Abstract
Methionine is an essential sulfur amino acid that is engaged in key cellular functions such as protein synthesis and is a precursor for critical metabolites involved in maintaining cellular homeostasis. In mammals, in response to nutrient conditions, the liver plays a significant role in regulating methionine concentrations by altering its flux through the transmethylation, transsulfuration, and transamination metabolic pathways. A comprehensive understanding of how hepatic methionine metabolism intersects with other regulatory nutrient signaling and transcriptional events is, however, lacking. Here, we show that methionine and derived-sulfur metabolites in the transamination pathway activate the GCN5 acetyltransferase promoting acetylation of the transcriptional coactivator PGC-1α to control hepatic gluconeogenesis. Methionine was the only essential amino acid that rapidly induced PGC-1α acetylation through activating the GCN5 acetyltransferase. Experiments employing metabolic pathway intermediates revealed that methionine transamination, and not the transmethylation or transsulfuration pathways, contributed to methionine-induced PGC-1α acetylation. Moreover, aminooxyacetic acid, a transaminase inhibitor, was able to potently suppress PGC-1α acetylation stimulated by methionine, which was accompanied by predicted alterations in PGC-1α-mediated gluconeogenic gene expression and glucose production in primary murine hepatocytes. Methionine administration in mice likewise induced hepatic PGC-1α acetylation, suppressed the gluconeogenic gene program, and lowered glycemia, indicating that a similar phenomenon occurs in vivo. These results highlight a communication between methionine metabolism and PGC-1α-mediated hepatic gluconeogenesis, suggesting that influencing methionine metabolic flux has the potential to be therapeutically exploited for diabetes treatment.
Keywords: acetylation, acetyltransferase, gluconeogenesis, methionine, peroxisome proliferator-activated receptor γ coactivator 1-α (PGC-1α) (PPARGC1α), transcription coactivator, glucose-6-phosphatase (G6pc), methionine transamination, methylthiopropionic acid (MTP), phosphoenolpyruvate carboxykinase (Pck1)
Introduction
Amino acid sensing is a critical mechanism that cells employ to maintain homeostasis and enable survival upon fluctuations in the nutritional environment (1, 2). Despite variability in side chain chemical structure, cells are able to distinguish the distinct amino acids through the use of specific tRNAs. The amino acid protein sensor GCN2 detects deficiencies in amino acids in a tRNA-dependent manner and reprograms cellular metabolism to modulate energy consumption and maintain homeostasis (3, 4). Although mTORC1 is not considered to be a direct sensor of amino acid levels, it functions similarly to GCN2 to alter metabolic pathways in response to amino acid deprivation (5). Methionine, a dietary essential amino acid, is among the more toxic of the l-amino acids, and hence its abundance needs to be precisely regulated (6, 7). The liver is the primary organ concerned with the detoxification of methionine, and hence its ability to sense alterations in concentrations of this amino acid is vital (8). The existence of any cross-talk between hepatic methionine metabolism and other nutrient-regulated metabolic processes in the liver, such as glucose production, requires further investigation.
Intracellularly, apart from being utilized for the synthesis of proteins, methionine acts as a precursor for various metabolites that are associated with the anabolism of biological macromolecules, including nucleic acids (9, 10). The two main routes for methionine catabolism include the transmethylation and transsulfuration pathways. The initial step in transmethylation involves conversion of methionine to S-adenosylmethionine (SAM).6 SAM plays a significant role as a donor of methyl groups and is also involved in formation of polyamines such as spermidine (11). As a consequence of methyl transfer, SAM is metabolized to homocysteine via the S-adenosyl homocysteine intermediate (9, 10). Homocysteine can then either be recycled back to methionine in a folate/choline-dependent manner or it can be shunted down the transsulfuration pathway. This transsulfuration process is composed of the condensation of homocysteine with serine succeeded by a hydrolysis reaction and results in the formation of cysteine via cystathionine. The cysteine produced can then be consumed in protein translation or synthesis of the antioxidant glutathione and the osmolyte taurine (9, 10).
In addition to the transmethylation and transsulfuration pathways, methionine is also shunted down the transamination pathway (12, 13). Flux of methionine down this pathway involves an initial transaminase-mediated conversion to α-keto-γ-methylthiobutyrate (KMTB) (14). KMTB is then oxidatively decarboxylated to 3-methylthiopropionate (MTP) through an irreversible reaction catalyzed by the branched chain 2-oxo acid dehydrogenase complex (BCKDC) (15). MTP is further metabolized to the gaseous methanethiol (16), which has been reported to then be broken down into simpler molecules, including hydrogen sulfide, dimethyl sulfide, and formic acid, with the end products being carbon dioxide and sulfur dioxide (17, 18). Although initial reports on methionine transamination suggested that it provides a route for the degradation and clearance of methionine (19), more recently researchers have claimed that transsulfuration serves as the major pathway for the detoxification of excessive methionine (20). Early studies in rats indicate that activity of the methionine transamination pathway is altered during fasting; however, no clear functional significance has been attributed to this pathway. Despite methionine transamination being suggested to occur in various rodent tissues including the liver, the fraction of methionine that is shunted through this pathway as well as its necessity in humans remains to be accurately determined.
One of the mechanisms that functions to maintain blood glucose levels within a narrow range involves glucose production by the liver, which is differentially regulated during the fasting and fed states (21). Hepatic gluconeogenesis is induced upon fasting and is extensively controlled by PGC-1α (22). This transcriptional coactivator interacts with hepatocyte nuclear factor 4α (HNF4α) and forkhead box protein O1 (FOXO1) to promote transcription of phosphoenolpyruvate carboxykinase (Pck1) and glucose-6-phosphatase (G6pc) genes, which encode two enzymes that significantly moderate gluconeogenesis (23, 24). The activity, localization, and stability of PGC-1α are regulated by various post-translational modifications, including acetylation, which is known to impede its transcriptional co-activating ability and leads to the suppression of gluconeogenesis (25–27). The acetylation status of PGC-1α is primarily determined by opposing activities of the general control nonrepressed protein 5 (GCN5) acetyltransferase and the NAD+-dependent silent mating type information regulation 2 homolog 1 (SIRT1) deacetylase (25, 26). Various signaling cascades converge on GCN5 and SIRT1 to regulate their activities, including those stimulated by insulin and glucagon (28, 29). These peptide hormones play a major role in defining the necessity for glucose production by the liver during fasting and fed states (30) and operate, at least in part, through regulating PGC-1α.
Identifying metabolites that link host nutritional status to hepatic glucose output is important for the development of novel therapeutics targeting diabetes. Here we report a potential role for methionine and its metabolic regulation in modulating PGC-1α-mediated hepatic gluconeogenesis and consequently blood glucose levels. Methionine flux down the transamination pathway leads to activation of the GCN5 acetyltransferase. This promotes PGC-1α acetylation and inhibition, leading to the suppression of hepatic glucose production. These results hint at the existence of cellular mechanisms that keep blood glucose levels in check through shunting metabolites down specific pathways in the liver to control gluconeogenesis.
