Abstract
A 43-year-old Japanese man presented with reddish nodules on the ankle. The nodules had a yellowish crust and eroded surface. Dermoscopy revealed red to milky-red globules at the periphery and some glomerular vessels in the center and a whitish-pink network, which corresponded to capillary dilatation in the papillary dermis and prominent acanthosis, respectively. These structures were surrounded by a yellowish peripheral structureless area and multiple white, small, round structures in the center, corresponding to the macerated horny layer and keratin plugs. Blood samples were positive for rapid plasma reagin (1:64), Treponema pallidum hemagglutination assay (1:20480), and fluorescent treponemal antibody-absorption (1:1280). A lesional skin biopsy specimen showed irregular acanthosis and papillomatosis. The Warthin-Starry and anti-Treponema pallidum antibody stains on the biopsy specimen revealed many spirochetes in the lower epidermis and the papillary dermis. A diagnosis of secondary syphilis with condylomata lata was made. After one week of treatment with oral benzylpenicillin benzathine hydrate (Bicillin® G granules 400,000 units; Banyu Pharmaceutical Co., Ltd, Tokyo, Japan), 1.6 million units (U) daily, the ankle lesions had resolved with a small ulcer and pigmentation. Although syphilis is a relatively common disease, this case study reports an unusual presentation as well as dermoscopy findings.
Keywords: condyloma lata, syphilis, dermoscopy, unusual location, ankle
Introduction
Syphilis is an infectious disease caused by Treponema pallidum. Secondary syphilis presents with generalized lesions on the skin and mucous membranes, primarily macules and then progressing to papules. When the papules become hypertrophic and coalesced on macerated skin or mucous membranes, they are called condyloma lata, which more commonly occur around the anus and vulva. We report a case of condylomata lata occurring on the ankle, an unusual site.
Case presentation
A 43-year-old Japanese man presented at a dermatology clinic with multiple erythema on the legs, which had been noticed for three months. Because treatment with a topical glucocorticosteroid, betamethasone butyrate propionate ointment (Antebate, Torii Pharmaceutical, Tokyo), was not effective and several nodules were also present on the left ankle the patient was referred to our University Hospital. The family history and patient’s past medical history were not remarkable. When asked, the patient denied contracting syphilis by a non-sexual route. His work history indicated he was a field superintendent and wore protective shoes throughout the workday.
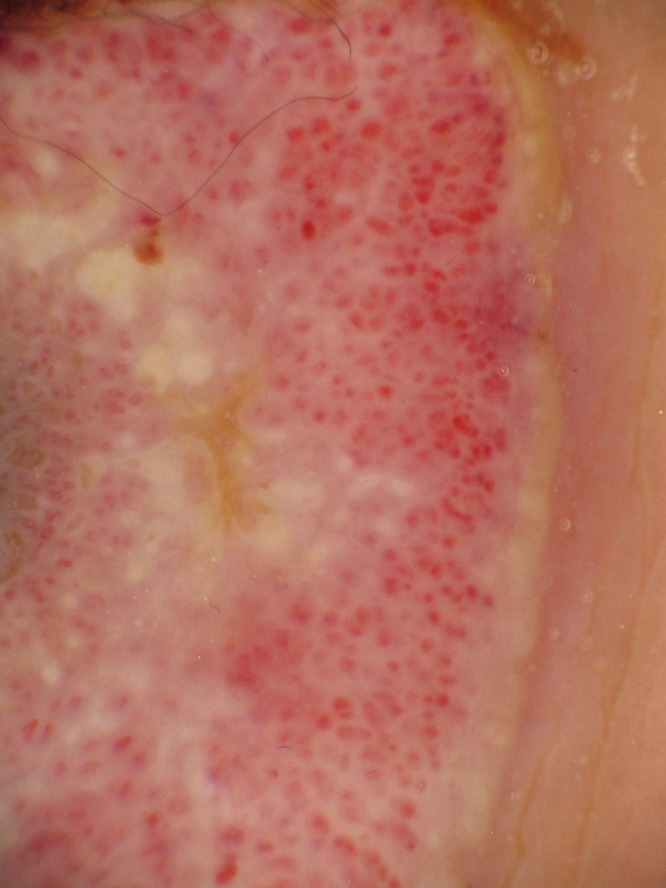
