Abstract
Dermoscopic findings for 17 cases of lichen planus-like keratosis (LPLK) were chronologically evaluated. Three males and 14 females were included in the study and the ages ranged from 43 to 85 years (median 65 years). Three cases were diagnosed based on stereotypical dermoscopic findings, while the other 14 cases were histopathologically diagnosed as LPLK. Dermoscopy photographs were divided into four groups depending on the number of days (D) from the initial visit: 1) D = 0 (initial visit or biopsy day); 2) D = 61 to 180; 3) D = 181 to 270; 4) D = 271 to 360. Dermoscopic findings, described as light brown pseudonetwork, pinkish area, gray pseudonetwork, annular granular structures, and blue-gray fine dots, were evaluated at every visit to the hospital.
Initial dermoscopy features included light brown pseudonetworks due to residual solar lentigo and overlapping pinkish areas attributed to lichenoid inflammation. Annular granular structures and gray pseudonetwork appeared to be the main features of the regressing stage; these features seemed to progress to “blue-gray fine dots” in the late regressing stage. Blue-gray dots or globules reflecting melanophages, the hallmark dermoscopic features of LPLK, were believed to resolve in approximately one to two years. Based on the clinical and dermoscopic observations, we have specified five stages of evolution of LPLK, namely 1) pre-existing solar lentigo, 2) early inflammatory stage, 3) early regressing stage, 4) regressing stage, and 5) late regressing stage.
The limitations of the study are that this is a small-sized, retrospective, observational study and that ethnicity of participants is limited to Japanese patients with skin phototype III.
Keywords: lichen planus-like keratosis, solar lentigo, dermoscopy
Introduction
Lichen planus-like keratosis (LPLK) is generally reported to resolve spontaneously, and its dermoscopy features are believed to change with lesion progression and regression [1].
Although LPLK is reported to show typical pigment networks and blue-gray dots by dermoscopy, there are limited reports describing its chronological changes [2]. We report on the dermoscopic findings of 17 cases of LPLK, and summarize the chronological evolution of dermoscopic features for a subset of lesions which was followed up longitudinally.
Methods
Institutional Review Board (IRB) approval was obtained for a dermoscopic observational study. Cases included in this retrospective study were histopathology proven LPLKs (diagnosis confirmed by authors MF and MT) or LPLKs with stereotypical dermoscopic findings diagnosed between 2008 and 2014 at our University Hospital.
All of the dermoscopic pictures were taken with Derma9500 (Derma Medical Inc., Yokohama, Japan) and K-Y Jelly (Johnson & Johnson, New Brunswick, NJ, USA) without polarization. All the dermoscopy images of each case were reviewed side by side for changes (by authors SW and MT). Dermoscopy photographs were divided into four groups depending on the number of days (D) from the initial visit: 1) D = 0 (initial visit or biopsy day); 2) D = 61 to 180; 3) D = 181 to 270; 4) D = 271 to 360. Dermoscopic findings of light brown pseudonetwork, pinkish area, gray pseudonetwork, annular granular structures, and blue-gray fine dots, were evaluated at every visit to the hospital. After considering the chronological changes observed in the follow-up cases, we have defined five sequential stages, 1) pre-existing solar lentigo, 2) early inflammatory stage, 3) early regressing stage, 4) regressing stage, and 5) late regressing stage.
Results
Two illustrative cases are detailed below, followed by the summary data for the entire case series of 17 LPLKs.
Case 1
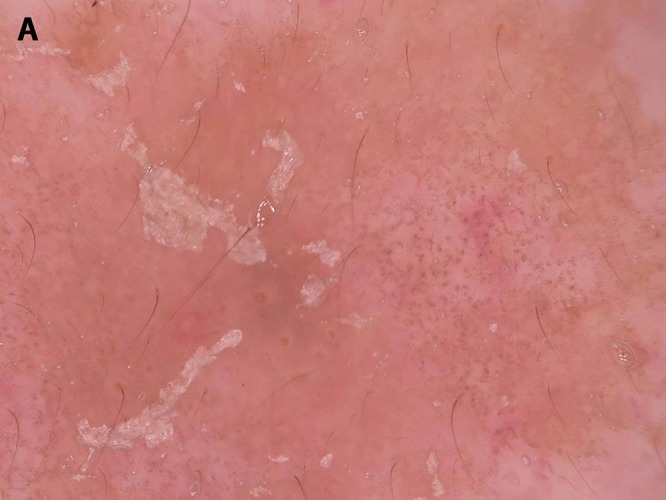
A 67-year-old Japanese woman presented with pigmentation on her left cheek that had persisted for several years. Dermoscopy examination at the initial visit showed light brown pseudonetwork and overlapping pinkish areas throughout. A partial gray pseudonetwork and annular granular structures were also noted (Figure 1A). A partial biopsy confirmed the diagnosis of LPLK. After three months, the pinkish area remained, with decreased brown color and gray pseudonetwork as the main features (Figure 1B). Follow-up at nine months revealed only blue-gray fine dots (Figure 1C). Most of the lesion had resolved entirely at the 21-month follow-up visit, with slight remnants of light brown pseudonetwork focally visible (Figure 1D).