Experimental Procedures
Cell Lines and Primary Hepatocytes Cultures
HEK293A and HepG2 cell lines were purchased from ATCC (CRL-1573 and HB-8065) and cultured in DMEM supplemented with 10% FBS. Cell cultures were maintained at 37 °C in a humidified incubator containing 5% CO2. Primary hepatocytes were isolated from 7–10-week-old male C57BL/6 mice by perfusion with liver digest medium (Life Technologies, 17703-034) followed by 70-μm mesh filtration. Primary hepatocytes were isolated from debris and other cell types by Percoll (Sigma, P7828) gradient centrifugation. Isolated hepatocytes were seeded in 6-well plates (4 × 105 cells per well) in plating medium (DMEM supplemented with 10% FBS, 2 mm sodium pyruvate, 1 μm dexamethasone, 100 nm insulin, and 1% penicillin/streptomycin). The medium was changed to maintenance medium (DMEM supplemented with 0.2% BSA, 2 mm sodium pyruvate, 0.1 μm dexamethasone, 1 nm insulin, and 1% penicillin/streptomycin) 3 h post-seeding. Medium was replaced daily with fresh maintenance medium for the duration of the experiment.
Adenoviruses and Infections
FLAG-HA-PGC-1α (mouse) and FLAG-GCN5 (mouse) adenoviruses were prepared as previously described (25, 26). Adenoviruses were generated using the pAdTrack/pAdEasy system and amplified in HEK293A cells. Adenoviruses were purified by cesium chloride gradient centrifugation and dialyzed in Buffer A (10 mm Tris-HCl (pH 8.0), 2 mm MgCl2, and 4% glycerol (v/v)). Cells were infected with the adenovirus (3 × 106 to 8 × 106 infectious particles per well) for 4 h after which the medium was changed. Cells were incubated for a further 48 h to allow for expression and then either lysed or treated with various stimuli before being lysed. Controls included infection with the adenovirus generated from the empty GFP backbone vector. Medium was replaced daily with fresh maintenance medium for the duration of the experiment as well as 3 h before harvesting.
Treatment of Cells with Stimuli
For treatment of primary hepatocytes with essential amino acids (EAAs), cells were incubated overnight with amino acid-free medium (Earle's balanced salt solution supplemented with 0.2% fatty-acid-free BSA, 25 mm glucose, Basal Medium Eagle (BME) vitamin mix, 2 mm sodium pyruvate, 0.1 μm dexamethasone, 1 nm insulin and 1% penicillin/streptomycin) to deplete all amino acids in the medium. For treatment of hepatocytes with methionine or its metabolites/analogs, before treatment cells were incubated for 3 h (unless indicated otherwise) in medium lacking methionine (DMEM (no methionine, no cystine) supplemented with 0.2 mm cystine, 0.2% fatty-acid-free BSA, 2 mm sodium pyruvate, 0.1 μm dexamethasone, 1 nm insulin, and 1% penicillin/streptomycin). For experiments monitoring the ectopically expressed PGC-1α acetylation status, primary hepatocytes were incubated in appropriate starvation medium for the indicated times. Cells were then treated with EAAs, methionine, or methionine metabolites/analogs for 2 h, unless indicated otherwise, after which they were harvested. For gene expression analysis in primary hepatocytes, starvation of cells was performed for 3 h as mentioned above; however, after methionine (or its metabolites/analogs) stimulation, cells were incubated for 4 h before harvesting. For gene expression analysis in HepG2 cells, cells were treated with DMSO or forskolin (30 μm) overnight after which HEPES or 1 mm methionine was added to the cells for 3 h before harvesting. Inhibition of deacetylases was accomplished with trichostatin A (TSA) or EX-527 (1 μm), which was added 4 h before methionine treatment. For studies utilizing rapamycin, the mTOR inhibitor (20 nm) was added 4 h before stimulation with methionine. In experiments involving aminooxyacetic acid (AOAA), the inhibitor was added 30 min before stimulation with methionine (or its metabolites/analogs).
Cell Lysis, Immunoprecipitation, and Western Blotting
Cell Lysis
After treatments, cells were washed twice in ice-cold PBS (pH 7.4) (Life Technologies) and lysed in ice-cold buffer. For whole cell extracts, cells were lysed in Buffer B (1× PBS (pH 7.4), 0.5% SDC (w/v), 0.1% SDS (w/v), 1 mm EDTA, 1 mm DTT, 1% IGEPAL (v/v), 5 mm NaF, 5 mm β-glycerophosphate, 5 mm sodium butyrate, and 20 mm nicotinamide) supplemented with cOmplete EDTA-free Protease Inhibitor Mixture (Roche Diagnostics). Lysates were then clarified by centrifugation at 15,000 × g for 15 min. To obtain nuclear extracts, cells were harvested in Buffer C (10 mm HEPES-KOH (pH 7.9), 10 mm KCl, 1.5 mm MgCl2, 0.5 mm DTT, 0.25% IGEPAL (v/v), 5 mm NaF, 5 mm β-glycerophosphate, 5 mm sodium butyrate, and 20 mm nicotinamide) supplemented with Protease Inhibitor Mixture. Once cytoplasmic fractions were separated, nuclear pellets were lysed in Buffer D (20 mm HEPES-KOH (pH 7.9), 125 mm NaCl, 1 mm EDTA, 1 mm DTT, 1% IGEPAL (v/v), 10% glycerol (v/v), 5 mm NaF, 5 mm β-glycerophosphate, 5 mm sodium butyrate, and 20 mm nicotinamide) supplemented with Protease Inhibitor Mixture.
Immunoprecipitation
Immunoprecipitation for ectopically expressed FLAG-HA-PGC-1α (for detection of PGC-1α acetylation) and FLAG-GCN5 (for GCN5 acetyltransferase activity assays) was performed with FLAG-beads (Sigma A2220) according to the manufacturer's protocol. Endogenous PGC-1α was immunoprecipitated with anti-PGC-1α antibody coupled to Dynabeads Protein A (Life Technologies 10001D). The lysates were precleared with Protein A-Sepharose CL-4B (GE Healthcare 17-0780-01). All immunoprecipitated samples were washed at least four times with lysis buffer. For all endogenous immunoprecipitation experiments, anti-rabbit IgG antibody was used as a negative control.
Western Blot Analysis
Samples were resolved by SDS-PAGE and then transferred to PVDF membranes (EMD Millipore). Membranes were blocked with 5% BSA or nonfat dry milk in Tris-buffered saline/Tween 20 (TBST) for 1 h and then incubated with primary antibodies at 4 °C overnight, according to the manufacturer's protocol. The membranes were washed with TBST and incubated with the appropriate HRP-conjugated secondary antibody at room temperature for 1 h. After washing with TBST, chemiluminescence detection was performed with ECL Western blotting detection reagents (Thermo Fisher Scientific).
Commercial Antibodies
Antibodies were: anti-acetylated-lysine (#9441), anti-GCN5 (#3305), anti-S6 (#2217), and anti-phospho-S6 (Ser-235/236) (#4856) (Cell Signaling Technology); anti-PGC-1α (#sc-13067) (Santa Cruz Biotechnology); anti-lamin B1 (#ab16048) and anti-rabbit IgG (#ab37415) (Abcam); anti-β-tubulin (#05-661) (Millipore); anti-rabbit IgG secondary (#711-035-152) and anti-mouse IgG secondary (#715-035-150) (Jackson ImmunoResearch).
Gene Expression Analysis
For gene expression analysis, after treatments, total RNA was isolated from cells or homogenized liver using TRIzol (Life Technologies) according to the manufacturer's protocol. cDNA was synthesized from 2 μg of RNA using random primers and a High Capacity cDNA Reverse Transcription kit (Applied Biosystems). A CFX384 Real-TimePCRSystem (Bio-Rad) and PowerSYBRGreenPCRMaster Mix (Applied Biosystems) were used to perform quantitative real-time-PCR gene expression analysis. Gene expression data were corrected against 36B4 control gene expression and normalized using the ΔΔCT method. All primers are available upon request.
