Abstract
Ethnic minority midlife women frequently do not recognize cardiovascular symptoms that they experience during the menopausal transition. Racial/ethnic differences in cardiovascular symptoms are postulated as a plausible reason for their lack of knowledge and recognition of the symptoms. The purpose of this study was to explore racial/ethnic differences in midlife women’s cardiovascular symptoms and to determine the factors related to these symptoms in each racial/ethnic group. This was a secondary analysis of the data from a larger study among 466 participants, collected from 2006 to 2011. The instruments included questions on background characteristics, health and menopausal status and the Cardiovascular Symptom Index for Midlife Women. The data were analyzed using inferential statistics, including Poisson regression and logistic regression analyses. Significant racial/ethnic differences were observed in the total numbers and total severity scores of cardiovascular symptoms (p<0.01). Non-Hispanic Asians had significantly lower total numbers and total severity scores compared to other racial/ethnic groups (p<0.05). The demographic and health factors associated with cardiovascular symptoms were somewhat different in each racial/ethnic group. Further studies are needed about possible reasons for the racial/ethnic differences and the factors associated with cardiovascular symptoms in each racial/ethnic group.
Keywords: cardiovascular symptoms, midlife women, race, ethnicity
Across all cultures and ethnicities, the population in the U.S. is aging (Pérez et al. 2009). The role of disease prevention and health promotion in midlife becomes more important as disease prevention and health promotion in the midlife years promise to be a significant predictor of better health in later years (Pérez et al. 2009). Indeed, midlife adults, including ethnic minority midlife adults, have been reported to be at increased risk of cardiovascular disease (CVD), as well as of other chronic diseases compared with their younger counterparts (U.S. Department of Health and Human Services 2013). CVD is the leading cause of mortality among midlife women in the U.S. (National Center for Health Statistics 2005).
The menopausal transition, which midlife women of all racial/ethnic groups undergo as they age, brings about several biological and psychosocial changes that are frequently linked to increased CVD risks (Pérez et al. 2009). Midlife women, during the menopausal transition, could experience cardiovascular symptoms that they did not experience previously as their estrogen levels decline and their CVD risks increase (Thurston et al. 2008; Sutton-Tyrrell et al. 2005). Indeed, a few studies, including the Study of Women Across the Nation (SWAN), have reported midlife women’s experience of CVD-related symptoms, vasomotor symptoms, and subclinical cardiovascular disease progression across the stages of menopause (Thurston et al. 2008; Sutton-Tyrrell et al. 2005). However, ethnic minority midlife women frequently do not recognize cardiovascular symptoms that they experience during their menopausal transition, which could delay seeking timely prevention or treatment for CVDs (McSweeney et al. 2007). Racial/ethnic differences in their cardiovascular symptoms are postulated as a plausible reason for the women’s lack of knowledge and recognition of the symptoms (McSweeney et al. 2007).
Richard-Davis and Wellons (2013) claimed that racial/ethnic differences in hormone levels during the menopausal transition could be subtle, but might still influence the development of racial/ethnic differences in hormonally related diseases, such as CVDs. Also, Sutton-Tyrrell et al. (2005) reported significant racial/ethnic differences in sex hormone-binding globulin (SHBG) and free androgen index (FAI) among a multi-racial/ethnic cohort of premenopausal and peri-menopausal women—higher levels of SHBG and lower levels of FAI among Non Hispanic (NH) African Americans and lower levels of SHBG and higher levels of FAI among Chinese compared with NH Whites. However, very few actual comparative studies on racial/ethnic differences in cardiovascular symptoms experienced during the menopausal transition have been conducted, and most comparative studies have focused on the prevalence and mortality rates of CVDs and/or CVD risk factors among different racial/ethnic groups (Thurston et al. 2008; Frank et al. 2013). Furthermore, most studies have focused on changes in biomarkers, such as aortic pulse-wave velocity, distinct lipid/lipoprotein profiles, and hormone levels rather than actual cardiovascular symptoms (Birru et al. 2011; Taechakraichana et al. 2007).
