Abstract
For young, active patients with healthy hip cartilage, pelvic osteotomy is a surgical option in to address hip pain and to improve mechanical loading conditions related to dysplasia. Hip dysplasia may lead to arthrosis at an early age due to poor coverage of the femoral head and abnormal loading of the joint articulation. In patients with symptomatic dysplasia and closed triradiate cartilage (generally over age 10), including adolescents and young adults (generally up to around age 40), the Bernese periacetabular osteotomy (PAO) is a durable technique for addressing underlying structural deformity. The PAO involves a modified Smith-Petersen approach. Advantages of the Bernese osteotomy include preservation of the weight-bearing posterior column of the hemi-pelvis, preservation of the acetabular blood supply, maintenance of the hip abductor musculature, and the ability to effect powerful deformity correction about an ideal center of rotation. There is an increasing body of evidence that preservation of the native hip can be improved through pelvic osteotomy. In contrast to hip osteotomy and joint preservation, the role of total hip arthroplasty in young, active patients with correctable hip deformity remains controversial. Moreover, the durability of hip replacement in young patients is inherently limited. Pelvic osteotomy should be considered the preferred method to address correctable structural deformity of the hip in the young, active patient with developmental dysplasia. The Bernese PAO is technically demanding, yet offers reproducible results with good long-term survivorship in carefully selected patients with preserved cartilage and the ability to meet the demands of rehabilitation.
Keywords: Periacetabular osteotomy, Hip dysplasia, Pelvis
Core tip: The periacetabular osteotomy has been used to address structural deformity in young patients with acetabular dysplasia. The technique through a modified Smith-Petersen approach offers advantages: Preservation of the posterior column adds to the stability of the hemipelvis and protection of the sciatic nerve, preservation of the acetabular blood supply, and maintenance of hip abductor musculature. The juxta-articular osteotomy planes offer the ability to effect powerful deformity correction about an ideal center of rotation. While maximizing joint stability, coverage and congruency, the acetabular reorientation must also be assessed in light of the impingement-free range of motion.
INTRODUCTION
The goal of pelvic osteotomy in the setting of hip dysplasia is to address the biomechanical and structural abnormalities that lead to secondary osteoarthrosis under improper loading conditions. Poor coverage and/or incongruity due to developmental hip dysplasia may be corrected through reorientation of the acetabulum into an ideal position[1]. By improving these loading conditions, the static and dynamic instability patterns seen with hip dysplasia can be appropriately countered. While reorienting the osteotomy fragment and increasing the femoral head coverage improve load distributions across the joint, the amount and direction of correction required depends on the individual patient. This correction remains the critical - and certainly the most challenging - part of the procedure.
Prior to surgery, a thorough history and physical examination is required, including a careful assessment of gait, leg lengths, joint stability, and range of motion. High-quality radiographs should be obtained. These studies include an anteroposterior pelvis projection in proper rotation and tilt, a Dunn lateral view of the hip (e.g., 45-degree projection), and a false profile (faux profile) view of the affected hemipelvis[2]. To estimate the ability for containment and the amount of correction and resulting congruency possible with reorientation of the acetabulum, a functional abduction and internal rotation radiograph should be obtained as well. The patient’s age, body mass index, level of activity, and functional goals must also be incorporated into a decision to pursue surgical intervention.
The Bernese, or Ganz, periacetabular osteotomy (PAO) is the author’s preferred method for correcting acetabular dysplasia. Other pelvic osteotomies (e.g., triple, rotational) vary in the nature of the osteotomy planes, the ability to address open vs closed triradiate cartilage, and ability to correct acetabular orientation in multiple planes. The most frequent indication for performing the Bernese PAO is symptomatic acetabular dysplasia in an adolescent or young adult[3] with correctable deformity and preserved range of motion. The procedure is generally performed after closure of the triradiate cartilage (generally after age 10). Older patients (into the fourth decade) may be suitable candidates for the procedure based on the degree of arthrosis, as well as other factors such as ability to cope with rehabilitation period, activity level, expectations, obesity, and systemic conditions.