Glucose Production Assays
Primary hepatocytes were infected with either GFP or FLAG-PGC-1α adenovirus. Two days post-infection, glucose production capacity of primary hepatocytes was measured by incubating the cells for 3 h in glucose-free medium (phenol-red/glucose-free DMEM, 0.2% BSA, ±2 mm sodium pyruvate, and ± 20 mm sodium lactate). Methionine (0.1, 3, 4 mm), MTP (4 mm), and methylthiopropylamine (4 mm) were added to the cells 3 h before collection of the medium samples. Medium aliquots were collected, and glucose levels were quantified using an enzyme-based glucose assay according to the manufacturer's protocol (Eton Bioscience). The glucose concentration was calculated based on the difference between pyruvate/lactate-free medium and pyruvate/lactate-supplemented medium.
In Vitro Acetyltransferase Activity Assays
Acetyltransferase assays were conducted with FLAG-tagged GCN5 immunoprecipitated from the nuclear fraction of hepatocytes infected with GCN5 adenovirus and treated with HEPES or 2 mm methionine as described earlier. Controls included immunoprecipitation from hepatocytes infected with the GFP adenovirus. FLAG-tagged GCN5 was eluted from FLAG antibody beads at 4 °C for 2 h with 3× FLAG peptide and used in a fluorometric acetyltransferase assay according to the manufacturer's protocol (Active Motif).
Animal Experiments
For mouse experiments, 7-week-old male C57BL/6 mice were purchased from Taconic Farms. After a 1-week acclimation period, mice were handled for 3 days and then fasted overnight for 16 h. Through intraperitoneal injections, mice were administered PBS, EAAs (300 mg/kg, dissolved in PBS), or methionine (100 mg/kg, 300 mg/kg, dissolved in PBS). All mice were sacrificed 2 h post-injection, and livers were removed and snap-frozen in liquid nitrogen until processed further for gene expression analysis or immunoprecipitation of PGC-1α. Before sacrifice, glycemia was measured by tail-bleeding using an Ascensia Elite Blood Glucose Meter (Bayer). The generation of the Gcn5 flox allele was previously described (31). To generate liver-specific deletion of Gcn5, Gcn5flox/flox (Gcn5f/f) mice were crossed with Gcn5flox/+; albumin-Cre+/− mice. Homozygous Gcn5f/f animals were identified using primers described in Lin et al. (31). Animal experiments were conducted in accordance with the Dana-Farber Cancer Institute Institutional Animal Care and Use Committee.
Statistics
All data are presented as the means ± S.E. One-way analysis of variance tests, and t tests were conducted along with corresponding post-tests as indicated; p < 0.05 was considered significant. *, p < 0.05; **, p < 0.01; ***, p < 0.001.
Results
Methionine Induces PGC-1α Acetylation in Primary Hepatocytes
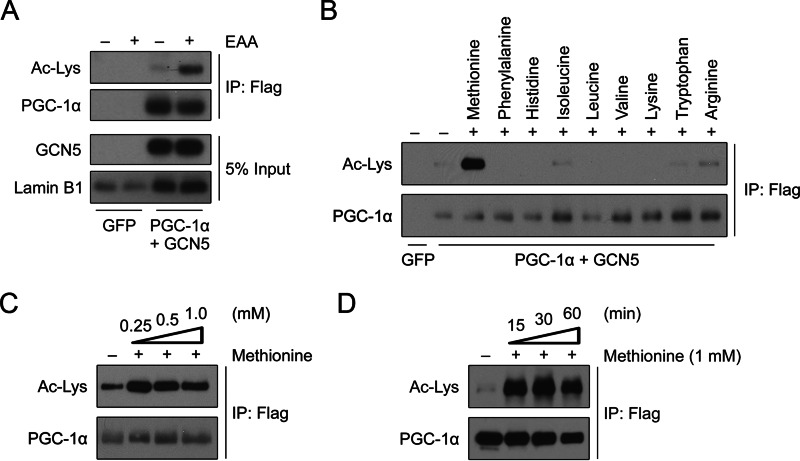
PGC-1α responds to nutrient and hormonal cues and plays a critical role in the regulation of energy metabolism in various tissues. Fasting induces PGC-1α activity in the liver to promote the gluconeogenic program. During fasting the availability of amino acids is also altered, and moreover, dietary amino acids are shown to contribute to the fed response along with insulin signaling (29). This suggests a possible role for the regulation of PGC-1α-mediated gluconeogenesis through amino acid signaling. To examine whether EAAs are able to regulate PGC-1α activity, we tested their ability to induce its acetylation in mouse primary hepatocytes, as this post-translational modification is known to inhibit the transcriptional coactivator gluconeogenic function. Interestingly, immunoprecipitation of ectopically expressed PGC-1α indicates an increase in its acetylation in hepatocytes treated with EAAs (Fig. 1A). To identify which of the EAAs contributed to the induction of PGC-1α acetylation, we incubated hepatocytes with individual EAAs (1 mm). Methionine promotes a marked increase in the acetylation of PGC-1α in contrast to the other EAAs tested (Fig. 1B). Methionine concentrations in murine hepatocytes are reported to range between 40 and 400 μm (32). In humans, plasma concentrations of methionine drop to around 30 μm during fasting, whereas after an oral methionine load they can reach around 1 mm and remain considerably elevated for a few hours (33). Dose and time dependence assays in primary hepatocytes indicate that 250 μm methionine administered for 4 h was sufficient to induce significant PGC-1α acetylation (Fig. 1C), with effects occurring relatively rapidly, within 15 min, when tested at 1 mm (Fig. 1D). These results suggest that the observed in vitro effects of methionine on PGC-1α acetylation occur at physiologically relevant methionine concentrations and durations of exposure.
FIGURE 1.
Methionine increased the acetylation of PGC-1α in primary hepatocytes. A, Western blot analysis of PGC-1α acetylation status upon EAA treatment. Primary hepatocytes were infected with FLAG-PGC-1α and GCN5 adenoviruses. The day after infection cells were treated overnight with Earle's balanced salt solution to deplete all amino acids in the medium. EAAs were added 4 h before harvesting. All cells were harvested within 48 h post-infection. FLAG-PGC-1α was immunoprecipitated (IP) with FLAG-antibody conjugated beads to analyze the acetylation status. B, Western blot analysis of PGC-1α acetylation status upon the addition of individual amino acids. The experiment follows the same procedure described in A, except the cells were treated with individual amino acids (1 mm) for 4 h before harvesting. C, Western blot analysis of PGC-1α acetylation status upon the addition of various concentrations of methionine for 4 h. The experiment follows the same procedure as described in A. D, Western blot analysis of PGC-1α acetylation status upon the addition of 1 mm methionine for various durations. The experiment follows the same procedure as described in A.
