Abstract
Background:
A lot of stigma and misconceptions about pulmonary tuberculosis still persist, in spite of the advances in treatment. Thus, a mere diagnosis of pulmonary tuberculosis can be a psychological trauma to an individual. The situation has aggravated with the association of tuberculosis with HIV infection.
Aim:
To study the psychiatric morbidity due to the various psychological stresses faced by a patient of pulmonary tuberculosis.
Materials and Methods:
The study group consisted of 100 inpatients admitted to pulmonary ward with diagnosis of pulmonary tuberculosis. The control group consisted of 100 inpatients admitted to pulmonary ward with nontuberculous pulmonary diseases. Psychiatric history and mental status were recorded on a specially designed proforma and diagnosis of any psychiatric illness, if present, arrived at as per International Classification of Diseases (ICD-10). The psychiatric tests applied were beck's depression inventory (BDI) and Taylor's Manifest Anxiety Scale (TMAS).
Results:
Of the patients of pulmonary tuberculosis, 24% could be given a diagnostic category, as per ICD-10, as compared to only 8% of the controls (P < 0.005). On BDI, 44% of patients of pulmonary tuberculosis showed depression as compared to 27% of the controls (P < 0.02). On TMAS, 38% of patients of pulmonary tuberculosis showed anxiety as compared to 24% of controls (P < 0.05). A greater incidence of depression (on BDI) and anxiety (on TMAS) was seen in those with longer duration of illness (P < 0.02) and in those with greater severity of illness (P < 0.02).
Conclusion:
In view of the high psychiatric morbidity associated with pulmonary tuberculosis, there is enough scope for psychiatric services to be made available to these patients. In addition, personnel involved in the treatment of these patients should be trained for early detection of psychiatric symptoms.
Keywords: Anxiety, depression, psychiatric morbidity, pulmonary tuberculosis
The diagnosis of pulmonary tuberculosis has been a cause of lot of fear and anxiety since thousands of years, because of the lack of any effective treatment and the high morbidity and mortality associated with it. Subsequently, the advent of chemotherapy markedly reduced the morbidity and mortality. Unfortunately, in spite of the advances in treatment, the misconceptions about tuberculosis still persist. Even now tuberculosis is thought to be an incurable disease, and a lot of stigma is associated with it. A mere diagnosis of tuberculosis can be a psychological trauma for a person, giving rise to varied psychiatric symptoms.
A high incidence of depression and anxiety has been found in pulmonary tuberculosis patients.[1,2,3,4] de Araújo et al.[5] found a positive and independent association between common mental disorders and tuberculosis.
Since 1985, a resurgence of tuberculosis has been observed in persons who are HIV positive.[6,7] In addition, tuberculosis and HIV co-infected individuals have a much higher risk of having common mental disorders.[8]
As mentioned above psychiatric symptoms in pulmonary tuberculosis patients can arise due to the various psychological stress faced by the patient. In addition, they can also be due to the various organic brain syndromes (central nervous system [CNS] tuberculosis and side effects of anti-tubercular drugs). Though much work has been done on the latter; there is paucity of recent work on the psychological problems caused by the various psychosocial stresses faced by the patient. These psychological problems often remain undiagnosed and untreated with adverse consequences on the prognosis of pulmonary tuberculosis as it has been found that psychiatric co-morbidity leads to poor compliance to anti-tuberculous therapy.[9,10]
In view of the above, this study was undertaken to find out the psychiatric morbidity due to the various psychological stress faced by a patient by a patient of pulmonary tuberculosis.
MATERIALS AND METHODS
The study was carried out in the Department of Pulmonary medicine and Psychiatry, in a tertiary care teaching hospital, during 1 year from July 2014 to June 2015. The study group consisted of 100 inpatients admitted to a pulmonary ward with diagnosis of pulmonary tuberculosis.
Selection criteria
Patients without any evidence of CNS involvement
Patients with no other major physical illness except pulmonary tuberculosis
Patients with no past history of psychiatric illness, including psychosomatic illness, and personality disorder
Patients were not on anti-tubercular drugs or any other regular medication
Only male patients could be included in the study, as due to administrative reasons, the hospital during the period of study was admitting only male patients for domiciliary treatment of tuberculosis.
The control group consisted of 100 inpatients admitted to pulmonary ward with nontuberculous pulmonary disease such as chronic bronchitis, emphysema or bronchiectasis. The study group and the controls where matched as nearly as possible for age, educational status, domicile, and duration of illness.
Each patient was interviewed separately. Detailed medical history was taken from the patient. Detailed physical examination was done to rule out CNS involvement. Psychiatric history and mental status were recorded on a specially designed proforma and diagnosis of any psychiatric illness, if present, arrived at as per International Classification of Diseases (ICD-10).
The following psychiatric tests were administered
Taylor's manifest anxiety scale
The Taylor manifest anxiety scale (TMAS)[11] is used as a measure of anxiety as a general personality trait. The test has been widely studied and used in research. The test consists of fifty statements as true or false and takes 4–10 min to complete. Higher score represents a higher level of anxiety. Test-retest correlations of 0.89, 0.82, and 0.81 were seen over intervals of 3 weeks, 5 months and nine to 17 months.
