Abstract
Objectives
The purpose of this study was to identify the clusters of midlife women by sleep-related symptoms in multi-ethnic groups and to examine racial/ethnic differences in the clusters.
Method
This secondary analysis was conducted on the data from 1,054 midlife women who participated in two cross-sectional descriptive national Internet Surveys. The instruments included questions on background characteristics and health and menopausal status and the Sleep Index for Midlife Women. The data were analyzed using hierarchical clustering methods, chi- square tests, ANOVA and multinomial logistic regression analyses.
Results
The four cluster solution was adopted: Cluster 1 (low total symptoms), Cluster 2 (high physical and psychosomatic symptoms), Cluster 3 (high psychological symptoms), and Cluster 4 (high total symptoms). There were significant differences in the level of education, employment status, family income, social support, country of birth, race/ethnicity, BMI, perceived general health, diagnosed disease, access to health care, and menopausal status among the clusters (p<.05). In Clusters 1, there were significant racial/ethnic differences in the total numbers and total severity scores of total symptoms and physical symptoms (p<.01). In Cluster 3, there were significant racial/ethnic differences in the total numbers of total symptoms and the severity scores of psychosomatic symptoms. Also, there were significant associations of race/ethnicity to individual symptoms in each cluster and significant racial/ethnic differences in individual symptoms in each cluster.
Conclusions
The racial/ethnic associations and differences need to be considered in development of future interventions related to midlife women's sleep-related symptoms.
Keywords: sleep difficulty, midlife women, race/ethnicity
Introduction
In their menopausal transition, midlife women experience a variety of symptoms mainly due to changes in their hormone levels.1 A typical type of symptoms experienced by midlife women are sleep related-symptoms; about 16%∼42% of premenopausal women and 35%∼60% of postmenopausal women reportedly experience sleep difficulties.2 Researchers have reported that midlife women's self-reported symptoms of difficulty falling asleep and difficulties staying asleep increase as their menopausal transition moves forward.3
An increasing number of studies begin to report significant racial/ethnic differences in menopausal symptoms, but very few studies have been conducted on racial/ethnic differences in sleep-related symptoms experienced in menopausal transition.4 Despite the small number of studies on sleep-related symptoms, certain racial/ethnic differences in sleep-related symptoms experienced in menopausal transition have been reported. Hispanics are more likely to have snoring symptoms and report longer sleep duration compared with Non-Hispanic (NH) Whites.4 However, because of the small number of studies on the racial/ethnic differences, further studies are warranted to clarify the association of race/ethnicity to the sleep-related symptoms experienced in menopausal transition through diverse approaches.
A cluster analysis is being widely used to categorize people with similar characteristics, subsequently identifying the association of specific factors to being included in the category.5 Categorizing midlife women who report similar sleep-related symptoms, and finding racial/ethnic differences in the clusters would be helpful in identifying the association of race/ethnicity to sleep-related symptom experience of midlife women during their menopausal transition.5 However, cluster studies have rarely been conducted on the sleep-related symptoms; virtually none was identified in the PUBMED searches. Instead, several cluster studies have been done on general menopausal symptoms reported by midlife women. For instance, the cluster analysis conducted by Cray, Woods, and Mitchell 6 indicated similar factor structures of menopausal symptoms across different menopausal stages, which included a mood component, a vasomotor component, and a pain component. Another example of a cluster analysis study on general menopausal symptoms is by Mishra & Kuh7; they analyzed the data of 695 midlife women in England, Scotland, and Wales using factor analysis and latent class analysis, and reported four clusters of menopausal symptoms including psychological, somatic, vasomotor, and sexual discomfort symptoms. Therefore, this study is one of the first cluster studies to examine the associations of race/ethnicity to sleep-related symptoms experienced by midlife women during their menopausal transition.
The purpose of this study was to identify the clusters of midlife women by sleep-related symptoms in multi-ethnic groups (Aim #1) and to examine racial/ethnic differences in the clusters (Aim #2). In this paper, “symptom experience” is defined as “subjective experiences reflecting changes in a person's bio-psycho-social function, sensation, and cognition”.9 Subsequently, “sleep-related symptom experience” means “subjective experiences reflecting changes in a person's bio-psycho-social function, sensation, and cognition due to sleep difficulties.” Here, a broad definition of sleep-related symptoms was taken; sleep-related symptoms refer to symptoms due to sleep disorders that are defined as “problems with sleeping, including trouble falling or staying asleep, falling asleep at the wrong times, too much sleep, or abnormal behaviors during sleep.”2 This is a secondary analysis of the data from two larger studies including four major racial/ethnic groups of midlife women in the U.S. (NH Whites, NH African Americans, NH Asians, and Hispanics). The original studies were Internet-based survey studies where the data were collected nationally through the Internet.
The UCSF symptom management model10 was used to theoretically guide this study. This model has been widely used in studies on symptom experience in various health care fields.10-12 The model consists of three major domains, three major concepts, and several related sub-concepts based on a literature review.10 The three domains include: person, health and illness, and environments. The three major concepts include: symptom experience, symptom management strategies, and outcomes. These major concepts include several sub-concepts. We targeted to identify the clusters of midlife women by sleep-related symptoms (a sub-concept of the major concept of symptom experience) in multi-ethnic groups (Aim #1) and to examine the influences of race/ethnicity (a sub-concept of the major domain of person) on sleep-related symptom experience (a sub-concept of the major concept of symptom experience)(Aim #2).
Methods
As mentioned above, this secondary analysis was conducted on the data from two cross-sectional descriptive national Internet Surveys. The study was approved by the institutional review board of the institutions that the researchers were affiliated.