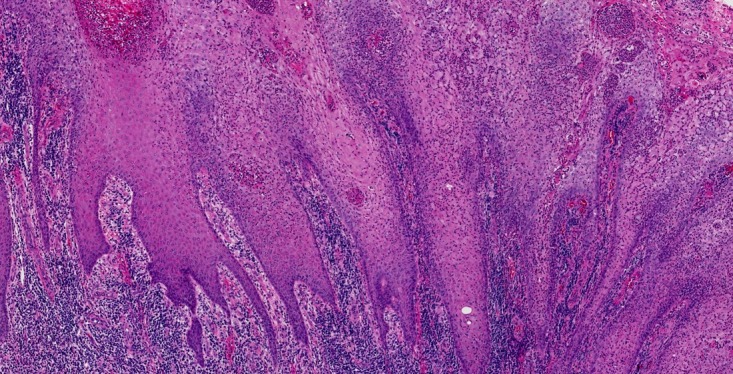
Physical examination showed an indurated reddish nodule measuring 30 × 25 mm with an “8”-shaped raised border and partly covered by yellowish crust (Figure 1A). There was another yellowish, crusted nodule measuring 15 × 5 mm near the heel. Multiple scaly reddish macules measuring up to 5 mm were noted on the palms and soles (Figure 1B). Dermoscopy of the largest nodule demonstrated red to milky red globules and some glomerular vessels and a whitish pink network on the raised border (Figure 2). A yellowish structureless area was noted at the periphery and multiple white, small, round structures were noted in the center.
Figure 1.



Clinical photographs. (A) An indurated reddish nodule of 30 × 25 mm with an “8”-shaped raised border partly covered by yellowish crust. (B, C) Multiple scaly erythematous plaques up to 5 mm on the palms and soles. [Copyright: ©2016 Ikeda et al.]
Figure 2.
Dermoscopy of condyloma lata. Red to milky-red globules, glomerular vessels and a whitish-pink network on the raised border. There is a yellowish structureless area at the periphery and multiple white, small, round structures in the center. [Copyright: ©2016 Ikeda et al.]
Laboratory data showed a white blood cell count of 10400/ml (normal, 3900 to 9800). The assays were positive with the following titers: blood rapid plasma reagin (serological test for syphilis) at 1:64 (normal, 1:<1), T. pallidum hemagglutination assay at 1:20480 (normal, 1:<80) and fluorescent treponemal antibody-absorption test at 1:1280 (normal, 1:<20). The anti-HIV antibody test was negative.
A biopsy sample was obtained from the larger nodule. The histopathological findings included irregular acanthosis and papillomatosis, a parakeratotic horny layer, and dense lymphocytic and plasma cell infiltration in the papillary and upper dermis (Figure 3A). Warthin-Starry (Figure 3B) and anti-T. pallidum antibody (Figure 3C) stains revealed many spirochetes in the lower epidermis and the papillary dermis. Based on the above clinical, serological, and histopathological findings, the diagnosis of secondary syphilis (condylomata lata on the ankle and syphilitic psoriasis on the palms and soles) was made.
Figure 3.
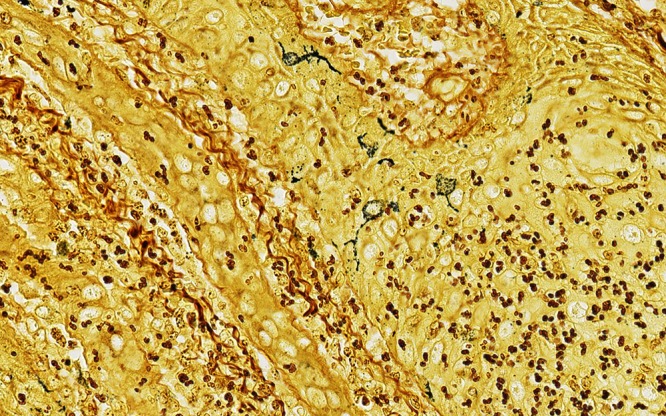
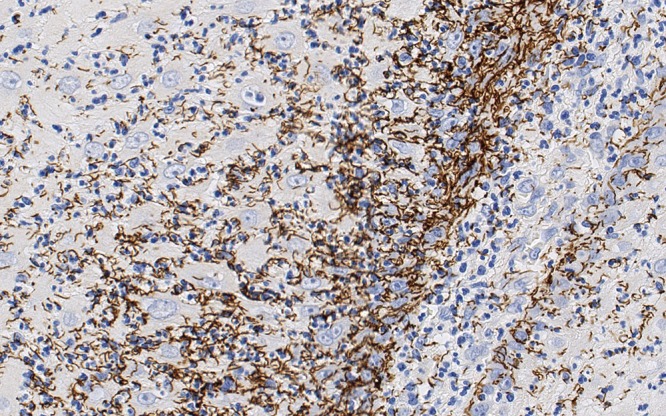
Histopathology from condyloma lata. Hematoxylin-eosin staining (A) showing irregular acanthosis and papillomatosis, a parakeratotic horny layer, and dense lymphocytic and plasma cell infiltration in the papillary and upper dermis. Warthin-Starry (B) and anti-Treponema pallidum antibody (C) stains revealing many spirochetes in the lower epidermis and the papillary dermis. [Copyright: ©2016 Ikeda et al.]