Beck's depression inventory
The beck depression inventory (BDI)[12] is a 21-item; self-report rating inventory that measures characteristic attitudes and symptoms of depression. The BDI takes approximately 10 min to complete. Internal consistency for the BDI ranges from 0.73 to 0.92 with a mean of 0.86. The BDI demonstrates high internal consistency, with alpha coefficients of. 86 and. 81 for psychiatric and nonpsychiatric populations, respectively).
For studying the relationship of severity of illness with the psychiatric morbidity, cases of pulmonary tuberculosis were divided into three categories according to the extent of X-ray lesions, as per the criteria proposed by American Thoracic Society.[13]
Minimal: Lesions of slight to moderate density but which do not contain demonstrable cavitations
Moderately advanced: Lesions may be present in one or both lungs, but the total extent does not exceed one-third the volume of one lung. Cavitations, if present must be <4 cm
Far advanced: Lesions more extensive than moderately advanced.
RESULTS
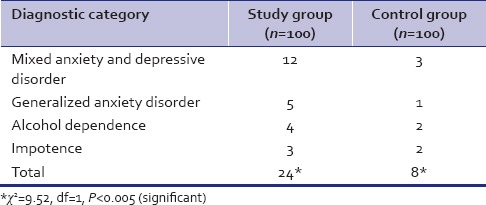
Age distribution, educational status, domicile, and duration of illness of both the study and control group are as brought out in Table 1. Both study and control group are comparable. Around one fourth of the patients of pulmonary tuberculosis could be given a diagnostic category as per ICD-10, which is higher than that of the controls. The difference is statistically significant (P < 0.005) [Table 2]. Table 2 further shows that the majority of the patient with psychiatric illness had mixed anxiety and depressive disorder followed by generalized anxiety disorder, alcohol dependence syndrome and impotence.
Table 1.
Sociodemographic characteristics of the sample
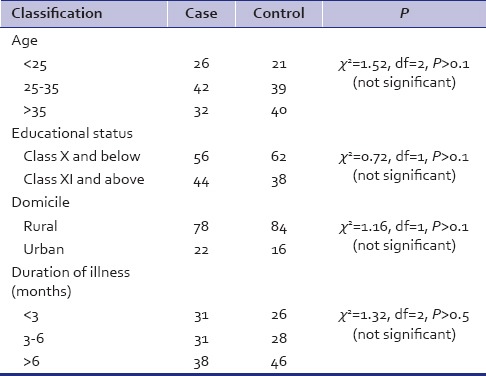
Table 2.
Number of patients who could be given a diagnostic category (as per International classification of diseases-10) on clinical psychiatric examination
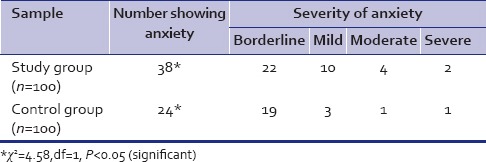
More number of patients of pulmonary tuberculosis showed depression on BDI, as compared to that of controls. The difference was significant statistically (P < 0.02) [Table 3]. Similarly, patients with pulmonary tuberculosis showed higher anxiety on TMAS, as compared to that of controls [Table 4].
Table 3.
Result of Beck's depression inventory
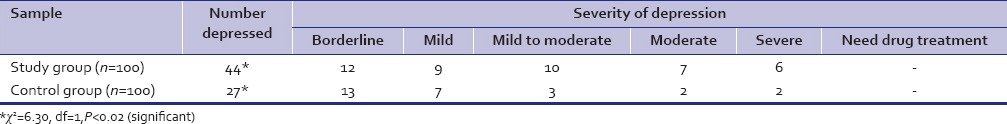
Table 4.
Result of Taylor's Manifest Anxiety Scale
On BDI, 48.2% of patients who were educated up to X class or less showed depression as compared to 38.6% of those who were more educated. The difference is not statistically significant (P > 0.1). On TMAS, 42.8% of those educated up to X class or less showed anxiety as compared to 31.8% of those who were more educated. This difference is also not statistically significant (P > 0.1).
On BDI, depression was observed in 25.8% of those with illness of <3 months duration. 38.7% of those with illness of 3–6 months duration and 63.1% of those with illness of more than 6 months duration. The difference is statistically significant (P < 0.01). Anxiety was observed in 22.5% of those with illness of <3 months and 55.2% of those with illness of more than 6 months duration. The difference is also statistically significant (P < 0.02).
On BDI, depression was observed in 27.2% of those with minimal X-ray lesions, 36.6% of those with moderately advanced lesions and 56.2% of those with far advanced lesions. The difference is statistically significant (P < 0.05). Anxiety was observed in 22.7% of those with minimal X-ray lesions, 26.6% of those with moderately advanced lesions and 52% of those with far advanced lesions. The difference is also statistically significant (P < 0.02).