Samples and Settings
This study included the data from a total of 1,054 midlife women (316 Non-Hispanic [N-H] Whites 255 Hispanics, 250 N-H African Americans, and 233 N-H Asians). Included were midlife women who were aged 40 to 60 years, who were able to read and write English, and who self-identified their ethnic identity as N-H White, Hispanic, N-H African American or N-H Asian. About 95% of the visitors at the project website participated in the study. Because this was a secondary analysis, the sample size was pre-determined. According to Formann,13 the least number of cases for a cluster analysis is no less than 2k cases (k=the total number of variables), but preferably over 5*2k. Thus, the pre-determined sample size from the original studies was enough for a cluster analysis because we used three sub-scale scores of the sleep-related symptoms.
Instruments
Multiple instruments were used in the original studies. For this analysis, only the data from the following instruments were analyzed.
Background characteristics, health status, and menopausal status
Questions on background characteristics included items on age, education, employment, family income, marital status, number of children, social support, and country of birth and self-reported ethic identity. Family income level was defined as the ability to pay for basic necessities (e.g., food, clothing, and shelter) and was categorized into “not hard,” “somewhat hard,” and “very hard.” Social support was defined as the amount of support received from family members, relatives, or friends, and was measured using one item on four-point ordinal scale: “none of the time,” “a little of the time,” “some of the time,” and “most of the time.”
The women's health status was measured by questions on body weight and height and by a Likert scale item on perceived general health (1 = very unhealthy to 5 = very healthy). Also, two items about diagnosed disease(s) and having no access to health care were included. To determine the women's menopausal status, seven items on the last menstrual cycle, menstrual regularity, and menstrual flow were used. When a woman had menstruation in the last 3 months, with no regularity change, she was considered as pre-menopausal. When a woman had menstrual bleeding in the previous 3 months, but had experienced increasing irregularity in cycle length over the past year, she was considered as early peri-menopausal. When a woman had menses in the previous 12 months but not in the previous 3 months, she was considered as late peri-menopausal. Finally, when a woman had no menstruation in the last one year, she was considered as post-menopausal.
The Sleep Index for Midlife Women (SIMW)
The Sleep Index for Midlife Women (SIMW) was adopted from the Midlife Women's Symptom Index (MSI).14 The original MSI includes 71 items on physical, psychological, and psychosomatic symptoms that midlife women could experience during their menopausal transition. The SIMW includes only 24 items to measure sleep-related symptoms in three categories (physical, psychological, and psychosomatic symptoms). These items were selected through an extensive literature review on symptoms related to sleep quality in general such as sleep disorders, chronic pain, mood disorders, and vasomotor symptoms.15-20 Again, we took a broad definition of sleep-related symptoms, and sleep-related symptoms refer to symptoms due to sleep disorders.2 Five items (poor appetite, painful swollen joint, back pain, night sweats, and night time urination) were categorized as physical symptoms. Fifteen items (feeling clumsy, feeling unhappy, often crying, feeling depressed, worrying gets you down, upset or irritated, feeling grouchy, feeling anxious, tense, or nervous, keyed up, jittery or restless, feeling panic, worrying about body, decreased sexual interest, loss of interest, problem in concentration, and being forgetful) were included as psychological symptoms. Four items (severe headache, dizziness, exhaustion or fatigue, and difficulty in falling or staying asleep) were included as psychosomatic symptoms.
The individual item has two parts: (a) a prevalence part on a dichotomous item (1 = yes; 0 = no) and (b) a severity part on a 6-point Likert scale item (0 = no symptom∼5 = extremely). The total number of all the symptoms included in the SIMW was calculated as the total number of total symptoms (0∼24). The total number of the symptoms in individual categories was also calculated as the total number of physical (0∼5), psychological (0∼15), and psychosomatic symptoms (0∼4). The total severity scores were also calculated by summing the severity scores of all the items in the SIMW (0∼120). Then, the total severity scores of the symptoms in individual categories were calculated by summing the severity scores of the items in each category (the total severity scores of physical [0∼25], psychological [0∼75], and psychosomatic symptoms [0∼20]). Higher scores indicate more prevalent and severe symptoms. The Cronbach's alpha of the SIMW was .90 (the prevalence part) and .93 (the severity part) in this study.
Data Collection Procedures
For the original studies, project websites were developed, and the websites conformed to the Health Insurance Portability and Accountability Act (HIPAA) and the SysAdmin, Audit, Network, Security (SANS)/Federal Bureau of Investigation (FBI) recommendations. When a woman visited the project websites first, she was mandated to review informed consent sheets and give her consent to participate. Then, she was checked against the inclusion criteria and the quota requirement, and linked to the Internet survey site if she met the criteria. She was required to enter her answers through the Internet.
Data Analysis
De-identified data from the original studies were analyzed using SPSS (version 19.0) software. Only those with less than 10% missing fields were included. First, to determine the clusters of women with sleep-related symptoms, hierarchical clustering methods were used with an agglomerative approach and the average linkage between clusters. Three categories scores of sleep-related symptoms (physical, psychological, and psychosomatic symptoms) were used for hierarchical clustering methods. We computed Z scores of the sum of each sub-category score to standardize continuous variables, and identified outliers.21 The research team used the Dendrogram and the variance ratio criteria to determine which clusters could be combined.21,22 To validate the cluster solution, ANOVA was used (the cluster as the independent variable and sleep-related symptoms as the dependents variables).21 Chi-square tests and multinomial logistic regression analyses were used to test differences in background characteristics, perceived general health, and menopausal status among the identified clusters.
Initially, each independent variable was tested through a univariate regression model. Independent variables with p-values of less than .05 from the likelihood ratio chi-square tests were identified. Then, they were included in a multivariable regression model. To check possible multicollinearity,17 we screened the correlations among independent variables, variance inflation factors, and tolerance values for the model, and determined that multicollinearity was not a concern for this model. As an indicator of the model fit, we used the likelihood ratio chi-square of 287.28 with a p-value < .01. To determine racial/ethnic differences in the sleep-related symptoms in each cluster, the analysis of covariance (ANCOVA) was employed using the general linear model to adjust independent variables that were significantly different among the four racial/ethnic groups in univariate analyses. Differences were regarded as statistically significant when p-values were smaller than 0.05.
