Abstract
Introduction:
The high prevalence, severity, and prematurity of coronary artery disease (CAD) in the Indian population cannot be completely explained by the conventional lipid parameters and the existing lipid indices.
Aims and Objectives:
To calculate newly defined advanced atherogenic index (AAI) in premature CAD patients and compare it between cases and controls and Correlate its values with the existing indices.
Material and Methods:
One hundred and twenty premature CAD patients and an equal number of age and sex matched healthy individuals were included in this study. Lipid profile and nonconventional lipid parameters like oxidized Low density lipoprotein (OX LDL), small dense LDL (SD LDL), lipoprotein (a) apolipoprotein B (Apo B), and apolipoprotein A1 (Apo A1) were estimated and their values were used to define AAI and existing lipid indices like AI, lipid tetrad index (LTI) and lipid pentad index (LPI).
Results:
The mean age of cases and controls was 37.29 + 4.50 and 36.13 + 3.53 years, respectively. The value of AAI was highly significant in cases (3461.22 ± 45.20) as compared to controls (305.84 ± 21.80). AAI has shown better statistical significance and correlation (P < 0.0001, r = 0.737) as compared to the earlier indices such as AI (P < 0.01, r = 0.52), LTI (P < 0.001, r = 0.677) and LPI (P < 0.001, r = 0.622) in premature CAD. Kolmogorov D statistic and cumulative distribution function plot has shown that AAI can discriminate cases and controls more accurately as compared to the earlier indices.
Conclusion:
Statistically AAI appears to be a better marker of consolidated lipid risk in premature CAD patients as compared to the earlier indices.
Keywords: Advanced atherogenic index, lipid pentad index, lipid tetrad index, premature coronary artery disease
INTRODUCTION
Premature coronary artery disease (CAD) is the occurrence of cardiac events at a younger age (before the age 45 years in men and before the age of 55 years in women).[1] In its severe form premature CAD occurs below the age of 40 years.
The incidence and prevalence of CAD in India is very high and currently India is having a maximum number of CAD patients in the world putting India in the state of a CAD epidemic.[2] High degree of mortality, morbidity, and prematurity of CAD has put a great burden on the society and health care expenditure, and it is the most common cause of death worldwide.[3] The higher degree of prematurity and the severity of CAD in the Indian population as compared to any other ethnic group[4] in the world can only be partially explained on the basis of conventional lipid parameters. Partial explanation is based on the fact that the Indians generally tend to have a higher level of Low density lipoprotein (LDL)-C and lower level of high-density lipoprotein (HDL)-C[5,6,7] as compared to their western counterparts. Dyslipidemia is one of the most common risk factors for the development of atherosclerosis, and the increased values of the conventional lipid parameters are associated with increased risk of CAD. Although many studies have shown a strong correlation between dyslipidemia and CAD, but it does not explain the high prevalence and severity of CAD completely in all the cases. It has been found in many studies that CAD occurs even in the patients who have normal levels of LDL and HDL. Therefore, researchers have defined many indices such as AI, lipid tetrad index (LTI), and lipid pentad index (LPI) on the basis of the values of the conventional lipid parameters for assessing consolidated lipid risk factor in CAD. Although these existing indices are better than the individual lipid parameters, the values of these indices are many times high even in normal persons free from CAD. Moreover, the occurrence of CAD in normolipidemic persons gives the insight to look beyond the conventional lipid profile and researchers have been trying to elucidate the possibility of other parameters that must be statistically better predictors in the pathogenesis of atherosclerosis which is the underlying pathology of CAD. Hence, in our study, we have estimated nonconventional lipid parameters such as oxidized (OX LDL), small dense (SD LDL), apolipoprotein A1 (Apo A1), lipoprotein (a), and apolipoprotein B (Apo B) and used these parameters for the calculation of advanced atherogenic index (AAI).