PGC-1α Acetylation Is Induced by Methionine through Modulating GCN5 Activity
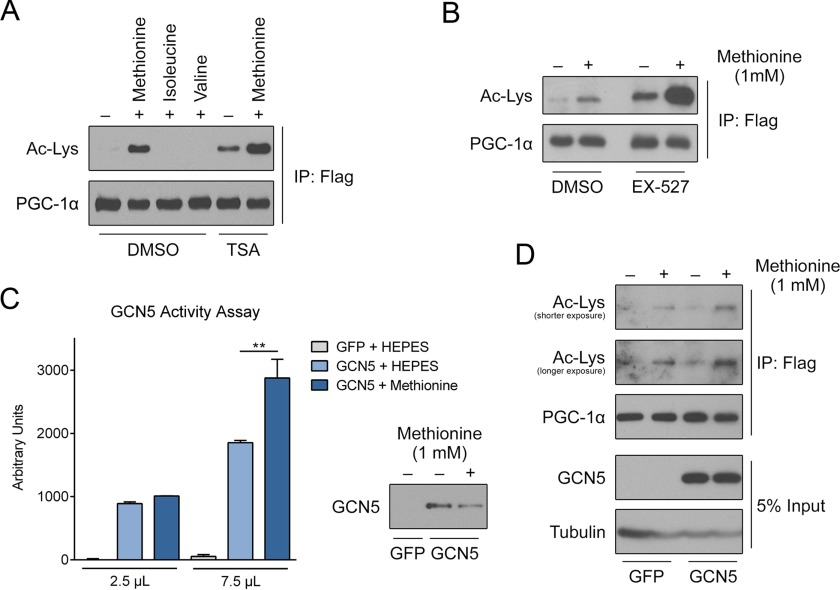
Regulation of PGC-1α acetylation levels is accomplished by the delicate interplay between acetyltransferases and histone deacetylases. To examine whether methionine-induced PGC-1α acetylation was a consequence of blunted histone deacetylase action, Class I/II histone deacetylases and SIRT1 were pharmacologically inhibited with TSA and EX-527, respectively. As expected, both TSA and EX-527 promote PGC-1α acetylation, but the inhibitors failed to suppress a further increase of PGC-1α acetylation induced by methionine (Fig. 2, A and B). As these results suggest the involvement of an acetyltransferase, we then tested whether methionine regulates PGC-1α acetylation through GCN5, a key PGC-1α acetyltransferase. Indeed, GCN5 immunoprecipitated from hepatocytes treated with methionine displayed an increase in catalytic activity in vitro relative to vehicle control (Fig. 2C). To further examine the involvement of GCN5 in methionine-induced PGC-1α acetylation, primary hepatocytes from liver-specific Gcn5−/− mice were employed. Ectopic expression of GCN5 in these Gcn5−/− hepatocytes enhances the effect of methionine on inducing PGC-1α acetylation (Fig. 2D). As methionine is also able to induce PGC-1α acetylation in the Gcn5−/− background, it implies that GCN5 may not account for the entire observed effect of methionine on PGC-1α acetylation; however, our results suggest that it a significant contributor. These results taken together suggest that methionine promotes PGC-1α acetylation, at least in part through activation of the GCN5 acetyltransferase.
FIGURE 2.
Methionine induced the acetylation of PGC-1α via modulating GCN5 activity. A, Western blot analysis of PGC-1α acetylation status upon methionine treatment with a Class I/II HDAC inhibitor, TSA. The experiment follows the same procedure as described in Fig. 1A except the cells were treated with TSA (1 μm) for 6 h before harvesting. Amino acids (1 mm) were added 2 h before harvesting. IP, immunoprecipitation. B, Western blot analysis of PGC-1α acetylation status upon methionine treatment with a SIRT1 inhibitor. The experiment follows the same procedure as described in A, except cells were treated with EX-527 (1 μm) for 6 h before harvesting. C, GCN5 in vitro acetyltransferase activity assay (n = 2). Primary hepatocytes were infected with either GFP or FLAG-GCN5 adenovirus. The cells were treated overnight with Earle's balanced salt solution medium, and methionine (1 mm) was added 2 h before harvesting. All cells were harvested within 48 h post-infection. FLAG-GCN5 was immunoprecipitated from nuclear extracts of cells that were treated with HEPES buffer or methionine. The activity assay was carried out according to the manufacturer's protocol. The corresponding amounts of GCN5 protein in the assay were analyzed via Western blot. D, Western blot analysis of PGC-1α acetylation status upon methionine treatment in Gcn5−/− primary hepatocytes. Primary hepatocytes were isolated from liver-specific Gcn5−/− mice. Primary hepatocytes were infected with FLAG-PGC-1α and either GFP or GCN5 adenovirus. Two days post-infection, cells were incubated in DMEM maintenance medium lacking methionine for 5 h before harvesting. Methionine (1 mm) was added 2 h before harvesting. For all multiple comparisons, one-way analysis of variance with post-hoc Tukey's test was used. **, p < 0.01.
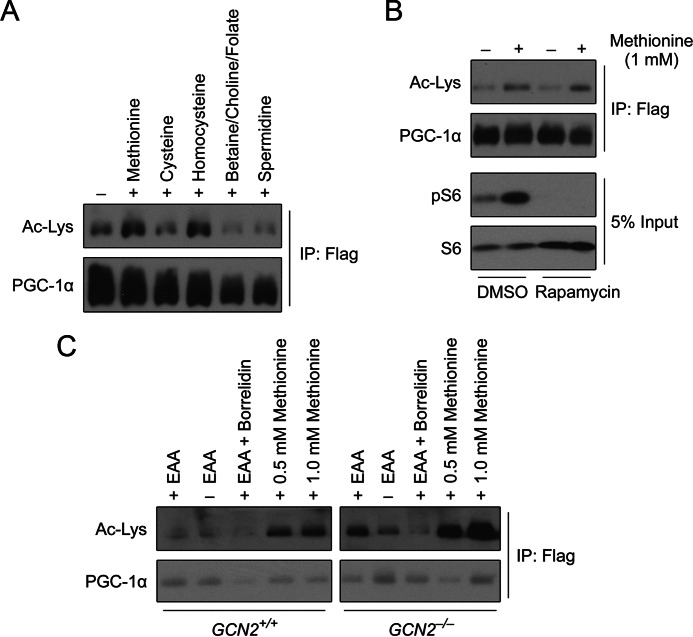
Classical Amino Acid Signaling Pathways Do Not Contribute to PGC-1α Acetylation Induced by Methionine
Metabolism of methionine primarily involves the transmethylation and transsulfuration pathways. To examine whether the flux of methionine through these pathways was responsible for the observed effects on PGC-1α acetylation, hepatocytes were treated with various pathway metabolites. Betaine/choline/folate, cysteine, and spermidine (1 mm each) were unable to induce PGC-1α acetylation (Fig. 3A). Interestingly, homocysteine was able to mimic the effects of methionine on the PGC-1α acetylation status (Fig. 3A); however, these effects are likely due to the reconversion of homocysteine to methionine. These results suggest that the methionine transmethylation and transsulfuration pathways are not significantly responsible for methionine-induced PGC-1α acetylation. Alternatively, amino acids can be sensed by mTORC1 and GCN2 to trigger downstream signaling cascades. To investigate whether the mTOR pathway was responsible for mediating the observed effects of methionine on PGC-1α, methionine treatments were performed in the presence or absence of rapamycin, an mTORC1 allosteric inhibitor. As indicated in Fig. 3B, rapamycin did not block methionine-induced PGC-1α acetylation. Levels of phosphorylated S6 were measured to determine the efficacy of rapamycin treatment. Additionally, to evaluate the involvement of GCN2, primary hepatocytes with the kinase knocked-out (GCN2−/−) were treated with methionine. Methionine-induced PGC-1α acetylation was unaffected in the GCN2−/− hepatocytes (Fig. 3C), suggesting that this amino acid sensor does not contribute to the process. Western blotting also indicated that there is an increased level of ectopically expressed GCN5 in GCN2−/− hepatocytes (data not shown). This could account for the increased PGC-1α acetylation observed in GCN2−/− hepatocytes (Fig. 3C). Collectively, these results suggest that methionine does not promote PGC-1α acetylation via the conventional amino acid signaling pathways.
FIGURE 3.