Results
Characteristics of the Participants
Background characteristics and health and menopausal status of the participants are summarized in Table 1. The average age of the participants was 48.97 years (SD=5.69). The proportion of those with high education (college and graduate degrees) was 86.6%, and the proportion of those with low family income (hard to pay the basics) was 17.6%. About 70% were married or partnered, and about 70% were born in the United States.
Table 1.
Background characteristics by cluster.
| Variables | Cluster1 n(%) | Cluster2 n(%) | Cluster3 n(%) | Cluster4 n(%) | Total n(%) | p-value | |
|---|---|---|---|---|---|---|---|
| Age (Mean ± SD) | 49.13±5.77 | 49.38±5.68 | 48.43±5.77 | 48.61±5.32 | 48.97±5.69 | .27 | |
| Education | |||||||
| ≤high school | 56(11.4) | 22(10.5) | 29(13.9) | 34(23.4) | 141(13.4) | <.01 | |
| >high school | 435(88.6) | 187(89.5) | 180(86.1) | 111(76.6) | 913(86.6) | ||
| Employment | |||||||
| Yes | 383(78.0) | 166(79.4) | 155(74.2) | 86(59.3) | 790(75.0) | <.01 | |
| No | 108(22.0) | 43(20.6) | 54(25.8) | 59(40.7) | 264(25.0) | ||
| Family Income a | |||||||
| Very Hard | 61(12.4) | 25(12.0) | 43(20.6) | 56(38.6) | 185(17.6) | <.01 | |
| Somewhat hard | 168(34.2) | 88(42.1) | 85(40.7) | 65(44.8) | 406(38.5) | ||
| Not Hard | 262(53.4) | 96(45.9) | 81(36.8) | 24(16.6) | 463(43.9) | ||
| Marital Status | |||||||
| Married/partnered | 347(70.7) | 139(66.5) | 135(64.6) | 93(64.1) | 714(67.7) | .27 | |
| Non-married/separated | 144(29.3) | 70(33.5) | 74(35.4) | 52(35.9) | 340(32.3) | ||
| Number of children | |||||||
| None | 95(19.3) | 42(20.1) | 34(16.3) | 21(14.5) | 192(18.2) | .06 | |
| 1-2 | 269(54.8) | 100(47.8) | 105(50.2) | 68(46.9) | 542(51.4) | ||
| More than 3 | 127(25.9) | 67(32.1) | 70(33.5) | 56(38.6) | 320(30.4) | ||
| Social support | |||||||
| None of time | 66(13.4) | 32(15.3) | 47(22.5) | 26(17.9) | 171(16.2) | <.01 | |
| A little of the time | 113(23.0) | 45(21.5) | 62(29.7) | 50(34.5) | 270(25.6) | ||
| Some of the time | 123(25.1) | 61(29.2) | 44(21.1) | 46(31.7) | 274(26.0) | ||
| Most of the time | 189(38.5) | 71(34.0) | 56(26.8) | 23(15.9) | 339(32.2) | ||
| Country of birth | |||||||
| U.S | 353(71.9) | 168(80.4) | 161(77.0) | 128(88.3) | 810(76.9) | <.01 | |
| Outside U.S | 138(28.1) | 41(19.6) | 48(23.0) | 17(11.7) | 244(23.1) | ||
| Race/ethnicity | |||||||
| Hispanic | 101(20.6) | 56(26.8) | 59(28.2) | 39(26.9) | 255(24.2) | <.01 | |
| N-H Asian | 145(29.5) | 32(15.3) | 42(20.1) | 14(9.7) | 233(22.1) | ||
| N-H African American | 118(24.0) | 55(26.3) | 45(21.5) | 32(22.1) | 250(23.7) | ||
| N-H White | 127(25.9) | 66(31.6) | 63(30.1) | 60(41.4) | 316(30.0) | ||
| Body Mass Index(kg/m2) | |||||||
| Normal(<25) | 237(48.3) | 67(32.1) | 81(38.8) | 38(26.2) | 423(40.1) | <.01 | |
| Overweight (25 to <30) | 123(25.1) | 53(25.4) | 55(26.3) | 34(23.4) | 265(25.1) | ||
| Obese (≥ 30) | 131(26.7) | 89(42.6) | 73(34.9) | 73(50.3) | 366(34.7) | ||
| Perceived general health | |||||||
| Unhealthy | 80(16.3) | 54(25.8) | 59(28.2) | 86(59.3) | 279(26.5) | <.01 | |
| Healthy | 411(83.7) | 155(74.2) | 150(71.8) | 59(40.7) | 775(73.5) | ||
| Diagnosed disease(s) | |||||||
| Yes | 174(35.4) | 102(48.8) | 105(50.2) | 91(62.8) | 472(44.8) | <.01 | |
| No | 317(64.6) | 107(51.2) | 104(49.8) | 54(37.2) | 582(55.2) | ||
| Access to health care | |||||||
| Yes | 410(83.5) | 190(90.9) | 186(89.0) | 127(87.6) | 913(86.6) | .04 | |
| No | 81(16.5) | 19(9.1) | 23(11.0) | 18(12.4) | 141(13.4) | ||
| Menopausal Status | |||||||
| Pre menopause | 166(33.8) | 52(24.9) | 55(26.3) | 14(9.7) | 287(27.2) | <.01 | |
| Early/late peri menopause | 129(26.3) | 67(32.1) | 86(41.1) | 67(46.2) | 349(33.1) | ||
| Post menopause | 196(39.9) | 90(43.1) | 68(32.5) | 64(44.1) | 418(39.7) | ||
| Total | 491(100.0) | 209(100.0) | 209(100.0) | 145(100.0) | 1,054(100.0) | ||
Family income was categorized as ‘not hard to pay for basics’, ‘somewhat hard to pay for basics’, and ‘hard to pay for basics’
Note. Cluster 1= low total symptom group/cluster 2=moderate physical and psychosomatic symptom group/cluster 3=moderate psychological symptom group/and cluster 4=high total symptom group.