Then we compared the values of AAI with that of the existing lipid indices that have already defined as an assessment of consolidated lipid risk factor in CAD. LTI was given by Enas,[8,9] and it explains the risk of dyslipidemia in CAD in the Indian population. LTI includes triglyceride (TC), total cholesterol (TG), lipoprotein (a) and HDL-C. LPI was given by Das et al.[10] for assessment of risk factors in the children of premature CAD patients includes TC, TG, Apo B, lipoprotein (a), and Apo A1. Although LPI have shown better discrimination between cases and controls but this index was actually calculated in the children of CAD patients rather than the patients themselves, and limited data are available in India, which has evaluated this index in CAD patients. Most importantly, none of the above indices included the more important lipid parameters such as OX LDL and SD LDL which are better markers of CAD as proved by many studies.[11,12]
The significance to include SD LDL instead of LDL lies in the fact that LDL is not homogenous in size and shape and on differential centrifugation it is divided into two fractions.[13] One fraction is small and dense, and the other one is large and buoyant. Persons usually have a combination of the two fractions. Studies have shown that higher proportion of SD LDL in an individual is associated with higher risk of occurrence of CAD because it has a higher tendency to get OX and OX LDL, in turn, is actually deposited inside the macrophages to form the foam cells.[14] Normal LDL deposited inside macrophages can be taken back by reverse transport cholesterol (RCT) by HDL, but once it is converted to OX LDL, then it down-regulates the scavenger receptors on the macrophages and decreases the extent of RCT because Apo A1 of HDL acts on these receptors.[15,16] Hence, higher amount of SD LDL will lead to the formation of increased amount of OX LDL. Studies have shown a strong correlation between the values of SD LDL and severity of CAD.[12,17,18,19] Therefore, the levels of SD LDL and OX LDL assumes greater importance as the lipid risk factors for the development of atherosclerosis. The increased values of SD LDL and OX LDL can explain the occurrence of CAD in patients with normal levels of LDL as many studies have shown the occurrence of CAD even in normolipidemic patients having a normal or subnormal level of LDL.[20,21] Therefore, lipid index which will include these parameters may prove to be a better predictor of consolidated lipid risk in CAD. This led us to calculate a new AAI from the values of the nonconventional lipid risk factors such as SD LDL, OX LDL, Apo A1, Apo B, and lipoprotein (a). Another importance of this index is that all the parameters used in its calculation are genetically determined and can explain the prematurity and severity of CAD in Indian population. Then we used various statistical methods to compare the AAI the existing indices such as AI, LTI, and LPI to check whether it offers any advantage in predicting the consolidated lipid risk in CAD.
MATERIALS AND METHODS
After taking prior ethical clearance from the ethical committee of the Institute, this study was conducted in a tertiary care multispecialty hospital in New Delhi. Our study included two hundred and forty subjects divided into two equal groups (cases and controls).
One hundred and twenty patients suffering from premature CAD (males of the age <45 years and females of the age <55 years)[1] admitted to the coronary care unit of a tertiary care hospital, were taken as the cases for this study. The diagnosis was based on detailed history, clinical examination, electrocardiography changes, angiography, increased cardiac enzymes (Troponin T, CK-MB fraction), and echocardiography. One hundred and twenty age and gender matched (males below the age of 45 years and females below the age of 55 years)[1] healthy individuals from the general population who were free from CAD based on clinical history or detailed examination constituted the control group. Patients having a history of smoking, chronic alcoholism, concomitant liver, or kidney disease and acute or chronic infection were excluded. Patients taking hypolipidemic drugs, oral contraceptives, or hormone replacement therapy were also excluded from this study.
Informed and written consent was taken from all the subjects (cases and controls) after explaining the details and the utility of this study. A detailed history of all the subjects admitted with premature CAD was taken, and clinical examination was performed. Details of laboratory investigations were noted for all the subjects.