The purpose of this study was, therefore, to explore racial/ethnic differences in midlife women’s cardiovascular symptom experience among four major racial/ethnic groups in the U.S. This was a secondary analysis of the data from a larger study that included four major racial/ethnic groups of midlife women in the U.S. (Non Hispanic [NH] Whites, Hispanic, NH African Americans, and NH Asians). The specific aims of this analysis were to determine: (a) racial/ethnic differences in cardiovascular symptoms among four major racial/ethnic groups of midlife women in the U.S. (Aim #1), (b) racial/ethnic differences in cardiovascular symptoms by menopausal status (Aim #2), and (c) factors associated with cardiovascular symptoms in each racial/ethnic group (Aim #3).
Definitions and Theoretical Basis
In this paper, “symptom experience” means “subjective experience reflecting changes in the bio-psycho-social functioning, sensations or cognition of an individual”(Dodd et al. 2001, p. 669). Thus, “cardiovascular symptom experience” refers to subjective experience indicating changes in bio-psycho-social functioning, sensations, or cognition of a person that are related to changes in the cardiovascular system (e.g., CVD). CVD means any disease of the cardiovascular systems that includes primarily cardiac diseases, vascular diseases of the brain and kidney, and peripheral arterial diseases (Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease 2010). We included a broad scope of symptoms related to CVD as cardiovascular symptoms, and studied cardiovascular symptoms as women themselves self-reported as in the original study.
The UCSF symptom management model (Dodd et al. 2001) was used to guide this analysis. This model has been widely accepted and used in a number of studies on symptom experience related to various diseases (Dodd et al. 2001). The model includes three major domains: person, health and illness, and environments. These three domains influence three major concepts of the model—symptom experience, symptom management strategies, and outcomes. All of these domains and concepts were supported by evidence from research and practice, and the assumptions of the model have been clearly delineated and supported in the literature (Dodd et al. 2001). Among the major concepts and sub-concepts, we aimed to determine the relation of race/ethnicity—a demographic characteristic of a person—to symptom experience (Aim #1). Also, we aimed to examine the factors related to the major domains of a person (background characteristics), health and illness (health and menopausal status), and environment (acculturation factors)(Aims #2 and 3).
Method
This was a secondary analysis of the data from a national Internet Survey on attitudes toward physical activity among four major racial/ethnic groups of midlife women in the U.S. More information on the original study has been published elsewhere (Authors 2012). The original study was reviewed and approved by the institutional review board of the institution where the authors were affiliated. The data were collected from 2006 to 2011.
Settings and Participants
In the original study, the study announcements were made through Internet communities/groups for racial/ethnic minorities in the U.S. Then, a total of 542 midlife women (157 NH Whites, 127 Hispanics, 135 NH African Americans, and 123 NH Asian) were recruited through the online announcement process. Only the midlife women aged 40 to 60 years who could read and write English, identified themselves as NH White, Hispanic, NH African American, or NH Asian, could participate in all forms of physical activity, and had online access were included. When the women visited the project website and gave their consent to participate, they were checked against the inclusion criteria and the quota requirement using the computer server-side programming. Only those women who met the inclusion criteria and quota requirement were recruited for the study. About 95% of the visitors at the project website participated in the study. Among the 542 participants, 76 women (14.0%) who experienced no menstruation due to severe stress, medication or pregnancy were excluded from the present analyses; thus, a total of 466 women (86.0%) were included. The statistical power for this sample size was determined through a power analysis using the G*power 3.1 program with an effect size of 0.20 (assumed based on a previous study)(Authors 2010), a two-sided alpha level of 0.05, and a power of 0.80. To detect significant racial/ethnic differences in cardiovascular symptoms, a total of 280 participants would be needed. With an effect size of 0.33 (Cohen’s f2) based on a previous study (Authors 2010), 75 participants per racial/ethnic group (n = 300) would be needed for a hierarchical multiple regression analysis with 17 independent variables. Additional power analysis showed that 123 participants in each racial/ethnic group could be adequate to address Aim #3 with an odds ratio of 3.402 (a relatively strong association) based on peri-menopausal status (binomial distribution, and Pr (Y=1 | X=1) H0 = 0.2), with R2 of 0.15, and α = 0.05.
