Abstract
Background:
Alopecia areata (AA) and psoriasis are associated with various psychiatric comorbidities. Both greatly affect the quality of life (QOL) of patients and psychiatric comorbidities can further worsen it. Thus there is need to recognise psychiatric comorbidities and treat them in these patients.
Aims:
To determine the psychiatric morbidity and the QOL in these patients to study the factors affecting them.
Methodology:
50 patients each of psoriasis and AA were included. 50 people accompanying these patients served as control group. They were diagnosed for psychiatric disorders by clinical interview. Scales used were severity of alopecia tool for AA, psoriasis area and severity index for psoriasis, WHO-QOL scale, Hamilton Rating Scale for anxiety and depression.
Results:
22% and 38% patients in AA and psoriasis group respectively suffered from psychiatric disorder, depression was present in 18% and 24% of patients and 4% and 12% had anxiety disorders in respective groups. The control group had only 6% of psychiatric comorbidities. QOL scores had negative correlation with Hamilton-A, Hamilton-D and severity of psoriasis scores and they were statistically significant but not with severity of AA.
Conclusion:
Thus AA and psoriasis patients had more prevalence of psychiatric comorbidities and it had bearing on their QOL.
Keywords: Alopecia, psoriasis, psychodermatology, psychopathology, quality of life
Alopecia areata (AA) is a psychophysical dermatitis characterized by circular, round or oval spots without hair usually the size of a coin and occur in the scalp or other parts of the body whereas psoriasis is a chronic inflammatory skin disease that is characterized by thick, red, scaly lesions that may appear on any part of the body affecting 1–2% of general population.[1,2] Various studies have shown 66–78% prevalence of psychiatric morbidity in AA patients and 25–67% in psoriasis patients.[3,4,5,6,7,8]
Thus, there are enough evidences which show that psychiatric morbidity is higher in patients of AA and psoriasis. If they are not taken care of these comorbidities have bearing on treatment improvement of primary dermatological condition as well. Timely intervention in this regards will definitely improve patient's condition and thereby his quality of life (QOL).
So we undertook this study with aims to determine the psychiatric morbidity and the QOL in patients suffering from AA and psoriasis and to determine various factors related with psychiatric morbidity and those affecting the QOL in these patients.
METHODOLOGY
Each group comprised of 50 cases, age 18–65 years, attending the hair clinic and psoriasis clinic in dermatology outpatient department of a Tertiary Care Hospital. The dermatological diagnosis was made by qualified dermatologist working in the dermatology department. Patients were selected on first come first basis and fulfilling the inclusion criteria. Fifty people who accompanied these patients and not suffering from any dermatological illness served as control group. Patients with chronic debilitating diseases such as cancer, liver, renal and cardiac diseases, hypertension, diabetes and pregnant/lactating women were excluded.
The study was approved by the Institutional Ethics Committee. The subjects were explained purpose and process of our study and then written consent was taken. The demographic profile was collected in the semi-structured preformat and following data were collected:
The phenomenology of the AA and psoriasis including age of onset, duration, course of illness and treatment details were taken
The phenomenology of the psychiatric disorder, if present, including its age of onset, duration, course and treatment details were taken by detailed history taking by investigator and diagnosis was made according to Diagnostic and Statistical Manual of Mental Disorders Fourth Edition, Text Revision
Scales used included severity of alopecia tool (SALT) for AA, psoriasis area and severity index (PASI) for psoriasis, WHO-QOL BREF scale, Hamilton rating scale for anxiety and depression.
