Abstract
Background:
Spitz/Reed nevi are melanocytic lesions that may mimic melanoma at clinical, dermatoscopic and histopathological levels. Management strategies of these lesions remain controversial.
Objectives:
We aim a correlation among clinical-dermatoscopic and histological features of a series of Spitz/Reed nevi diagnosed during 7 years at the Department of Dermatology.
Methods:
Clinical, dermatoscopic and histological features of Spitz/Reed nevi diagnosed at our tertiary hospital from 2008 to 2014 were reviewed in order to seek correlation.
Results:
All described dermatoscopic patterns for Spitz/Reed nevi were found among the 47 enrolled patients; starburst and atypical/multicomponent patterns prevailed (57.4%). Reticular pattern predominated among children younger than 12 years, whereas homogeneous pattern was more frequent in patients older than 12 years, although these differences were not statistically significant (P=0.785). Among histological atypical lesions, all dermatoscopic patterns were represented, but the atypical/multicomponent predominated (56.3%). Two out of 11 dermatoscopically atypical lesions did not show histopathological counterpart.
Conclusions:
The excision of Spitz/Reed nevi in adults is supported, given the inability to accurately predict those with histopathological atypia, based on clinical and dermatoscopic features, which may raise concern about malignancy.
Keywords: dermatoscopy, Reed nevus, spindle and/or epithelioid cell nevus, Spitz nevus
Introduction
The term “Spitz lesion” was first introduced in 1948 by Sophie Spitz referring to “melanomas of childhood” [1]. These lesions were later reclassified as benign melanocytic and considered likely to occur also in older patients. Usually presenting as a pink-red papule on the face or lower extremities, Spitz nevus displays a benign clinical behavior. In 1975, Reed et al [2] described a benign pigmented melanocytic lesion, predominantly found on the lower extremities and thereafter named Reed nevus, which is currently regarded as the pigmented counterpart of Spitz nevus [3,4]. The main concern with these lesions remains their propensity to mimic melanoma at clinical, dermatoscopic and histopathological levels [5].
Dermoscopy improves diagnostic accuracy in many cutaneous lesions, including Spitz/Reed nevi, for which the following patterns were identified: globular, reticular (inverse white and superficial black network), starburst, homogeneous and atypical/multicomponent [4,6].
Despite the attempts, there is no consensus in the histopathological classification of these lesions [7,8]. Although considered by some authors [3] an exclusively spindle-cell nevus, Reed nevus may display a mixed pattern with epithelioid and spindle cells. In classical Spitz nevus, melanocytes are characteristically epithelioid but often also spindle-shaped [3]. Spitz/Reed nevi with atypia include a subset of lesions not fulfilling the histopathological criteria for melanoma, but displaying at least one of the following: a) asymmetry; b) poor lateral circumscription; c) predominance of single melanocytes over nests; d) ulceration; e) extensive involvement of the dermis and subcutis; f) impaired maturation; g) excessive mitotic activity; and h) deep dermal mitoses [3].
This manuscript aims to correlate the clinical-dermatoscopic and histological findings in a series of Spitz/Reed nevi in adults and children followed at the Department of Dermatology of an University Hospital, reviewing and discussing the latest available data on this particular issue.
Methods
We conducted a cross-sectional and retrospective study at the Department of Dermatology of a tertiary University Hospital over a 76-month period, from January 2008 until April 2014. In this Department, adult patients with a suspicion of Spitz/Reed nevi on clinical and dermatoscopic grounds were submitted to excision of these lesions. All patients with a histologically confirmed diagnosis of Spitz/Reed nevi were enrolled. Demographic and clinical data were collected from comprehensive databases including patient age, gender, lesion color and location on the body, as well as any relevant medical history. Dermoscopic images were reviewed and classified in terms of the abovementioned respective patterns. Histopathological features, such as the presence of a junctional component, spindle cells and atypia, based on abovementioned criteria, were further analyzed by two independent double-blinded pathologists. There were no specific requirements regarding the technical equipment for image acquisition and both polarized and nonpolarized dermoscopic images were included, although the most common system used was FotoFinder® dermoscope (FotoFinder Systems, Inc, Bad Birnbach, Germany). The histological classification of excisional biopsies was based on hematoxylin-eosin (HE) stained slides, which were considered representative of the lesion. Whenever necessary, new slides were prepared from the stored paraffin blocks.
The research was focused on the correlation of clinical-dermoscopic and histological features, using image examples, whenever possible.