Instruments
In the original study, multiple instruments were used. Only the data from the questions on background characteristics, perceived health and menopausal status and the Midlife Women’s Symptom Index (derived for the Cardiovascular Symptom Index for Midlife Women-CSIMW) were used for this secondary analysis.
Background characteristics, perceived health, and menopausal status
In the original study, multiple questions on age, education, marital status, employment, financial strain (a proxy of family income), number of children, self-reported ethnic identity, race, country of birth, level of acculturation and length of stay in the U.S. (in years) were used to collect the data on the participants’ background characteristics. When a woman was born outside the U.S., her level of acculturation was measured using five items about preferences for foods, music, customs, language, and close friends (1 = exclusively own ethnic group to 5 = exclusively American). The acculturation questions were derived from the Suinn-Lew Asian Self-Identity Acculturation Scale (SL-ASIA; Suinn, Ahuna, & Khoo 1992; Suinn, Rickard-Figueroa, Lew, & Vigil 1987) and used in several previous studies (Authors 2005; 2010; 2012). The average of the five items was used as the level of acculturation. The reliability and validity of the questions were well-established among multi-ethnic groups of midlife women in previous studies (Cronbach’s alpha = 0.84)(Authors 2010). Cronbach’s alpha for these questions in the original study was 0.96.
Financial strain was measured using a question on subjective perception of the adequacy of family income for basic needs, such as food, housing, clothing, and healthcare. Then, financial strain was subsequently categorized into: very hard to pay for basic needs (very low income), somewhat hard to pay for basic needs (somewhat low income), and not hard to pay for basic needs (not low income). Perceived health status was measured using two items on body weight and height and a Likert scale question on perceived general health (1 = very unhealthy to 5 = very healthy). Two questions on diagnosed diseases and medicine were used to measure health status, and seven items about last menstrual cycle, regularity, and flow were used to measure menopausal status. Menopausal status was determined based on the women’s answers to seven questions, and categorized into pre-, peri-, and postmenopausal using criteria adapted from the SWAN (Avis 2001). When a woman had menses in the previous 3 months with no increase in irregularity, she was categorized as pre-menopausal. When a woman had menses in the previous 12 months, but had experienced increasing irregularity in cycle length, she was categorized as peri-menopausal. Finally, when a woman had no menses in the previous 12 months (not due to medication, pregnancy, or severe weight loss), she was categorized as post-menopausal.
The Cardiovascular Symptom Index for Midlife Women (CSIMW)
The CSIMW was derived from the Midlife Women’s Symptom Index (MSI) (Im 2006). The MSI includes 71 items of physical, psychological, and psychosomatic symptoms and is a 25-item sub-scale of the MSI to measure specifically cardiovascular symptoms that women have experienced during the past six months. These 25 items were selected from an extensive literature search through which symptoms associated with CVD were determined (Khan et al. 2013; National Heart, Lung, and Blood Institute 2011). Sample items are: do you feel your heart race? Do you often have difficulty in breathing? Do you ever feel like you are suffocating? Do you often have dizziness? Do you feel your heart race? The CSIMW has two sub-scales: (a) the symptom frequency sub-scale using dichotomous items (1 = yes; 0 = no) and (b) the symptom severity sub-scale using 6-point Likert scale items (0 = no symptom; 5 = extremely). The total numbers of cardiovascular symptoms were calculated by counting the items checked as yes in the frequency sub-scale (ranged from zero to 25). The total severity scores were also calculated by adding the severity of the 25 items (ranged from zero to 125). The Cronbach’s alpha was 0.87 for the symptom frequency subscale, and 0.89 for the symptom severity subscale.