Clusters of Midlife Women by Sleep-related Symptoms
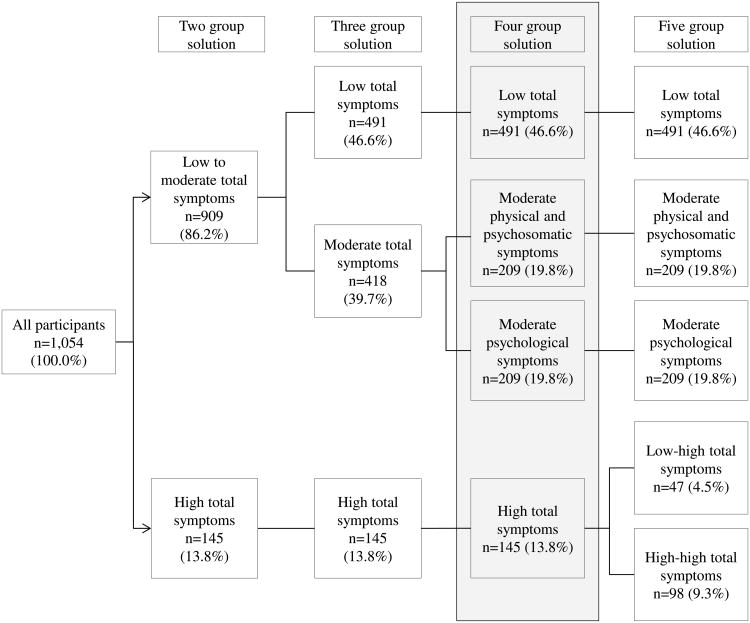
The number of clusters was identified based on the Dendrogram and the variance ratio criteria. The minimum number of the clusters that could be selected was four in this analysis (Figure 1). Forty-six percent of the participants were categorized into Cluster 1 (low total symptom group); 19.8% were categorized into Cluster 2 (moderate physical and psychosomatic symptom group); 19.8% were categorized into Cluster 3 (moderate psychological symptom group); and 13.8% were categorized into Cluster 4 (high total symptom group). There were significant differences in the total number and total severity scores of sleep-related symptoms among the four clusters (p<.01)(Table 2).
Figure 1. The distributions of participants by cluster solution (two, three, four and five cluster solutions).
Table 2.
Sleep-related symptoms by clusterinthe four cluster solution.
| Variables | Cluster 1a (n=491) m±SD | Cluster 2b (n=209) m±SD | Cluster 3c (n=209) m±SD | Cluster4d (n=145) m±SD | Total m±SD | F(p) |
|---|---|---|---|---|---|---|
| Total number of symptoms(0-24) | 2.69±2.07 | 7.81±2.80 | 12.04±3.23 | 17.07±4.34 | 7.53±5.97 | 1177.49(<.01) a<b<c<d |
| Physical symptoms(0-5) | 0.53±0.69 | 1.41±0.88 | 0.90±0.72 | 3.31±0.89 | 1.16±1.20 | 507.88(<.01) a<c<d<b |
| Psychological symptoms(0-15) | 1.80±1.69 | 4.16±2.25 | 9.44±2.48 | 10.79±3.72 | 5.02±4.35 | 864.45(<.01) a<b<c<d |
| Psychosomatic symptoms(0-4) | 0.36±0.48 | 2.24±0.61 | 1.70±1.05 | 2.97±0.99 | 1.36±1.24 | 653.71(<.01) a<c<b<d |
| Total severity score(0-120) | 7.44±6.42 | 23.38±10.41 | 37.70±13.93 | 60.90±21.92 | 23.95±22.30 | 853.77(<.01) a<b<c<d |
| Physical symptoms(0-25) | 1.46±2.12 | 4.45±3.18 | 2.92±2.55 | 11.66±3.93 | 3.75±4.33 | 527.45(<.01) a<c<b<d |
| Psychological symptoms(0-75) | 4.85±5.07 | 11.73±7.27 | 29.08±11.06 | 38.19±17.51 | 15.60±15.86 | 645.53(<.01) a<b<c<d |
| Psychosomatic symptoms(0-20) | 1.12±1.57 | 7.21±2.77 | 5.70±3.73 | 11.01±4.49 | 4.60±4.60 | 557.314(<.01) a<c<b<d |
Note. Cluster 1=low total symptom group/cluster 2=moderate physical and psychosomatic symptom group/cluster 3=moderate psychological symptom group/and cluster 4=high total symptom group.
Differences in Characteristics among Clusters
No significant differences among the four clusters were found in age, marital status, and number of children. However, there were significant differences in education, employment status, family income, social support, country of birth, race/ethnicity, BMI, perceived general health, diagnosed disease(s), access to health care, and menopausal status among the clusters (p<.05)(Table 1). The women in the low symptom group (Cluster 1) tended to report their family income as “not hard to pay for basics”, identify themselves as Asian American, have high social support, have no diagnosed disease, perceive their general health as healthy, and be pre or post menopausal.
Table 3 summarized the results of the multinominal logistic regression analyses to identify the predictors of being in Clusters 1, 2, 3 and 4. Compared with being in the low total symptom group (Cluster 1), being in the moderate physical and psychosomatic symptoms group (Cluster 2) was significantly associated with being Asian American, being obese, perceiving their general health as unhealthy, having no access to health care, and being in early/late peri menopausal status. Compared with being in the low total symptom group (Cluster 1), being in the moderate psychological symptom group (Cluster 3) was significantly associated with having low family income, having low social support, perceiving their general health as unhealthy, having a diagnosed disease, having no access to health care, and being early/late peri menopausal. Comparing with being in the low total symptom group (Cluster 1), being in the high total symptom group (Cluster 4) was significantly associated with having low family income, having low social support, perceiving their general health as unhealthy, having a diagnosed disease, having no access to health care, and being early/late peri menopausal or post menopausal.