Figure 1.




Chronological dermoscopic changes in Case 1. (A) First visit. (B) 3 months later. (C) 9 months later. (D) 21 months later. [Copyright: ©2016 Watanabe et al.]
Case 2
A 50-year-old Japanese man presented with pigmentation on his left cheek that had persisted for 10 years. Dermoscopy at the initial visit revealed a pinkish area and gray pseudonetwork (Figure 2A). LPLK was diagnosed based on the typical dermoscopy features. After two months, blue-gray dots were the main feature (Figure 2B), which had decreased by the six-month follow-up (Figure 2C). The lesion had almost entirely disappeared at the eight-month follow-up (Figure 2D).
Figure 2.



Chronological dermoscopic changes in Case 2. (A) First visit. (B) 2 months later. (C) 4 months later. (D) 9 months later. [Copyright: ©2016 Watanabe et al.]
Clinical and dermoscopic findings for the entire case series (n=17)
Seventeen patients (3 males and 14 females; age range 43–85 years, median 65) contributing a total of 17 LPLKs were included in this study. Of these, three LPLKs were diagnosed based on stereotypical dermoscopic findings, while 14 cases were histopathologically diagnosed as LPLK. Affected sites included the face (n=13), back of the hand (n=2), and thigh (n=2). Clinical diagnoses at the initial visit included LPLK (n=3), actinic keratosis (n=5), seborrheic keratosis (n=4), Bowen’s disease (n=3), and lentigo maligna (n=2).
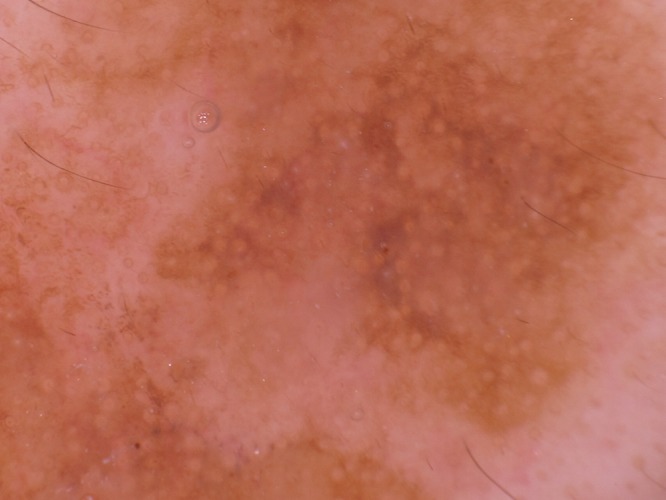
The representative dermoscopy findings of the 17 LPLK cases included light brown pseudonetwork (Figure 3), pinkish background (Figure 4), annular granular structures (Figure 5), gray pseudonetwork composed of diffuse blue-gray dots (Figure 6), and discrete distribution of fine blue-gray dots (Figure 7).
Figure 3.
Light brown pseudonetwork. [Copyright: ©2016 Watanabe et al.]
Figure 4.

Annular granular structure. [Copyright: ©2016 Watanabe et al.]
Figure 5.