Statistical analysis was performed using software (SPSS v22.0, IBM Corp, Armonk, NY). Descriptive frequencies were calculated to characterize the study population. Kruskal-Wallis test was performed to determine whether dermoscopic patterns differed among age groups. P values below 0.05 were considered statistically significant.
Results
Of the 47 enrolled patients, 80.9% (38/47) were females, and the overall median age was of 15 years (range 3–72 years), including 59.6% (28/47) under 18 years of age (3–17 years) and 40.4% (19/47) adults (19–72 years). The most common lesion sites were the lower extremities (24/47, 51.1%), followed by the upper extremities (11/47, 23.4%), the trunk (7/47, 14.9%) and the face (5/47, 10.6%). Most frequently described were black (20/47, 42.6%) and brown lesions (17/47, 36.2%). Only 5 out of 47 (10.6%) lesions were pink-red.
Table 1 details the clinical and histological features according to the main dermatoscopic patterns. The prevailing dermatoscopic patterns were the starburst and the atypical/multicomponent, which accounted for 57.4% (27/47) of the cases. Reticular pattern predominated among young children under 12 years of age (3/5, 60%), whereas homogeneous pattern was more frequently found among patients over 12 years old (6/8, 75%), although these differences were not statistically significant (P=0.785, Kruskal-Wallis test). The reticular pattern encompassed the inverse white (n=3) and the superficial black network (n=2).
TABLE 1.
Clinical and histological features of the cases according to the dermatoscopic pattern. [Copyright: ©2016 Pedrosa et al.]
| Clinicopathological Data | Dermatoscopic Pattern | ||||
|---|---|---|---|---|---|
|
Homogeneous n (%) 8 (17.0) |
Globular n (%) 7 (14.9) |
Reticular n (%) 5 (10.7) |
Starburst n (%) 16 (34.0) |
Atypical n (%) 11 (23.4) |
|
| Age in years (median/range) | 22/69 | 16/25 | 11/32 | 16/46 | 12/60 |
| Female gender (n/%) | 5/62.5 | 6/85.7 | 3/60 | 14/87.5 | 10/90.9 |
| Color, n (%) | |||||
| Black | 5 (62.5) | 2 (28.6) | 1 (20) | 10 (62.5) | 2 (18.2) |
| Brown | 1 (12.5) | 4 (57.1) | 1 (20) | 4 (25) | 7 (63.6) |
| Grayish | - | - | 1 (20) | 2 (12.5) | 2 (18.2) |
| Pink-red | 2 (25) | 1 (14.3) | 2 (40) | - | - |
| Location, n (%) | |||||
| Face and neck | 2 (25.0) | 1 (14.3) | - | - | 2 (18.2) |
| Upper extremities | 3 (37.5) | 1 (14.3) | 1 (20) | 5 (31.3) | 1 (9.1) |
| Lower extremity | 2 (25.0) | 5 (71.4) | 1 (20) | 5 (31.3) | 8 (72.7) |
| Buttocks | - | - | 1 (20) | 2 (12.5) | - |
| Trunk | 1 (12.5) | - | 2 (40) | 4 (25.0) | - |
| Histology, n (%) | |||||
| Junctional component | 6 (75.0) | 1 (14.3) | 2 (40.0) | 6 (37.5) | 2 (18.2) |
| Spindle cells | 7 (87.5) | 6 (85.7) | 4 (80.0) | 12 (75.0) | 8 (72.7) |
| Atypical features | 1 (12.5) | 1 (14.3) | 2 (40.0) | 3 (18.8) | 9 (81.8) |
The clinical-dermatoscopic-histological correlation of excised Spitz/Reed nevi revealed overlapping histopathological features among lesions displaying distinct dermatoscopic patterns (Figures 1–3). Among lesions with histopathological atypia (16/47, 34.0%), all dermatoscopic patterns were represented, although the atypical/multicomponent predominated (9/16, 56.3%). Conversely, in 2 out of 11 cases (18.2%) exhibiting dermatoscopic atypia, particularly asymmetry and atypical network, the histopathological sections did not confirm the presence of criteria of atypia. So far, none of the cases developed local recurrence or distant spread after excision (median follow-up time of 14 months).
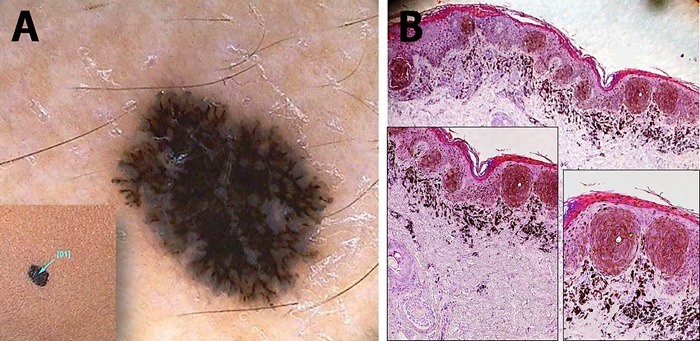
Figure 1.
