Abstract
Objective
Evaluate over-prescribing of antidepressant medication for minimal or mild depression.
Method
Electronic records data from four large healthcare systems identified outpatients aged 18 or older starting a new episode of antidepressant treatment with an ICD9 diagnosis of depressive disorder (296.2, 296.3, 311, or 300.4). PHQ9 depression severity scores at time of treatment initiation were used to examine the distribution of baseline severity and the association between baseline severity and patients' demographic and clinical characteristics.
Results
Of 19,751 adults beginning treatment in 2011, baseline PHQ9 scores were available for 7051. In those with a baseline score, 85% reported moderate or severe symptoms (PHQ9 score 10 or more), 12% reported mild symptoms (PHQ score 5 to 9), and 3% reported minimal symptoms (PHQ9 score less than 5). The proportion reporting minimal or mild symptoms when starting treatment increased with age, ranging from 11% in those under age 30 to 26% in those aged 65 and older. The proportion with minimal or mild symptoms was also moderately higher among patients living in wealthier neighborhoods and those treated by psychiatrists. Nevertheless, across all subgroups defined by sex, race/ethnicity, prescriber specialty, and treatment history, the proportions with minimal or mild symptoms did not exceed 18%. Secondary analyses, including weighting and subgroup analyses, found no evidence that estimates of baseline severity were biased by missing PHQ9 scores.
Conclusions
In these health systems, prescribing of antidepressant medication for minimal or mild depression is much less common than suggested by previous reports. Given that this practice may sometimes be clinically appropriate, our findings indicate that over-prescribing of antidepressants for mild depression is not a significant public health concern.
Use of antidepressants has increased dramatically over the past 20 years in the US and in other higher-income countries (1–5). Approximately 10% of US adults now fill one or more antidepressant prescriptions in any calendar year (3). Antidepressants prescribed by primary care physicians account for the majority of this increase (2, 3).
Increasing rates of antidepressant treatment have raised concerns about over-prescribing to patients with less severe depression (6, 7). Community surveys suggest that the rates of antidepressant use may now exceed the prevalence of depression, especially among older adults (8). In the 2003 Collaborative Psychiatric Epidemiologic Surveys, 26% of recent antidepressant users did not meet diagnostic criteria for any lifetime psychiatric diagnosis according to a structured research interview (9). In the 2010 National Survey on Drug Use and Health, only 44% of respondents using antidepressants reported experiencing a major depressive episode during the past year (10). These findings were interpreted as evidence for significant diagnostic inflation (11) and attracted significant public attention (12, 13).
Cross-sectional community surveys, however, may not accurately assess indications for antidepressant treatment. While recall of depression severity is reasonably accurate over several weeks (14), more remote episodes of depression are often under-reported (15–18). If current antidepressant users were asked about past depression, failure to recall prior episodes would over-estimate the proportion without a clear history of significant depression.
Here we use data from four large healthcare systems to examine severity of depression at initiation of antidepressant treatment. We take advantage of the increasing use of standard depression severity measures to examine how often outpatients starting antidepressant treatment reported only minimal or mild symptoms at the time of the initial prescription. These ratings should be less subject to error or bias than would previous studies (9, 10) relying on long-term recall.
METHODS
Data are drawn from the Mental Health Research Network (MHRN), a consortium of public-domain research centers affiliated with 11 large not-for-profit integrated healthcare systems. Each of these systems provides comprehensive care (including general medical and specialty mental health care) to a defined population of members or patients. Across these systems, electronic medical records, insurance claims, and other administrative data systems have been organized in a Virtual Data Warehouse to facilitate population-based research (19). Protected health information remains at each member health system, but common data definitions and formats facilitate sharing of de-identified data for research. Institutional Review Boards and privacy boards at each health system approved all study procedures and granted waivers of consent for this research use of de-identified records data.
The four MHRN healthcare systems contributing data to this study include Group Health Cooperative, HealthPartners, Kaiser Permanente Colorado, and Kaiser Permanente Hawaii. These four systems serve a combined population of approximately 2 million members/patients in the states of Washington, Idaho, Minnesota, Colorado, and Hawaii. Members are enrolled through employer-sponsored insurance, individual insurance plans, and capitated Medicare and Medicaid programs and are generally representative of each system's regional population. In 2011, the 10.2% of all adult members of these healthcare systems filled one or more antidepressant prescriptions, similar to national rates (3). While Group Health and HealthPartners are mixed-model healthcare systems (providing care through both internal or group-model providers and external or network-model providers), this sample was limited to patients receiving prescriptions from internal providers to ensure availability of complete electronic medical records.