Methionine did not induce the acetylation of PGC-1α via classical amino acid signaling pathways. A, Western blot analysis of PGC-1α acetylation status upon methionine metabolite treatment. The experiment follows the same procedure as described in Fig. 1A except the cells were treated with various metabolites of methionine (1 mm each) for 2 h before harvesting. IP, immunoprecipitation. B, Western blot analysis of PGC-1α acetylation status upon methionine treatment with rapamycin. The experiment follows the same procedure as described in Fig. 1A. Rapamycin (20 nm) and methionine (1 mm) were added 6 h and 2 h before harvesting, respectively. Western blot of phospho-S6 was analyzed to ensure the efficiency of rapamycin treatment. C, Western blot analysis of PGC-1α acetylation status upon methionine treatment in GCN2+/+ and GCN2−/− primary hepatocytes. Primary hepatocytes were isolated from GCN2+/+ and GCN2−/− mice. The experiment follows the same procedure as described in Fig. 1A. EAAs or methionine were added 2 h and borrelidin (1 μm) 30 min before harvesting.
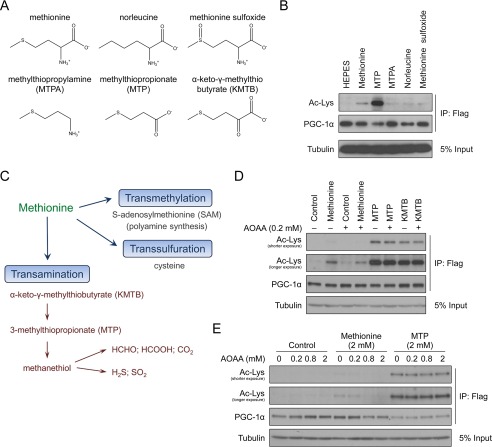
Flux of Methionine through the Methionine Transamination Pathway Increases the Acetylation of PGC-1α
To further investigate the mechanism through which methionine induces PGC-1α acetylation, various methionine analogs (Fig. 4A) were tested for their ability to mimic the effects of the amino acid. Despite significant structural similarity with methionine, methylthiopropylamine (MTPA), norleucine, and methionine sulfoxide were unable to induce PGC-1α acetylation; surprisingly, however, MTP was strikingly more potent than methionine (Fig. 4B). This result suggests a couple of things. First, because MTP should not be able to charge tRNAMet, it is unlikely that a mechanism involving tRNAMet contributes to the methionine-induced effects on PGC-1α; second, MTP is an intermediary metabolite that is generated through shunting of methionine down the transamination pathway (Fig. 4C), which raises the possibility that PGC-1α acetylation is a consequence of methionine transamination. To test this, KMTB, the intermediate metabolite between methionine and MTP, was tested for its ability to induce PGC-1α acetylation. Similar to MTP, KMTB is able to promote PGC-1α acetylation (Fig. 4D). Furthermore, AOAA, an aminotransferase inhibitor that blocks conversion of methionine to KMTB, is able to blunt PGC-1α acetylation induced by methionine but not that by KMTB and MTP (Fig. 4D). An AOAA dose-response assay indicates that the inhibitor is able to suppress methionine-induced PGC-1α acetylation to levels comparable with control treatment while being ineffective against MTP stimulation (Fig. 4E). In combination, these data indicate that methionine-induced PGC-1α acetylation primarily occurs via flux of the amino acid through the methionine transamination pathway.
FIGURE 4.
Methionine increased the acetylation of PGC-1α via the methionine transamination pathway. A, structures of methionine analogs used in this study. B, Western blot analysis of PGC-1α acetylation status upon treatment with methionine and its analogs. Primary hepatocytes were infected with FLAG-PGC-1α adenovirus. The day after infection cells were incubated overnight in DMEM maintenance medium lacking methionine and cysteine. Methionine and its analogs (2 mm) were added 2 h before harvesting. IP, immunoprecipitation. C, summary of the methionine transamination pathway. D, Western blot analysis of PGC-1α acetylation status upon treatment with AOAA, a transaminase inhibitor. The experiment follows a similar procedure as described in B, except the day after infection cells were incubated in DMEM maintenance medium lacking methionine for 6 h before harvesting. AOAA (0.2 mm) and methionine and its analogs (2 mm) were added 2.5 h and 2 h before harvesting, respectively. E, Western blot analysis of PGC-1α acetylation status upon the addition of methionine transamination pathway metabolites with various concentrations of AOAA. The experiment follows the same procedure as described in D except for treatment with various concentrations of AOAA.
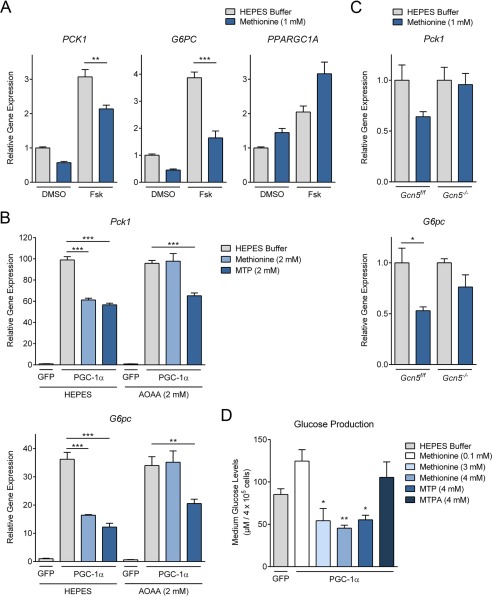
Methionine Suppresses Gluconeogenesis in Primary Hepatocytes
As acetylation of PGC-1α restricts its ability to stimulate gluconeogenesis and promote hepatic glucose production, we evaluated the physiological effects of methionine on the gluconeogenic program in liver cells in culture. We assessed the influence of methionine on two key enzymes in the gluconeogenic pathway, phosphoenolpyruvate carboxykinase (Pck1) and glucose-6-phosphatase (G6pc), which are well characterized targets of PGC-1α coactivation. In HepG2 human liver carcinoma cells we used forskolin treatment to activate the CREB pathway, which induces endogenous PGC-1α expression and activity. In these cells methionine was able to potently suppress forskolin-induced expression of Pck1 and G6pc (Fig. 5A). In mouse primary hepatocytes with ectopically expressed PGC-1α, methionine and MTP also caused a significant suppression of the PGC-1α-induced Pck1 and G6pc expression (Fig. 5B). Moreover, in accordance with earlier data, AOAA rescued methionine-induced, but not MTP-induced, repression of Pck1 and G6pc expression (Fig. 5B). To test the contribution of GCN5 to this suppression, we used the Gcn5−/− hepatocytes. Fig. 5C indicates that loss of GCN5 blunts the effects of methionine on Pck1 and G6pc gene suppression, suggesting that GCN5 at least partially contributes to the observed effect, which supports our earlier data on PGC-1α acetylation. Concomitant with the methionine-mediated reduction in gluconeogenic gene expression, we observed a decrease in ability of hepatocytes to produce glucose; methionine and MTP, but not methylthiopropylamine, were able to suppress PGC-1α-mediated glucose production in mouse primary hepatocytes (Fig. 5D). These data suggest that methionine, through its metabolism via the transamination pathway, is able to potently suppress the PGC-1α-mediated hepatic gluconeogenic program in vitro.
FIGURE 5.