Tools used
Severity of alopecia tool score
National AA foundation working committee has devised “SALT score” (SALT score). Scalp is divided into four areas namely: Vertex - 40% (0.4) of scalp surface area; right profile of scalp - 18% (0.18) of scalp surface area; left profile of scalp - 18% (0.18) of scalp surface area; posterior aspect of scalp - 24% (0.24) of scalp surface area. Percentage of hair loss in any of these areas is percentage hair loss multiplied by percent surface area of the scalp in that area. SALT score is the sum of percentage of hair loss in all above mentioned areas.[9]
Psoriasis area and severity index score
PASI examines four body regions: (i) The head and neck, (ii) the hands and arms, (iii) the chest, abdomen and back (trunk) and (iv) the buttocks, thighs and legs. Each region is given a score to show how much of the region is affected by psoriasis (area) and a score to record how bad the psoriasis is (severity). The area score can range from 0 (no psoriasis) to 6 (all of the skin affected). The severity score for each region is reached by adding scores for redness, thickness and scale, each of which is graded from 0 to 4, giving a maximum of 12. The region scores are each weighted by the given amount and then added together to give the final PASI score.[10]
Statistical analysis
The data obtained was analysed and the tests used were the ANOVA, Chi-square test, Student's t-test and correlation was analyzed using Pearson's correlation coefficient. Two-tailed “P” value was obtained for all statistical analysis and score of P ≤ 0.05 was considered as statistically significant.
RESULTS
Sample characteristics
-
AA (n = 50):1.1. Mean age: 27.76 years
1.2. Males: 33, females: 17
-
Psoriasis (n = 50):2.1. Mean age: 39.76 years
2.2. Males: 35, females: 15
-
Control (n = 50):
3.1. Mean age: 32.84 years
3.2. Males: 14, females: 36.
Psychopathology
-
Mean duration of skin condition (P < 0.01):
1.1. AA: 2.67 years (range 1–12 years)
1.2. Psoriasis: 8.58 years (range 1–25 years)
-
Severity scoring of skin condition (P = 0.001):
2.1. Mean SALT score: 12.22 (0.4–71)
2.2. Mean PASI score: 4.424 (0.2–42)
-
Prevalence of psychiatric disorder (P = 0.001):
3.1. AA: 11 (22%)
3.2. Psoriasis: 19 (38%)
3.3. Control: 3 (6%)
-
Type of psychiatric disorders present (P = 0.005):
4.1. AA: Anxiety disorder: 2 (4%), depression: 9 (18%)
4.2. Psoriasis: Anxiety disorder: 6 (12%), depression: 12 (24%), schizophrenia: 1 (2%)
4.3. Control: Anxiety disorder: 2 (4%), schizophrenia: 1 (2%)
-
Presence of substance use (P < 0.01):
5.1. AA: 9 (18%)
5.2. Psoriasis: 26 (52%)
5.3. Control: 0 (0%).
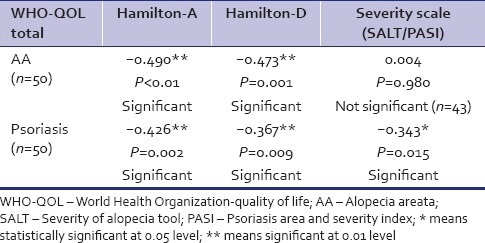
The mean WHO-QOL scores were higher in AA group (276.52) compared to 245.76 in psoriasis group and 265.56 in control group and the difference was statistically significant (P = 0.01) [Table 1]. There was significant correlation of QOL with psychiatric comorbidity, severity of psychiatric illness. In AA group, no statistically significant correlation was found with severity of illness but his was not true in psoriasis group [Table 2].
Table 1.
WHO-QOL scores
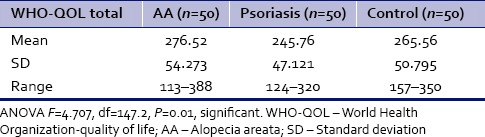
Table 2.
Correlation of QOL with psychiatric comorbidity and severity of skin condition
DISCUSSION
Depression was the major psychiatric comorbidity in our study. A study by Colón et al. in 31 AA patients by structured psychiatric interview showed prevalence of 74% psychiatric disorders with rates of depression and anxiety being 39% each.[11] Another comparative study done by Saleh et al. in 50 patients found psychiatric illness in 36% of AA patients, with anxiety in 24% and depression in 14% patients.[12] None of the patients in AA group had schizophrenia. One case series of 14 patients showed no association between AA and schizophrenia. Disturbances of dopaminergic neurotransmission are essential to pathophysiology of schizophrenia and glutamatergic hypofunction is important in dopamine dysfunction. Thus high levels of glutamate in anxiety and obsessive-compulsive disorder and hypo glutamate in schizophrenia might explain low rates of schizophrenia in AA group.[13]
However, in other studies on psoriasis patients with psychiatric morbidity, the percentages of patients with depression and anxiety on standardized psychiatric diagnosis were higher than those detected in our study (50–97% and 15–50% respectively).[14,15] Jowett and Ryan, 1985 found that 24% of psoriasis patients had depression and 58% suffered from anxiety.[16] A cross-sectional study on 103 psoriasis outpatients found 22.33% rate of psychiatric disorders.[17] The profile of psychiatric diagnosis was 65% adjustment disorder depressed type, 30% depressive episodes and 4% dysthymia. However, no anxiety disorders were detected in this study.