Collection of blood samples
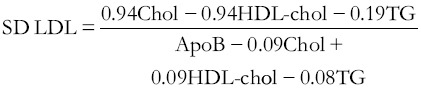
Because fasting samples are needed for the estimation of various lipid parameters, hence after taking advice from the attending cardio physician, the willing patients were asked for an overnight fasting for 10–14 h a day before taking samples. The fasting samples were taken the next morning taking all aseptic precautions from an antecubital vein. The blood was centrifuged for 10 min and separated serum was collected in different aliquots for the estimation of routine lipid profile, OX LDL, Apo A1, lipoprotein (a), SD LDL, and Apo B (Apo B-100). Lipid profile was estimated on fully automated Biochemistry analyzer “Olympus-AU 400” TC was estimated by enzymatic end-point cholesterol esterase-peroxidase method (Accurex Biomedical Pvt. Limited, Mumbai). TCs were estimated by enzymatic end-point glycerol phosphate oxidase-peroxidase method (Accurex Biomedical Pvt Limited, Mumbai). HDL-C was estimated by direct Assay based on precipitation method where selective precipitation of LDL, very LDL (VLDL) and TG occurs, and only HDL is measured enzymatically by cholesterol oxidase and cholesterol esterase followed by Trinder reaction. LDL-C was estimated by direct Assay based on precipitation method where LDL, VLDL, and chylomicrons react with precipitating reagents and selected detergents which prevent these to react with cholesterol oxidase and cholesterol esterase, whereas HDL reacts. Further addition of specific detergent releases LDL from the precipitated complex which is now measured enzymatically followed by trinder reactionon. OX LDL was estimated by ELISA Kit (Mercodia, Sweden) which is based on the direct sandwich technique in which two monoclonal antibodies are directed against separate antigenic determinants on the OX Apo B molecule. Lipoprotein (a) was estimated by ELISA Kit (immunozym, Progen Biotechnik GMBH, Germany) which is based on a one-step sandwich ELISA using specific monovalent anti-apo (a) antibodies. Apo A1 and Apo B were measured by using immunoassay based immunoturbidimetric kit (Diasys) on fully automated “Olympus AU 400” auto analyzer. SD LDL was calculated indirectly by using the formula given by Hattori et al.[22]
AI was defined by Dobiášová and Frohlich[23,24] by using the formula: AI = (Log [TG/HDL-C]). LTI, which was given by Enas et al.,[25] was calculated by the formula: LTI = TC × TG × lipoprotein (a) ÷ HDL-C. LPI was calculated by the formula:[10] LPI = TC × TG × lipoprotein (a) × Apo B ÷ Apo A-1. We defined a new AAI for the estimation of consolidated lipid risk in premature CAD patients in India. The formula for the calculation of this index is based on the earlier indices in which the parameters which correlate directly with CAD is taken as the numerator and those which correlate indirectly are taken as the denominator. But this index includes SD LDL and OX LDL in addition to Apo B, Apo A1, and Lipoprotein (a). The formula used for calculating AAI is as follows: AAI = {OX LDL × lipoprotein (a) × Apo B} ÷ (Apo A1 × SD LDL)
Statistical analysis
The statistical analysis was performed by using SPSS version 17.0 by SPSS inc., Chicago, USA. Continuous variables were expressed as mean ± standard deviation and discrete variables were expressed as a percentage. A t-test was applied to lognormal values of lipoprotein (a), TG and Apo B as they followed lognormal distribution as proved by probability plots while t-test was applied directly to the rest of the lipid values because they followed normal distribution. F-test was applied to paired data in the cases and controls to determine the significance of variance.
The comparison of data in the two groups was done by nonparametric Mann–Whitney U-test. Significance was calculated using Kruskal–Wallis test. Differences were considered to be significant if the P < 0.05. Spearman's rank correlation (which theoretically lies between − 1 and + 1) was used to calculate the correlation between different parameters. Cumulative distribution function (CDF) plots were used to check how far AAI can discriminate between case and controls. Kolmogorov–Sminrov D statistics was applied to various lipid indices to check their ability to discriminate cases from controls. Histogram was used to assess the frequency of patients in a different range of the AAI.
RESULTS
Table 1 shows age and gender distribution in the subjects. The number of males was more than that of females (Male:Female ratio 2.15) suggesting a higher prevalence of premature CAD in the males as compared to the females. As shown in Table 2, a maximum number of patients in our study were in the age of 36–45 years (80 out of 120, 66.67%). Figures 1 and 2 show that 24 out of 38 female patients were in the age group of 46–55 years, which explains that with increasing age, chances of ischemic heart disease also increase in the females.
Table 1.
Age and gender distribution in the subjects
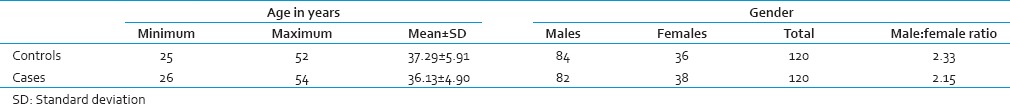
Table 2.
Lipid parameters in cases and controls
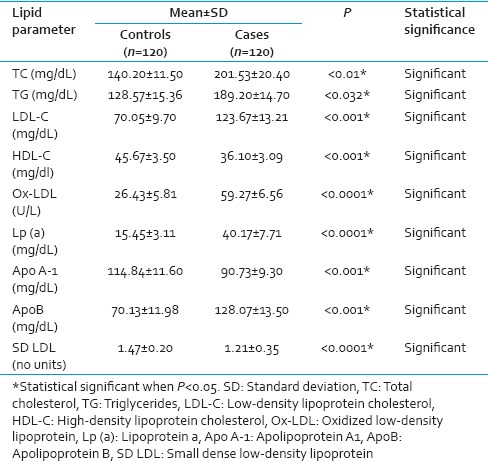
Figure 1.
