the right 2nd toe. The patient had a history of renal cell carcinoma in the left kidney. One month before admission, he underwent left nephrectomy. Preoperative CT angiography showed diffuse, long-segment occlusion of the right superficial femoral and popliteal arteries. The femoro-popliteal bypass was performed using the ipsilateral greater saphenous vein. After successful revascularization, amputation of the gangrenous toe was planned. The ICGA was used to determine the tissue perfusion around the gangrenous portion after bypass surgery. Fig. 4 shows no perfusion in the right second toe and adequate perfusion around the gangrenous portion. After amputation of the right second toe, the wound was completely healed.
Fig. 4. Indocyanine green angiography (ICGA) for toe gangrene. (A) Gangrene of the right second toe is shown (arrow). (B) An ICGA grayscale image after bypass surgery shows no perfusion in the right second toe and adequate perfusion in the surrounding tissue. (C) The objective numbers are shown in an ICGA grayscale image. (D) An ICGA heat-map image shows adequate perfusion in the right foot after bypass surgery.
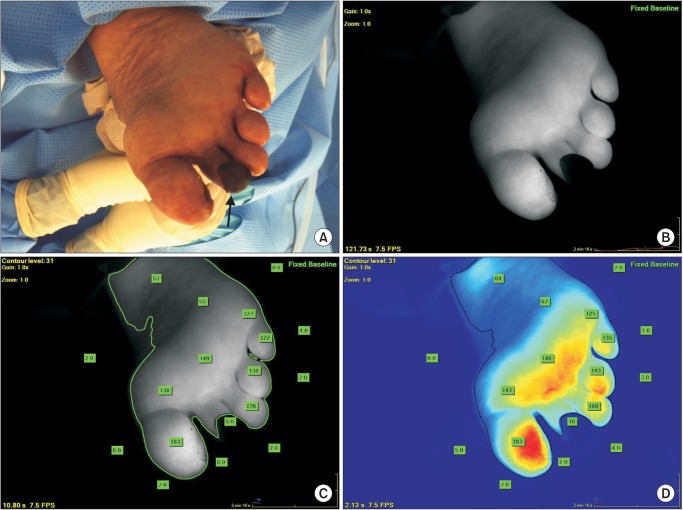
Patient 4
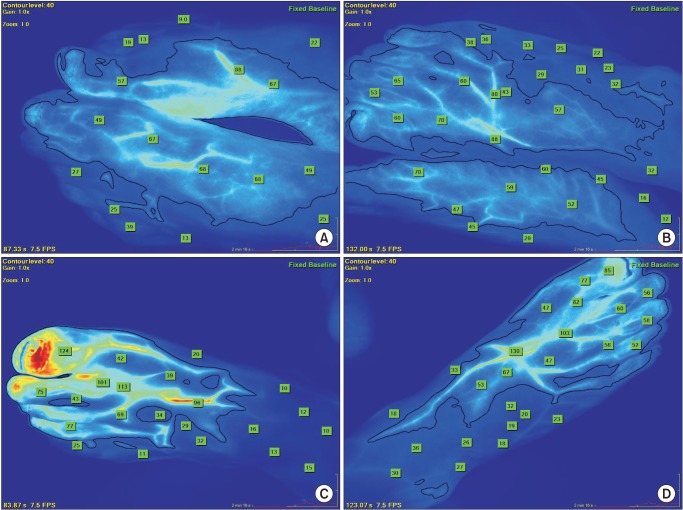
A 80-year-old male patient presented with severe claudication in both lower extremities. The patient had a history of hypertension. Preoperative CT angiography showed diffuse stenosis of the right superficial femoral artery and short segment occlusion of the left external iliac artery. The ICGA was used to determine the increased blood flow after revascularization. Revascularization was performed with transluminal atherectomy in the right superficial femoral artery and stent placement in the left external iliac artery. Fig. 5A and B show the baseline ICGA at 87 and 132 seconds, respectively. After stent placement in the left external iliac artery, ICGA showed markedly increased blood flow in the left leg at 83 seconds (Fig. 5C). After transluminal atherectomy in the right superficial femoral artery, ICGA showed increased perfusion in the right foot at 123 seconds (Fig. 5D). On left foot, the intensity of flow around the great toe increased from 49 to 124. And that of right great toe increased from 60 to 82.