One week after treatment with oral benzylpenicillin benzathine hydrate (Bicillin® G granules 400,000 units; Banyu Pharmaceutical Co., Ltd, Tokyo, Japan) 1.6 million U daily, the ankle lesions had almost resolved with a small ulcer and pigmentation remaining. The Jarisch-Herxheimer reaction was not seen during the treatment. The patient discontinued hospital visits after four weeks of oral treatment.
Conclusions
Condylomata lata consist of flat-topped eroded weeping papules occurring mainly on the perianal area and the vulva [1]. Unusual sites of occurrence include the axilla, palms, face, umbilicus, and toe webs [2–7]. The reason for the unusual or widespread lesions could be attributed to mechanical friction and local hyperhidrosis [2, 3]. The present case showed an extremely rare site for the occurrence of condylomata lata. This rare occurrence of condylomata lata on the ankle could be explained by the patient’s work history of wearing protective shoes that cause a hyperhidrotic environment coupled with the physical friction associated with walking. We hypothesize that the cause for condyloma lata in this case might be due to the patient’s work history of wearing protective shoes that provide an ideal environment for the proliferation of the treponemal spirochetes. The route of transmission of infection is unknown because the patient denied any route.
Dermoscopy of condyloma lata has not been previously reported in the literature. The pathological features of prominent acanthosis seemed to correspond to the whitish-pink network on dermoscopy. The capillary dilatation in the papillary dermis appeared to be corresponding to red to milky-red globules. The yellowish structureless area at the periphery and multiple whitish clods in the center could be explained by the macerated horny layer and keratin plugs.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
This study was presented at the 113th Annual Meeting of the Japanese Dermatological Association.
References
- 1.Syphilis and bacterial sexually transmitted infections. In: Kinghorn GR, editor; Burns DA, Breathnach SM, Cox NH, et al., editors. Rook’s Textbook of Dermatology. 8th ed. 34. Southern Gate: Blackwell; 2010. pp. 1–14. [Google Scholar]
- 2.Fiumara NJ. Unusual location of condyloma lata. A case report. Br J Vener Dis. 1977;53:391–3. doi: 10.1136/sti.53.6.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Saad El-Rifaie M. Condylomata lata of the palms: an unusual site. Br J Vener Dis. 1980;56:267–8. doi: 10.1136/sti.56.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sundararaj AS, Williams J, Gopinathan R, Deivam S. Unusual manifestations of early syphilis in a married male. Florid manifestations of condylomata lata on the face. Int J STD AIDS. 1995;6:52–3. doi: 10.1177/095646249500600112. [DOI] [PubMed] [Google Scholar]
- 5.Hayashi M, Ito K, Ishiji T, et al. Secondary-stage syphilis with unusual clinical features. Pract Dermatol. 2012;34:1189–92. [Google Scholar]
- 6.Tham SN, Lee CT. Condyloma latum mimicking keratoacanthoma in patient with secondary syphilis. Genitourin Med. 1987;63:339–40. doi: 10.1136/sti.63.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen T, Hwong H. Pedal interdigital condylomata lata: a rare sign of secondary syphilis. Sex Transm Dis. 2001;28:184–6. doi: 10.1097/00007435-200103000-00011. [DOI] [PubMed] [Google Scholar]