The difference in the prevalence of anxiety and depression in different studies could be due to difference in diagnostic systems used. In addition, different methodology such as patients’ recruitment and difference in population characters make the comparison between these studies difficult.
In our study we found that QOL was poorer in patients with psychiatric disorders compared to those not having it. Also the QOL had negative correlation with severity of psychiatric disorder in both groups. The QOL also had negative correlation with severity of psoriasis but in AA group QOL did not have statistically significant correlation with its severity. Sampogna et al. and Saleh et al. also found that QOL had correlation with severity of skin condition in both psoriasis and AA.[12,18] In contrast to our findings studies by Sampogna et al. and Hariram et al. have found weak correlation between severity of psoriasis and QOL.[19,20] This may be due to different sampling methods and different scales used to measure disease severity and QOL.
Many factors contributing to lower QOL in psoriasis include the chronic nature of the disease and the lack of control over unexpected outbreaks of the symptoms.[21] Patients may feel humiliated when they need to expose their bodies during swimming, intimate relationships, using public showers, or living in conditions that do not provide adequate privacy.[22] Psoriasis affects patients’ social life, daily activities, occupational, and sexual functioning.[23]
Our study had some limitations in form that it was cross-sectional in nature and also patients were not followed up to see the effects of treating psychiatric comorbidities whether it reduces skin condition's severity and improves QOL.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Devrimci-Ozguven H, Kundakci TN, Kumbasar H, Boyvat A. The depression, anxiety, life satisfaction and affective expression levels in psoriasis patients. J Eur Acad Dermatol Venereol. 2000;14:267–71. doi: 10.1046/j.1468-3083.2000.00085.x. [DOI] [PubMed] [Google Scholar]
- 2.Grahovac T, Ruzić K, Sepić-Grahovac D, Dadić-Hero E, Radonja AP. Depressive disorder and alopecia. Psychiatr Danub. 2010;22:293–5. [PubMed] [Google Scholar]
- 3.Ruiz-Doblado S, Carrizosa A, García-Hernández MJ. Alopecia areata: Psychiatric comorbidity and adjustment to illness. Int J Dermatol. 2003;42:434–7. doi: 10.1046/j.1365-4362.2003.01340.x. [DOI] [PubMed] [Google Scholar]
- 4.Koo JY, Shellow WV, Hallman CP, Edwards JE. Alopecia areata and increased prevalence of psychiatric disorders. Int J Dermatol. 1994;33:849–50. doi: 10.1111/j.1365-4362.1994.tb01018.x. [DOI] [PubMed] [Google Scholar]
- 5.Ghanizadeh A. Comorbidity of psychiatric disorders in children and adolescents with alopecia areata in a child and adolescent psychiatry clinical sample. Int J Dermatol. 2008;47:1118–20. doi: 10.1111/j.1365-4632.2008.03743.x. [DOI] [PubMed] [Google Scholar]
- 6.Gaikwad R, Deshpande S, Raje S, Dhamdhere DV, Ghate MR. Evaluation of functional impairment in psoriasis. Indian J Dermatol Venereol Leprol. 2006;72:37–40. doi: 10.4103/0378-6323.19716. [DOI] [PubMed] [Google Scholar]