Contraindications to the Bernese PAO include advanced arthrosis (e.g., Tönnis Grade 2 or 3), subluxation resulting in a femoral head within a neoacetabulum, and a mismatch between a smaller acetabular radius and that of the femoral head which may cause worsening of joint congruity after reorientation. Patients with severe restrictions in range of motion are also poor surgical candidates.
SURGICAL TECHNIQUE
Equipment
An epidural catheter is placed pre-operatively and is continued post-operatively for pain control. Either regional anesthesia (e.g., spinal/epidural) vs general anesthesia with selective muscle relaxation may be used. General anesthesia may be performed with total intravenous anesthesia to maintain the ability to perform neuromonitoring during key exposure and reduction maneuvers that might put neurologic structures at highest risk. A Foley urinary catheter is also placed at the time of surgery. The patient is positioned supine on a radiolucent operating room table.
A fluoroscopy machine with a wide field of view may be used during the case for accurate and safe osteotomy cuts. A portable X-ray machine for obtaining intra-operative radiographs of the entire pelvis after acetabular correction is essential. Neuromonitoring during the case[4] is optional but advised to ensure safe dissection and osteotomy maneuvers. A cell-salvage system is used to collect intra-operative blood loss, and tranexamic acid is routinely dosed prior to incision and during wound closure. A foot rest for stabilizing the limb in a position of hip flexion is attached to the operating table, or, alternatively, a radiolucent triangle or specialized sterile leg holder may be used to achieve hip flexion throughout the majority of the procedure.
Specialized PAO retractors, osteotomes (including Ganz-type osteotomes), and surgical instruments may be obtained through commercial sets (e.g., manufactured by Subtilis/Smith and Nephew). Steinman pins and Kirschner wires (including 1/8th, 5/64th, 3/32nd diameters), as well as Schanz screws (5.0 mm, 6.0 mm) with appropriate T-handle adaptors for intra-operative reduction maneuvers should be available. Likewise, a ball-spike pusher and bone-holding forceps/clamps, including Weber-type (e.g., as found on Synthes Pelvic Reduction instrument tray) are important for fragment reduction and fixation. Long 3.5 mm/4.5 mm screws and appropriate length depth gauge, drill bits, bone taps (as found on a Synthes Large Fragment and/or Pelvic Reconstruction set) are needed for fixation. Reconstruction plates may be used if poor bone quality is encountered or if there is a very large correction performed. Wide and narrow oscillating saw blades are used for osteotomy cuts, and a high-speed bur is used for acetabuloplasty and/or osteochondroplasty. Bone wax, drains (e.g., medium Hemovac), and heavy non-absorbable suture for tendinous repair are other miscellaneous equipment needed during the procedure.
Other equipment that should be available, but necessarily open for the start of the case, includes appropriate femoral osteotomy plating system, if performing concurrent femoral osteotomy; and acetabular labral suture anchors, with appropriate drilling system, for labral repair if indicated. Similarly, hip arthroscopy equipment and viewing tower should be available if a concomitant hip arthroscopy procedure is preferred over capsulotomy.
Patient positioning and draping
The patient is placed in the supine position on a radiolucent table. The ipsilateral upper limb may be placed across the chest, and all bony prominences are well-padded. Fluoroscopic views (antero-posterior pelvis and roll-over oblique) should be confirmed prior to definitive prep and draping of the limb. Access to above the level of the iliac crest of the operative hemipelvis and down to the ipsilateral foot must be included within the prepped field. Neuromonitoring leads may be secured to the involved extremity before final sterile draping.
Surgical exposure
The modified Smith-Petersen approach, with preservation of the abductor musculature, is utilized. A curvilinear skin incision, centered about the anterior superior iliac spine (ASIS) is used. This incision extends proximally along the iliac crest and distally along the internervous interval of the tensor fascia lata and sartorius muscles. The fascia over the tensor is incised along the orientation of the muscle fibers. The lateral femoral cutaneous nerve is protected proximally about the ASIS, as well as during distal superficial exposure. The tensor fascial muscle belly is separated from the fascial envelope bluntly and retracted laterally; slight abduction may make this separation easier. Maintenance of this fascial sleeve also helps to protect the cutaneous nerve.