Table 3.
Differences in background characteristics among the clusters.
| Variables | Cluster 2 Vs Cluster 1 Adjusted OR(95% CI) | Cluster 3 Vs Cluster 1 Adjusted OR (95% CI) | Cluster 4 Vs Cluster 1 Adjusted OR (95% CI) |
|---|---|---|---|
| Family Income | |||
| Very Hard | 1.82(1.07-3.09)* | 4.18(2.15-8.13)** | |
| Somewhat hard | 1.43(0.97-2.13) | 2.56(1.47-4.48)** | |
| Not hard to pay | 1.00 | 1.00 | |
| Social support | |||
| None of time | 2.45(1.47-4.07)** | 2.36(1.15-4.82)* | |
| A little of the time | 1.61(1.04-2.56)* | 1.94(1.04-3.64)* | |
| Some of the time | 1.20(0.74-1.94) | 2.45(1.31-4.58)** | |
| Most of the time | 1.00 | 1.00 | |
| Race/ethnicity | |||
| Hispanic | 0.98(0.61-1.57) | ||
| N-H Asian | 0.47(0.25-0.89)* | ||
| N-H African | 0.76(0.48-1.21) | ||
| N-H White | 1.00 | ||
| BMI | |||
| Overweight (25 to <30) | 1.25(0.80-1.94) | ||
| Obese (≥ 30) | 1.70(1.10-2.63)* | ||
| Normal | 1.00 | ||
| Perceived general health | |||
| Unhealthy | 1.57(1.03-2.41)* | 1.53(1.0-2.34)* | 4.18(2.60-6.73)** |
| healthy | 1.00 | 1.00 | 1.00 |
| Diagnosed disease(s) | |||
| Yes | 1.65(1.15-2.36)** | 2.04(1.30-3.21)** | |
| No | 1.00 | 1.00 | |
| Access to health care | |||
| No | 1.80(1.02-3.17)* | 1.83(1.06-3.15)* | 1.97(1.01-3.84)* |
| Yes | 1.00 | 1.00 | 1.00 |
| Menopausal Status | |||
| Early/late peri | 1.66(1.07-2.58)* | 2.00(1.31-3.05)** | 4.97(2.54-9.70)** |
| Post menopause | 1.35(0.89-2.05) | 0.92(0.60-1.41) | 2.65(1.37-5.13)** |
| Pre menopause | 1.00 | 1.00 | 1.00 |
Note. Cluster 1=low total symptom group/cluster 2=moderate physical and psychosomatic symptom group/cluster 3=moderate psychological symptom group/and cluster 4=high total symptom group.
Ten independent variables including education, employment, family income, country of birth, race/ethnicity, body mass index, perceived general health, diagnosed disease, access to health care, and menopausal status were adjusted and only significant variables were presented in this table.
p<.05,
p<.01
Racial/Ethnic Differences in Sleep-Related Symptoms by Cluster
Table 4 summarizes racial/ethnic differences in the total number, total severity scores, and three sub-scale scores in each cluster (ANCOVA tests). There were no significant racial/ethnic differences in the total number and total severity scores in the moderate physical and psychosomatic symptom group (Cluster 2), in the moderate psychological symptom group (Cluster 3), and in the high total symptom group (Cluster 4). However, only in the low total symptom group (Cluster 1), there were significant racial/ethnic differences in the total number and total severity scores of physical symptoms (p<.01). In the low total symptom group, White and African women had higher total number and higher total severity scores of physical symptoms than Hispanic and Asian women (p<.01). When racial/ethnic differences in individual symptoms in each cluster were determined, there existed no consistent racial/ethnic differences. Rather, there existed a few racial/ethnic differences in some individual symptoms, which could be mainly due to multiple comparisons that were conducted in the analyses.
Table 4. Racial/ethnic differences in the numbers andseverity scores of sleep-related symptoms in each cluster.
| Clusters | Symptoms | Whitea | Hispanicb | N-H Asianc | N-H Africand | Total | F*(p) |
|---|---|---|---|---|---|---|---|
| M±SD | M±SD | M±SD | M±SD | M±SD | |||
| Numbers of symptoms | |||||||
| Cluster1 | Physical symptoms(0-5) | 0.65±0.74 | 0.42±0.64 | 0.34±0.57 | 0.75±0.74 | 0.53±0.69 | 5.68(<.01) b, c<a, d |
| Psychosomatic symptoms(0-4) | 0.43±0.50 | 0.37±0.48 | 0.30±0.46 | 0.36±0.48 | 0.36±0.48 | 1.18(.31) | |
| psychological symptoms(0-15) | 1.90±1.68 | 1.97±1.83 | 1.66±1.57 | 1.71±1.72 | 1.80±1.68 | 1.17(.32) | |
| Total number of symptoms(0-24) | 2.97±2.17 | 2.75±2.07 | 2.30±1.87 | 2.82±2.13 | 2.69±2.07 | 1.52(.21) | |
| Cluster 2 | Physical symptoms(0-5) | 1.47±0.90 | 1.48±0.91 | 1.16±0.85 | 1.42±0.83 | 1.41±0.88 | 1.61(.19) |
| Psychosomatic symptoms(0-4) | 2.11±0.66 | 2.33±0.69 | 2.28±0.47 | 2.27±0.53 | 2.24±0.61 | 0.92(.43) | |
| Psychological symptoms(0-15) | 4.48±2.27 | 4.23±2.01 | 3.94±2.56 | 3.84±2.27 | 4.16±2.25 | 1.23(.30) | |
| Total number of symptoms(0-24) | 8.06±2.73 | 8.05±2.72 | 7.38±2.72 | 7.53±2.71 | 7.81±2.80 | 1.56(.20) | |
| Cluster 3 | Physical symptoms(0-5) | 1.06±0.69 | 0.75±0.73 | 0.83±0.73 | 0.96±0.71 | 0.90±0.72 | 1.56(.20) |
| Psychosomatic symptoms(0-4) | 1.94±1.03 | 1.44±1.02 | 1.60±1.13 | 1.80±0.99 | 1.70±1.05 | 1.59(.19) | |
