Abstract
IMPORTANCE
Physicians in training are at high risk for depression. However, the estimated prevalence of this disorder varies substantially between studies.
OBJECTIVE
To provide a summary estimate of depression or depressive symptom prevalence among resident physicians.
DATA SOURCES AND STUDY SELECTION
Systematic search of EMBASE, ERIC, MEDLINE, and PsycINFO for studies with information on the prevalence of depression or depressive symptoms among resident physicians published between January 1963 and September 2015. Studies were eligible for inclusion if they were published in the peer-reviewed literature and used a validated method to assess for depression or depressive symptoms.
DATA EXTRACTION AND SYNTHESIS
Information on study characteristics and depression or depressive symptom prevalence was extracted independently by 2 trained investigators. Estimates were pooled using random-effects meta-analysis. Differences by study-level characteristics were estimated using meta-regression.
MAIN OUTCOMES AND MEASURES
Point or period prevalence of depression or depressive symptoms as assessed by structured interview or validated questionnaire.
RESULTS
Data were extracted from 31 cross-sectional studies (9447 individuals) and 23 longitudinal studies (8113 individuals). Three studies used clinical interviews and 51 used self-report instruments. The overall pooled prevalence of depression or depressive symptoms was 28.8% (4969/17 560 individuals, 95% CI, 25.3%-32.5%), with high between-study heterogeneity (Q = 1247, τ2 = 0.39, I2 = 95.8%, P < .001). Prevalence estimates ranged from 20.9% for the 9-item Patient Health Questionnaire with a cutoff of 10 or more (741/3577 individuals, 95% CI, 17.5%-24.7%, Q = 14.4, τ2 = 0.04, I2 = 79.2%) to 43.2% for the 2-item PRIME-MD (1349/2891 individuals, 95% CI, 37.6%-49.0%, Q = 45.6, τ2 = 0.09, I2 = 84.6%). There was an increased prevalence with increasing calendar year (slope = 0.5% increase per year, adjusted for assessment modality; 95% CI, 0.03%-0.9%, P = .04). In a secondary analysis of 7 longitudinal studies, the median absolute increase in depressive symptoms with the onset of residency training was 15.8% (range, 0.3%-26.3%; relative risk, 4.5). No statistically significant differences were observed between cross-sectional vs longitudinal studies, studies of only interns vs only upper-level residents, or studies of nonsurgical vs both nonsurgical and surgical residents.
CONCLUSIONS AND RELEVANCE
In this systematic review, the summary estimate of the prevalence of depression or depressive symptoms among resident physicians was 28.8%, ranging from 20.9% to 43.2% depending on the instrument used, and increased with calendar year. Further research is needed to identify effective strategies for preventing and treating depression among physicians in training.
Studies have suggested that resident physicians experience higher rates of depression than the general public.1-5 Beyond the effects of depression on individuals, resident depression has been linked to poor-quality patient care and increased medical errors.6-8 However, estimates of the prevalence of depression or depressive symptoms vary across studies, from 3% to 60%.9,10 Studies also report conflicting findings about resident depression depending on specialty, postgraduate year, sex, and other characteristics.4,11-13 A reliable estimate of depression prevalence during medical training is important for informing efforts to prevent, treat, and identify causes of depression among residents.14 We conducted a systematic review and meta-analysis of published studies of depression or depressive symptoms in graduate medical trainees.
Methods
Search Strategy and Study Eligibility
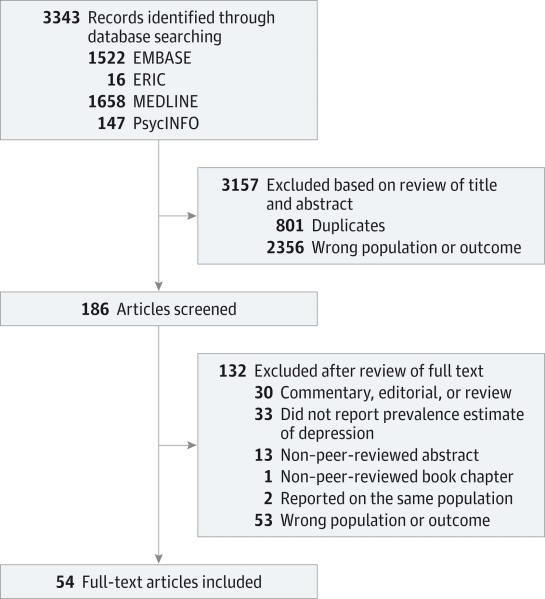
Cross-sectional and longitudinal studies published between January 1963 and September 2015 that reported on the prevalence of depression or depressive symptoms in interns, resident physicians, or both were identified using EMBASE, ERIC, MEDLINE, and PsycINFO (independently performed by D.A.M. and M.A.R.); by screening the reference lists of articles identified; and by correspondence with study investigators using the approach recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1).15 The computer-based searches combined terms related to interns, resident physicians, and study design with those related to depression, without language restriction (full details of the search strategy are provided in eMethods 1 in the Supplement). Studies were included if they reported data on resident physicians, were published in peer-reviewed journals, and used a validated method to assess for depression or depressive symptoms.16
Figure 1. Flow Diagram for Identifying Studies on the Prevalence of Depression or Depressive Symptoms Among Resident Physicians.
All studies identified by hand searching reference lists were found in the database search. For simplicity, this number is not duplicated in the diagram.
Data Extraction and Quality Assessment
The following information was independently extracted from each article by 2 trained investigators (D.A.M. and M.A.R.) using a standardized form: study design, geographic location, years of survey, specialty, postgraduate level, sample size, average age of participants, number and percentage of male participants, diagnostic or screening method used, outcome definition (ie, specific diagnostic criteria or screening instrument cutoff), and reported prevalence of depression or depressive symptoms. The most comprehensive publication was used when there were several involving the same population of residents. A modified version of the Newcastle-Ottawa Scale was used to assess the quality of nonrandomized studies included in systematic reviews and meta-analyses.17 This scale assesses quality in several domains: sample representativeness and size, comparability between respondents and nonrespondents, ascertainment of depressive symptoms, and statistical quality (full details regarding scoring are provided in eMethods 2 in the Supplement). Studies were judged to be at low risk of bias (≥3 points) or high risk of bias (<3 points). All discrepancies were resolved by discussion and adjudication of a third reviewer (S.S.).
Data Synthesis and Analysis
Prevalence estimates of depression or depressive symptoms were calculated by pooling the study-specific estimates using random-effects meta-analysis that accounted for between-study heterogeneity.18 Binomial proportion confidence intervals for individual studies were calculated using the Clopper-Pearson method, which allows for asymmetry. When longitudinal studies reported prevalence estimates made at different time periods within the year, the overall period prevalence for the time period was used. Between-study heterogeneity was assessed by standard χ2 tests and the I2 statistic (ie, the percentage of variability in prevalence estimates due to heterogeneity rather than sampling error, or chance, with values ≥75% indicating considerable heterogeneity)19,20 and by comparing results from studies grouped according to prespecified study-level characteristics (study design, country, year of baseline survey, specialty, postgraduate level, Newcastle-Ottawa Scale components, age, sex, and diagnostic method) using stratified meta-analysis and meta-regression.21,22 The influence of individual studies on the overall prevalence estimate was explored by serially excluding each study in a sensitivity analysis. A secondary analysis restricted to longitudinal studies reporting both preresidency and intraresidency depressive symptom prevalence estimates was performed to better isolate associations with the residency experience from associations with assessment tools. Bias secondary to small study effects was investigated by funnel plot and Egger test.23,24 All analyses were performed using R version 3.2.2 (R Foundation for Statistical Computing).25 Statistical tests were 2-sided and used a significance threshold of P < .05.