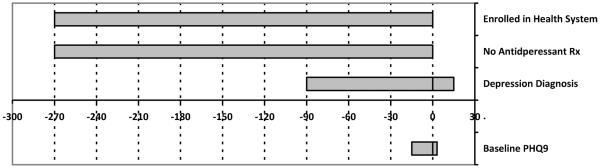
The study sample included all adult members filling a new outpatient antidepressant prescription from an internal healthcare system provider between 1/1/2011 and 12/31/2011. Eligible antidepressant medications included all drugs approved by the US Food and Drug Administration for treatment of major depression, excluding trazodone (more often prescribed for insomnia). A list of included medications and corresponding National Drug Codes is available at www.mhresearchnetwork.org. A new episode of antidepressant treatment was defined by an interval of at least 270 days since the last filled antidepressant prescription. While this interval is longer than that used to define new prescriptions in NCQA/HEDIS measures (20) and in some of our previous research (21, 22), it is based on two findings in records data from MHRN health systems. First, analyses of the frequency distributions of intervals between filled antidepressant prescriptions across health systems found that the rate of prescription fills remained elevated above the background rate for approximately 270 days. Second, review of full text medical records for visits between antidepressant fills found that 50% of visit notes reported continued medication use 180 days after the prior fill, with this rated dropping to 25% by 270 days. Details of both of these analyses are available as an online appendix (see eAppendix). The study sample was limited to those with a recorded diagnosis of any depressive disorder (ICD9 diagnosis 296.2, 296.3, 300.4, or 311) in the interval starting 90 days before the index prescription and ending 15 days after. In these healthcare systems, approximately 60% of adults receiving antidepressant treatment have a recorded diagnosis of depressive disorder, with most of the remainder having recorded diagnoses of anxiety disorders or attention deficit disorders (23). Patients with any diagnosis of bipolar disorder or psychotic disorder prior to the index prescription were excluded. To ensure availability of records data to assess inclusion and exclusion criteria, the sample was limited to those continuously enrolled in the participating healthcare systems for at least 270 days prior to the index prescription. These criteria are illustrated in Figure 1.
Figure 1.
Criteria defining a new antidepressant treatment episode included: at least 270 days of enrollment in the health system, at least 270 days since the most recent antidepressant prescription fill, and a recorded depression diagnosis in the interval from 90 days before to 15 days after the index prescription. The inclusion window for baseline PHQ9 severity measures extended from 15 days before to 3 days after the index prescription.
During the study period, participating healthcare systems all recommended use of the PHQ9 (24–26) for initial assessment of depression severity and at all follow-up visits for depression care. Procedures for use of the PHQ9 varied between health systems and between clinics within health systems. In general medical clinics, use of the PHQ9 depended on practice teams' implementation of this recommended practice. Questionnaires could be administered prior to the visit by a nurse or medical assistant (if depression was identified in advance) or by the physician during the visit. Procedures also varied across mental health specialty clinics, with some clinics routinely administered the PHQ9 prior to every outpatient visit and some relying on providers to administer it during visits as clinically indicated. As described below, actual adherence to recommended use of the PHQ9 was variable.
Electronic medical records and healthcare system administrative databases were used to identify the specialty of the prescribing physician and the following patient characteristics: sex, age at initiation of antidepressant treatment, race/ethnicity, and neighborhood income.
For these analyses, we defined a baseline PHQ9 score as any measurement in the interval between 15 days prior to and 3 days after the index prescription. For patients with more than one PHQ9 record in this interval, the PHQ9 score recorded prior to and closest to the index prescription date was considered the baseline value.
Descriptive analyses examined the availability of baseline PHQ9 scores and distributions of scores across healthcare systems and patient subgroups. Severity of depression according to PHQ9 score was categorized as 0 to 4 (minimal depression), 5 to 9 (mild depression), 10 to 14 (moderate depression), 15 to 19 (moderately severe depression), and 20 or more (severe depression) (26). Predictors of a baseline PHQ9 score being recorded in the medical record and predictors of that baseline PHQ9 score being less than 10 were examined using logistic regression. To account for possible selection bias due to missing baseline PHQ9 scores, weighted distributions of baseline scores were calculated using inverse probability weights (27, 28) based on all covariate information listed in Table 1.