Fig. 5. Indocyanine green (ICG) angiography after revascularization in a patient with claudication. (A, B) Baseline ICG angiograms show decreased perfusion in both feet at 87 seconds and 132 seconds, respectively. (C) After stent placement in the left external iliac artery, ICG angiogram shows increased blood flow in the left foot at 83 seconds. (D) After transluminal atherectomy of the right superficial femoral artery, ICG angiogram shows increased perfusion in the right foot at 123 seconds.
Patient 5
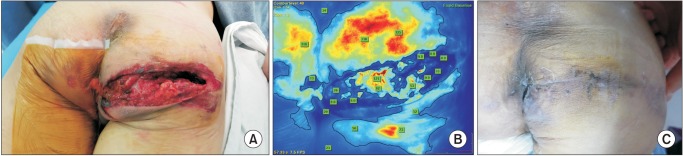
A 72-year-old female patient presented with a laceration wound on her right buttock due to traffic accident (Fig. 6A). The CT angiogram showed active bleeding from the branch of right hypogastric artery. For bleeding control, coil embolization was performed. After successful coil embolization, active bleeding was controlled. Before definite wound closure, ICGA was used to determine the blood supply to the tissue supplied by the artery that was embolized. Fig. 6A shows the open wound. ICGA after coil embolization showed adequate perfusion of the tissue around the open wound (Fig. 6B). After successful closure of the wound, complete healing was achieved (Fig. 6C).
Fig. 6. Indocyanine green (ICG) angiography for vascular trauma. (A) Initial picture shows a deep lacerated wound on the right buttock. (B) The ICG angiogram after coil embolization shows adequate perfusion of the tissue surrounding the injury. (C) Complete wound healing was achieved with the indication of ICG angiogram.
DISCUSSION
The SPY system provides an intraoperative laser angiograph as a vascular imaging methodology. This system utilizes a laser diode array to illuminate a maximum field of 18.5 cm2 × 13.5 cm2. A CCD camera can be configured to capture image sequences at 3.75 to 30 frames per second, depending on the desired recording time of between 30 seconds and up to a maximum of 4.5 minutes. Images are viewed on a high-definition monitor in real time, allowing for immediate evaluation in the operating room [7].
The SPY system utilizes ICG as a fluorescence agent to enable visualization. ICG is an inert, water soluble, nonradioactive and nontoxic contrast agent, which has been approved by the U.S. Food and Drug Administration since 1959. ICG is rapidly bound to plasma albumin upon intravenous administration and is exclusively excreted through the biliary system in an unconjugated form, without enterohepatic circulation, and a half-life in blood of 2.5 to 3 minutes [8]. ICG can be safely administered multiple times to the same person. It has an extremely low incidence of adverse reactions, 1/60,000 dose [8,9].
It has been already reported that the SPY system provides a useful assessment of tissue perfusion in a variety of clinical applications including breast reconstructive surgery, anastomotic perfusion during colorectal surgery, tissue perfusion during a large ventral hernia repair, and coronary artery bypass graft. In case series and prospective studies about breast reconstructive surgery, adequate intraoperative perfusion assessment using the SPY system was associated with reduced rates of postoperative necrosis and flap loss compared to clinical judgment alone [10,11,12,13]. In colorectal surgery, ICGA of colorectal anastomosis at the time of their construction is feasible and readily achievable with minimal added intraoperative time [14,15]. Patel et al. [8] reported the use of ICGA in complex abdominal wall reconstruction in patients with large ventral hernia defects. Operative debridement and wound infection development occurred more frequently in the non-ICG cohort compared with the ICG cohort (17% vs. 0%, respectively). Waseda et al. [16] evaluated the SPY system for the real-time assessment of graft patency during off-pump coronary artery bypass grafting in a total of 507 grafts in 137 patients. They concluded that the SPY system helped reduce procedure-related, early graft failures in off-pump bypass patients.