Results
Study Characteristics
Thirty-one cross-sectional10-13,26-52 and 23 longitudinal4,6-8,53-71 studies involving a total of 17 560 individuals were included in the study (Figure 1, Table 1, and Table 2). Thirty-five took place in North America, 9 in Asia, 5 in Europe, 4 in South America, and 1 in Africa. Twenty-eight studies recruited residents from multiple specialties, while 26 recruited exclusively from single specialties. Thirteen studies included interns only, 36 included both interns and residents, and 5 included upper-level residents only. The median number of participants per study was 141 (range, 27-2323). Eleven studies assessed for depressive symptoms using the Beck Depression Inventory (BDI),72 11 used the Center for Epidemiologic Studies Depression Scale (CES-D),73 8 used the 2-item Primary Care Evaluation of Mental Disorders questionnaire (PRIME-MD),74 7 used the 9-item Patient Health Questionnaire (PHQ-9),75 4 used the Zung Self-rating Depression Scale (SDS),76 3 used the Harvard Department of Psychiatry/National Depression Screening Day Scale (HANDS),77 and 7 used other methods.78-82 Three assessed for depression using structured interviews.83 The diagnostic criteria and scoring cutoffs used by the studies are summarized in Table 1. When evaluated by Newcastle-Ottawa quality assessment criteria, out of 5 possible points, 3 studies received 5 points, 13 received 4 points, 23 received 3 points, 10 received 2 points, 4 received 1 point, and 1 received 0 points (scores for individual studies are presented in eTable 1 in the Supplement).
Table 1.
Selected Characteristics of the 31 Cross-sectional Studies Included in This Systematic Review and Meta-analysis
| Source | Country | Survey Years | Specialty | PGY | No. of Participants | Age, y | Men, No. (%) | Diagnostic Method | Outcome Definition | NOS |
|---|---|---|---|---|---|---|---|---|---|---|
| de Oliveira et al,47 2013 | United States | 2011 | Anesthesia | 1-4 | 1384 | No. (%) ≤30 y: 779 (54.0) | 850 (57.0) | HANDS | >9 | 5 |
| Waldman et al,43 2009 | Argentina | 2007 | Cardiology | 3-4 | 106 | Mean (SD), 29.1 (2.4) | 70 (66.0) | 21-Item BDI | ≥10 | 3 |
| Hasanović and Herenda,39 2008 | Bosnia and Herzegovina | 2004 | Family medicine | ≥1 | 78 | Median (range), NR (30-45) | 12 (15.4) | HSCL-25 | ≥1.75 | 3 |
| Godenick et al,29 1995 | United States | 1992 | Family medicine | 1-4 | 164 | Mean (SD), 30.3 (4.6) | 133 (74.7) | 21-Item BDI | ≥10 | 3 |
| Oriel et al,33 2004 | United States | NR | Family medicine | 1-4 | 185 | Mean (range), 33 (26-57) | 87 (47.0) | 9-Item survey | DSM-IV criteria | 1 |
| Earle and Kelly,34 2005 | Canada | 2002 | Family medicine | ≥1 | 254 | Mean (SD), 29 (NR) | 90 (35.4) | PHQ-9 | ≥10 | 4 |
| Hainer and Palesch,30 1998 | United States | 1993-1996 | Family medicine | 1-3 | 268 | Mean (SD), 30.4 (5.2) | 239 (68.3) | 21-Item BDI | ≥10 | 4 |
| Lam et al,44 2010 | Hong Kong | 2005 | General internship | 1 | 95 | Mean (range), 24.4 (23-28) | 48 (49.5) | DASS-21 | ≥10 | 3 |
| Sakata et al,40 2008 | Japan | 2005 | General internship | 1-2 | 196 | Mean (SD), 27.3 (2.9) | 149 (76) | CES-D | ≥19 | 3 |
| Hsieh et al,13 2011 | Taiwan | 2004-2005 | General internship | 1 | 302 | NR | 216 (71.5) | Zung SDS | ≥41 | 2 |
| Costa et al,45 2012 | Brazil | 2008 | Internal medicine | 1 | 84 | Mean (SD), 24.6 (3.8) | 45 (53.6) | 21-Item BDI | ≥10 | 3 |
| Shanafelt et al,32 2002 | United States | 2001 | Internal medicine | 1-3 | 115 | NR | 54 (47.0) | PRIME-MD | Yes to either item | 0 |
| Yi et al,37 2006 | United States | 2003 | Medical and pediatric | ≥1 | 227 | Mean (SD), 28.7 (3.8) | 95 (42) | CES-D | ≥10 | 3 |
| Raviola et al,31 2002 | Kenya | 1997-1999 | Medical and surgical | 3-4 | 50 | Mean (SD), 33 (NR) | NR | Structured interview | DSM-IV criteria | 2 |
| Valko and Clayton,27 1975 | United States | 1972 | Medical and surgical | 1 | 53 | NR | NR | Structured interview | DSM-II criteria | 2 |
| Kirsling et al,12 1989 | United States | 1987-1988 | Medical and surgical | 1 | 58 | NR | 38 (62.3) | 21-Item BDI | ≥10 | 3 |
| Cruz EP,36 2006 | Mexico | NR | Medical and surgical | 1-6 | 80 | Mean (SD), 27.5 (1.8) | 53 (66.3) | Zung SDS | ≥41 | 1 |
| Demir et al,38 2007 | Turkey | 2004 | Medical and surgical | ≥1 | 86 | Mean (SD), 28.2 (3.2) | 38 (44.2) | 21-Item BDI | ≥11 | 3 |
| Sánchez et al,41 2008 | Mexico | 2007-2008 | Medical and surgical | 1-3 | 90 | Mean (SD), 28.6 (0.5) | 49 (54.4) | HAM-D | ≥8 | 4 |
| Al Ghafri et al,48 2014 | Oman | 2011 | Medical and surgical | 1-4 | 132 | 73%<30 y | 42 (31.8) | PHQ-9 | ≥12 | 3 |
| Al-Maddah et al,51 2015 | Saudi Arabia | 2012 | Medical and surgical | 1-5 | 171 | Median (range), NR (25-35) | 72 (42) | 21-Item BDI | ≥10 | 3 |
| Yousuf et al,10 2011 | Pakistan | 2008 | Medical and surgical | ≥1 | 172 | No. (%) <30 y: 104 (70.3) | 111 (64.5) | Zung SDS | ≥45 | 2 |
| Steinert et al,28 1991 | Canada | 1984 | Medical and surgical | 1-6 | 255 | Mean (range), 27.7 (21-52) | 182 (71.4) | Zung SDS | ≥50 | 4 |
| Stoesser and Cobb,50 2014 | United States | 2009 | Medical and surgical | ≥1 | 260 | Mean (range), 30.8 (25-55) | 126 (50.2) | PHQ-9 | ≥10 | 4 |
| Pereira-Lima and Loureiro,52 2015 | Brazil | 2012 | Medical and surgical | 1-5 | 305 | Mean (SD), 28 (2.5) | 159 (52.1) | PHQ-4 | ≥3 | 4 |
| Goebert et al,42 2009 | United States | 2003-2004 | Medical and surgical | 1-4 | 532 | NR | 254 (48) | CES-D | ≥16 | 3 |
| Dyrbye et al,49 2014 | United States | 2011-2012 | Medical and surgical | 1-7 | 1701 | Median (range), 31 (NR) | 824 (48.6) | PRIME-MD | Yes to either item | 3 |
| Hsu and Marshall,11 1987 | Canada | 1984-1985 | Medical and surgical | ≥1 | 1785 | Mean (SD), 29 (4.2) | 1184 (66.3) | CES-D | ≥16 | 4 |
| Govardhan et al,46 2012 | United States | 2009 | Ob/gyn | 1-4 | 56 | Mean (SD), 30.1 (3.0) | 5 (8.8) | CES-D | >16 | 3 |
| Becker et al,35 2006 | United States | 2004 | Ob/gyn | 1-4 | 120 | Mean (SD), 29.3 (3.0) | 26 (20.8) | CES-D | ≥16 | 3 |
| Waring EM,26 1974 | United Kingdom | NR | Psychiatry | ≥1 | 83 | NR | NR | GHQ | ≥12 | 2 |
Abbreviations: BDI, Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale;DASS-21, 21-item Depression, Anxiety, and Stress Scale; DSM, Diagnostic and Statistical Manual of Mental Disorders; GHQ, General Health Questionnaire; HADS-D, Hospital Anxiety and Depression Scale; HAM-D, Hamilton Depression Rating Scale; HANDS, Harvard Department of Psychiatry/National Depression Screening Day Scale; HSCL-25, 25-item Hopkins Symptom Checklist; NOS, Newcastle-Ottawa score; NR, not reported; PGY, postgraduate year; PHQ-9, 9-item Patient Health Questionnaire; PRIME-MD, 2-item Primary Care Evaluation of Mental Disorders questionnaire; SSTDS, Spielberger State-Trait Depression Scale; Zung SDS, Zung Self-rating Depression Scale.