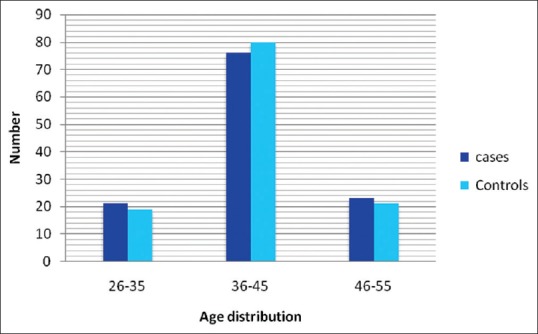
Age distribution in cases and controls
Figure 2.
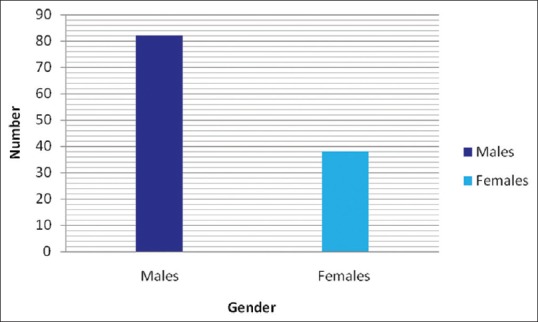
Gender distribution in cases
According to the Table 2, the values of TC (P < 0.01), TG (P < 0.032), LDL (P < 0.001), OX LDL (P < 0.0001), Lipoprotein (a) (P < 0.0001), and Apo B (P < 0.001) were significantly higher while HDL (P < 0.01), SD LDL (P < 0.0001), and Apo A1 (P < 0.001) were significantly lower in the cases as compared to the controls.
As shown in Table 3, the values of AI, LTI, LPI, and AAI were significantly high in cases as compared to controls. Out of the all indices newly defined AAI showed maximum correlation
Table 3.
Comparisons of lipid tetrad index, lipid pentad index and advanced atherogenic index in cases and controls
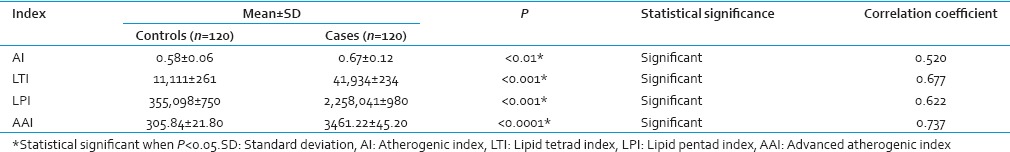
(P < 0.0001, r = 0.737) with the disease as compared to AI (P < 0.01, r = 0.520), LTI (P < 0.001, r = 0.677) and LPI (P < 0.001, r = 0.622).
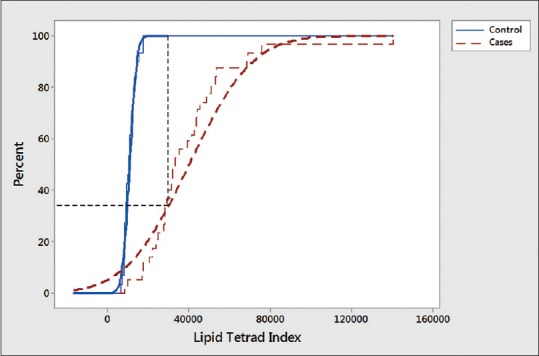
According to CDF plots, the chances of wrongly classifying the cases as controls were 78%, 38%, and 23% in AI, LTI, and LPI, respectively [Figures 3–5]. The percentage of cases which can be wrongly classified as controls by AAI was only 17%. Therefore, it is evident from CDF plots, that if AAI is used as a consolidated lipid risk marker in CAD than chances of wrongly classifying patients as normal is minimum. Then we applied Kolmogorov statistic to find the D value which a measure of the extent to which cases can be discriminated from controls. Kolmogorov statistic was highly significant in AAI and LPI (<0.00001) and significant in LTI (<0.001) and AI (P < 0.01). D value for AAI was higher (0.84) as compared to D values of LPI (0.72), LTI (0.64) and AI (0.51). Higher D value of AAI implies that it can discriminate between cases and controls better than other indices. As shown by dotted lines in the CDF plots of various indices, AAI shows the maximum vertical deviation between the curves of cases and controls [Figure 6]. The more the vertical separation between the curves higher is power to discriminate between the cases and the controls. Hence, the order of discriminating power of various indices is AAI > LPI > LTI > AI.