Data Collection Procedures
For the original study, a project website was developed to conform to the Health Insurance Portability and Accountability Act and the SysAdmin, Audit, Network, Security /Federal Bureau of Investigation recommendations. The project website included an informed consent sheet and Internet survey questions. When a woman visited the project website, she was asked to review the informed consent sheet and give her consent to participate by clicking the button of I agree to participate. As mentioned above, after obtaining her consent, the woman was asked about several questions related to the inclusion criteria, and she was also screened against the quota requirement. Only those women who met the inclusion criteria and quota requirement were allowed to enter the Internet survey site. Then, the women were asked to fill out the questions through the Internet. The data were kept confidential, and only the research team had access to the de-identified data. The identity information was separately saved in a locked cabinet in the research office.
Data Analysis
The data were analyzed using the Statistical Package for the Social Sciences 20.0 for Windows (SPSS, Inc., an IBM Company, Chicago, Illinois, USA). All the data from the original study were checked for data-entry accuracy and against the assumptions of the statistical tests that were conducted. Data on background characteristics, menopausal status, and the frequencies and severity of cardiovascular symptoms were analyzed using descriptive statistics and inferential statistics. All statistical analyses were 2-tailed, and a p value < 0.05 was considered to be statistically significant. Chi-square tests were conducted to determine racial/ethnic differences in the frequencies of individual symptoms. Analysis of variance (ANOVA) was performed with post hoc tests using the Duncan’s method to examine racial/ethnic differences in the total numbers and severity scores of cardiovascular symptoms and the severity scores of individual symptoms. Two-way ANOVA with post hoc tests using the Bonferroni’s method was conducted to identify the main effects of racial/ethnic group and menopausal status and the effects of the interaction term race/ethnicity * menopausal status on the total numbers and total severity scores of cardiovascular symptoms. Except for the race/ethnicity * menopausal status interaction, this study did not consider any other interactions in the regression analyses.
Multinomial logistic regression analyses were performed to compare the frequencies and severity scores of individual cardiovascular symptoms among racial/ethnic groups, after controlling for age, body mass index (BMI), menopausal status, and the diagnosis of CVDs. Confounding variables that were reported to be risk factors for CVDs (National Heart, Lung, and Blood Institute, 2011) were controlled and included as covariates. NH Whites were the reference group. Logistic regression analyses were also performed to determine the factors associated with the total severity scores of cardiovascular symptoms for each racial/ethnic group with the Hosmer & Lemeshow goodness of fit test (Cohen, Cohen, West, & Aiken, 2003).
Finally, a Poisson regression analysis was performed to identify significant variables associated with the total number of cardiovascular symptoms. Because the total numbers of cardiovascular symptoms were count-data and the assumption of normal distribution (tested with Kolmogorov-Smirnov test) was violated (p<0 .001), Poisson regression was chosen (Osgood 2000). The likelihood ratio χ2 test was performed to examine the goodness of fit.
Findings
General Characteristics of the Participants
The mean age of the participants was 49.33 years (SD=6.08), and the mean BMI was 28.57 (SD=6.89). Sixty-seven percent of the participants had obtained an education beyond the college level, and 66.5% were married or partnered. Fifty-three percent were post-menopausal, and 19.3% had CVDs (by self-report of a physician ever diagnosing them with CVDs) (Table 1). The CVDs included: hypertension, mitral valve regurgitation, bicuspid aortic valve, murmur, congenital heart malformation, and congestive heart failure.
Table 1.