DISCUSSION
The psychological aspects of tuberculosis have always been a topic of interest over the centuries. Our study shows that depression and anxiety disorders were the commonest illness found in patients of pulmonary tuberculosis. These findings are comparable with some of the earlier works.[1,2,3,4] The high incidence of depression and anxiety found in patients of pulmonary tuberculosis could be due to the various psychosocial stresses faced by the patient like social stigma attached to the illness, set back in occupation, social isolation with damaged status, lowered self-esteem, fear of spreading the illness to others and helplessness brought about by incapacitation due to chronic illness.
It can be seen that no patient had a breakdown of psychotic nature in our study. This finding is also in agreement with that of Mathai et al.[1] They detected a breakdown of psychotic nature (Schizophrenia) in only 1 of the 70 patients of pulmonary tuberculosis they studied. The one schizophrenic that they detected had contracted tuberculosis during his admission in the mental hospital and had been shifted to the chest hospital. However, Srivastava et al.[4] found brief psychotic disorder in 6% of their patients. Yadav et al.[14] found paranoid reaction in 4 out of 80 patients in their study.
In our study, a greater incidence of depression and anxiety was seen in these with longer duration of illness. A similar observation has been reported by Srivastava et al.[4] and Natani et al.[15] This positive correlation might be due to the longer period of suffering, social isolation, and strain on the financial resources.
The high occurrence of depression and anxiety seen in our study in those with greater severity of illness has been observed in several previous studies also.[1,2,15]
There appears to be a complex interplay of duration and severity of illness and psychological factors in causing the depression and anxiety in patients of pulmonary tuberculosis.
The study was a cross-sectional one and has limitation to the interpretation of its finding. A longitudinal perspective would have reflected more on the causal relation or the strength of association. A multi-centric study would have led to wider generalization of findings and thus preferred.
CONCLUSION
Tuberculosis is a disease of both individual and society. A lot of fear and misconception is still prevalent about pulmonary tuberculosis, leading to a high incidence of psychiatric morbidity. It has been seen that psychiatric illness can lead to poor drug compliance, resulting in drug resistance and increased morbidity and mortality due to pulmonary tuberculosis.
In view of the above, there is enough scope for psychiatric services to be made available to these patients. In addition, chest physicians and nursing staff involved in the care of these patients should be trained for early detection of any psychiatric symptoms in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mathai PJ, Ravindran P, Joshi P, Sundaram P. Psychiatric morbidity in pulmonary tuberculosis-a clinical study. Indian J Psychiatry. 1981;23:66–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, Kamiya Y. Prevalence and associated factors of depressive state among pulmonary tuberculosis patients in Manila, The Philippines. Int J Tuberc Lung Dis. 2014;18:174–9. doi: 10.5588/ijtld.13.0335. [DOI] [PubMed] [Google Scholar]
- 3.Chandrashekar TR, Denzil P, Rajendrkumar K, Shantha AR, Bhagyashri RH, Joshi AV. A study of psychiatric morbidity among patients suffering from pulmonary tuberculosis. Med Leg Update. 2012;12:26–9. [Google Scholar]
- 4.Srivastava AS, Ramdinee NA, Matah SC, Tripathi MN, Pandit B, Yadav JS. Psychiatric morbidities in patients with pulmonary tuberculosis. Dysphrenia. 2014;5:133–7. [Google Scholar]
- 5.de Araújo GS, Pereira SM, dos Santos DN, Marinho JM, Rodrigues LC, Barreto ML. Common mental disorders associated with tuberculosis: A matched case-control study. PLoS One. 2014;9:e99551. doi: 10.1371/journal.pone.0099551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamholz SL. Resurgence of tuberculosis: The perspective a dozen years later. J Assoc Acad Minor Phys. 1996;7:83–6. [PubMed] [Google Scholar]
- 7.Pedersen C, Kolmos HJ, Nielsen JO. Tuberculosis and the HIV pandemic. Risk of nosocomial tuberculosis infection. Ugeskr Laeger. 1997;159:1233–8. [PubMed] [Google Scholar]
- 8.Deribew A, Tesfaye M, Hailmichael Y, Apers L, Abebe G, Duchateau L, et al. Common mental disorders in TB/HIV co-infected patients in Ethiopia. BMC Infect Dis. 2010;10:201. doi: 10.1186/1471-2334-10-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pachi A, Bratis D, Moussas G, Tselebis A. Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013. 2013:489865. doi: 10.1155/2013/489865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 11.Taylor JA. A personality scale of manifest anxiety. J Abnorm Soc Psychol. 1953;48:285–90. doi: 10.1037/h0056264. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 13.Hinshaw CA. 3rd ed. Philadelphia, London: WB Saunders Coy; 1969. Disease of the chest; pp. 542–4. [Google Scholar]
- 14.Yadav BS, Jain SC, Sharma G, Mehrotra ML, Kumar A. Psychiatric morbidity in pulmonary tuberculosis. Indian J Tuberc. 1980;27:167–71. [Google Scholar]
- 15.Natani GD, Jain NK, Sharma TN, Gehlot PS, Agrawal SP, Koolwal S, et al. Depression in tuberculosis patients: Correlation with duration of disease and response to anti-tuberculous chemotherapy. Indian J Tuberc. 1985;32:195–8. [Google Scholar]