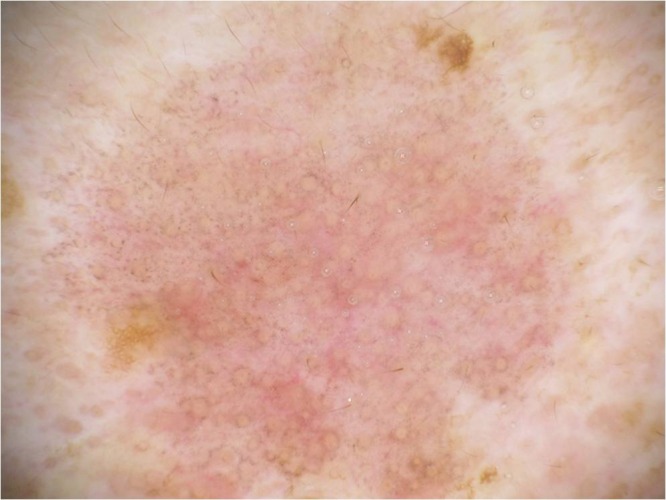
Pinkish area. [Copyright: ©2016 Watanabe et al.]
Figure 6.
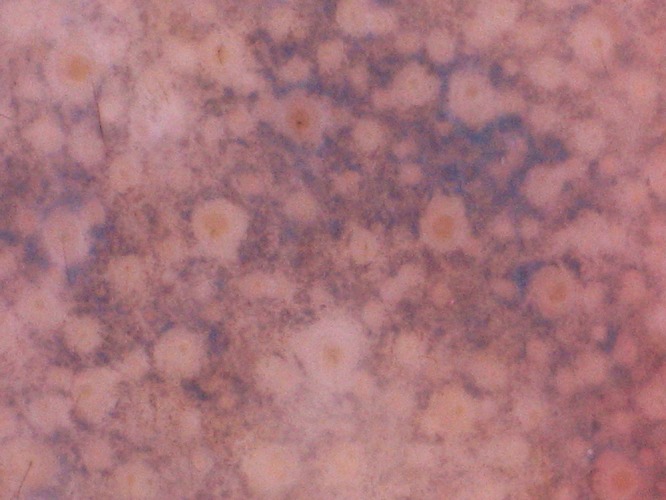
Gray pseudonetwork. [Copyright: ©2016 Watanabe et al.]
Figure 7.
Blue-gray fine dots. [Copyright: ©2016 Watanabe et al.]
The distribution of dermoscopic findings over the study visits are chronologically summarized in Table 1. Nine cases were followed-up from 22 to 659 days (mean; 248); only four patients were followed up for at least 12 months after the initial visit. Notably, not all patients visited the hospital during the early stage, but some initially visited in later stages. Most cases (76%) showed pinkish background with residual solar lentigo at the initial visit. Other features were also present in varying degrees. Light brown pseudonetwork disappeared and pinkish areas decreased over time. Annular granular structures, gray pseudonetwork, and fine blue-gray dots were the main features of the regressing stage.
TABLE 1.
Chronological changes in dermoscopy findings in 17 cases of lichen planus-like keratosis. [Copyright: ©2016 Watanabe et al.]
| Case # | Dermoscopy findings at | |||
|---|---|---|---|---|
| Initial visit | 60 to 180 days | 181 to 270 days | 271 to 360 days | |
| 1 | PA, AGS, BGFD* | LD | ||
| 2 | AGS, GPN* | PA,AGS, BGFD | AGS, BGFD | |
| 3 | AGS, GPN* | AGS, GPN | GPN | |
| 4 | AGS, BGFD** | |||
| 5 | PA, BGFD** | |||
| 6 | PA, BGFD* | |||
| 7 | LBP, PA** | |||
| 8 | PA, AGS, BGFD* | LD | ||
| 9 | PA, AGS, BGFD** | |||
| 10 | PA, BGFD** | |||
| 11 | PA, BGFD* | |||
| 12 | PA, AGS, BGFD* | |||
| 13 | PA, BGFD* | LD | ||
| 14 | LBP, PA, BGFD | PA, BGFD | BGFD | LD |
| 15 | AGS, BGFD* | LD | ||
| 16 | LBP, BGFD | LBP, BGFD | BGFD | |
| 17 | BGFD | LD | ||
| Total lesions per visit | N=17 | N=7 | N=3 | N=4 |
LBP, Light brown pseudonetwork; PA, Pinkish area; AGS, Annular granular structures; GPN, Gray pseudonetwork; BGFD, Blue-gray fine dots;
biopsy;
excision; LD, Lesion disappeared
Discussion
LPLK is thought to be an inflammatory process to eliminate residual solar lentigo or seborrheic keratosis that often disappears spontaneously [3]. The period of spontaneous regression has been reported to range between 3 and18 months [4]. Dermoscopic and histopathological findings were believed to change over time; however, there were few reports describing these chronological changes. Notably, we did not observe any case of LPLK on the chest and presume there might be a racial difference regarding the site of anatomic predilection.