The ASIS is then osteotomized (block or wafer). This osteotomy maintains the origins of the sartorius and ilioinguinal ligament in continuity with the mobile fragment. The external oblique is dissected off the iliac wing in a subperiosteal plane for access to the inner pelvis down to the pelvic brim. The periosteum is elevated along with the iliacus muscle using straight and angled long Cobb-type elevators. If bleeding is encountered from the iliolumbar artery as it penetrates the iliac crest, the arterial orifice may be enlarged and then filled with bone wax.
The deep distal exposure is competed by reflecting the rectus tendon from the anterior inferior iliac spine, preserving a bed of tendon for later repair. As the deep fascia is opened distally, the pedicle to the tensor is exposed. This pedicle is freed, mobilized, and preserved. By dissecting the iliocapsularis muscle off the anterior hip capsule, an interval is developed medially under the iliopsoas tendon. The hip should be flexed up on a radiolucent triangle (or rested upon a foot bump) at this time to relax the anterior soft tissues. Completion of the dissection between the iliocapsularis, especially at its inferolateral border, allows the surgeon to palpate the calcar femoris through the capsule as well as the anterior surface of the ischium using closed scissors. Medial dissection exposes the iliopectineal bursa. Further subperiosteal exposure of the quadrilateral surface and pubic root allows for placement of a sharp Hohmann into the pubis, medial to the iliopectineal eminence.
Periacetabular osteotomies
The location of the various periacetabular osteotomy cuts are shown in Figure 1. Exposing the hip capsule inferiorly, the ischium is palpated with scissors. The ischium is triangular in shape with the base posterior. The infracotyloid groove, along with the obturator foramen medially and hamstrings origin laterally, is appreciated. The tips of the long curved dissecting scissors should be kept proximal to the obturator externus muscle. This scissor trajectory then guides the placement of a specialized curved osteotome to create the osteotomy just distal to the infracotyloid groove. The osteotome may be slid behind the scissors to ensure no entrapment of soft tissues. The position of the osteotome may be verified in anteroposterior and oblique fluoroscopic projections.
Figure 1.
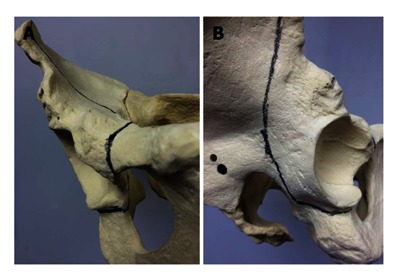
Location of osteotomy planes in the bernese periacetabular osteotomy. Frontal (A) and lateral (B) views of the pelvis demonstrating placement of juxta-acetabular osteotome cuts (dark lines).
The inferior retro-acetabular osteotomy begins at the infracotyloid groove and progresses toward the midpoint of the ischial spine. The osteotomy is done in both medial and lateral limbs: The osteotomy is begun on the medial side. During the lateral osteotomy, the sciatic nerve should be relaxed with the limb abducted, the hip extended, and the knee in slight flexion. Both tactile and aural feedback is critical in assuring the osteotome is within bone, as well as to prevent violation of the posterior column. The ischial osteotomy is an incomplete osteotomy, with depth to about 2.5 cm. It is important to cut the thicker medial cortex, while the thinner lateral cortex may break in a controlled fashion during the final osteotomy expansion maneuvers.
An assistant may then adduct the hip (maintaining flexion) to aid in access to the pubic ramus. The ramus periosteum is sharply cut on the superior cortical surface, and square-tip retractors are placed around the postero-inferior and postero-superior aspects of the pubic ramus. These retractors encircle the bone and protect the obturator nerve. Adequate circumferential release of the periosteum must be ensured to allow later fragment mobility, especially in younger patients with thick periosteum. A spiked Hohmann is secured into the superior cortex of the ramus a couple centimeters medial to the medial border of the iliopectineal eminence. This safely retracts the iliopsoas and the femoral neurovascular bundle medially, while maintaining a safe distance from the joint. A thin-kerf narrow saw (may alternatively use an osteotome) is used to start the osteotomy at an angle away from the joint; the osteotomy is completed with an osteotome. Removing a thin wafer of bone from the anterior cortex may help with sounding the far posterior cortex. The posterior cortex cut should exit medial to the obturator nerve. An osteotome may be used to gently splay the osteotomy ends to ensure that the cut is complete.