Black-colored, flat lesion on the right thigh of an 11-year-old female child. (A) A superficial black network emerges under the dermatoscopic examination, overlying a diffuse bluish pigmentation. (B) Histopathology shows a junctional melanocytic lesion with focal areas of pigmented parakeratosis (black arrow) which explains the superficial black network seen in (A). The dense band of superficial dermal melanophages is thought to be responsible for the bluish background (HE, ×20). Pigmented spindle-shaped melanocytes predominate in well-demarcated junctional nests (insets, ×100 and ×200). [Copyright: ©2016 Pedrosa et al.]
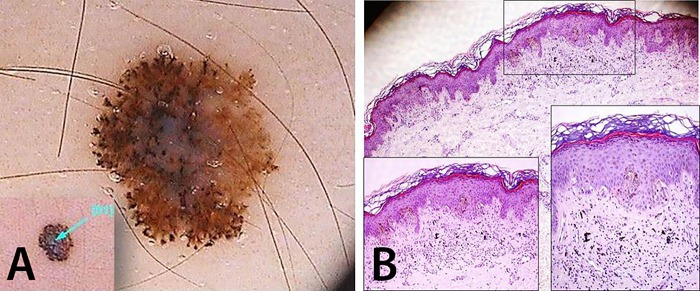
Figure 2.
Brown-colored lesion on the left arm of a 33-year-old female. (A) This atypical/multicomponent patterned lesion is dermatoscopically asymmetric typified by pseudopods irregularly distributed at the periphery and an atypical network attenuated at the right side. (B) Histopathology unveils a junctional asymmetric lesion with epidermal hyperplasia, hyperkeratosis and hypergranulosis exhibiting a focal infiltration of dermal melanophages responsible for the blue-whitish veil seen under dermoscopy (HE, ×40). Confluent epithelioid and spindle-shaped melanocyte nests are observed in insets (HE, ×100 and ×200). [Copyright: ©2016 Pedrosa et al.]
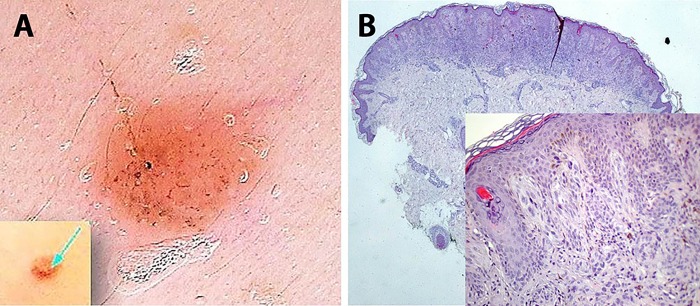
Figure 3.
A pink pale papule on the face of a 5-year-old female child. (A) A homogeneous pink-red pattern exhibiting dermatoscopically dotted and linear vessels and sparse pigmented globules not apparent at naked eye examination. (B) Histopathology shows a compound, symmetrical lesion with shallow depth, well-demarcated borders and a marked dermal inflammatory cell infiltrate in lower magnification (HE, ×40). Epithelioid and spindle-cell nests of melanocytes and sparse melanophages are observed, as well as scant pigment deposition (inset, ×200). [Copyright: ©2016 Pedrosa et al.]
In the pediatric patients (aged under 18 years) with suspected Spitz/Reed nevus by dermoscopy who had submitted to excision (n=28), histopathology confirmed the diagnosis without any prepubertal melanoma diagnosed, although 8 cases (8/28, 28.6%) exhibited at least one histopathological criteria of atypia. Six additional pediatric patients under 12 years of age and displaying lesions clinical and dermatoscopically very suggestive of Spitz/Reed nevi were initially monitored with follow-up visits: 4 lesions showed an involution pattern and 2 showed a growing or stable pattern along 6 to 24 months.