Table 1.
Proportion of outpatients starting antidepressant treatment with and without a recorded PHQ9 depression score at baseline (Odds Ratios from logistic model including all covariates in table).
| No Baseline PHQ9 | Yes Baseline PHQ9 | Odds Ratio for Yes (95% CI) | |
|---|---|---|---|
| Sex | |||
| Female | 8555 (65%) | 4693 (35%) | Reference |
| Male | 4145 (64%) | 2358 (36%) | 1.18 (1.10 – 1.26) |
| Age | |||
| 18–29 | 2081 (56%) | 1624 (44%) | Reference |
| 30–44 | 3257 (62%) | 2025 (38%) | 0.74 (0.67 – 0.81) |
| 45–64 | 4828 (66%) | 2439 (38%) | 0.57 (0.52 – 0.62) |
| 65+ | 2534 (72%) | 963 (28%) | 0.37 (0.34 – 0.42) |
| Race / Ethnicity | |||
| Non-Hispanic White | 7343 (59%) | 5089 (41%) | Reference |
| Asian | 516 (63%) | 303 (37%) | 0.75 (0.64 – 0.87) |
| Non-Hispanic Black | 345 (51%) | 325 (49%) | 1.28 (1.09 – 1.51) |
| Hispanic | 941 (65%) | 512 (35%) | 0.72 (0.64 – 0.82) |
| Native Hawaiian/Pacific Islander | 135 (69%) | 60 (31%) | 0.52 (0.38 – 0.72) |
| Native American / Alaskan Native | 47 (51%) | 45 (49%) | 1.35 (0.88 – 2.07) |
| Mixed Race | 421 (65%) | 230 (35%) | 0.65 (0.55 – 0.74) |
| Other or Unknown | 2952 (86%) | 487 (14%) | 0.27 (0.25 – 0.31) |
| Neighborhood Income | |||
| >= $25,0000 | 11292 (65%) | 6099 (35%) | Reference |
| < $25,000 | 1408 (60%) | 952 (40%) | 1.36 (1.23 – 1.50) |
| Prescriber Specialty | |||
| Primary Care or Other | 9360 (62%) | 5639 (38%) | Reference |
| Psychiatry | 3340 (70%) | 1412 (30%) | 0.48 (0.44 – 0.52) |
| Prescriber Volume | |||
| 1 to 5 patients per year | 3789 (85%) | 691 (15%) | Reference |
| 6 to 10 | 2001 (66%) | 1037 (34%) | 2.54 (2.26 – 2.84) |
| 11 to 15 | 1760 (54%) | 1486 (46%) | 3.97 (3.56 – 4.44) |
| 16 to 20 | 1495 (54%) | 1254 (46%) | 3.97 (3.54 – 4.46) |
| 21 or more | 3655 (59%) | 2583 (41%) | 4.39 (3.95 – 4.87) |
RESULTS
Healthcare system records identified 19,751 patients aged 18 and over with an eligible episode of antidepressant treatment in 2011. This included 7141 (36%) initial prescriptions for citalopram, 4427 (22%) for fluoxetine, 2838 (14%) for sertraline, and 2361 (12.%) for bupropion. No other single medication accounted for more than 5% of initial prescriptions. 7051 (36%) episodes had a baseline PHQ9 score recorded in the electronic medical record. As shown in Table 1, baseline PHQ9 scores were recorded slightly more often among men than women. The proportion with a recorded baseline depression severity score declined progressively with age, decreasing from 44% in younger patients to only 28% in those 65 and older. Recording of a baseline severity score varied moderately across racial/ethnic groups (higher among Non-Hispanic Blacks and Native Americans, lower among Hispanics, Asians, and Native Hawaiians). Baselines scores were recorded much less often in those with no recorded race or ethnicity. Presence of a baseline PHQ9 score was moderately higher among patients residing in economically disadvantaged neighborhoods and lower among patients treated by psychiatrists. The strongest predictor of having a recorded baseline severity score was the prescribing provider's number of patients starting antidepressant treatment for depression during the study year. The proportion with a baseline score increased from approximately 15% in those treating 5 or fewer patients to over 40% in those treating 11 or more patients.