Characteristics of the participants (N=466).
| n (%) | Mean (SD) | ||
|---|---|---|---|
| Age (years) | 49.33 (6.08) | ||
| BMI (Kg/m2) | 28.57 (6.89) | ||
| Education | ≤High school | 46(9.9) | |
| Partial college | 108 (23.2) | ||
| ≥College graduation | 312 (67.0) | ||
| Marital status | Married/partnered | 310 (66.5) | |
| Single/separated | 156 (33.5) | ||
| Employment | Yes | 361 (77.5) | |
| No | 105 (22.5) | ||
| Financial strain | Very high | 81 (17.4) | |
| Somewhat high | 185 (39.7) | ||
| Not high | 200 (42.9) | ||
| Race/Ethnicity | Non-Hispanic (NH) Whites | 138 (29.6) | |
| Hispanic | 102 (21.9) | ||
| NH Asian | 107 (23.0) | ||
| NH African American | 119 (25.5) | ||
| Menopause | Pre-menopause | 142 (30.5) | |
| Peri-menopause | 75 (16.1) | ||
| Post-menopause | 249 (53.4) | ||
| Cardiovascular | Yes | 90 (19.3) | |
| Diseases | No | 376 (80.7) |
Racial/Ethnic Differences in the Frequencies of Cardiovascular Symptoms (Aim #1)
The mean total number of cardiovascular symptoms was 5.47 (SD=4.83, range 0 – 23) for all participants. Significant racial/ethnic differences were observed in the unadjusted total numbers of cardiovascular symptoms (p<0.01); NH Asians (4.05±4.53) had significantly lower total numbers of cardiovascular symptoms compared to other racial/ethnic groups (p<0.05) (Table 2). The most frequently reported cardiovascular symptoms among all participants were feeling hot or cold (53.6%), neck pain (43.6%), exhaustion (36.9%), and hot flushes (36.9%). Statistically significant racial/ethnic differences were observed in the unadjusted frequencies of neck pain, palpitation, suffocating, joint swelling, night sweats, feeling hot or cold, hot flushes, and exhaustion (p<0.05). Compared to other racial/ethnic groups, NH Whites were more likely to report palpitation (23.2%), feeling hot or cold (60.9%), and exhaustion (46.4%); Hispanics were more likely to report suffocating (12.7%) and joint swelling (16.7%); and NH African Americans were more likely to report night sweats (28.6%) and hot flushes (50.4%). NH Asians had the lowest symptom prevalence across all cardiovascular symptoms, except neck pain in which NH African Americans showed the lowest symptom prevalence. The most frequently reported cardiovascular symptoms were similar across racial/ethnic groups. Feeling hot or cold, shoulder pain, and neck pain were the top three symptoms for NH Whites, Hispanics, and NH Asians while feeling hot or cold, hot flushes, and shoulder pain were the most frequently reported cardiovascular symptoms for NH African Americans.
Table 2.
Frequencies of cardiovascular symptoms by racial/ethnic group (N=466).
| Total | NH White | Hispanic | NH AA | NH Asian | χ2 (p) | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Neck pain | 203 (43.6) | 70(50.7) | 51 (50.0) | 42 (35.3) | 40 (37.4) | 9.570 (0.023) |
| Palpitation | 71 (15.2) | 32 (23.2) | 14 (13.7) | 16 (13.4) | 9 (8.4) | 11.092 (0.011) |
| Suffocating | 30 (6.4) | 9 (6.5) | 13 (12.7) | 5 (4.2) | 3 (2.8) | 8.936 (0.027)¶ |
| Joint swelling | 47 (10.1) | 8 (5.8) | 17 (16.7) | 16 (13.4) | 6 (5.6) | 11.517 (0.009) |
| Night sweats | 91 (19.5) | 35 (25.4) | 14 (13.7) | 34 (28.6) | 8 (7.5) | 21.257 (<0.001) |
| Feeling hot/cold |
250 (53.6) | 84 (60.9) | 52 (51.0) | 71 (59.7) | 43 (40.2) | 12.715 (0.005) |
| Hot flushes | 172 (36.9) | 55 (39.9) | 36 (35.3) | 60 (50.4) | 21 (19.6) | 23.682 (<0.001) |
| Exhaustion | 172 (36.9) | 64 (46.4) | 41 (40.2) | 40 (33.6) | 27 (25.2) | 12.604 (0.006) |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | F (p) | |
| Total frequency |
5.47(4.83) | 6.14(4.80)b | 5.82(5.07)b | 5.68(4.69)b | 4.05(4.53)a | 4.333 (0.005) |
Note. Post hoc tests by Duncan (a <b). CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American.