Discussion
Similarly to Ferrara et al [3], we found overlapping histopathological features between lesions categorized as epithelioid and/or spindle-cell nevi supporting the unifying denomination of Spitz/Reed nevi. Additionally, as in the abovementioned study [3], an association between dermatoscopic and histopathological atypia was not always found, especially referring to dermatoscopic asymmetry, raising the possibility that histological sections may not always be representative of the whole lesion. A blue-whitish central veil or a diffuse bluish pigmentation found in lesions with distinct dermatoscopic patterns (Figures 1, 2) usually results from dermal accumulation of melanophages and does not imply regression and therefore should not be considered as an atypical dermatoscopic finding in this setting. We report a prevalence of an atypical/multicomponent dermatoscopic pattern of 23.4%, which is in accordance with other studies [9]. The reticular pattern predominated in children under 12 years old, although without statistical significance, this finding may support the importance of this pattern in early stages of development of these nevi [9]. Conversely, the homogeneous pattern was more frequent among older patients, as expected by the presumed natural evolution of these lesions [8].
Histopathological features that favor the diagnosis of Spitz/Reed nevus over spitzoid melanoma are the symmetrical architecture, cellular maturation in the deep dermis, and absence or scant mitotic activity. However, the histological differential diagnosis of spitzoid tumors often represents a difficult challenge, with several lesions uncovered in a “gray zone” raising interobserver disagreement [3,10].
The presented results support that Spitz/Reed nevi should be excised in adults and children older than 12 years old, in agreement with Lallas et al [10], given the inability to predict with accuracy those with histopathological atypia that may raise concern about aggressive behavior and hinder the differential diagnosis with spitzoid melanoma.
Clinical and dermatoscopic follow-up was the first choice in 6 pediatric patients under 12 years of age with lesions classified as typical Spitz/Reed nevi on clinical and dermatoscopic grounds, and an involution pattern was observed in more than half of the cases along 6 to 24 months, supporting an observational initial approach with clinical and dermatoscopic follow-up of Spitz/Reed nevi in young children, in accordance with other authors [7,8].
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Spitz S. Melanomas of childhood. Am J Pathol. 1948;24:591–609. [PMC free article] [PubMed] [Google Scholar]
- 2.Reed RJ, Ichinose H, Clark WH, Jr, Mihm MC., Jr Common and uncommon melanocytic nevi and borderline melanomas. Semin Oncol. 1975;2:119–47. [PubMed] [Google Scholar]
- 3.Ferrara G, Argenziano G, Soyer HP, et al. The spectrum of Spitz nevi: a clinicopathologic study of 83 cases. Arch Dermatol. 2005;141:1381–7. doi: 10.1001/archderm.141.11.1381. [DOI] [PubMed] [Google Scholar]
- 4.Argenziano G, Soyer HP, Ferrara G, et al. Superficial black network: an additional dermoscopic clue for the diagnosis of pigmented spindle and/or epithelioid cell nevus. Dermatology. 2001;203:333–5. doi: 10.1159/000051784. [DOI] [PubMed] [Google Scholar]
- 5.Ferrara G, Gianotti R, Cavicchini S, et al. Spitz nevus, Spitz tumor, and spitzoid melanoma: a comprehensive clinicopathologic overview. Dermatol Clin. 2013;31:589–98. viii. doi: 10.1016/j.det.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Zalaudek I, Kittler H, Hofmann-Wellenhof R, et al. “White” network in Spitz nevi and early melanomas lacking significant pigmentation. J Am Acad Dermatol. 2013;69:56–60. doi: 10.1016/j.jaad.2012.12.974. [DOI] [PubMed] [Google Scholar]
- 7.Tlougan BE, Orlow SJ, Schaffer JV. Spitz nevi: beliefs, behaviors, and experiences of pediatric dermatologists. JAMA Dermatol. 2013;149:283–91. doi: 10.1001/jamadermatol.2013.1124. [DOI] [PubMed] [Google Scholar]
- 8.Nino M, Brunetti B, Delfino S, et al. Spitz nevus: follow-up study of 8 cases of childhood starburst type and proposal for management. Dermatology. 2009;218:48–51. doi: 10.1159/000161120. [DOI] [PubMed] [Google Scholar]
- 9.de Giorgi V, Savarese I, Rossari S, et al. Clinical and dermoscopic features of small Reed nevus (<6 mm) J Eur Acad Dermatol Venereol. 2013;27:919–21. doi: 10.1111/j.1468-3083.2012.04457.x. [DOI] [PubMed] [Google Scholar]
- 10.Lallas A, Moscarella E, Longo C, et al. Likelihood of finding melanoma when removing a Spitzoid-looking lesion in patients aged 12 years or older. J Am Acad Dermatol. 2015;72:47–53. doi: 10.1016/j.jaad.2014.09.037. [DOI] [PubMed] [Google Scholar]