Table 2.
Selected Characteristics of the 23 Longitudinal Studies Included in This Systematic Review and Meta-analysis
| Source | Country | Survey Years | Specialty | PGY | No. of Participants | Age, y | Men, No. (%) | Diagnostic Method | Outcome Definition | NOS |
|---|---|---|---|---|---|---|---|---|---|---|
| Katz et al,57 2006 | United States | 2003-2004 | Emergency medicine | 1-4 | 31 | Median (range), 29 (24-49) | 33 (66.0) | CES-D | >14 | 3 |
| Revicki et al,55 1993 | United States | 1989-1992 | Emergency medicine | 1-3 | 1117 | Mean (SD), 30 (3.6) | 827 (74.0) | CES-D | >16 | 4 |
| Kleim et al,68 2014 | Switzerland | NR | General rotating internship | 1 | 47 | Mean (SD), 24 (2) | 20 (42.5) | PHQ-9 | ≥5 | 2 |
| Ito et al,70 2015 | Japan | 2011 | General rotating internship | 1 | 1209 | Mean (SD), 26 (3) | 668 (65.5)a | CES-D | ≥16 | 4 |
| Rosen et al,58 2006 | United States | 2002-2003 | Internal medicine | 1 | 47 | NR | 28 (48.3) | 13-Item BDI | ≥8 | 2 |
| Reuben DB,54 1985 | United States | 1981-1982 | Internal medicine | 1-3 | 68 | NR | NR | CES-D | ≥16 | 1 |
| Campbell et al,62 2010 | United States | 2003-2008 | Internal medicine | 1-3 | 86 | Mean (SD), NR (26-40) | 44 (51.1) | PRIME-MD | Yes to either item | 1 |
| Wada et al,59 2007 | Japan | 2005-2006 | Internal medicine | 1 | 99 | Median (range), NR (24-39) | 71 (71.7) | CES-D | ≥19 | 4 |
| Gopal et al,56 2005 | United States | 2003-2004 | Internal medicine | 1-3 | 121 | Median (range), NR (26-40) | 53 (43.8) | PRIME-MD | Yes to either item | 2 |
| West et al,6 2006 | United States | 2003-2006 | Internal medicine | 1-3 | 149 | No. (%) ≤30 y: 129 (70.1) | 94 (51.1) | PRIME-MD | Yes to either item | 2 |
| Beckman et al,63 2012 | United States | 2009-2010 | Internal medicine | 1-3 | 202 | ≥24 | 116 (57.4) | PRIME-MD | Yes to either item | 3 |
| West et al,8 2009 | United States | 2003-2009 | Internal medicine | 1-3 | 239 | No. (%) ≤30 y: 240 (63.2) | 236 (62.1) | PRIME-MD | Yes to either item | 3 |
| West et al,65 2012 | United States | 2007-2011 | Internal medicine | 1-3 | 278 | No. (%) ≤30 y: 209 (84.3) | 208 (61.2) | PRIME-MD | Yes to either item | 3 |
| Ford and Wentz,53 1984 | United States | NR | Medical and surgical | 1 | 27 | Median (range), 26 (NR) | 22 (81.4) | Structured interview | DSM-III criteria | 3 |
| Jiménez-López et al,71 2015 | Mexico | NR | Medical and surgical | 2 | 100 | Mean (SD), 26.4 (1.8) | 70 (64.8) | 13-Item BDI | ≥5 | 2 |
| Buddeberg-Fischer et al,61 2009 | Switzerland | 2001-2007 | Medical and surgical | 2, 4, 6 | 390 | Mean (SD), 33 (2.2) | 176 (45.1) | HADS-D | ≥8 | 3 |
| Weigl et al,54 2012 | Germany | NR | Medical and surgical | 2-3 | 415 | Mean (SD), 30.5 (2.7) | 218 (52.5) | 10-Item SSTDS | >24.21 | 4 |
| Sen et al,4 2010 | United States | 2007-2009 | Medical and surgical | 1 | 740 | Mean (SD), 27.9 (2.8) | 337 (45.6) | PHQ-9 | ≥10 | 5 |
| Sen et al,66 2013 | United States | 2009-2011 | Medical and surgical | 1 | 2323 | Mean (SD), 27.6 (2.9) | 1140 (49.1) | PHQ-9 | ≥10 | 5 |
| Cubero et al,69 2015 | Brazil | 2010-2011 | Medical oncology | ≥1 | 50 | Median (IQR), 28.4 (27.4-29.7) | 29 (53.7) | 21-Item BDI | ≥16b | 3 |
| Velásquez-Pérez et al,67 2013 | Mexico | 2010-2011 | Neurology, neurosurgery, psychiatry | 1 | 43 | Mean (range), 25 (24-41) | 26 (60.5) | 21-Item BDI | ≥10 | 3 |
| Fahrenkopf et al,7 2008 | United States | 2003 | Pediatrics | 1-3 | 123 | No. (%) <30 y: 76 (62.0) | 37 (30.1) | HANDS | ≥9 | 4 |
| Landrigan et al,60 2008 | United States | 2003-2004 | Pediatrics | 1-3 | 209 | Mean (SD), 29.7 (NR) | 64 (30.4) | HANDS | >9 | 4 |
Abbreviations: BDI, Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; DSM-III, Diagnostic and Statistical Manual of Mental Disorders (Third Edition); HADS-D, Hospital Anxiety and Depression Scale; HANDS, Harvard Department of Psychiatry/National Depression Screening Day Scale; NOS, Newcastle-Ottawa score; NR, not reported; PGY, postgraduate year; PHQ-9, 9-item Patient Health Questionnaire; PRIME-MD, 2-item Primary Care Evaluation of Mental Disorders questionnaire; SSTDS, Spielberger State-Trait Depression Scale.