Among those with a baseline PHQ9 score, 5988 or 85% (95% CI 84% to 86%) reported a score of 10 or more (indicating moderate or severe symptoms). Approximately 12% (95% CI 12% to 13%) had baseline scores between 5 and 9 (indicating mild symptoms of depression) and approximately 3% (95% CI 2% to 3%) had baseline scores less than 5 (indicating minimal symptoms of depression). As shown in Table 2, the distribution of baseline PHQ9 scores did vary across the four healthcare systems more than expected by chance (Chi square = 72.1, df = 12, p<.0001), but the overall pattern was similar across all four systems. The proportion with minimal symptoms of depression ranged from 2% to 4% and the proportion with mild symptoms of depression ranged from 11% to 21%.
Table 2.
Distribution of baseline PHQ9 depression scores among outpatients starting antidepressant treatment in four healthcare systems.
| 0 to 4 | 5 to 9 | 10 to 14 | 15 to 19 | 20 or more | |
|---|---|---|---|---|---|
| Group Health Coop. | 102 (3%) | 434 (11%) | 1139 (28%) | 1354 (34%) | 987 (25%) |
| HealthPartners | 41 (4%) | 158 (15%) | 319 (30%) | 310 (30%) | 209 (20%) |
| KP Colorado | 29 (2%) | 222 (13%) | 517 (31%) | 540 (32%) | 385 (23%) |
| KP Hawaii | 12 (4%) | 65 (21%) | 62 (20%) | 98 (32%) | 68 (22%) |
| Total | 184 (3%) | 879 (12%) | 2037 (29%) | 2302 (33%) | 1649 (23%) |
Table 3 shows the proportion of patients with baseline PHQ9 scores less than 10 for subgroups defined by sex, age, race/ethnicity, neighborhood income, and prescriber characteristics. The proportion with a low baseline severity score increased steadily with age – from approximately 11% among young adults to 26% among those aged 65 or older. The proportion with minimal or mild symptoms was lower for all minority racial/ethnic groups compared to Non-Hispanic Whites, but odds ratios for individual racial/ethnic groups (compared to Non-Hispanic Whites) did not differ significantly from 1 after adjustment for other covariates. Low baseline PHQ9 scores were less common among patients residing in economically disadvantaged neighborhoods and more common among those treated by psychiatrists. The proportion with baseline PHQ9 score less than 10 did not differ according the prescribing provider's number of patients treated during the study period.
Table 3.
Proportion of outpatients starting antidepressant treatment with baseline PHQ9 depression scores above or below threshold of 10 (Odds Ratios from logistic model including all covariates in table)
| Baseline PHQ9 <10 | Baseline PHQ9 >=10 | Odds Ratio for <10 (95% CI) | |
|---|---|---|---|
| Sex | |||
| Female | 690 (15%) | 4003 (85%) | Reference |
| Male | 373 (16%) | 1985 (84%) | 1.03 (0.89 – 1.18) |
| Age | |||
| 18–29 | 179 (11%) | 1445 (89%) | Reference |
| 30–44 | 274 (14%) | 1751 (86%) | 1.27 (1.04 – 1.56) |
| 45–64 | 360 (15%) | 2079 (85%) | 1.39 (1.14 – 1.68) |
| 65+ | 250 (26%) | 713 (74%) | 2.76 (2.22 – 3.42) |
| Race / Ethnicity | |||
| Non-Hispanic White | 804 (16%) | 4825 (84%) | Reference |
| Asian | 41 (14%) | 262 (86%) | 0.86 (0.61 – 1.21) |
| African American | 35 (11%) | 290 (89%) | 0.71 (0.50 – 1.02) |
| Hispanic | 73 (14%) | 439 (86%) | 0.95 (0.74 – 1.24) |
| Hawaiian/Pacific Islander | 4 (7%) | 56 (93%) | 0.44 (0.16 – 1.21) |
| Native American | 3 (7%) | 42 (93%) | 0.39 (0.12 – 1.28) |
| More than one | 33 (14%) | 197 (86%) | 1.01 (0.69 – 1.47) |
| Unknown | 70 (14%) | 417 (86%) | 0.98 (0.75 – 1.28) |
| Neighborhood Income | |||
| >= $25,0000 | 950 (16%) | 5149 (84%) | Reference |
| < $25,000 | 113 (12%) | 839 (88%) | 0.81 (0.68 – 0.98) |
| Prescriber Specialty | |||
| Primary Care or Other | 829 (15%) | 4810 (85%) | Reference |
| Psychiatry | 234 (17%) | 1178 (83%) | 1.16 (1.03 – 1.45) |
| Prescriber Volume | |||
| 1 to 5 patients per year | 94 (14%) | 597 (86%) | Reference |
| 6 to 10 | 158 (15%) | 869 (85%) | 1.10 (0.84 – 1.46) |
| 11 to 15 | 241 (16%) | 1245 (84%) | 1.16 (0.90 – 1.51) |
| 16 to 20 | 185 (15%) | 2198 (85%) | 1.04 (0.79 – 1.36) |
| 21 or more | 1063 (15%) | 5988 (85%) | 1.01 (0.79 – 1.30) |
Two secondary analyses examined the possibility that missing baseline PHQ9 scores could bias estimates of baseline depression severity. First, the distribution of baseline PHQ9 scores was recalculated after weighting each observation according to the inverse probability of PHQ9 score availability (27, 28) for each combination of predictors in Table 1. Second, analyses were limited to the subgroup patients treated by prescribers who recorded baseline PHQ9 scores for at least 75% of patients starting antidepressant treatment in the study year. As shown in Table 4, the distribution of baseline depression severity scores using either of these methods was essentially identical to the unweighted results in the full sample.