In our case series, the first 3 patients had an ischemic wound on their feet. ICGA was able to determine tissue perfusion and to confirm the extent of viable tissue after revascularization. Yamamoto et al. [17] reported that ICGA could accurately assess peripheral arterial perfusion in the saphenous vein graft anastomosed to the paramalleolar artery in 12 patients. Perry et al. [18] used ICGA to assess the viable tissue in patients with diabetic foot. ICGA clarified the extent of necessary debridement and provided an immediate indication of improvement in regional perfusion status following revascularization.
In the fourth patient, we used the SPY system to evaluate the improved perfusion after revascularization in a claudicant. For comparing the initial ICGA imaging with postrevascularization imaging, we captured the image at a similar time. The initial imaging depicted in Fig. 5A and B showed similar perfusion due to the occlusive lesion in the artery in both lower extremities. However, imaging after stent placement depicted in Fig. 5C and D showed markedly improved perfusion. But it is not possible to describe quantification of foot perfusion. Braun et al. [19] performed ICGA within 5 days of 31 revascularization procedures in patients with Rutherford class 5 and 6 ischemia. In this study, ICGA provided rapid visual and quantitative information about regional foot perfusion. Although ICGA can show this valuable information, it may not be used in real practice.
In cases of vascular trauma, traditional means for assessing viability using Doppler and angiography can have limited application. Connolly et al. [20] reported a case of complicated ankle fracture with severe vascular compromise, which illustrates the role of ICGA as an assessment tool to guide therapy and decision-making in cases of acute limb threat. Postoperative SPY imaging showed rapid uptake in the foot, which corresponded with the patient's clinical improvement. Complete limb salvage was achieved. In our case series, the last patient suffered vascular trauma. SPY imaging was the guide to decide on wound closure. Eventually, we achieved complete wound healing.
There are several limitations of this device. SPY technology is limited by perfusion information at a depth of 5 mm, therefore providing information solely on the superficial capillary system and is incapable of assessing deep tissue perfusion. Additionally, patients allergic to iodine or sulfa and penicillin should be excluded from any procedures involving ICG. It is not known whether ICGA provides the same or higher level of sensitivity and specificity demonstrated by other nonvascular measurements [18].
In conclusion, ICGA can determine the surface tissue viability in PAD patients with an ischemic wound. This imaging modality endeavors to delineate regional foot perfusion to guide revascularization therapy in PAD patients with claudication. In cases of severe vascular trauma, the SPY system can be used to determine the tissue perfusion. Further study is warranted to help define the utility of this technology to assess perfusion, response to revascularization, and potentially, to predict the likelihood of wound healing.
Acknowledgements
This work was supported by a grant from the Kyung Hee University in 2010 (KHU-20101886).
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Ahn S, Park YJ, Min SI, Kim SY, Ha J, Kim SJ, et al. High prevalence of peripheral arterial disease in Korean patients with coronary or cerebrovascular disease. J Korean Med Sci. 2012;27:625–629. doi: 10.3346/jkms.2012.27.6.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JY, Lee SW, Lee WS, Han S, Park YK, Kwon CH, et al. Prevalence and clinical implications of newly revealed, asymptomatic abnormal ankle-brachial index in patients with significant coronary artery disease. JACC Cardiovasc Interv. 2013;6:1303–1313. doi: 10.1016/j.jcin.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Park IH, Lee SC, Park IS, Nam CH, Ahn HS, Park HY, et al. Asymptomatic peripheral vascular disease in total knee arthroplasty: preoperative prevalence and risk factors. J Orthop Traumatol. 2015;16:23–26. doi: 10.1007/s10195-014-0305-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jallali N, Ridha H, Butler PE. Postoperative monitoring of free flaps in UK plastic surgery units. Microsurgery. 2005;25:469–472. doi: 10.1002/micr.20148. [DOI] [PubMed] [Google Scholar]