| Psychological symptoms(0-15) | 9.79±2.35 | 8.90±2.18 | 9.71±2.71 | 9.38±2.77 | 9.44±2.48 | 0.64(.59) | |
| Total number of symptoms(0-24) | 12.79±2.91 | 11.08±3.06 | 12.14±3.32 | 12.13±3.57 | 12.04±3.23 | 1.49(.22) | |
| Cluster 4 | Physical symptoms(0-5) | 3.40±0.91 | 3.13±0.77 | 3.36±1.01 | 3.38±0.94 | 3.32±0.89 | 1.26(.29) |
| Psychosomatic symptoms(0-4) | 2.97±0.99 | 3.08±0.93 | 3.14±0.66 | 2.75±1.16 | 2.97±0.99 | 0.44(.73) | |
| Psychological symptoms(0-15) | 11.27±3.70 | 10.56±3.86 | 12.00±2.5 | 9.63±3.93 | 10.79±3.72 | 0.70(.55) | |
| Total number of symptoms(0-24) | 17.63±3.40 | 16.77±4.25 | 18.50±2.82 | 15.75±4.66 | 17.07±4.34 | 0.41(.75) | |
| Severity scores | |||||||
| Cluster1 | Physical symptoms(0-25) | 1.83±2.38 | 1.05±1.71 | 0.86±1.60 | 2.19±2.39 | 1.47±2.12 | 6.44(<.01) |
| Psychosomatic symptoms(0-20) | 1.28±1.56 | 1.10±1.53 | 0.93±1.51 | 1.19±1.67 | 1.12±1.57 | 0.44(.73) | |
| psychological symptoms(0-75) | 5.09±5.00 | 5.56±5.79 | 4.23±4.33 | 4.73±5.30 | 4.85±5.07 | 1.47(.22) | |
| Total severity scores (0-120) | 8.20±6.74 | 7.71±6.68 | 6.02±5.34 | 8.11±6.85 | 7.43±6.42 | 1.07(.36) | |
| Cluster 2 | Physical symptoms(0-25) | 5.14±3.60 | 4.38±3.11 | 3.34±2.67 | 4.33±2.84 | 4.45±3.18 | 1.54(.21) |
| Psychosomatic symptoms(0-20) | 7.23±2.79 | 7.64±3.36 | 6.50±1.87 | 7.16±2.49 | 7.21±2.77 | 0.62(.60) | |
| psychological symptoms(0-75) | 13.41±7.98 | 11.50±5.77 | 10.41±8.12 | 10.71±7.03 | 11.73±7.27 | 1.21(.31) | |
| Total severity scores (0-120) | 25.77±11.19 | 23.52±9.68 | 20.25±10.51 | 22.20±9.66 | 23.38±10.41 | 1.57(.20) | |
| Cluster 3 | Physical symptoms(0-25) | 3.43±2.60 | 2.46±2.60 | 2.60±2.44 | 3.13±2.46 | 2.92±2.55 | 1.13(.34) |
| Psychosomatic symptoms(0-20) | 6.60±3.82 | 4.68±3.28 | 5.36±4.18 | 6.11±3.41 | 5.70±3.73 | 1.54(.21) | |
| psychological symptoms(0-75) | 30.14±10.63 | 27.71±10.31 | 30.31±11.86 | 28.22±11.88 | 29.08±11.06 | 0.46(.71) | |
| Total severity scores (0-120) | 40.17±13.20 | 34.85±13.39 | 38.26±14.51 | 37.47±14.80 | 37.70±13.93 | 0.38(.77) | |
| Cluster 4 | Physical symptoms(0-25) | 12.15±4.19 | 11.49±3.43 | 10.86±4.50 | 11.31±3.81 | 11.66±3.93 | 0.23(.87) |
| Psychosomatic symptoms(0-20) | 11.32±4.60 | 11.67±3.95 | 11.00±3.53 | 9.84±4.50 | 11.06±4.49 | 0.63(.60) | |
| psychological symptoms(0-75) | 40.02±17.79 | 38.64±18.37 | 39.64±13.10 | 33.56±17.53 | 38.19±17.51 | 0.39(.76) | |
| Total severity scores (0-120) | 63.48±23.22 | 61.79±21.36 | 61.50±17.39 | 54.72±21.62 | 60.90±21.92 | 0.35(.79) | |
Note. N-H=nonhispanic/post-hoc tests=Scheffe tests/cluster 1=low total symptom group/cluster 2=moderate physical and psychosomatic symptom group/cluster 3=moderate psychological symptom group/and cluster 4=high total symptom group.
Adjusted F scores after controlling for multiple variables (employment, family income, maternal status, number of children, country of birth, body mass index, perceived general health, diagnosed disease, and access to health care) using ANCOVA.
Discussion
The findings reported in this secondary analysis agree with some previous studies that reported racial/ethnic differences in sleep-related symptoms.4, 23, 24 The finding of this study on Asian women's sleep-related symptoms agrees with that of the previous studies; compared with other racial/ethnic groups, Asians reported significantly lower total numbers and total severity scores of sleep-related symptoms and lower frequencies and severity scores of some individual symptoms. However, the finding that Hispanic women had lower total number of sleep-related physical symptoms compared with White and African American women is different from the literature reporting that Hispanics had significantly higher numbers and severity scores of sleep-related symptoms compared with other racial/ethnic groups.4
The finding on significant racial/ethnic differences only in the low total symptom group needs to be highlighted. The finding supports that racial/ethnic differences become prominent when midlife women experience low total number and low total severity scores of total symptoms. As many researchers working with midlife women have suggested,1, 25-29 understanding on symptoms experienced during menopausal transition, including sleep-related symptoms, needs to be based on contextual understanding of a woman's life and her psychological state, psychological influences, cultural and social background, social contexts, the microenvironment of the household, and the aging process. Maybe in the low total symptom group, the influences of these contextual factors could be more prominent than in other moderate or high symptom groups in some reasons.