Figure 3.
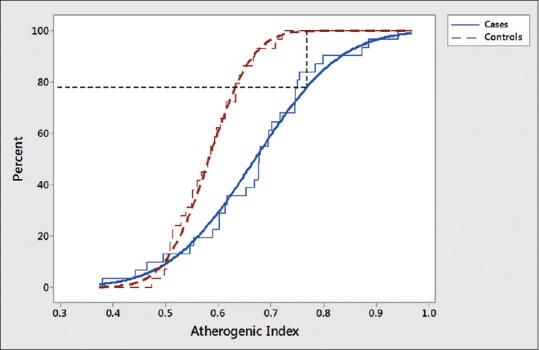
Cumulative distribution function plots of atherogenic index in cases and controls (staircase curves show empirical cumulative distribution function from the observed data and smooth curves are lognormal cumulative distribution function fit of the observed data)
Figure 5.
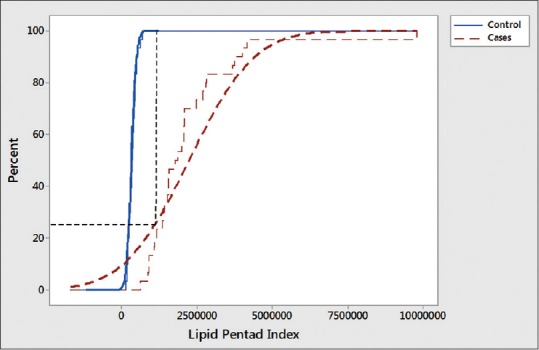
Cumulative distribution function plots of lipid pentad index in cases and controls (staircase curves show empirical cumulative distribution function from the observed data and Smooth curves are lognormal cumulative distribution function fit of the observed data)
Figure 6.
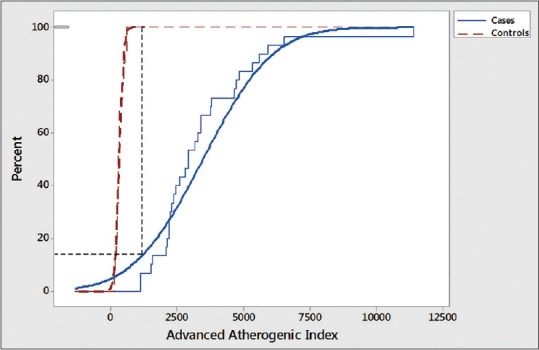
Cumulative distribution function plots of advanced atherogenic index in cases and controls (staircase curves show empirical cumulative distribution function from the observed data and smooth curves are lognormal cumulative distribution function fit of the observed data)
Figure 4.
Cumulative distribution function plots of lipid tetrad index in cases and controls (staircase curves show empirical cumulative distribution function from the observed data and smooth curves are lognormal cumulative distribution function fit of the observed data)
Histogram of AAI with the corresponding lognormal fit curve shows that the number of patients in a different range of values of this index [Figures 7 and 8]. The value of AAI is >7500 in 74/120 patients and only 23/120 controls which further support the importance of this index for better discrimination between cases and controls groups [Figure 9].
Figure 7.
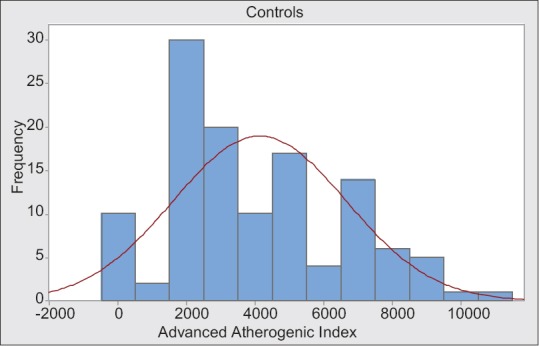
Histogram of advanced atherogenic index with lognormal fitcurve in controls
Figure 8.