Based on a subset of participants.
The authors do not explicitly report a cutoff, but the study they cite suggests that it is 16.
Prevalence of Depression or Depressive Symptoms Among Resident Physicians
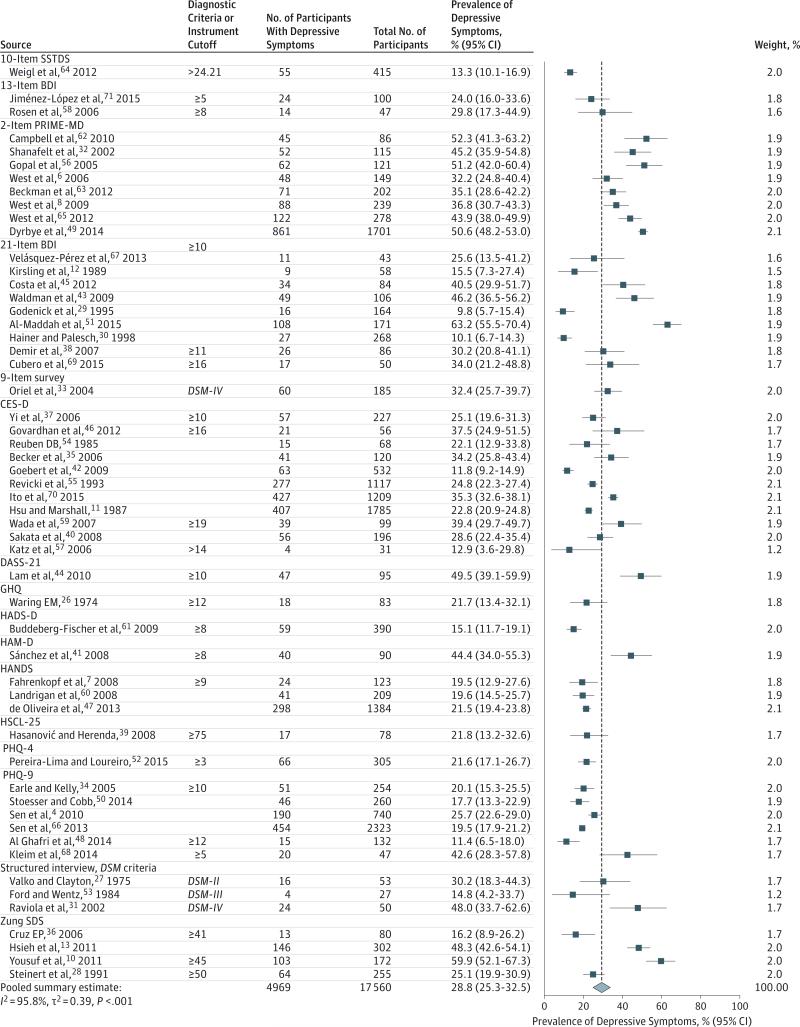
Meta-analytic pooling of the prevalence estimates of depression or depressive symptoms reported by the 54 studies yielded a summary prevalence of 28.8% (4969/17 560 individuals, 95% CI, 25.3%-32.5%), with significant evidence of between-study heterogeneity (Q = 1247, P < .001, τ2 = 0.39, I2 = 95.8%) (Figure 2). Sensitivity analysis, in which the meta-analysis was serially repeated after exclusion of each study, demonstrated that no individual study affected the overall prevalence estimate by more than 1% (eTable 2 in the Supplement).
Figure 2. Meta-analysis of the Prevalence of Depression or Depressive Symptoms Among Resident Physicians.
Contributing studies are stratified by screening modality and ordered by increasing sample size. The area of each square is proportional to the inverse variance of the estimate. The dotted line marks the overall summary estimate for all studies, 28.8% (4969/17 560 individuals, 95% CI, 25.3%-32.5%, Q = 1247.11, τ2 = 0.39, I2 = 95.8% [95% CI, 95.0%-96.4%], P < .001). (Refer to footnotes of Table 1 and Table 2 for expanded names of diagnostic instruments.)
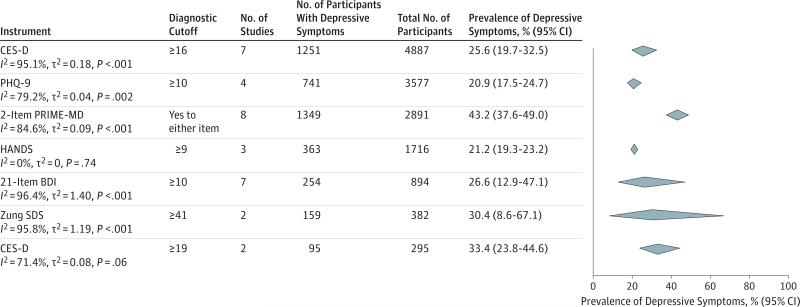
To provide a range of the depression or depressive symptom prevalence estimates identified by these methodologically diverse studies, estimates were stratified by screening instrument and cutoff score (Figure 3). Summary prevalence estimates ranged from 20.9% for the PHQ-9 with cutoff of 10 or more (741/3577 individuals, 95% CI, 17.5%-24.7%, Q = 14.4, τ2 = 0.04, I2 = 79.2%) to 43.2% for the 2-item PRIME-MD (1349/2891 individuals, 95% CI, 37.6%-49.0%, Q = 45.6, τ2 = 0.09, I2 = 84.6%). The 8 studies using the 2-item PRIME-MD yielded significantly higher estimates than did the others (Q = 69.0, P < .001). In contrast, there were no significant differences between estimates made using the CES-D, PHQ-9, HANDS, BDI, or Zung SDS (Q = 8.65, P = .12), suggesting that variation between instruments did not explain the heterogeneity in the observed depression or depressive symptom prevalence estimates. A model including only those studies4,7,34,47,48,50,60,66 using inventories with specificities greater than 88% yielded a prevalence estimate of 20.2% (1119/5425, 95% CI, 18.0%-22.6%, Q = 22.0, P < .01, τ2 = 0.02, I2 = 68.2%).
Figure 3. Meta-analyses of the Prevalence of Depressive Symptoms Among Resident Physicians in Subsets of Studies Stratified by Screening Modality and Cutoff Score.
The area of each diamond is proportional to the inverse variance of the estimate. BDI indicates Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; HANDS, Harvard Department of Psychiatry/National Depression Screening Day Scale; PHQ-9, 9-item Patient Health Questionnaire; PRIME-MD, 2-item Primary Care Evaluation of Mental Disorders questionnaire; Zung SDS, Zung Self-rating Depression Scale.
Prevalence of Depression or Depressive Symptoms by Study-Level Characteristics
Among all 54 studies, the prevalence of depression or depressive symptoms significantly increased with baseline survey year (slope = 0.5% per calendar-year increase; 95% CI, 0.03%-0.9%; test of moderator, Q = 4.4, P = .04). This association persisted when studies using the 2-item PRIME-MD were excluded and the analysis was restricted to the 23 studies using the CES-D, PHQ-9, HANDS, BDI, or Zung SDS presented in Figure 3 (slope = 0.6% per calendar-year increase; 95% CI, 0.1%-1.2%, P = .02).