The ischial spine is identified with a reverse Eva retractor placed on the inside of the ischial spine after subperiosteal presentation of the quadrilateral surface. A muscular window along the lateral surface of the iliac wing is created, and a second reverse Eva is placed laterally. This tunnel along the outer table protects the gluteal muscles. The level of this iliac osteotomy is at a sufficient distance from the acetabulum to minimize risk of injury to the superior gluteal artery (supra-acetabular branch) and vascular arcade supplying the acetabulum. Furthermore, a larger bone bridge allows for better purchase of the Schanz screw during reduction, as well as to minimize the chance of joint surface violation while performing the second limb of the retro-acetabular cuts. A burr is used to make a target hole approximately 1 cm superolateral to the brim of the true pelvis. Alternatively, an osteotome may be used to mark this eventual vertex of the 120-degree osteotomy limbs. The osteotomy of the ilium is started with an oscillating saw: The first cut is along the medial cortex; subsequently, with the leg held in abduction, the lateral portion of the cortex is cut. Osteotomy of the posterior column is performed at an angle of 120 degrees to the previous iliac cut. Fluoroscopy may be used to confirm safe depth and trajectory. As with the iliac osteotomy, the posterior column cut begin within the medial cortex. The cut may be initiated using a straight or angled osteotome depending on the body habitus and angle of the osteotomy plane. To ensure that the retro-acetabular portion is complete, a straight osteotome is passed in a distal-ward direction; likewise, a Ganz-type osteotome is passed from the inside of the pelvis aiming laterally in sequential steps. Tactile and aural feedback is important at this step, and the bone may displace subtlety during progressive osteotomy maneuvers. Maintaining a safe distance from the subchondral bone prevents iatrogenic intra-articular fracture propagation.
A laminar spreader is placed into the iliac osteotomy site; a second laminar spreader may be placed in the second limb of the retro-acetabular osteotomy to effect the final displacement. Residual tethering of the posterior column osteotomy, if present, may be freed under direct vision with an angled bifid osteotome from the inside. During this maneuver the hip is again extended and abducted to relax the sciatic nerve.
Acetabular correction
A Schanz screw (5.0 mm) is inserted into the superior aspect of the mobile fragment, and rotatory motions test the osteotomy segment mobility. Combined movement of the Schanz screw and an inwards turn of the laminar spreader placed at the vertex of the supra-retro-acetabular osteotomy may help to free the fragment and maintain an adequate reorientation. A small bone hook or Weber clamp may be applied to the pubic segment to aid in reduction. The lack of complete mobility prompts the surgeon to review three problematic sites: The pubic osteotomy and accompanying periosteum, the posterior cortex at the vertex (junction of iliac and posterior column segments), and the inferior ischial cut. Mobility is again verified with the ability to flip the fragment.
The reorientation is then performed, keeping in mind that there is one ideal position of the fragment that optimizes joint loading conditions, while maintaining range of motion about an ideal center of hip rotation. For the more common hip dysplasia morphology, the acetabulum is usually repositioned with a combination of internal rotation, forward tilt/extension, and medial translation. As before, adjunctive reorientation tools may include a ball-spike pusher, Weber clamp, small bone hook, or a second Schanz pin. Provisional fixation is maintained with several terminally threaded or smooth Kirschner wires; the surgeon may choose to place two antegrade and one retrograde wires.
A properly projected and rotated pelvic radiograph is then obtained intra-operatively. This X-ray must be critically evaluated for the final acetabular orientation: The lateral center-edge angle, Tönnis angle/inclination, adequate medialization of the hip center of rotation, teardrop position, restoration of Shenton’s line, and version of the acetabulum. It is essential to not retrovert the acetabulum in addressing classic dysplasia. An example of an acetabular correction performed for hip dysplasia is presented in Figure 2.
Figure 2.