Dermoscopic findings and corresponding histopathological findings in LPLK by stage are summarized in Table 2. The light brown pseudonetwork likely corresponds to remaining precursor solar lentigo lesions. Capillary dilatation during the inflammatory lichenoid reaction would then correspond to the visible pinkish area. Melanin incontinence initially appears as blue-gray dots/globules surrounding hair follicles, which would correspond to annular granular structures, and then distribute diffusely in the papillary dermis, which would correspond to the gray pseudonetwork. Melanophages would gradually decrease in number visible by dermoscopic examination as fine blue-gray dots. As shown in Table 1, not all of the cases necessarily show the early stage, but some cases appeared to be in the late dermoscopic stages at the initial visit. If dermoscopic features for each stage of LPLK were known to correspond to certain pathological stages, then LPLK could be diagnosed without biopsy. However, LPLK in the middle or late stages would often lose the characteristic dermoscopic findings of solar lentigo or seborrheic keratosis and might show irregular dots or globules, irregular streaks, or rhomboid structures suggestive of lentigo maligna [5–7]. Therefore, distinction between LPLK and lentigo maligna would be crucial, and careful observation or biopsy is necessary [4,8].
TABLE 2.
Dermoscopy-pathology relationship. [Copyright: ©2016 Watanabe et al.]
| Stage | Dermoscopic Findings | Histopathological Correlates |
|---|---|---|
| Pre-existing solar lentigo | Light brown pseudonetwork
|
Mild acanthosis with basal melanosis |
| Early inflammatory | Pinkish area
|
Lymphocytic infiltration and capillary dilatation in the papillary and upper dermis |
| Early regressing | Annular granular structures
|
Melanophages surrounding hair follicles |
| Regressing | Gray pseudonetwork
|
Prominent melanophages in the papillary dermis |
| Late regressing | Blue-gray fine dots
|
Discrete melanophages in the papillary dermis |
N = 14 cases
The limitations of the study are that it is a small-sized, retrospective, observational study and that ethnicity of participants is limited to Japanese patients with skin phototype III.
Dermoscopy is quite helpful to assess the stage of regression in LPLK.
Acknowledgments
These cases were presented at the 41st Annual Meeting of the Society for Skin Structure Research, Tokyo, Japan.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Bugatti L, Filosa G. Dermoscopy of lichen planus-like keratosis: a model of inflammatory regression. J Eur Acad Dermatol Venereol. 2007;21:1392–7. doi: 10.1111/j.1468-3083.2007.02296.x. [DOI] [PubMed] [Google Scholar]
- 2.Shono M, Nakamori R, Miki A, et al. A case of lichen planus-like keratosis diagnosed with dermoscopic findings. Skin Research. 2009;8:187–91. [in Japanese] [Google Scholar]
- 3.Ito H, Ishizaki S, Oryu F. Two cases of lichen planus-like keratosis. Rinsho Derma (Tokyo) 1994;36:513–6. (in Japanese) [Google Scholar]
- 4.Mobini N, et al. In: Lever’s Histopathology of the Skin. 10th ed. Elder D, editor. Philadelphia: Lippincott Wilkins; 2009. p. 364. [Google Scholar]
- 5.Lallas A, Apalla Z, Moscarella E, et al. Extensive regression in pigmented skin lesions: a dangerous confounding feature. Dermatol Pract Concept. 2012;2(2):8. doi: 10.5826/dpc.0202a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raptoulis G, Spencer R, Einstein B, et al. Lichen planus-like keratosis of the face: a simulator of melanoma in situ. Dermatol Surg. 2007;33:854–6. doi: 10.1111/j.1524-4725.2007.33183.x. [DOI] [PubMed] [Google Scholar]
- 7.Zaballos P, Marti E, Cuellar F, et al. Dermoscopy of lichenoid regressing seborrheic keratosis. Arch Dermatol. 2006;142:410. doi: 10.1001/archderm.142.3.410. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka M, Sawada M, Kobayashi K. Key points in dermoscopic differentiation between lentigo maligna and solar lentigo. J Dermatol. 2011;38:53–8. doi: 10.1111/j.1346-8138.2010.01132.x. [DOI] [PubMed] [Google Scholar]