Table 4.
Secondary analyses examining possible bias due to missing baseline PHQ scores
| 0 to 4 | 5 to 9 | 10 to 14 | 15 to 19 | 20 or more | |
|---|---|---|---|---|---|
| Full sample, unweighted | 184 (3%) | 879 (12%) | 2037 (29%) | 2302 (33%) | 1649 (23%) |
| Full sample, weighted* | 176 (3%) | 840 (12%) | 2032 (29%) | 2342 (33%) | 1661 (24%) |
| Limited to providers using PHQ9 >=75%** | 66 (3%) | 278 (11%) | 762 (29%) | 870 (34%) | 615 (24%) |
Notes:
Weighted according to inverse probability of baseline PHQ availability according to patients' sex, age, race/ethnicity, and neighborhood income as well as prescribing provider's specialty and number of patients treated for depression
Limited to patients treated by prescribing providers for whom baseline PHQ9 was recorded for 75% or more of patients in study sample
DISCUSSION
Our data do not support the prior claim (10) that the majority of patients treated with antidepressants have not experienced depression severe enough to warrant pharmacotherapy. In this sample, approximately 85% of adult outpatients starting antidepressants reported moderate or severe symptoms at the time of the initial prescription. This proportion was generally similar across healthcare systems.
Consistent with previous reports (8, 10), we did find that the proportion of antidepressant users reporting mild symptoms was greater in older patients: 26% of patients 65 and older compared to approximately 13% in those under age 65. Others have suggested that traditional symptoms scales or diagnostic assessments may under-represent depression in older adults who may more often present with somatic symptoms or cognitive complaints (29). Alternatively, older adults' more frequent contact with health care may result in a higher likelihood that less severe depression will be recognized and treated.
Lower baseline depression scores were more common in patients living in more economically advantaged neighborhoods. This pattern could reflect either a general tendency toward less severe depression in more advantaged patients or a tendency for more advantaged patients with mild depression to more often seek or receive treatment. Our data also suggest a higher threshold for prescribing of antidepressants to members of racial/ethnic minority groups. This could reflect a bias in providers' decision processes or a difference in patients' treatment preferences. Previous research does suggest that African American and Hispanic patients are less likely than Non-Hispanic whites to prefer antidepressants for treatment of depression (30). Our data cannot distinguish between differences due to providers' biases and differences due to patients' preferences. It is also possible that the PHQ9 may not accurately reflect severity of depression in some racial/ethnic groups, but previous research supports the validity of this measure across a wide range of language, culture, and race/ethnicity (24, 26).
Lower baseline depression scores were also more common among patients treated by psychiatrists. This may reflect a lower threshold for prescribing among psychiatrists or the fact that patients seen in specialty settings may more often present with other indications for treatment (such as comorbid psychiatric conditions or a past history of severe depression). Our data do not support concerns that increasing antidepressant prescribing by primary care physicians has led to diagnostic inflation or more frequent prescribing for mild depression.