Methionine repressed gluconeogenesis in primary hepatocytes. A, real-time PCR analysis of gluconeogenic gene expression upon methionine treatment in human liver carcinoma cells (n = 3). HepG2 cells were treated with DMSO or 30 μm forskolin (Fsk) overnight. HEPES buffer or methionine (1 mm) was added to the cells 3 h before harvesting. cDNA was generated from RNA, extracted using TRIzol-chloroform extraction methods. B, real-time PCR analysis of gluconeogenic gene expression upon the addition of methionine and MTP combined with AOAA treatment in primary hepatocytes (n = 3). Primary hepatocytes were infected with either GFP or FLAG-PGC-1α adenovirus. Two days post-infection, cells were incubated in DMEM maintenance medium lacking methionine for 7.5 h before harvesting. AOAA (0.2 mm) was added 4.5 h before harvesting. Methionine and MTP (2 mm) were added 4 h before harvesting. C, real-time PCR analysis of gluconeogenic gene expression upon the addition of methionine in Gcn5f/f and Gcn5−/− primary hepatocytes (n = 3). Primary hepatocytes were isolated from liver-specific Gcn5f/f and Gcn5−/− mice. Primary hepatocytes were infected with either GFP or FLAG-PGC-1α adenovirus. Two days post-infection, cells were incubated in DMEM maintenance medium lacking methionine for 7 h before harvesting. Methionine (1 mm) was added 4 h before harvesting. D, hepatic glucose production assay (n = 3). Primary hepatocytes were infected with either GFP or FLAG-PGC-1α adenovirus. Two days post-infection, glucose production capacity of primary hepatocytes was measured by incubating the cells in glucose free medium for 3 h. Methionine (0.1, 3, 4 mm), MTP (4 mm), and methylthiopropylamine (MTPA; 4 mm) were added to the cells 3 h before collection of the media samples. The glucose concentration was calculated based on the difference between pyruvate/lactate-free medium and 2 mm pyruvate/20 mm lactate-containing medium. For all multiple comparisons, one-way analysis of variance with post-hoc Tukey's test was used. *, p < 0.05; **, p < 0.01; ***, p < 0.001.
Gluconeogenesis Is Repressed by Methionine in Fasted Mice
Fasting is known to induce hepatic PGC-1α to promote gluconeogenesis. To evaluate if methionine has a physiological effect on PGC-1α in vivo, 8-week old male C57BL/6 mice were fasted overnight (16 h) and then administered methionine (100 mg/kg) intraperitoneally. Analysis of hepatic gene expression 2 h post-injection indicates that compared with vehicle control, methionine administration significantly repressed Pck1 and G6pc expression in vivo, which was accompanied by a reduction in blood glucose levels (Fig. 6A). Methionine administration in vivo decreased Ppargc1a expression (Fig. 6A), which contrasts the effects observed in HepG2 cells (Fig. 5A). One possibility that could account for this difference is that HepG2 being a cancer cell line is proliferative in nature, which could potentially result in metabolic variations when compared with normal hepatocytes. To verify that methionine induces PGC-1α acetylation in vivo, endogenous PGC-1α immunoprecipitated from liver nuclear extracts of fasted mice was assessed. Both EAAs (300 mg/kg) and methionine (100 and 300 mg/kg) administration notably increased PGC-1α acetylation compared with vehicle control (Fig. 6B), supporting data obtained from cultured mouse primary hepatocytes. These results highlight a potential role for amino acids, in particular methionine and its metabolic regulation, in modulating PGC-1α-mediated hepatic gluconeogenesis and consequently blood glucose levels.
FIGURE 6.
Methionine repressed gluconeogenesis in vivo. A, real-time PCR analysis of in vivo hepatic gluconeogenic gene expression and whole body glycemia upon methionine (100 mg/kg) intraperitoneal injection (n = 3). Eight-week old male C57BL/6 mice were fasted overnight (16 h). PBS or methionine (100 mg/kg, dissolved in PBS) was intraperitoneally injected into the mice. All mice were sacrificed 2 h post-injection, and livers were snap-frozen for gene expression analysis. Glycemia was measured via tail-bleeding at the time of harvesting. B, Western blot analysis of endogenous PGC-1α acetylation status in vivo. Endogenous PGC-1α was immunoprecipitated (IP) from nuclear extracts of livers. The experiment follows the same procedure as described in A. Mice were intraperitoneally injected with PBS, essential amino acids (300 mg/kg), or methionine (100 mg/kg, 300 mg/kg). For two experimental comparisons, two-tailed Student's t test was used. *, p < 0.05; ***, p < 0.001.
Discussion
The liver plays a major role in maintaining normal blood glucose homeostasis by increasing endogenous glucose production during periods of low nutrient availability. Upon refeeding, when nutrients become available, hormonal and nutritional cues signal the liver to suppress glucose production and switch to an energy storage mode. In type 2 diabetes, hepatic glucose production becomes refractory to these cues, and glucose production remains elevated even in the refed state, where it significantly contributes to fasting hyperglycemia observed in these patients (34). Although the hormonal signaling associated with the refed state, specifically insulin, has been extensively studied, the role of specific nutrients in the hepatic response to the refed state is largely unknown. Here, we identify the essential amino acid methionine as the only amino acid that is able to increase the acetylation state of PGC-1α. As a result, methionine leads to a suppression of hepatic glucose production in isolated mouse primary hepatocytes and to a reduction in fasting blood glucose in vivo.
Acute administration of methionine to isolated hepatocytes potently increases the acetylation status of PGC-1α by augmenting the catalytic activity of GCN5, the major acetyltransferase toward PGC-1α (26). Interestingly, the effect of methionine on PGC-1α acetylation does not require an active mTORC1, as in the presence of rapamycin methionine can still increase PGC-1α acetylation. In addition, in the absence of GCN2, the only known amino acid sensor that is activated during amino acid deficiency (35), methionine is still able to induce PGC-1α acetylation. These observations suggest that methionine and maybe other amino acids as well can induce specific cellular responses independently of these two pathways and modulate the response of the liver to the refed state. Specifically, we have found that flux of methionine through the transamination pathway is responsible for the methionine-induced PGC-1α acetylation.
We recently reported that dietary supplementation of essential amino acids to mice can contribute to the refed response by increasing hepatic cyclin D1 expression levels (29). As a result, the cyclin D1-CDK4 complex is activated, leading to an increase in GCN5 activity and suppression of PGC-1α during refeeding. Although the methionine-induced PGC-1α acetylation does not seem to be mediated by this pathway (data not shown), our study highlights the importance of GCN5 as a critical component of the refed response that can potentially be manipulated to control glucose homeostasis in the diabetic state. The molecular mechanisms underlying the methionine-mediated increase of GCN5 activity are currently unknown, and future studies will hopefully shed more light on this matter. It is possible that alteration in the post-translational modifications on GCN5, such as phosphorylation (28, 36) or acetylation (28), could be responsible for the increased activity observed. GCN5 is part of the SAGA (Spt-Ada-Gcn5 acetyltransferase) and ATAC (Ada2a-containing) coactivator complexes (37). Thus, there is the alternative possibility that other proteins in the acetyltransferase complexes could undergo post-translational modification to alter the complex composition and increase GCN5 activity, as has been described earlier (38). GCN5 is highly conserved across species (39) and was originally identified in yeast as an essential component for proper activation of the transcriptional response to amino acid starvation mediated by GCN4 (40). It was recently shown in lower organisms that amino acids can activate acetyltransferase activity of GCN5-related N-acetyltransferase (GNAT) protein (41). Whether GCN5 is a conserved component that can be activated in response to amino acid availability is of particular interest.