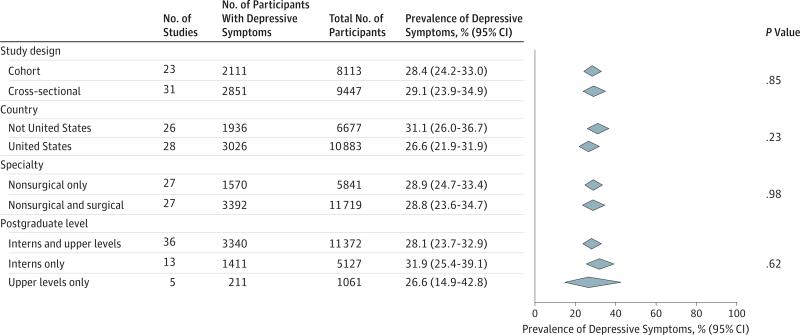
Among the full set of studies, no statistically significant differences in prevalence estimates were noted between cross-sectional vs longitudinal studies (2851/9447, 29.1% [95% CI, 23.9% to 34.9%] vs 2111/8113, 28.4% [95% CI, 24.2% to 33.0%]; test for subgroup differences, Q = 0.04, P = .85), studies in the United States vs elsewhere (3026/10 883, 26.6% [95% CI, 21.9% to 31.9%] vs 1936/6677, 31.1% [95% CI, 26.0% to 36.7%]; Q = 1.4, P = .23), studies of non-surgical vs both nonsurgical and surgical residents (1570/5841, 28.9% [95% CI, 24.7% to 33.4%] vs 3392/11 719, 28.8% [95% CI, 23.6% to 34.7%]; Q = 0, P = .98), or studies of only interns vs those of only upper-level residents (1411/5127, 31.9% [95% CI, 25.4% to 39.1%] vs 211/1061, 26.6% [95% CI, 14.9% to 42.8%]; Q = 0.9, P = .62) (Figure 4). There were no significant associations between prevalence and mean or median age (slope = −1.0% per year [95% CI, −2.8% to 0.8%]; Q = 1.2, P = .28) or percentage of males (slope = 3.4% per percentage increase in males [95% CI, −28.9% to 22.1%]; Q = 0.1, P = .79).
Figure 4. Meta-analyses of the Prevalence of Depression or Depressive Symptoms Among Resident Physicians Stratified by Study-Level Characteristics.
The area of each diamond is proportional to the inverse variance of the estimate.
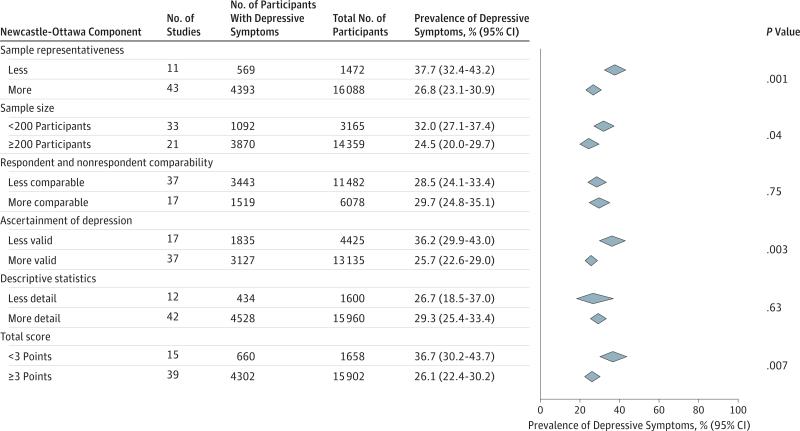
When evaluated by Newcastle-Ottawa criteria, studies with lower total overall quality scores yielded higher depression estimates (660/1658, 36.7% [95% CI, 30.2%-43.7%] vs 4302/15 902, 26.1% [95% CI, 22.4%-30.2%]; Q = 7.3, P = .007) (Figure 5). In terms of individual quality assessment criteria, higher prevalence estimates were found among studies with less representative participant populations (569/1472, 37.7% [95% CI, 32.4%-43.2%] vs 4393/16 088, 26.8% [95% CI, 23.1%-30.9%]; Q = 10.4, P = .001) and less valid assessment methods (1835/4425, 36.2% [95% CI, 29.9%-43.0%] vs 3127/13 135, 25.7% [95% CI, 22.6%-29.0%]; Q = 8.6, P = .003). No statistically significant differences in prevalence estimates were noted when studies were stratified by respondent/nonrespondent comparability criteria (Q = 0.11, P = .75) or by quality of descriptive statistic reporting (Q = 0.23, P = .63).
Figure 5. Meta-analyses of the Prevalence of Depression or Depressive Symptoms Among Resident Physicians Stratified by Newcastle-Ottawa Scale Components and by Total Score.
The area of each diamond is proportional to the inverse variance of the estimate.
Heterogeneity Within Screening Instruments
To identify potential sources of heterogeneity independent of assessment modality, heterogeneity was examined within the studies using common instruments when at least 5 studies were available and at least 2 studies were in each comparator subgroup. Among the 7 studies using the CES-D and a cutoff of 16 or greater, heterogeneity was not accounted for by study design (Q = 0.3, P = .61), baseline survey year (Q = 1.3, P = .25), specialty (Q = 0.2, P = .70), sample size (Q = 2.1, P = .15), age (Q = 0.7, P = .41), or sex (Q = 0.7, P = .41) (full results are provided in eTable3 in the Supplement). Among the 8 studies using the 2-item PRIME-MD, heterogeneity was partially explained by study design (cross-sectional studies yielded higher estimates, 49.8% vs 41.3%; Q = 5.2, P = .02) and respondent/nonrespondent comparability (studies that established comparability yielded lower estimates, 39.6% vs 50.4%; Q = 10.3, P = .001) but was not significantly explained by sample size (Q = 0.2, P = .64), sex (Q = 2.7, P = .10), baseline survey year (Q = 0.1, P = .80), or Newcastle-Ottawa score (Q = 0.2, P = .64). Among 7 studies using the 21-item BDI with cutoff of 10 or greater, heterogeneity was in part explained by country (United States vs other, 10.7% vs 44.6%; Q = 30.7, P < .001), baseline survey year (Q = 13.4, P < .001), and sex (Q = 10.7, P = .001), but not by specialty (Q = 0.3, P = .58), postgraduate year (Q = 0, P = .99), age (Q = 1.3, P = .26), or respondent/nonrespondent comparability (Q = 0, P = .99).
Secondary Analysis of Longitudinal Studies
In a secondary analysis of 7 longitudinal studies,4,58,59,66-68,70 the temporal relationship between exposure to residency training and increased depressive symptoms was assessed (Table 3). Because studies used different assessment instruments, the relative change in depressive symptoms was calculated for each study individually (ie, follow-up divided by baseline prevalence), and then the relative changes derived from individual studies were meta-analyzed. Overall, the median absolute increase in depressive symptoms with the onset of residency training was 15.8% (range, 0.3%-26.3%; relative risk, 4.5).
Table 3.