The findings of this study also support multiple predictors of sleep-related symptoms that have been reported in the literature. Studies have reported that sleep-related symptoms are associated with multiple factors including chronic stress, psychological symptoms (anxiety, depression), low self-perceived health, vasomotor symptoms associated with menopause (hot flashes, night sweats), underlying sleep disorders (apnea, restless leg syndrome), musculoskeletal pain, medication side-effects, etc.30-36 The findings reported in this paper support some of these predictors such as race/ethnicity (specifically not being Asian American), obesity, perceived general health, social support, diagnosed disease(s), access to health care, and family income.
The literature is clear that midlife women have different sleep experiences throughout their pre-menopausal, peri-menopausal, and post-menopausal periods.36,37 Menopausal status has been reported to be a significant predictor associated with sleep-related symptoms, 37,38 which is supported by the findings of this analysis. Across the clusters that we found in this secondary analysis except the low total symptom cluster (Cluster 1), being in early/late peri menopause was significantly associated with being in each cluster. Studies have reported that peri-menopausal women are more likely to report poor sleep quality compared to pre- and post-menopausal women due to sleep onset latency and lack of sleep efficiency.34
This study has some limitations due to the inherent nature of a secondary analysis. First of all, because the original studies were Internet survey studies, the participants tended to be highly educated, married, and employed women. Also, the participants did not represent all sub-ethnic groups within individual racial/ethnic groups, and the data were self-reported data. Thus, there could exist some selection bias. Second, there was no control of the sample size and variables because this was a secondary analysis. Finally, there could exist some limitations due to multiple comparisons conducted in this study. As described above, the racial/ethnic differences found in some individual symptoms did not show consistent patterns, which we interpreted as a result of multiple comparisons that were conducted with four clusters, four subscales of symptoms, and four racial/ethnic groups.
Conclusions
This study indicated four clusters of midlife women by their sleep-related symptoms during menopausal transition, and reported racial/ethnic differences in the total number and total severity scores of physical symptoms only in the low total symptom group (p<.01). The study supported significant associations of selected predictors to the women's sleep-related symptoms as well. Based on the study findings, we propose the following implications for future research and practice with midlife women experiencing sleep-related symptoms in their menopausal transition. First of all, in future intervention development for and health care practice with midlife women in menopausal transition, researchers need to consider that racial/ethnic differences could be prominent in midlife women with low sleep-related symptoms. Also, to make an intervention effective for midlife women in menopausal transition, the predictors of their sleep-related symptoms by symptom cluster need to be considered and incorporated into the intervention design. Finally, racial/ethnic differences in midlife women's sleep-related symptom experience by symptom cluster need to be further examined as this paper adds some new findings.
Acknowledgments
This study was conducted as part of a larger study funded by the National Institutes of Health (NIH/NINR/NIA; R01NR008926 and NIH/NINR/NHLBI; R01NR010568). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflict of interest/financial disclosure.
References
- 1.Avis NE, Stellato R, Crawford S, et al. Is there a menopausal syndrome? Menopausal status and symptoms across racial/ethnic groups. Soc Sci Med. 2001;52:345–356. doi: 10.1016/s0277-9536(00)00147-7. [DOI] [PubMed] [Google Scholar]
- 2.U. S. National Library of Medicine. Sleep disorders - overview. [Accessed Novemebr 22 2014]; http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001803/. Updated January 22 2014.
- 3.Kravitz HM, Joffe H. Sleep during the perimenopause: a SWAN story. Obstet Gynecol Clin North Am. 2011;38:567–586. doi: 10.1016/j.ogc.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramos AR, Wohlgemuth WK, Dong C, et al. Race-ethnic differences of sleep symptoms in an elderly multi-ethnic cohort: the Northern Manhattan Study. Neuroepidemiology. 2011;37:210–215. doi: 10.1159/000334315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massart DL, Kaufman L. The interpretation of analytical chemical data by the use of cluster analysis. New York, NY: John Wiley & Sons, Inc.; 1983. [Google Scholar]
- 6.Cray LA, Woods NF, Mitchell ES. Identifying symptom clusters during the menopausal transition: observations from the Seattle Midlife Women's Health Study. Climacteric. 2013;16:539–549. doi: 10.3109/13697137.2012.746657. [DOI] [PubMed] [Google Scholar]
- 7.Mishra GD, Kuh D. Health symptoms during midlife in relation to menopausal transition: British prospective cohort study. BMJ. 2012;344:e402. doi: 10.1136/bmj.e402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sievert LL, Obermeyer CM. Symptom clusters at midlife: a four-country comparison of checklist and qualitative responses. Menopause. 2012;19:133–144. doi: 10.1097/gme.0b013e3182292af3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blacklow RS. MacBryde's signs and symptoms Applied pathologic physiology and clinical interpretation. 6th. Philadelphia, PA: JB Lippincott Co.; 1983. [Google Scholar]