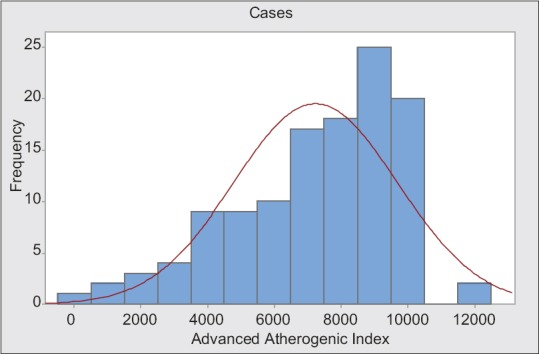
Histogram of advanced atherogenic index with lognormal fit curve in cases
Figure 9.
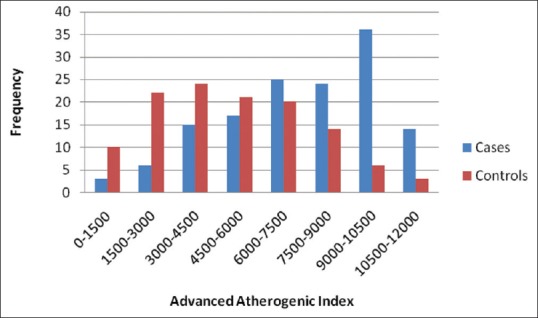
Histogram of advanced atherogenic index in cases and controls
DISCUSSION
Dyslipidemia is very important lipid risk factor in the pathogenesis of CAD. Abnormal lipid parameters have been used for many years as the risk factors for CAD. Many studies have been done and proved the importance of the conventional lipid parameters, i.e., TC, LDL, HDL, and TG in the pathogenesis of atherosclerosis which is a basic pathology in CAD. But in many cases, the conventional lipid parameters fail to explain the higher occurrence or severity of CAD in Indian population which emphasize that other lipid parameters are involved in the pathogenesis of CAD. Recent studies have shown that the advanced lipid parameters such as OX LDL, SD LDL Apo A1, and Apo B, a lipoprotein (a), are better discriminator of CAD and can explain higher incidence and prevalence of CAD in the Indian population and has shown better correlation with the severity of CAD as compared to conventional lipid parameters[21,26,27,28] an existing lipid indices.
For determination of consolidated lipid risk factor, few indices have already been given and include AI, LTI, and LPI. AI was given by Dobiásová et al. and calculated by taking the logarithm of the ratio of TG to HDL-C.[23] The values of AI were higher in patients with CAD as compared to the controls. However, this index has the limitation because it includes only two lipid parameters. This index does not include LDL, which is a more important risk factor for CAD.
LTI was given by Enas et al.[25] for the assessment of cardiovascular risk. LTI is calculated by multiplying atherogenic particles, i.e., TC, TG, and lipoprotein (a) and dividing it by HDL which is antiatherogenic. This index gives consolidated lipid risk factor in CAD. In our study, LTI values were significantly higher in patients of CAD as compared to controls as compared to the healthy persons (P < 0.001).
A study by Morais et al.[29] showed a positive correlation between LTI and LDL which is important risk factor for the pathogenesis of CAD but LDL is not included in the calculation of this index.
LPI was given by Das et al.[10] and is calculated by the product of TC, TG, lipoprotein (a), and Apo B divided by Apo A1. However, LPI was given in the children of the premature CAD patients in India. Only a few studies are available to the best of our knowledge, which have evaluated LPI and LTI in healthy individuals.[29] Although LPI values were higher in children of premature CAD patients as compared to the children of normal healthy individuals but to the best of our knowledge, LPI is not tested in the premature CAD patients for the assessment of lipid risk factors. In this study, we have compared this index in cases and of premature CAD with the healthy individuals.
Although LTI and LPI have shown higher values in CAD patients, these indices do not include OX LDL and SD LDL. OX LDL and SD LDL are metabolically better indicators of dyslipidemia and have emerged out to be the recent putative markers implicated in CAD. Any index which will incorporate these all important lipid parameters may prove to be a better marker in the assessment of consolidated lipid risk in the CAD. Therefore, in this study we have defined AAI which is calculated by multiplying OX LDL, lipoprotein (a) and Apo B and dividing it by Apo A1 and SD LDL. Surprisingly, the value of AAI was significantly high (P < 0.0001) in patients of premature CAD patients as compared to the normal individuals. Moreover, AAI has shown strong correlation with premature CAD and its correlation coefficient (r = 0.737) was higher as compared to AI (r = 0.520), LTI (r = 0.677) and LPI (r = 0.622). Thus according to our study AAI seems to have better discriminating power (D value 0.84) between cases of premature CAD from controls. Moreover, OX LDL, SD LDL, lipoprotein (a), Apo B, and Apo A1 are genetically determined and are included in the AAI. Hence, this index can explain higher incidence, severity, and prematurity of CAD in the Indian population. AAI may prove to be an important screening test for early detection and intervention in CAD patients in the Indian population.