It is possible that patterns of antidepressant prescribing in these healthcare systems differ from those in other practice settings. Practice guidelines in these systems all recommended routine use of the PHQ9 for initial evaluation of depression. Guidelines in all systems did not recommend prescription of antidepressants for minimal or mild symptoms (PHQ9 scores of 9 or less) and also advised that medication is not always indicated for moderate depression (PHQ9 scores between 10 and 14). Those guidelines recommended either pharmacotherapy or psychotherapy as initial treatment for patients with moderate or moderately severe depression (PHQ9 scores between 10 and 19) and combined pharmacotherapy and psychotherapy for those with more severe or chronic depression. Prescription of antidepressants for minimal or mild symptoms of depression could be more common in practice settings without these standard assessment procedures or practice guidelines. Nevertheless, the overall rate of antidepressant use in these healthcare systems was generally consistent with the rate in the US population. And use of standard measures, such as the PHQ9, to guide depression treatment is increasingly common in both primary care and specialty mental health practice (31, 32). Furthermore, guideline recommendations regarding antidepressant treatment in these healthcare systems followed consensus recommendations, such as those of the Institute for Clinical Systems Improvement (33).
Baseline depression severity scores were available for only 36% of patients starting antidepressant treatment, and this could bias our estimates of baseline severity. Availability of baseline severity scores was related to patient age, race/ethnicity, and neighborhood income (Table 1), but weighting for those predictors of missing baseline severity data had no meaningful effect on our estimates of baseline severity (Table 4). Availability of baseline severity scores was much more strongly related to provider characteristics (Table 1), and limiting our analyses to providers with high rates of PHQ availability also had no meaningful effect on estimates of baseline severity (Table 4). Overall, we do not find evidence that missing baseline PHQ9 scores biased our primary finding, that only 15% of outpatients starting antidepressant treatment had only minimal or mild symptoms at the time of the initial prescription.
We believe these practice-based data more accurately assess severity of depression at initiation of treatment than do retrospective data from community surveys. As discussed above, longitudinal studies suggest that past episodes of depression are often not recalled (15, 18). Furthermore, those who are not depressed at the time of interview are less likely to recall prior symptoms of depression (14). Consequently, those who experience remission of depression while taking medication would be less likely to recall past symptoms of depression. Given this bias in recall, what appears to be unnecessary or inappropriate prescription of antidepressants for mild depression may actually represent successful treatment.
Several recent meta-analyses of placebo-controlled trials have attempted to identify a depression severity threshold for antidepressant prescribing – using varying patient samples and analytic methods (34–38). These analyses have generally agreed regarding benefit of antidepressants for patients with severe depression and the absence of clear benefit for patients with mild depression. Conclusions have been mixed regarding a specific benefit of antidepressants for patients with moderate depression. Furthermore, the category of moderate depression is heterogeneous, including some with a high likelihood of spontaneous improvement and some for whom improvement without specific treatment is less likely.
We should acknowledge, however, that prescribing of antidepressants to patients with mild symptoms of depression may sometimes be appropriate. While every patient in the sample did receive a diagnosis of depressive disorder, it is possible that medication was prescribed primarily to address some other indication, such as co-occurring anxiety disorder. Standardized assessments, such as the PHQ9, may not be an accurate measure of depression severity or depression-related impairment for every single patient. Some patients in our sample classified as having minimal or mild depression by the PHQ9 could have indicated more severe symptoms to the prescribing physician during the visit. For a patient experiencing a relapse of depression following successful prior treatment with medication, reinitiating antidepressants when mild symptoms re-appear (before more severe recurrence or relapse) would certainly be a reasonable practice. Our data do not allow us to identify these specific clinical decisions. Nevertheless, it is likely that these reasonable practices account for at least some of 15% of patients initiating antidepressant treatment for whom PHQ9 scores indicated only minimal or mild depression.
The severity threshold for prescribing antidepressants is certainly not a bright line. Any attempt to evaluate the appropriateness of prescribing must allow for both the imperfection of standardized measures and the variability in individual patients' clinical histories. With those allowances, our finding that approximately 15% of outpatients starting antidepressant treatment reported mild or minimal depression does not seem particularly surprising or concerning. Data from these four healthcare systems do not indicate that over-prescription of antidepressants for minimal or mild depression is a significant public health concern.
CLINICAL POINTS.
Community antidepressant prescribing is usually consistent with guideline recommendations, with only a small proportion of patients starting treatment having minimal or mild symptoms.
Psychiatrists may be more likely than primary care physicians to start or re-start antidepressants when symptoms of depression are mild.