- 7.Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in vitiligo and psoriasis: A comparative study from India. J Dermatol. 2001;28:424–32. doi: 10.1111/j.1346-8138.2001.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 8.Kumar V, Mattoo SK, Handa S. Psychiatric morbidity in pemphigus and psoriasis: A comparative study from India. Asian J Psychiatr. 2013;6:151–6. doi: 10.1016/j.ajp.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, et al. Alopecia areata investigational assessment guidelines – Part II. National Alopecia Areata Foundation. J Am Acad Dermatol. 2004;51:440–7. doi: 10.1016/j.jaad.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 10.Fredriksson T, Pettersson U. Severe psoriasis – Oral therapy with a new retinoid. Dermatologica. 1978;157:238–44. doi: 10.1159/000250839. [DOI] [PubMed] [Google Scholar]
- 11.Colón EA, Popkin MK, Callies AL, Dessert NJ, Hordinsky MK. Lifetime prevalence of psychiatric disorders in patients with alopecia areata. Compr Psychiatry. 1991;32:245–51. doi: 10.1016/0010-440x(91)90045-e. [DOI] [PubMed] [Google Scholar]
- 12.Saleh HM, Salem SA, El-Sheshetawy RS, El-Samei AM. Comparative study of psychiatric morbidity and quality of life in psoriasis, vitiligo and alopecia areata. Egypt Dermatol Online J. 2008;4:2. [Google Scholar]
- 13.Chu SY, Chen YJ, Tseng WC, Lin MW, Chen TJ, Hwang CY, et al. Psychiatric comorbidities in patients with alopecia areata in Taiwan: A case-control study. Br J Dermatol. 2012;166:525–31. doi: 10.1111/j.1365-2133.2011.10714.x. [DOI] [PubMed] [Google Scholar]
- 14.Mummer S, Tuba A, Yelda K, Hamdi O. Psychiatric morbidity in dermatology patients: Frequency and results of consultations. Indian J Dermatol. 2006;51:18–22. [Google Scholar]
- 15.Deshapande N, Desai N, Mundra VK. Psychiatric aspect of psoriasis. Arch Indian Psychiatry. 1998;4:61–4. [Google Scholar]
- 16.Jowett S, Ryan T. Skin disease and handicap: An analysis of the impact of skin conditions. Soc Sci Med. 1985;20:425–9. doi: 10.1016/0277-9536(85)90021-8. [DOI] [PubMed] [Google Scholar]
- 17.Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in psoriasis: Prevalence and correlates in India. German J Psychiatry. 2005;8:17–22. [Google Scholar]
- 18.Sampogna F, Picardi A, Chren MM, Melchi CF, Pasquini P, Masini C, et al. Association between poorer quality of life and psychiatric morbidity in patients with different dermatological conditions. Psychosom Med. 2004;66:620–4. doi: 10.1097/01.psy.0000132869.96872.b2. [DOI] [PubMed] [Google Scholar]
- 19.Sampogna F, Sera F, Abeni D. IDI Multipurpose Psoriasis Research on Vital Experiences (IMPROVE) Investigators. Measures of clinical severity, quality of life, and psychological distress in patients with psoriasis: A cluster analysis. J Invest Dermatol. 2004;122:602–7. doi: 10.1046/j.0022-202X.2003.09101.x. [DOI] [PubMed] [Google Scholar]
- 20.Hariram P, Mosam A, Aboobaker J, Esterhuizen T. Quality of life in psoriasis patients in KwaZulu Natal, South Africa. Indian J Dermatol Venereol Leprol. 2011;77:333–4. doi: 10.4103/0378-6323.79716. [DOI] [PubMed] [Google Scholar]
- 21.Gelfand JM, Feldman SR, Stern RS, Thomas J, Rolstad T, Margolis DJ. Determinants of quality of life in patients with psoriasis: A study from the US population. J Am Acad Dermatol. 2004;51:704–8. doi: 10.1016/j.jaad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Fortune DG, Richards HL, Griffiths CE. Psychologic factors in psoriasis: Consequences, mechanisms, and interventions. Dermatol Clin. 2005;23:681–94. doi: 10.1016/j.det.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel EJ. Quantifying the harmful effect of psoriasis on health-related quality of life. J Am Acad Dermatol. 2002;47:512–8. doi: 10.1067/mjd.2002.122755. [DOI] [PubMed] [Google Scholar]