Methionine can be further metabolized in the liver through several different biochemical pathways. Of particular metabolic significance is the transmethylation pathway that involves the generation of SAM, the major methyl donor in the cell. Methionine degradation includes the transsulfuration and transamination pathways. Whether methionine degradation through transamination is quantitatively important is not clear. Although some studies suggest that this pathway might be important in rodents (9), other studies found that methionine is mostly degraded via transsulfuration (42). Studies in humans show that transamination exists, but its importance is not clear (13). Our study implies that under some conditions of methionine load, degradation through the transamination pathway can contribute to glucose homeostasis in the refed state.
Several studies have demonstrated the benefits of methionine restriction, which include prevention of insulin resistance and obesity (43), increase in energy expenditure (44) and life span extension (45). Interestingly, methionine restriction has also been reported to improve hepatic insulin sensitivity (46), which promotes glucose homeostasis. Here, we demonstrate that methionine administration upon fasting is able to suppress the hepatic gluconeogenic program. Methionine restriction studies are usually conducted over relatively longer durations, which differ from our experiments, which involve acute administration of methionine in the fasted state. An insight into any cross-talk between metabolic pathways stimulated under methionine restriction and methionine administration would be critical for developing dietary regimens employed for treating metabolic disorders.
Collectively, we have identified a novel role for the amino acid methionine in the adaptive response of the liver to the refed state. Our study highlights the importance of specific metabolites in the regulation of molecular components of insulin signaling, specifically the acetylation state of PGC-1α, and suggests that manipulation of these metabolites' flux can be potentially utilized to improve diabetic symptoms.
Author Contributions
J. E. D. and P. P. conceived the project. C. D. J. T., K. S., J. E. D., Y. L., and P. P. designed the research strategy and experimental approach. C. D. J. T., K. S., J. E. D., and Y. L. conducted the experiments. C. D. J. T., K. S., J. E. D., Y. L., and P. P. analyzed the data. M. I., J. M. O., M. P. J., and T. M. K. assisted in performing the experiments. C. D. J. T. and K. S. wrote the manuscript with editing from J. E. D. and P. P. P. R. G., S. P. G., and P. P. supervised the studies.
Acknowledgments
We thank members of the Puigserver laboratory for discussions on this project. We also thank Malcolm Whitman for helpful discussions and GCN2−/− hepatocytes. We thank Sharon Dent for Gcn5f/f mice.
This work was supported, in whole or in part, by National Institutes of Health Grants RO11069966 (NIDDK; to P. P.) and R24DK080261–06 (NIDDK; to P. P. and P. R. G.). The authors declare that they have no conflicts of interest with the contents of this article. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
- SAM
- S-adenosylmethionine
- KMTB
- α-keto-γ-methylthiobutyrate
- MTP
- 3-methylthiopropionate
- EAA
- essential amino acid
- TSA
- trichostatin A
- AOAA
- aminooxyacetic acid.
References
- 1. Gietzen D. W., and Rogers Q. R. (2006) Nutritional homeostasis and indispensable amino acid sensing: a new solution to an old puzzle. Trends Neurosci. 29, 91–99 [DOI] [PubMed] [Google Scholar]
- 2. Gallinetti J., Harputlugil E., and Mitchell J. R. (2013) Amino acid sensing in dietary-restriction-mediated longevity: roles of signal-transducing kinases GCN2 and TOR. Biochem. J. 449, 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wek R. C., Jackson B. M., and Hinnebusch A. G. (1989) Juxtaposition of domains homologous to protein kinases and histidyl-tRNA synthetases in GCN2 protein suggests a mechanism for coupling GCN4 expression to amino acid availability. Proc. Natl. Acad. Sci. U.S.A. 86, 4579–4583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dong J., Qiu H., Garcia-Barrio M., Anderson J., and Hinnebusch A. G. (2000) Uncharged tRNA activates GCN2 by displacing the protein kinase moiety from a bipartite tRNA-binding domain. Mol. Cell 6, 269–279 [DOI] [PubMed] [Google Scholar]
- 5. Sancak Y., Peterson T. R., Shaul Y. D., Lindquist R. A., Thoreen C. C., Bar-Peled L., and Sabatini D. M. (2008) The Rag GTPases bind raptor and mediate amino acid signaling to mTORC1. Science 320, 1496–1501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harper A. E., Benevenga N. J., and Wohlhueter R. M. (1970) Effects of ingestion of disproportionate amounts of amino acids. Physiol. Rev. 50, 428–558 [DOI] [PubMed] [Google Scholar]
- 7. Benevenga N. J. (1974) Toxicities of methionine and other amino acids. J. Agric. Food Chem. 22, 2–9 [DOI] [PubMed] [Google Scholar]
- 8. Marchesini G., Bugianesi E., Bianchi G., Fabbri A., Marchi E., Zoli M., and Pisi E. (1992) Defective methionine metabolism in cirrhosis: relation to severity of liver disease. Hepatology 16, 149–155 [DOI] [PubMed] [Google Scholar]
- 9. Griffith O. W. (1987) Mammalian sulfur amino acid metabolism: an overview. Methods Enzymol. 143, 366–376 [DOI] [PubMed] [Google Scholar]
- 10. Stipanuk M. H. (2004) Sulfur amino acid metabolism: pathways for production and removal of homocysteine and cysteine. Annu. Rev. Nutr. 24, 539–577 [DOI] [PubMed] [Google Scholar]
- 11. Fontecave M., Atta M., and Mulliez E. (2004) S-Adenosylmethionine: nothing goes to waste. Trends Biochem. Sci. 29, 243–249 [DOI] [PubMed] [Google Scholar]
- 12. Livesey G., and Lund P. (1980) Methionine metabolism via the transamination pathway in rat liver. Biochem. Soc. Trans. 8, 540–541 [DOI] [PubMed] [Google Scholar]
- 13. Blom H. J., Boers G. H., van den Elzen J. P., Gahl W. A., and Tangerman A. (1989) Transamination of methionine in humans. Clin. Sci. 76, 43–49 [DOI] [PubMed] [Google Scholar]
- 14. Scislowski P. W., and Pickard K. (1993) Methionine transamination: metabolic function and subcellular compartmentation. Mol. Cell. Biochem. 129, 39–45 [DOI] [PubMed] [Google Scholar]
- 15. Steele R. D., and Benevenga N. J. (1978) Identification of 3-methylthiopropionic acid as an intermediate in mammalian methionine metabolism in vitro. J. Biol. Chem. 253, 7844–7850 [PubMed] [Google Scholar]
- 16. Scislowski P. W., Bremer J., van Thienen W. I., and Davis E. J. (1989) Heart mitochondria metabolize 3-methylthiopropionate to CO2 and methanethiol. Arch. Biochem. Biophys. 273, 602–605 [DOI] [PubMed] [Google Scholar]
- 17. Toue S., Kodama R., Amao M., Kawamata Y., Kimura T., and Sakai R. (2006) Screening of toxicity biomarkers for methionine excess in rats. J. Nutr. 136, 1716S–1721S [DOI] [PubMed] [Google Scholar]
- 18. Dever J. T., and Elfarra A. A. (2008) l-Methionine toxicity in freshly isolated mouse hepatocytes is gender-dependent and mediated in part by transamination. J. Pharmacol. Exp. Ther. 326, 809–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mitchell A. D., and Benevenga N. J. (1978) The role of transamination in methionine oxidation in the rat. J. Nutr. 108, 67–78 [DOI] [PubMed] [Google Scholar]