ACKNOWLEDGEMENTS
The Mental Health Research Network is supported by a cooperative agreement (U19MH092201) with the National Institute of Mental Health. The funder did not participate in data analyses, interpretation of results, or preparation of this manuscript. This research made use of the HMO Research Network (HMORN) Virtual Data Warehouse (VDW), a distributed data model that facilitates multi-site research while protecting patient privacy and proprietary health practice information. Many groups have contributed to the development of this resource over time. See www.hmorn.org for a list of acknowledgements or to learn more about the HMORN VDW.
Drs. Simon and Penfold have received salary support from research grants by Bristol Myers Squibb and Otsuka Pharmaceuticals to Group Health Research Institute. Dr. Shortreed has received salary support from research grants by Johnson&Johnson, Pfizer and Bristol Myers Squibb to Group Health Research Institute.
REFERENCES
- 1.Kessler R, Demier O, Frank R, Olfson M, Pincus H, Walters E, et al. Prevalence and treatment of mental disorders: 1990 to 2003. N Engl J Med. 2005;352:2515–23. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mojtabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. J Clin Psychiatry. 2008;69(7):1064–74. doi: 10.4088/jcp.v69n0704. Epub 2008/04/11. [DOI] [PubMed] [Google Scholar]
- 3.Mojtabai R, Olfson M. National trends in long-term use of antidepressant medications: results from the US National Health and Nutrition Examination Survey. J Clin Psychiatry. 2013 doi: 10.4088/JCP.13m08443. Epub 2013/12/19. [DOI] [PubMed] [Google Scholar]
- 4.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–56. doi: 10.1001/archgenpsychiatry.2009.81. Epub 2009/08/05. [DOI] [PubMed] [Google Scholar]
- 5.Moore M, Yuen HM, Dunn N, Mullee MA, Maskell J, Kendrick T. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. Bmj. 2009;339:b3999. doi: 10.1136/bmj.b3999. Epub 2009/10/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spence D. Are antidepressants overprescribed? Yes. Bmj. 2013;346:f191. doi: 10.1136/bmj.f191. Epub 2013/01/24. [DOI] [PubMed] [Google Scholar]
- 7.Middleton H, Moncrieff J. 'They won't do any harm and might do some good': time to think again on the use of antidepressants? Br J Gen Pract. 2011;61(582):47–9. doi: 10.3399/bjgp11X548983. Epub 2011/03/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hollingworth SA, Burgess PM, Whiteford HA. Affective and anxiety disorders: prevalence, treatment and antidepressant medication use. Aust N Z J Psychiatry. 2010;44(6):513–9. doi: 10.3109/00048670903555138. Epub 2010/05/21. [DOI] [PubMed] [Google Scholar]
- 9.Pagura J, Katz LY, Mojtabai R, Druss BG, Cox B, Sareen J. Antidepressant use in the absence of common mental disorders in the general population. J Clin Psychiatry. 2011;72(4):494–501. doi: 10.4088/JCP.09m05776blu. Epub 2011/02/08. [DOI] [PubMed] [Google Scholar]
- 10.Mojtabai R. Clinician-identified depression in community settings: concordance with structured-interview diagnoses. Psychother Psychosom. 2013;82(3):161–9. doi: 10.1159/000345968. Epub 2013/04/04. [DOI] [PubMed] [Google Scholar]
- 11.Batstra L, Frances A. Diagnostic inflation: causes and a suggested cure. J Nerv Ment Dis. 2012;200(6):474–9. doi: 10.1097/NMD.0b013e318257c4a2. Epub 2012/06/02. [DOI] [PubMed] [Google Scholar]
- 12.Rabin RC. New York Times. Aug 13, 2013. A glut of antidepressants? 2013;Sect. D. [Google Scholar]
- 13.Ulene V. LA Times. May 11, 2009. Antidepressants: The right people aren't always getting them. 2009. [Google Scholar]
- 14.Rutter C, Simon G. A Bayesian method for estimating the accuracy of recalled depression. Applied Statistics. 2004;53:341–53. [Google Scholar]
- 15.Simon GE, VonKorff M. Recall of psychiatric history in cross-sectional surveys: Implications for epidemiologic research. Epidemiol Rev. 1995;17:221–7. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- 16.Patten SB, Williams JV, Lavorato DH, Bulloch AG, D'Arcy C, Streiner DL. Recall of recent and more remote depressive episodes in a prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-011-0385-5. Epub 2011/05/03. [DOI] [PubMed] [Google Scholar]