However, its importance as marker of dyslipidemia in premature CAD patients has to be further explored in larger groups before it can actually be used clinically. Despite the limitation of sample size, our study does prove that this new AAI is a statistically better index as compared to previously known indices, i.e., AI, LTI, and LPI.
CONCLUSION
The values of AAI which is calculated from various lipid parameters including the important SD LDL and OX LDL were significantly higher in premature CAD patients in Indian population as compared to the age and gender matched controls (P < 0.001). AAI showed maximum correlation with the disease (r = 0.737) as compared to AI (0.520), LTI (r = 0.677) and LPI (r = 0.622). Statistically, it appears that AAI has better discriminating value in CAD patients as compared to earlier indices. Because parameters included in this index are genetically determined, it may also explain the higher degree of prevalence and prematurity of CAD in Indian population. However, this index has to further explore, by taking bigger sample size before it can be used clinically.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Farmer JA, Gotto AN. Dyslipidemia and other risk factors for coronary artery disease. In: Braunwald E, editor. Braunwald's Heart Disease. A Text Book of Cardiovascular Disease. Vol. 5. Philadelphia: WB Saunders and Co; 1997. pp. 1126–60. [Google Scholar]
- 2.Krishnan MN. Coronary heart disease and risk factors in India – On the brink of an epidemic? Indian Heart J. 2012;64:364–7. doi: 10.1016/j.ihj.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sekhri T, Kanwar RS, Wilfred R, Chugh P, Chhillar M, Aggarwal R, et al. Prevalence of risk factors for coronary artery disease in an urban Indian population. BMJ Open. 2014;4:e005346. doi: 10.1136/bmjopen-2014-005346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah B, Mathur P. Surveillance of cardiovascular disease risk factors in India: The need and scope. Indian J Med Res. 2010;132:634–42. doi: 10.4103/0971-5916.73420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enas EA. Coronary artery disease epidemic in Indians: A cause for alarm and call for action. J Indian Med Assoc. 2000;98:694. [PubMed] [Google Scholar]
- 6.Guptha S, Gupta R, Deedwania P, Bhansali A, Maheshwari A, Gupta A, et al. Cholesterol lipoproteins and prevalence of dyslipidemias in urban Asian Indians: A cross sectional study. Indian Heart J. 2014;66:280–8. doi: 10.1016/j.ihj.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emerging Risk Factors Collaboration. Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enas EA, Dhawan J, Petkar S. Coronary artery disease in Asian Indians: Lessons learnt and the role of lipoprotein (a) Indian Heart J. 1997;49:25–34. [PubMed] [Google Scholar]
- 9.Rajappa M, Sridhar MG, Balachander J, Sethuraman KR. Lipoprotein (a) and comprehensive lipid tetrad index as a marker for coronary artery disease in NIDDM patients in South India. Clin Chim Acta. 2006;372:70–5. doi: 10.1016/j.cca.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 10.Das B, Daga MK, Gupta SK. Lipid Pentad Index: A novel bioindex for evaluation of lipid risk factors for atherosclerosis in young adolescents and children of premature coronary artery disease patients in India. Clin Biochem. 2007;40:18–24. doi: 10.1016/j.clinbiochem.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Moon JY, Kwon HM, Kwon SW, Yoon SJ, Kim JS, Lee SJ, et al. Lipoprotein (a) and LDL particle size are related to the severity of coronary artery disease. Cardiology. 2007;108:282–9. doi: 10.1159/000099097. [DOI] [PubMed] [Google Scholar]
- 12.Meisinger C, Baumert J, Khuseyinova N, Loewel H, Koenig W. Plasma oxidized low-density lipoprotein, a strong predictor for acute coronary heart disease events in apparently healthy, middle-aged men from the general population. Circulation. 2005;112:651–7. doi: 10.1161/CIRCULATIONAHA.104.529297. [DOI] [PubMed] [Google Scholar]