- 10.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33:668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 11.Linder L. Analysis of the UCSF Symptom Management Theory: implications for pediatric oncology nursing. J Pediatr Oncol Nurs. 2010;27:316–324. doi: 10.1177/1043454210368532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skelly AH, Leeman J, Carlson J, Soward A, Burns D. Conceptual model of symptom‐focused diabetes care for African Americans. J Nurs Scholarsh. 2008;40:261–267. doi: 10.1111/j.1547-5069.2008.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Formann AK. Die latent-class-analyse: Einführung in theorie und anwendung[Latent class nalysis: Introduction to theory and application] Weinheim: Beltz; 1984. [Google Scholar]
- 14.Im EO. The midlife women's symptom index (MSI) Health Care Women Int. 2006;27:268–287. doi: 10.1080/07399330500506600. [DOI] [PubMed] [Google Scholar]
- 15.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 16.Douglass AB, Bornstein R, Nino-Murcia G, et al. The Sleep Disorders Questionnaire I: Creation and multivariate structure of SDQ. Sleep. 1994;17:160–167. doi: 10.1093/sleep/17.2.160. [DOI] [PubMed] [Google Scholar]
- 17.Fuller KH, Waters WF, Binks PG, Anderson T. Generalized anxiety and sleep architecture: a polysomnographic investigation. Sleep. 1997;20:370–376. doi: 10.1093/sleep/20.5.370. [DOI] [PubMed] [Google Scholar]
- 18.Koseoglu BF, Gokkaya NK, Ergun U, Inan L, Yesiltepe E. Cardiopulmonary and metabolic functions, aerobic capacity, fatigue and quality of life in patients with multiple sclerosis. Acta Neurol Scand. 2006;114:261–267. doi: 10.1111/j.1600-0404.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- 19.Krystal AD, Edinger J, Wohlgemuth W, Marsh GR. Sleep in peri-menopausal and post-menopausal women. Sleep Med Rev. 1998;2:243–253. doi: 10.1016/s1087-0792(98)90011-9. [DOI] [PubMed] [Google Scholar]
- 20.Owens JF, Matthews KA. Sleep disturbance in healthy middle-aged women. Maturitas. 1998;30:41–50. doi: 10.1016/s0378-5122(98)00039-5. [DOI] [PubMed] [Google Scholar]
- 21.Mooi E, Sarstedt M. A concise guide to market research The process, data and methods using IBM SPSS statictics. Berlin Heidelberge: Springer-Verlag Berlin Heidelberge; 2011. [Google Scholar]
- 22.Calinske T, Harabasz J. A dendrite method for cluster analysis. Commun Stat Theory Methods. 1974;3:1–27. [Google Scholar]
- 23.Mansikkamäki K, Raitanen J, Nygård CH, et al. Sleep quality and aerobic training among menopausal women--a randomized controlled trial. Maturitas. 2012;72:339–345. doi: 10.1016/j.maturitas.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Tworoger SS, Yasui Y, Vitiello MV, et al. Effects of a yearlong moderate-intensity exercise and a stretching intervention on sleep quality in postmenopausal women. Sleep. 2003;26:830–838. doi: 10.1093/sleep/26.7.830. [DOI] [PubMed] [Google Scholar]
- 25.Carolan M. Menopause: Irish women's voices. J Obstet Gynecol Neonatal Nurs. 2000;29:397–404. doi: 10.1111/j.1552-6909.2000.tb02062.x. [DOI] [PubMed] [Google Scholar]
- 26.Deeks AA. Psychological aspects of menopause management. Best Pract Res Clin Endocrinol Metab. 2003;17:17–31. doi: 10.1016/s1521-690x(02)00077-5. [DOI] [PubMed] [Google Scholar]
- 27.Hewner SJ. Postmenopausal function in context: biocultural observations on Amish, neighboring non-Amish, and Ifugao household health. Am J Hum Biol. 2001;13:521–530. doi: 10.1002/ajhb.1084. [DOI] [PubMed] [Google Scholar]
- 28.Obermeyer CM. Menopause across cultures: a review of the evidence. Menopause. 2000;7:184–192. doi: 10.1097/00042192-200007030-00009. [DOI] [PubMed] [Google Scholar]
- 29.Sievert LL, Obermeyer CM, Saliba M. Symptom groupings at midlife: cross-cultural variation and association with job, home, and life change. Menopause. 2007;14:798–807. doi: 10.1097/gme.0b013e31804f8175. [DOI] [PubMed] [Google Scholar]
- 30.Ameratunga D, Goldin J, Hickey M. Sleep disturbance in menopause. Intern Med J. 2012;42(7):742–747. doi: 10.1111/j.1445-5994.2012.02723.x. [DOI] [PubMed] [Google Scholar]
- 31.Brown JP, Gallicchio L, Flaws JA, Tracy JK. Relations among menopausal symptoms, sleep disturbance and depressive symptoms in midlife. Maturitas. 2009;62:184–189. doi: 10.1016/j.maturitas.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joffe H, Chang Y, Dhaliwal S, et al. Lifetime history of depression and anxiety disorders as a predictor of quality of life in midlife women in the absence of current illness episodes. Arch Gen Psychiatry. 2012;69:484–492. doi: 10.1001/archgenpsychiatry.2011.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joffe H, Massler A, Sharkey KM. Evaluation and management of sleep disturbance during the menopause transition. Semin Reprod Med. 2010;28:404–421. doi: 10.1055/s-0030-1262900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Minarik PA. Sleep disturbance in midlife women. J Obstet Gynecol Neonatal Nurs. 2009;38:333–343. doi: 10.1111/j.1552-6909.2009.01031.x. [DOI] [PubMed] [Google Scholar]
- 35.Shaver JL. Women and sleep. Nurs Clin North Am. 2002;37:707–718. doi: 10.1016/s0029-6465(02)00033-6. [DOI] [PubMed] [Google Scholar]
- 36.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8:119–132. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 37.Greenblum CA, Rowe MA, Neff DF, Greenblum JS. Midlife women: symptoms associated with menopausal transition and early postmenopause and quality of life. Menopause. 2013;20:22–27. doi: 10.1097/gme.0b013e31825a2a91. [DOI] [PubMed] [Google Scholar]
- 38.Xu M, Belanger L, Ivers H, Guay B, Zhang J, Morin CM. Comparison of subjective and objective sleep quality in menopausal and non-menopausal women with insomnia. Sleep Med. 2011;12(1):65–69. doi: 10.1016/j.sleep.2010.09.003. [DOI] [PubMed] [Google Scholar]