- 17.Wells JE, Horwood LJ. How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychol Med. 2004;34(6):1001–11. doi: 10.1017/s0033291703001843. Epub 2004/11/24. [DOI] [PubMed] [Google Scholar]
- 18.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of Reports of Lifetime Mental and Physical Disorders: Results From the Baltimore Epidemiological Catchment Area Study. JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2013.3579. Epub 2014/01/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ross TR, Ng D, Brown JS, Pardee R, Hornbrook MC, Hart G, et al. The HMO Research Network Virtual Data Warehouse: A Putlic Data Model to Support Collaboration. eGEMs. 2014;2(1) doi: 10.13063/2327-9214.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coltin K, Beck A. The HEDIS Antidepressant Measure. Behavioral Healthcare Tomorrow. 1999 Jun;:40–7. [PubMed] [Google Scholar]
- 21.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 22.Simon GE, Von Korff M, Rutter CM, Peterson DA. Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry. 2001;58(4):395–401. doi: 10.1001/archpsyc.58.4.395. [DOI] [PubMed] [Google Scholar]
- 23.Simon GE, Stewart C, Beck A, Ahmedani BK, Coleman K, Whitebird RR, et al. How common are antidepressant prescriptins without mental health diagnosis? Psychiatr Serv. 2013 in press. [Google Scholar]
- 24.Huang F, Chung H, Kroenke K, Delucchi K, Spitzer R. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–52. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer R, Williams J. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59. doi: 10.1016/j.genhosppsych.2010.03.006. Epub 2010/07/17. [DOI] [PubMed] [Google Scholar]
- 27.Little RJ, Rubin DB. Statisitical analysis with missing data. John Wiley and Sons; New York: 2002. 1987. [Google Scholar]
- 28.Robins J, Rotnitzky A. Semiparametric efficiency in multivariate regression models with missing data. J Am Stat Assoc. 1995;(90):122–9. [Google Scholar]
- 29.Koenig H, George L, Peterson B, Pieper C. Depression in medically ill hospitalized older adults: Prevalence, characteristics, and course of symptoms according ot six diagnostic schemes. Am J Psychiatry. 1997;154:1376–83. doi: 10.1176/ajp.154.10.1376. [DOI] [PubMed] [Google Scholar]
- 30.Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. Epub 2003/04/01. [DOI] [PubMed] [Google Scholar]
- 31.Harding KJ, Rush AJ, Arbuckle M, Trivedi MH, Pincus HA. Measurement-based care in psychiatric practice: a policy framework for implementation. J Clin Psychiatry. 2011;72(8):1136–43. doi: 10.4088/JCP.10r06282whi. Epub 2011/02/08. [DOI] [PubMed] [Google Scholar]
- 32.Valuck RJ, Anderson HO, Libby AM, Brandt E, Bryan C, Allen RR, et al. Enhancing Electronic Health Record Measurement of Depression Severity and Suicide Ideation: A Distributed Ambulatory Research in Therapeutics Network (DARTNet) Study. J Am Board Fam Med. 2012;25(5):582–93. doi: 10.3122/jabfm.2012.05.110053. Epub 2012/09/08. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell J, Trangle MA, Degnan B, Gabert T, Haight B, Kessler D, et al. Adult Depression in Primary Care (Updated, September 2013) Insititute for Clinical Systems Improvement; Minneapolis: 2013. [Google Scholar]
- 34.Kirsch I, Deacon B, Huedo-Medina T, Scoboria A, Moore T, Johnson B. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLOS Med. 2008;5:e45. doi: 10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47–53. doi: 10.1001/jama.2009.1943. Epub 2010/01/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khan A, Leventhal R, Khan S, Brown W. Severity of depression and response to antidepressants and placebo: an analysis of the Food and Drug Administration database. J Clin Psychopharmacol. 2004;22:40–5. doi: 10.1097/00004714-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Vohringer PA, Ghaemi SN. Solving the antidepressant efficacy question: effect sizes in major depressive disorder. Clin Ther. 2011;33(12):B49–61. doi: 10.1016/j.clinthera.2011.11.019. Epub 2011/12/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barbui C, Cipriani A, Patel V, Ayuso-Mateos JL, van Ommeren M. Efficacy of antidepressants and benzodiazepines in minor depression: systematic review and meta-analysis. Br J Psychiatry. 2011;198(1):11–6. doi: 10.1192/bjp.bp.109.076448. sup 1. Epub 2011/01/05. [DOI] [PMC free article] [PubMed] [Google Scholar]