Secondary Analysis of 7 Longitudinal Studies Reporting Prevalence Estimates Both Prior to and During Internship
| Baseline |
Follow-up |
Comparison |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Source | Instrument | Cutoff | Follow-up | No. Depressed | Total No. | Prevalence, % (95% CI) | No. Depressed | Total No. | Prevalence, % (95% CI) | Absolute Increase, % (95%CI) | Relative Increase Ratio, (95% CI) |
| Velásquez-Pérez et al,67 2013 | 21-Item BDI | ≥10 | 1y | 1 | 43 | 2.3 (0.1-12.3) | 5 | 32 | 15.6 (5.3-32.8) | 13.3 (13.2-13.4) | 6.7 (6.6-7.0) |
| Rosen et al,58 2006 | 13-Item BDI | ≥8 | 1y | 2 | 58 | 3.4 (0.4-11.9) | 14 | 47 | 29.8 (17.3-44.9) | 26.3 (26.3-26.5) | 8.6 (8.6-8.9) |
| Kleim et al,68 2014 | PHQ-9 | ≥5 | 3 mo | 12 | 47 | 25.5 (13.9-40.4) | 20 | 47 | 42.6 (28.3-57.8) | 17.0 (17.0-17.3) | 1.7 (1.7-1.7) |
| Wada et al,59 2007 | CES-D | ≥19 | 1y | 16 | 62 | 25.8 (15.5-38.5) | 12 | 46 | 26.1 (14.3-41.1) | 0.3 (0.1-0.5) | 1.0 (1.0-1.0) |
| Sen et al,4 2010 | PHQ-9 | ≥10 | 1y | 29 | 740 | 3.9 (2.6-5.6) | 190 | 740 | 25.7 (22.6-29.0 | 21.8 (21.8-21.8) | 6.6 (6.6-6.6) |
| Ito et al,70 2015 | CES-D | ≥16 | 3 mo | 189 | 1209 | 15.6 (13.6-17.8) | 238 | 1020 | 23.3 (20.8-26.1) | 7.7 (7.7-7.7) | 1.5 (1.5-1.5) |
| Sen et al,66 2013 | PHQ-9 | ≥10 | 1y | 86 | 2323 | 3.7 (3.0-4.6) | 454 | 2323 | 19.5 (18.0-21.2) | 15.8 (15.8-15.8) | 5.3 (5.3-5.3) |
Abbreviations: BDI, Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; PHQ-9, 9-item Patient Health Questionnaire.
Assessment of Publication Bias
Although visual inspection of the funnel plot revealed relatively minimal asymmetry (eFigure in the Supplement), there was evidence of small studies effect (Egger test P = .02), with smaller studies (<200 participants) reporting more extreme depression prevalence estimates than larger studies (32.0% [95% CI, 27.1%-37.4%] vs 24.5% [95% CI, 20.0%-29.7%]; Q = 4.2, P = .04) (Figure 5).
Discussion
This systematic review and meta-analysis of 54 studies involving 17 560 physicians in training demonstrated that between 20.9% and 43.2% of trainees screened positive for depression or depressive symptoms during residency. Because the development of depression has been linked to a higher risk of future depressive episodes and greater long-term morbidity, these findings may affect the long-term health of resident doctors.84,85 Depression among residents may also affect patients, given established associations between physician depression and lower-quality care.6-8 These findings highlight an important issue in graduate medical education.
In interpreting the results of this meta-analysis, it is important to note that the vast majority of participants were assessed through self-report inventories that measured depressive symptoms, rather than gold-standard diagnostic clinical interviews for major depressive disorder. The sensitivity and specificity of these instruments for diagnosing major depressive disorder vary substantially (eTable 4 in the Supplement).86 Instruments such as the 2-item PRIME-MD have low specificity (66%, 95% CI, 48%-84%) and should be viewed as screening tools. In contrast, other commonly used instruments, such as the PHQ-9, have high sensitivity (88%, 95% CI, 74%-96%) and specificity (88%, 95% CI, 85%-90%) for diagnosing major depressive disorder and have been shown to be comparable with clinician-administered assessments. Furthermore, although self-report measures of depressive symptoms have limitations, there is evidence that among medical trainees the absence of anonymity in formal diagnostic assessments may compromise accurate assessment of sensitive personal information such as depressive symptoms.87 To reflect the heterogeneity of the measures included in this meta-analysis, a range of prevalence estimates (ie, 20.9%-43.2%) was reported in addition to a single measure (ie, 28.8%).
This study found an increase in depressive symptoms among residents over time that in part explained the heterogeneity between studies. This increase, while modest, is notable given efforts by the Accreditation Council for Graduate Medical Education,88 European Working Time Directive,89 and others90 to limit trainee duty hours and improve work conditions. The identified trend may reflect the medical community's increased awareness of depression or developments external to medical education.91 Future studies should explore specific factors that may explain this trend.
A secondary analysis restricted to longitudinal studies found a significant increase in depressive symptoms among trainees after the start of residency. The median absolute increase in depressive symptoms among trainees was 15.8% (range, 0.3%-26.3%) within a year of beginning training. This finding, in combination with evidence that the prevalence of depressive symptoms is similar across specialties and countries, suggests that the underlying causes of depressive symptoms are common to the residency experience. Identifying the factors that negatively affect trainee mental health may help inform the development of effective interventions for the reduction of depression that would be generalizable to different countries and specialties.
Variation in study sample size contributed importantly to the observed heterogeneity in the data. Studies with fewer participants generally yielded more extreme prevalence estimates, suggesting the presence of publication bias. Furthermore, some studies used screening instruments in nonstandard ways (eg, with cutoff scores that have not been validated). These variations were captured in part by Newcastle-Ottawa score, which assessed the risk of bias in each study. Studies with higher risk of bias yielded higher prevalence estimates of depressive symptoms. Study design (ie, cross-sectional vs longitudinal), country, survey years, specialty, postgraduate level, age, and sex also contributed to the heterogeneity between studies.
Limitations should be considered when interpreting the findings of this study. First, a substantial amount of the heterogeneity among the studies remained unexplained by the variables examined. Unexamined factors, such as the institutional cultures of specific residency programs, may contribute to the risk for depressive symptoms among trainees. A better understanding of program culture and working environments may help elucidate some of the root causes of depressive symptoms. Second, the data were derived from studies that used different designs and involved different groups of trainees (eg, from different countries, specialties, and years of training). For example, all but 3 studies used screening tools to measure depressive symptoms, and the 3 that employed structured interviews used convenience samples not representative of the resident population at large. Because the studies were heterogeneous with respect to screening inventories and resident populations, the prevalence of major depressive disorder could not be precisely determined. However, a secondary meta-analysis of studies using validated, high-specificity (>88%) inventories involving 5425 participants yielded a prevalence of 20.2%, which may better reflect the true prevalence of major depression. Third, the analysis relied on aggregated published data. A multicenter prospective study using a single validated measure of depression and structured diagnostic interviews in a random subset of participants would provide a more accurate estimate of the prevalence of depression among physicians in training.
Conclusions
In this systematic review, the summary estimate of the prevalence of depression or depressive symptoms among resident physicians was 28.8%, ranging from 20.9% to 43.2% depending on the instrument used, and increased with time. Further research is needed to identify effective strategies for preventing and treating depression among physicians in training.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported in part by a US Department of State Fulbright Scholarship (D.A.M.), National Institutes of Health (NIH) funding (R01MH101459 to S.S.), and NIH Medical Scientist Training Program funding (TG 2T32GM07205 to M.A.R.).
Role of the Funder/Sponsor: The study funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Mata had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Mata.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Mata, Ramos.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Mata, Bansal, Di Angelantonio. Obtained funding: Guille, Sen.
Administrative, technical, or material support: Guille, Sen.
Study supervision: Guille, Sen.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources.