- 20. Yamada H., Akahoshi N., Kamata S., Hagiya Y., Hishiki T., Nagahata Y., Matsuura T., Takano N., Mori M., Ishizaki Y., Izumi T., Kumagai Y., Kasahara T., Suematsu M., and Ishii I. (2012) Methionine excess in diet induces acute lethal hepatitis in mice lacking cystathionine γ-lyase, an animal model of cystathioninuria. Free Radic. Biol. Med. 52, 1716–1726 [DOI] [PubMed] [Google Scholar]
- 21. Cahill G. F., Jr. (1970) Starvation in man. N. Engl. J. Med. 282, 668–675 [DOI] [PubMed] [Google Scholar]
- 22. Yoon J. C., Puigserver P., Chen G., Donovan J., Wu Z., Rhee J., Adelmant G., Stafford J., Kahn C. R., Granner D. K., Newgard C. B., and Spiegelman B. M. (2001) Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature 413, 131–138 [DOI] [PubMed] [Google Scholar]
- 23. Puigserver P., Rhee J., Donovan J., Walkey C. J., Yoon J. C., Oriente F., Kitamura Y., Altomonte J., Dong H., Accili D., and Spiegelman B. M. (2003) Insulin-regulated hepatic gluconeogenesis through FOXO1-PGC-1α interaction. Nature 423, 550–555 [DOI] [PubMed] [Google Scholar]
- 24. Rhee J., Inoue Y., Yoon J. C., Puigserver P., Fan M., Gonzalez F. J., and Spiegelman B. M. (2003) Regulation of hepatic fasting response by PPARγ coactivator-1α (PGC-1): requirement for hepatocyte nuclear factor 4α in gluconeogenesis. Proc. Natl. Acad. Sci. U.S.A. 100, 4012–4017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodgers J. T., Lerin C., Haas W., Gygi S. P., Spiegelman B. M., and Puigserver P. (2005) Nutrient control of glucose homeostasis through a complex of PGC-1α and SIRT1. Nature 434, 113–118 [DOI] [PubMed] [Google Scholar]
- 26. Lerin C., Rodgers J. T., Kalume D. E., Kim S. H., Pandey A., and Puigserver P. (2006) GCN5 acetyltransferase complex controls glucose metabolism through transcriptional repression of PGC-1α. Cell Metab. 3, 429–438 [DOI] [PubMed] [Google Scholar]
- 27. Patten I. S., and Arany Z. (2012) PGC-1 coactivators in the cardiovascular system. Trends Endocrinol. Metab. 23, 90–97 [DOI] [PubMed] [Google Scholar]
- 28. Dominy J. E. Jr., Lee Y., Jedrychowski M. P., Chim H., Jurczak M. J., Camporez J. P., Ruan H. B., Feldman J., Pierce K., Mostoslavsky R., Denu J. M., Clish C. B., Yang X., Shulman G. I., Gygi S. P., and Puigserver P. (2012) The deacetylase Sirt6 activates the acetyltransferase GCN5 and suppresses hepatic gluconeogenesis. Mol. Cell 48, 900–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee Y., Dominy J. E., Choi Y. J., Jurczak M., Tolliday N., Camporez J. P., Chim H., Lim J. H., Ruan H. B., Yang X., Vazquez F., Sicinski P., Shulman G. I., and Puigserver P. (2014) Cyclin D1-Cdk4 controls glucose metabolism independently of cell cycle progression. Nature 510, 547–551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cherrington A. D., Stevenson R. W., Steiner K. E., Davis M. A., Myers S. R., Adkins B. A., Abumrad N. N., and Williams P. E. (1987) Insulin, glucagon, and glucose as regulators of hepatic glucose uptake and production in vivo. Diabetes Metab. Rev. 3, 307–332 [DOI] [PubMed] [Google Scholar]
- 31. Lin W., Zhang Z., Srajer G., Chen Y. C., Huang M., Phan H. M., and Dent S. Y. (2008) Proper expression of the Gcn5 histone acetyltransferase is required for neural tube closure in mouse embryos. Dev. Dyn. 237, 928–940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Korendyaseva T. K., Kuvatov D. N., Volkov V. A., Martinov M. V., Vitvitsky V. M., Banerjee R., and Ataullakhanov F. I. (2008) An allosteric mechanism for switching between parallel tracks in mammalian sulfur metabolism. PLoS Comput. Biol. 4, e1000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fukagawa N. K., Martin J. M., Wurthmann A., Prue A. H., Ebenstein D., and O'Rourke B. (2000) Sex-related differences in methionine metabolism and plasma homocysteine concentrations. Am. J. Clin. Nutr. 72, 22–29 [DOI] [PubMed] [Google Scholar]
- 34. Lin H. V., and Accili D. (2011) Hormonal regulation of hepatic glucose production in health and disease. Cell Metab. 14, 9–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Dever T. E. (1999) Translation initiation: adept at adapting. Trends Biochem. Sci. 24, 398–403 [DOI] [PubMed] [Google Scholar]
- 36. Barlev N. A., Poltoratsky V., Owen-Hughes T., Ying C., Liu L., Workman J. L., and Berger S. L. (1998) Repression of GCN5 histone acetyltransferase activity via bromodomain-mediated binding and phosphorylation by the Ku-DNA-dependent protein kinase complex. Mol. Cell. Biol. 18, 1349–1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang L., and Dent S. Y. (2014) Functions of SAGA in development and disease. Epigenomics 6, 329–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Riss A., Scheer E., Joint M., Trowitzsch S., Berger I., and Tora L. (2015) Subunits of ADA-two-A-containing (ATAC) or Spt-Ada-Gcn5-acetyltrasferase (SAGA) coactivator complexes enhance the acetyltransferase activity of GCN5. J. Biol. Chem. 290, 28997–29009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sternglanz R., and Schindelin H. (1999) Structure and mechanism of action of the histone acetyltransferase Gcn5 and similarity to other N-acetyltransferases. Proc. Natl. Acad. Sci. U.S.A. 96, 8807–8808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Georgakopoulos T., and Thireos G. (1992) Two distinct yeast transcriptional activators require the function of the GCN5 protein to promote normal levels of transcription. EMBO J. 11, 4145–4152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Xu J. Y., You D., Leng P. Q., and Ye B. C. (2014) Allosteric regulation of a protein acetyltransferase in Micromonospora aurantiaca by the amino acids cysteine and arginine. J. Biol. Chem. 289, 27034–27045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Finkelstein J. D., and Martin J. J. (1986) Methionine metabolism in mammals: adaptation to methionine excess. J. Biol. Chem. 261, 1582–1587 [PubMed] [Google Scholar]
- 43. Ables G. P., Perrone C. E., Orentreich D., and Orentreich N. (2012) Methionine-restricted C57BL/6J mice are resistant to diet-induced obesity and insulin resistance but have low bone density. PloS ONE 7, e51357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hasek B. E., Stewart L. K., Henagan T. M., Boudreau A., Lenard N. R., Black C., Shin J., Huypens P., Malloy V. L., Plaisance E. P., Krajcik R. A., Orentreich N., and Gettys T. W. (2010) Dietary methionine restriction enhances metabolic flexibility and increases uncoupled respiration in both fed and fasted states. Am. J. Physiol. Regul. Integr. Comp. Physiol. 299, R728–R739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lee B. C., Kaya A., and Gladyshev V. N. (2016) Methionine restriction and life-span control. Ann. N.Y. Acad. Sci. 1363, 116–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stone K. P., Wanders D., Orgeron M., Cortez C. C., and Gettys T. W. (2014) Mechanisms of increased in vivo insulin sensitivity by dietary methionine restriction in mice. Diabetes 63, 3721–3733 [DOI] [PMC free article] [PubMed] [Google Scholar]