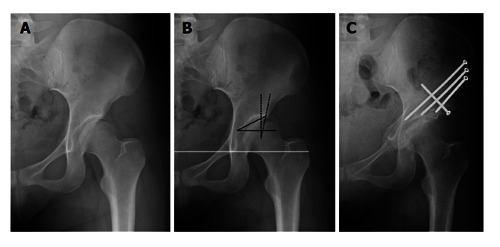
Acetabular radiographic measurements and correction. Pre-operative (A) antero-posterior radiograph of a hip with classic dysplastic. Basic radiographic measurements of dysplasia (B) include the lateral center edge angle (dashed black line; measure of lateral acetabular coverage), Tönnis angle (solid black line; measure of sourcil angle); the solid white line is the inter-teardrop line, which is the reference for pelvic tilt in the coronal plane; an anterior center edge angle on a false profile view completes the basic radiographic work-up. The post-operative (C) antero-posterior radiographic view of the same hip demonstrating satisfactory acetabular reorientation to correct bony dysplasia.
On-table range of motion is then performed to assess for potential secondary impingement or residual instability after the acetabular correction. The hip flexion should be at least 100 degrees. The mobile segment is secured with several 3.5 mm/4.5 mm fully threaded screws in antegrade and/or retrograde fashion. Fluoroscopic images may confirm that the acetabular reduction is maintained, along with position of fixation hardware.
After fragment fixation, an arthrotomy may be performed. This offers the opportunity to examine the acetabular labrum for repair if needed, as well as to address any offset abnormalities of the femoral neck region. Labral debridement vs repair (with possible augmentation) is performed, depending on the characteristics of the labral tear and quality of tissue. Osteochondroplasty using a curved osteotome and a burr may be performed at this time at the sites of femoroacetabular impingement.
Wound closure
After thorough irrigation of the joint and surgical field, the capsular incision is closed. Any bony prominences of the reoriented fragment may be trimmed with a saw and/or burr; the autograft may be used to fill the iliac osteotomy site. The rectus tendon is repaired with non-absorbable suture back to its footprint. The subspine region may be decompressed if impinging on the femur in deep flexion. The ASIS fragment is repositioned and fixed with a small-fragment screw or heavy suture in trans-osseous fashion. Closed suction drains may be used per surgeon preference. The fascia over the iliac wing, as well as distally over the tensor, is closed. Establishing a watertight seal of the fascia is important. The remainder of the superficial wound is closed in a routine, layered fashion.
POST-OPERATIVE CARE AND REHABILITATION
Mobility and weight-bearing status depends on whether the PAO has been performed alone or in conjunction with other procedures, such as femoral osteotomy and/or surgical hip dislocation. With maintenance of the posterior column and with good bone quality, partial weight-bearing (15 kg) is prescribed for the first 4-6 wk. A period of non-weight-bearing may be used in the setting of large corrections or poor bone quality. A continuous passive motion machine may be employed, especially if intra-articular work is performed. Routine deep venous thrombosis prophylaxis (e.g., low molecular weight heparin or aspirin) is used for the first six weeks. Heterotopic ossification prophylaxis is not routinely used. At four weeks, abduction strengthening exercises (first standing and then laying on opposite hip) is allowed, along with a stationary bike. Active flexion of the hip joint is prohibited for at least six weeks to protect the reattached hip flexor muscles. At eight weeks postoperatively, the patient is assessed clinically and radiographically: Healing is usually sufficient for full weight-bearing, and full muscular strengthening can be started. Flexion strength may take up to six months to return, and complete bony union will take several months to achieve. The majority of patients have pain-free range of motion at 2-3 mo, depending on how significant of a correction has been performed. Patients may generally return to sports activity between 6-12 mo, but patients with severe preexisting abductor and other functional weakness may take up to a year for complete rehabilitation.
CONCLUSION
The Bernese PAO is one of several acetabular osteotomies to address structural deformity in patients with closed triradiate cartilage, including adolescents and young adults with symptomatic dysplasia. The PAO technique involves a modified Smith-Petersen approach. Advantages of the Bernese PAO include preservation of the weight-bearing posterior column of the acetabulum, preservation of the acetabular blood supply, maintenance of the hip abductor musculature, and powerful deformity correction about an ideal center of rotation.
The Bernese PAO has been applied to complex acetabular dysplasia cases for over 30 years[5]. While it remains a technically demanding procedure[6-8], the potential to improve the natural history of hip dysplasia is well-demonstrated in mid- and long-term clinical studies[9-11]. Refinements in surgical technique and patient indications, in combination with the application of key femoroacetabular impingement concepts, have increased the understanding of hip pathomorphology and the parameters for acetabular reorientation[12].