REFERENCES
- 1.Schneider SE, Phillips WM. Depression and anxiety in medical, surgical, and pediatric interns. Psychol Rep. 1993;72(3 pt 2):1145–1146. doi: 10.2466/pr0.1993.72.3c.1145. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. 2006;81(4):354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Sen S, Kranzler HR, Krystal JH, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67(6):557–565. doi: 10.1001/archgenpsychiatry.2010.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joules N, Williams DM, Thompson AW. Depression in resident physicians: a systematic review. Open J Depress. 2014;03(03):89–100. [Google Scholar]
- 6.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 7.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–491. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 9.Buddeberg-Fischer B, Klaghofer R, Buddeberg C. Stress at work and well-being in junior residents [in German]. Z Psychosom Med Psychother. 2005;51(2):163–178. doi: 10.13109/zptm.2005.51.2.163. [DOI] [PubMed] [Google Scholar]
- 10.Yousuf A, Ishaque S, Qidwai W. Depression and its associated risk factors in medical and surgical post graduate trainees at a teaching hospital: a cross sectional survey from a developing country. J Pak Med Assoc. 2011;61(10):968–973. [PubMed] [Google Scholar]
- 11.Hsu K, Marshall V. Prevalence of depression and distress in a large sample of Canadian residents, interns, and fellows. Am J Psychiatry. 1987;144(12):1561–1566. doi: 10.1176/ajp.144.12.1561. [DOI] [PubMed] [Google Scholar]
- 12.Kirsling RA, Kochar MS, Chan CH. An evaluation of mood states among first-year residents. Psychol Rep. 1989;65(2):355–366. doi: 10.2466/pr0.1989.65.2.355. [DOI] [PubMed] [Google Scholar]
- 13.Hsieh Y-H, Hsu C-Y, Liu C-Y, Huang T-L. The levels of stress and depression among interns and clerks in three medical centers in Taiwan: a cross-sectional study. Chang Gung Med J. 2011;34(3):278–285. [PubMed] [Google Scholar]
- 14.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr LK, Kerr LD., Jr Screening tools for depression in primary care: the effects of culture, gender, and somatic symptoms on the detection of depression. West J Med. 2001;175(5):349–352. doi: 10.1136/ewjm.175.5.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 18.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sterne JAC, Jüni P, Schulz KF, Altman DG, Bartlett C, Egger M. Statistical methods for assessing the influence of study characteristics on treatment effects in ‘meta-epidemiological’ research. Stat Med. 2002;21(11):1513–1524. doi: 10.1002/sim.1184. [DOI] [PubMed] [Google Scholar]
- 22.van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med. 2002;21(4):589–624. doi: 10.1002/sim.1040. [DOI] [PubMed] [Google Scholar]
- 23.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 25. [November 6, 2015];The R project for statistical computing. http://www.R-project.org/.
- 26.Waring EM. Emotional illness in psychiatric trainees. Br J Psychiatry. 1974;125(0):10–11. doi: 10.1192/bjp.125.1.10. [DOI] [PubMed] [Google Scholar]
- 27.Valko RJ, Clayton PJ. Depression in the internship. Dis Nerv Syst. 1975;36(1):26–29. [PubMed] [Google Scholar]
- 28.Steinert Y, Magonet G, Rubin G, Carson K. Emotional well-being of house staff: comparison of residency training programs. Can Fam Physician. 1991;37:2130–2138. [PMC free article] [PubMed] [Google Scholar]
- 29.Godenick MT, Musham C, Palesch Y, Hainer BL, Michels PJ. Physical and psychological health of family practice residents. Fam Med. 1995;27(10):646–651. [PubMed] [Google Scholar]
- 30.Hainer BL, Palesch Y. Symptoms of depression in residents: a South Carolina Family Practice Research Consortium study. Acad Med. 1998;73(12):1305–1310. doi: 10.1097/00001888-199812000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Raviola G, Machoki M, Mwaikambo E, Good MJD. HIV, disease plague, demoralization and “burnout”: resident experience of the medical profession in Nairobi, Kenya. Cult Med Psychiatry. 2002;26(1):55–86. doi: 10.1023/a:1015289132151. [DOI] [PubMed] [Google Scholar]
- 32.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 33.Oriel K, Plane MB, Mundt M. Family medicine residents and the impostor phenomenon. Fam Med. 2004;36(4):248–252. [PubMed] [Google Scholar]
- 34.Earle L, Kelly L. Coping strategies, depression, and anxiety among Ontario family medicine residents. Can Fam Physician. 2005;51:242–243. [PMC free article] [PubMed] [Google Scholar]
- 35.Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195(5):1444–1449. doi: 10.1016/j.ajog.2006.06.075. [DOI] [PubMed] [Google Scholar]
- 36.Cruz EP. Burnout syndrome as a risk factor of depression in medical residents. Med Interna Mex. 2006;22(4):282–286. [Google Scholar]
- 37.Yi MS, Luckhaupt SE, Mrus JM, et al. Religion, spirituality, and depressive symptoms in primary care house officers. Ambul Pediatr. 2006;6(2):84–90. doi: 10.1016/j.ambp.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 38.Demir F, Ay P, Erbaş M, Ozdil M, Yaşar E. The prevalence of depression and its associated factors among resident doctors working in a training hospital in Istanbul [in Turkish]. Turk Psikiyatri Derg. 2007;18(1):31–37. [PubMed] [Google Scholar]
- 39.Hasanović M, Herenda S. Post traumatic stress disorder, depression and anxiety among family medicine residents after 1992-95 war in Bosnia and Herzegovina. Psychiatr Danub. 2008;20(3):277–285. [PubMed] [Google Scholar]
- 40.Sakata Y, Wada K, Tsutsumi A, et al. Effort-reward imbalance and depression in Japanese medical residents. J Occup Health. 2008;50(6):498–504. doi: 10.1539/joh.l8043. [DOI] [PubMed] [Google Scholar]
- 41.Sánchez MJB, Islas CLR, Escobar, Rico LES. Symptoms of anxiety and depression in resident physicians at high risk of stress. Psiquiatr Biol. 2008;15(5):147–152. [Google Scholar]
- 42.Goebert D, Thompson D, Takeshita J, et al. Depressive symptoms in medical students and residents: a multischool study. Acad Med. 2009;84(2):236–241. doi: 10.1097/ACM.0b013e31819391bb. [DOI] [PubMed] [Google Scholar]
- 43.Waldman SV, Diez JCL, Arazi HC, Linetzky B, Guinjoan S, Grancelli H. Burnout, perceived stress, and depression among cardiology residents in Argentina. Acad Psychiatry. 2009;33(4):296–301. doi: 10.1176/appi.ap.33.4.296. [DOI] [PubMed] [Google Scholar]
- 44.Lam TP, Wong JGWS, Ip MSM, Lam KF, Pang SL. Psychological well-being of interns in Hong Kong: what causes them stress and what helps them. Med Teach. 2010;32(3):e120–e126. doi: 10.3109/01421590903449894. [DOI] [PubMed] [Google Scholar]
- 45.Costa EF, Santana YS, Santos AT, Martins LA, Melo EV, Andrade TM. Depressive symptoms among medical intern students in a Brazilian public university [in Portuguese]. Rev Assoc Médica Bras. 2012;58(1):53–59. [PubMed] [Google Scholar]
- 46.Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–395. [PubMed] [Google Scholar]
- 47.de Oliveira GS, Jr, Chang R, Fitzgerald PC, et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg. 2013;117(1):182–193. doi: 10.1213/ANE.0b013e3182917da9. [DOI] [PubMed] [Google Scholar]