- 13.Mora S, Szklo M, Otvos JD, Greenland P, Psaty BM, Goff DC, Jr, et al. LDL particle subclasses, LDL particle size, and carotid atherosclerosis in the Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2007;192:211–7. doi: 10.1016/j.atherosclerosis.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Levitan I, Volkov S, Subbaiah PV. Oxidized LDL: Diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal. 2010;13:39–75. doi: 10.1089/ars.2009.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koba S, Hirano T, Ito Y, Tsunoda F, Yokota Y, Ban Y, et al. Significance of small dense low-density lipoprotein-cholesterol concentrations in relation to the severity of coronary heart diseases. Atherosclerosis. 2006;189:206–14. doi: 10.1016/j.atherosclerosis.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Byfield FJ, Tikku S, Rothblat GH, Gooch KJ, Levitan I. OxLDL increases endothelial stiffness, force generation, and network formation. J Lipid Res. 2006;47:715–23. doi: 10.1194/jlr.M500439-JLR200. [DOI] [PubMed] [Google Scholar]
- 17.El Harchaoui K, van der Steeg WA, Stroes ES, Kuivenhoven JA, Otvos JD, Wareham NJ, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: The EPIC-Norfolk prospective population study. J Am Coll Cardiol. 2007;49:547–53. doi: 10.1016/j.jacc.2006.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi K, Kishi M, Atsumi T, Bertolaccini ML, Makino H, Sakairi N, et al. Circulating oxidized LDL forms complexes with beta2-glycoprotein I: Implication as an atherogenic autoantigen. J Lipid Res. 2003;44:716–26. doi: 10.1194/jlr.M200329-JLR200. [DOI] [PubMed] [Google Scholar]
- 19.Huang H, Mai W, Liu D, Hao Y, Tao J, Dong Y. The oxidation ratio of LDL: A predictor for coronary artery disease. Dis Markers. 2008;24:341–9. doi: 10.1155/2008/371314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haidari M, Moghadam M, Chinicar M, Ahmadieh A, Doosti M. Apolipoprotein B as the best predictor of coronary artery disease in Iranian normolipidemic patients. Clin Biochem. 2001;34:149–55. doi: 10.1016/s0009-9120(01)00192-8. [DOI] [PubMed] [Google Scholar]
- 21.Ridker PM, Rifai N, Cook NR, Bradwin G, Buring JE. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA. 2005;294:326–33. doi: 10.1001/jama.294.3.326. [DOI] [PubMed] [Google Scholar]
- 22.Hattori Y, Suzuki M, Tsushima M, Yoshida M, Tokunaga Y, Wang Y, et al. Development of approximate formula for LDL-chol, LDL-apo B and LDL-chol/LDL-apo B as indices of hyperapobetalipoproteinemia and small dense LDL. Atherosclerosis. 1998;138:289–99. doi: 10.1016/s0021-9150(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 23.Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: Correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER (HDL)) Clin Biochem. 2001;34:583–8. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 24.Onat A, Can G, Kaya H, Hergenç G. “Atherogenic index of plasma” (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4:89–98. doi: 10.1016/j.jacl.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Enas EA, Yusuf S, Mehta J. Meeting of the International Working Group on coronary artery disease in South Asians 24 March 1996, Orlando, Florida, USA. Indian Heart J. 1996;48:727–32. [PubMed] [Google Scholar]
- 26.Rahmani M, Raiszadeh F, Allahverdian S, Kiaii S, Navab M, Azizi F. Coronary artery disease is associated with the ratio of apolipoprotein A-I/B and serum concentration of apolipoprotein B, but not with paraoxonase enzyme activity in Iranian subjects. Atherosclerosis. 2002;162:381–9. doi: 10.1016/s0021-9150(01)00715-8. [DOI] [PubMed] [Google Scholar]
- 27.Gupta R, Vasisht S, Bahl VK, Wasir HS. Correlation of lipoprotein (a) to angiographically defined coronary artery disease in Indians. Int J Cardiol. 1996;57:265–70. doi: 10.1016/s0167-5273(96)02800-8. [DOI] [PubMed] [Google Scholar]
- 28.Segrest JP, Jones MK, De Loof H, Dashti N. Structure of apolipoprotein B-100 in low density lipoproteins. J Lipid Res. 2001;42:1346–67. [PubMed] [Google Scholar]
- 29.Morais CA, Oliveira SH, Lima LM. Lipid Tetrad Index (LTI) and Lipid Pentad Index (LPI) in healthy subjects. Arq Bras Cardiol. 2013;100:322–7. [PubMed] [Google Scholar]