Compared with a number of other pelvic osteotomy techniques, the Bernese PAO maintains the posterior column. By not violating the posterior column, prolonged immobilization and/or extensive pelvic fixation methods are obviated, and there remains inherent stability and good potential for union of the mobile fragment to the residual pelvis. The juxta-articular osteotomy planes also maintain the dimensions of the true pelvis and effects a powerful correction about an ideal center of hip rotation. With medialization of the hip joint, the abductor lever arm is maximized, and joint reaction forces are dampened.
Since its initial description, the PAO surgical technique has undergone various modifications[13]. The original approach involved stripping of the abductors from the iliac crest during the iliac and supra-acetabular osteotomy segment. Protecting the abductors not only preserves muscle function but also decreases the risk of osteonecrosis due to compromised acetabular vascular supply. Associated vessels include branches of the obturator, superior and inferior gluteal arteries, and capsular contributions to acetabular perfusion. Initially, the bone cuts were performed from both sides of the iliac wing; the bone cuts are now predominantly performed from the inner aspect of the pelvis to further preserve the abductors. More recently, it has become apparent that hip flexion strength is decreased post-operatively, and thus a rectus-sparing approach has been supported by some centers. This technique variation leaves the direct and indirect heads of the rectus femoris attached. It is unclear whether this will solve the problem of flexion strength deficits, or whether injury to the most proximal branches of the femoral nerve during osteotomy of the pubis may be increased.
Other modifications to the original surgical technique include a two-incision technique. In this manner, the ischial osteotomy has been performed under direct visualization. The primary disadvantage of this technique involves dissection of the external rotators posteriorly, with risk to the medial femoral circumflex artery and blood supply to the femoral head. Additional variations to the technique include various minimally invasive incisions, including a trans-sartorial approach. Other investigators have presented the use of hip arthroscopy at the time of PAO to evaluate the articular cartilage and to address labral pathology, which obviates the need for capsulotomy and more distal exposure.
The femoral head in a dysplastic hip may have a decreased head-neck offset and lateral flattening from a hypertrophic gluteus minimus. When the acetabulum is reoriented in a position of excess lateral and/or anterior coverage, secondary femoroacetabular impingement may occur. Impingement has been recognized as a potential cause for continued pain after PAO. As a result, an arthrotomy (or hip arthroscopy as above) has been incorporated for evaluation and correction of intra-articular impingement. Careful recognition of acetabular version (e.g., avoidance of iatrogenic retroversion) during the correction also helps to minimize secondary impingement.
The osteotomy technique is technically demanding, yet offers reproducible results with good long-term survivorship in carefully selected patients with preserved cartilage and the ability to meet rehabilitation demands. Pelvic osteotomy should be considered as a preferred alternative to arthroplasty in the young, active patient with correctable structural deformity of the hip.
Footnotes
Conflict-of-interest statement: The author has no conflicts of interest to disclose pertaining to the subject of this review manuscript.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 25, 2015
First decision: October 8, 2015
Article in press: February 16, 2016
P- Reviewer: Konya MN, Papachristou GC, Robertson GA S- Editor: Gong XM L- Editor: A E- Editor: Liu SQ
References
- 1.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001;50:229–238. [PubMed] [Google Scholar]
- 2.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26–36. [PubMed] [Google Scholar]
- 4.Pring ME, Trousdale RT, Cabanela ME, Harper CM. Intraoperative electromyographic monitoring during periacetabular osteotomy. Clin Orthop Relat Res. 2002;(400):158–164. doi: 10.1097/00003086-200207000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am. 2010;92:1707–1714. doi: 10.2106/JBJS.I.00829. [DOI] [PubMed] [Google Scholar]
- 7.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 8.Hussell JG, Rodriguez JA, Ganz R. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;(363):81–92. [PubMed] [Google Scholar]
- 9.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 11.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 12.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 13.Leunig M, Ganz R. Evolution of technique and indications for the Bernese periacetabular osteotomy. Bull NYU Hosp Jt Dis. 2011;69 Suppl 1:S42–S46. [PubMed] [Google Scholar]