- 5.Mothes H, Dönicke T, Friedel R, Simon M, Bach O, Markgraf E. Indocyanine-green fluorescence video angiography used clinically to evaluate tissue perfusion in microsurgery. J Trauma. 2004;57:1018–1024. doi: 10.1097/01.ta.0000123041.47008.70. [DOI] [PubMed] [Google Scholar]
- 6.Boulton AJ, Armstrong DG, Albert SF, Frykberg RG, Hellman R, Kirkman MS, et al. Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31:1679–1685. doi: 10.2337/dc08-9021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurtner GC, Jones GE, Neligan PC, Newman MI, Phillips BT, Sacks JM, et al. Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res. 2013;7:1. doi: 10.1186/1750-1164-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel KM, Bhanot P, Franklin B, Albino F, Nahabedian MY. Use of intraoperative indocyanin-green angiography to minimize wound healing complications in abdominal wall reconstruction. J Plast Surg Hand Surg. 2013;47:476–480. doi: 10.3109/2000656X.2013.787085. [DOI] [PubMed] [Google Scholar]
- 9.Cherrick GR, Stein SW, Leevy CM, Davidson CS. Indocyanine green: observations on its physical properties, plasma decay, and hepatic extraction. J Clin Invest. 1960;39:592–600. doi: 10.1172/JCI104072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pestana IA, Coan B, Erdmann D, Marcus J, Levin LS, Zenn MR. Early experience with fluorescent angiography in free-tissue transfer reconstruction. Plast Reconstr Surg. 2009;123:1239–1244. doi: 10.1097/PRS.0b013e31819e67c1. [DOI] [PubMed] [Google Scholar]
- 11.Newman MI, Samson MC. The application of laser-assisted indocyanine green fluorescent dye angiography in microsurgical breast reconstruction. J Reconstr Microsurg. 2009;25:21–26. doi: 10.1055/s-0028-1090617. [DOI] [PubMed] [Google Scholar]
- 12.Murray JD, Jones GE, Elwood ET, Whitty LA, Garcia C. Fluorescent intraoperative tissue angiography with indocyanine green: evaluation of nipple-areola vascularity during breast reduction surgery. Plast Reconstr Surg. 2010;126:33e–34e. doi: 10.1097/PRS.0b013e3181dab2c2. [DOI] [PubMed] [Google Scholar]
- 13.Munabi JD, Jones GE, Elwood ET, Whitty LA, Garcia C. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: a prospective trial. J Plast Reconstr Aesthet Surg. 2014;67:449–455. doi: 10.1016/j.bjps.2013.12.040. [DOI] [PubMed] [Google Scholar]
- 14.Protyniak B, Dinallo AM, Boyan WP, Jr, Dressner RM, Arvanitis ML. Intraoperative indocyanine green fluorescence angiography: an objective evaluation of anastomotic perfusion in colorectal surgery. Am Surg. 2015;81:580–584. doi: 10.1177/000313481508100621. [DOI] [PubMed] [Google Scholar]
- 15.Ris F, Hompes R, Cunningham C, Lindsey I, Guy R, Jones O, et al. Near-infrared (NIR) perfusion angiography in minimally invasive colorectal surgery. Surg Endosc. 2014;28:2221–2226. doi: 10.1007/s00464-014-3432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waseda K, Ako J, Hasegawa T, Shimada Y, Ikeno F, Ishikawa T, et al. Intraoperative fluorescence imaging system for on-site assessment of off-pump coronary artery bypass graft. JACC Cardiovasc Imaging. 2009;2:604–612. doi: 10.1016/j.jcmg.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto M, Orihashi K, Nishimori H, Wariishi S, Fukutomi T, Kondo N, et al. Indocyanine green angiography for intraoperative assessment in vascular surgery. Eur J Vasc Endovasc Surg. 2012;43:204–208. doi: 10.1016/j.ejvs.2011.12.030. [DOI] [PubMed] [Google Scholar]
- 18.Perry D, Bharara M, Armstrong DG, Mills J. Intraoperative fluorescence vascular angiography: during tibial bypass. J Diabetes Sci Technol. 2012;6:204–208. doi: 10.1177/193229681200600125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braun JD, Trinidad-Hernandez M, Perry D, Armstrong DG, Mills JL., Sr Early quantitative evaluation of indocyanine green angiography in patients with critical limb ischemia. J Vasc Surg. 2013;57:1213–1218. doi: 10.1016/j.jvs.2012.10.113. [DOI] [PubMed] [Google Scholar]
- 20.Connolly PH, Meltzer AJ, Spector JA, Schneider DB. Indocyanine green angiography aids in prediction of limb salvage in vascular trauma. Ann Vasc Surg. 2015;29:1453, e1–e4. doi: 10.1016/j.avsg.2015.04.090. [DOI] [PubMed] [Google Scholar]