- 48.Al-Ghafri G, Al-Sinawi H, Al-Muniri A, et al. Prevalence of depressive symptoms as elicited by Patient Health Questionnaire (PHQ-9) among medical trainees in Oman. Asian J Psychiatr. 2014;8:59–62. doi: 10.1016/j.ajp.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 49.Dyrbye LN, West CP, Satele D, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 50.Stoesser K, Cobb NM. Self-treatment and informal treatment for depression among resident physicians. Fam Med. 2014;46(10):797–801. [PubMed] [Google Scholar]
- 51.Al-Maddah EM, Al-Dabal BK, Khalil MS. Prevalence of sleep deprivation and relation with depressive symptoms among medical residents in King Fahd University Hospital, Saudi Arabia. Sultan Qaboos Univ Med J. 2015;15(1):e78–e84. [PMC free article] [PubMed] [Google Scholar]
- 52.Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med. 2015;20(3):353–362. doi: 10.1080/13548506.2014.936889. [DOI] [PubMed] [Google Scholar]
- 53.Ford CV, Wentz DK. The internship year: a study of sleep, mood states, and psychophysiologic parameters. South Med J. 1984;77(11):1435–1442. doi: 10.1097/00007611-198411000-00019. [DOI] [PubMed] [Google Scholar]
- 54.Reuben DB. Depressive symptoms in medical house officers: effects of level of training and work rotation. Arch Intern Med. 1985;145(2):286–288. [PubMed] [Google Scholar]
- 55.Revicki DA, Gallery ME, Whitley TW, Allison EJ. Impact of work environment characteristics on work-related stress and depression in emergency medicine residents: a longitudinal study. J Community Appl Soc Psychol. 1993;3(4):273–284. [Google Scholar]
- 56.Gopal R, Glasheen JJ, Miyoshi TJ, Prochazka AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005;165(22):2595–2600. doi: 10.1001/archinte.165.22.2595. [DOI] [PubMed] [Google Scholar]
- 57.Katz ED, Sharp L, Ferguson E. Depression among emergency medicine residents over an academic year. Acad Emerg Med. 2006;13(3):284–287. doi: 10.1197/j.aem.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 58.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 59.Wada K, Sakata Y, Fujino Y, et al. The association of needlestick injury with depressive symptoms among first-year medical residents in Japan. Ind Health. 2007;45(6):750–755. doi: 10.2486/indhealth.45.750. [DOI] [PubMed] [Google Scholar]
- 60.Landrigan CP, Fahrenkopf AM, Lewin D, et al. Effects of the Accreditation Council for Graduate Medical Education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 61.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Anxiety and depression in residents: results of a Swiss longitudinal study [in German]. Z Psychosom Med Psychother. 2009;55(1):37–50. doi: 10.13109/zptm.2009.55.1.37. [DOI] [PubMed] [Google Scholar]
- 62.Campbell J, Prochazka AV, Yamashita T, Gopal R. Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med. 2010;85(10):1630–1634. doi: 10.1097/ACM.0b013e3181f0c4e7. [DOI] [PubMed] [Google Scholar]
- 63.Beckman TJ, Reed DA, Shanafelt TD, West CP. Resident physician well-being and assessments of their knowledge and clinical performance. J Gen Intern Med. 2012;27(3):325–330. doi: 10.1007/s11606-011-1891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weigl M, Hornung S, Petru R, Glaser J, Angerer P. Depressive symptoms in junior doctors: a follow-up study on work-related determinants. Int Arch Occup Environ Health. 2012;85(5):559–570. doi: 10.1007/s00420-011-0706-8. [DOI] [PubMed] [Google Scholar]
- 65.West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138–1144. doi: 10.1016/j.mayocp.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–662. doi: 10.1001/jamainternmed.2013.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Velásquez-Pérez L, Colin-Piana R, González-González M. Coping with medical residency: depression burnout [in Spanish]. Gac Med Mex. 2013;149(2):183–195. [PubMed] [Google Scholar]
- 68.Kleim B, Thörn HA, Ehlert U. Positive interpretation bias predicts well-being in medical interns. Front Psychol. 2014;5:640. doi: 10.3389/fpsyg.2014.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cubero DIG, Fumis RRL, de Sá TH, et al. Burnout in medical oncology fellows: a prospective multicenter cohort study in Brazilian institutions. J Cancer Educ. doi: 10.1007/s13187-015-0850-z. published online May 9, 2015 doi: 10.1007/s13187-015-0850-z. [DOI] [PubMed] [Google Scholar]
- 70.Ito M, Seo E, Ogawa R, Sanuki M, Maeno T, Maeno T. Can we predict future depression in residents before the start of clinical training? Med Educ. 2015;49(2):215–223. doi: 10.1111/medu.12620. [DOI] [PubMed] [Google Scholar]
- 71.Jiménez-López JL, Arenas-Osuna J, Angeles-Garay U. Depression, anxiety and suicide risk symptoms among medical residents over an academic year [in Spanish]. Rev Med Inst Mex Seguro Soc. 2015;53(1):20–28. [PubMed] [Google Scholar]
- 72.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 73.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 74.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 75.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Biggs JT, Wylie LT, Ziegler VE. Validity of the Zung Self-rating Depression Scale. Br J Psychiatry. 1978;132:381–385. doi: 10.1192/bjp.132.4.381. [DOI] [PubMed] [Google Scholar]
- 77.Baer L, Jacobs DG, Meszler-Reizes J, et al. Development of a brief screening instrument: the HANDS. Psychother Psychosom. 2000;69(1):35–41. doi: 10.1159/000012364. [DOI] [PubMed] [Google Scholar]
- 78.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 80.Spielberger CD. Manual for the State-Trait Personality Inventory (Form Y) Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- 81.Wilkinson MJB, Barczak P. Psychiatric screening in general practice: comparison of the general health questionnaire and the hospital anxiety depression scale. J R Coll Gen Pract. 1988;38(312):311–313. [PMC free article] [PubMed] [Google Scholar]
- 82.Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther. 1997;35(1):79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- 83.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 84.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190((7)(suppl)):S54–S60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 85.Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. Am J Psychiatry. 1998;155(1):4–11. doi: 10.1176/ajp.155.1.4. [DOI] [PubMed] [Google Scholar]
- 86.Williams JW, Jr, Pignone M, Ramirez G, Perez Stellato C. Identifying depression in primary care: a literature synthesis of case-finding instruments. Gen Hosp Psychiatry. 2002;24(4):225–237. doi: 10.1016/s0163-8343(02)00195-0. [DOI] [PubMed] [Google Scholar]
- 87.Myers M. On the importance of anonymity in surveying medical student depression. Acad Psychiatry. 2003;27(1):19–20. doi: 10.1176/appi.ap.27.1.19. [DOI] [PubMed] [Google Scholar]
- 88.Accreditation Council for Graduate Medical Education. Report of the ACGME Work Group on Resident Duty Hours. 2002 Jun 11; [Google Scholar]
- 89. [November 6, 2015];Organisation of working time: Council Directive 93/104/EC. http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:31993L0104.
- 90.Final report on doctor work reform. [November 6, 2015];Steering Committee on Doctor Work Hour, Hospital Authority. https://www.ha.org.hk/haho/ho/hesd/FinalReportonDWR_2009_10_Full_Version.pdf.
- 91.Daskivich TJ, Jardine DA, Tseng J, et al. Promotion of wellness and mental health awareness among physicians in training: perspective of a national, multispecialty panel of residents and fellows. J Grad Med Educ. 2015;7(1):143–147. doi: 10.4300/JGME-07-01-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.