Fisher’s exact
In the multinomial logistic regression analyses (see Table 3), Hispanics were more likely to report joint swelling (OR=5.23, 95% Confidence Interval [CI] =1.92–14.23) whereas they were less likely to report night sweats (OR=0.37, 95% CI=0.16–0.87) than NH Whites. NH African Americans were more likely to report joint swelling (OR=3.42, 95% CI=1.27–9.19), while they were less likely to report neck pain (OR=0.50, 95% CI=0.28–0.90) and exhaustion (OR=0.52, 95% CI=0.28–0.95) compared to NH Whites. NH Asians were less likely to report night sweats (OR=0.34, 95% CI=0.13–0.93) compared to NH Whites.
Table 3.
Associations of demographic and health characteristics with cardiovascular symptoms by racial/ethnic group (multinomial logistic regression analysis)(N=466).
| Hispanics | NH AA | NH Asian | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age (years) | 0.97 (0.92–1.02) | 0.99 (0.94–1.04) | 0.97 (0.92–1.02) |
| BMI (Kg/m2) | 1.06 (1.01–1.10)* | 1.06 (1.01–1.10)** | 0.81 (0.76–0.87)*** |
| Menopause (post) | |||
| Pre- | 1.30 (0.65–2.60) | 1.25 (0.62–2.51) | 1.35 (0.66–2.75) |
| Peri- | 1.47 (0.67–3.26) | 1.13 (0.53–2.42) | 1.76 (0.77–4.00) |
| CVD (no) | 0.94 (0.45–1.97) | 0.47 (0.24–0.91)* | 0.65 (0.28–1.48) |
| Neck pain | 1.07 (0.59–1.96) | 0.50 (0.28–0.90)* | 0.95 (0.51–1.79) |
| Palpitation | 0.53 (0.24–1.17) | 0.55 (0.26–1.14) | 0.41 (0.16–1.06) |
| Suffocating | 2.62 (0.92–7.41) | 0.61 (0.18–2.07) | 1.18 (0.24–5.77) |
| Joint swelling | 5.23 (1.92–14.23)** | 3.42 (1.27–9.19)* | 2.22 (0.61–8.07) |
| Night sweats | 0.37 (0.16–0.87)* | 1.29 (0.64–2.59) | 0.34 (0.13–0.93)* |
| Feeling hot/cold | 0.67 (0.35–1.26) | 0.86 (0.46–1.61) | 0.70 (0.37–1.34) |
| Hot flushes | 1.37 (0.67–2.80) | 1.89 (0.96–3.72) | 0.76 (0.35–1.67) |
| Exhaustion | 0.58 (0.31–1.10) | 0.52 (0.28–0.95)* | 0.86 (0.43–1.72) |
Notes.
p < 0.05,
p < 0.01,
p < 0.001
Cox & Snell R2 = 0.35, Nagelkerke R2 = 0.37, Likelihood ratio χ2 (p) = 197.92 (p < 0.001).
Reference group for racial/ethnic group = NH Whites, reference group for menopause = post menopause, CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American, OR = Odd ratio, 95% CI = 95% confidence interval.
Racial/Ethnic Differences in the Severity of Cardiovascular Symptoms (Aim #1)
The mean total severity score was 16.10 (SD=16.45, range 0 – 92) for all participants. Significant racial/ethnic differences were observed in the unadjusted mean total severity scores (p<.01); NH Asians (11.64±15.39) had significantly lower total severity scores compared to other racial/ethnic groups (p<.05) (Table 4). The severity scores of neck pain, palpitation, joint swelling, shoulder pain, night sweats, feeling hot or cold, hot flushes, and exhaustion were significantly different by racial/ethnic group (p<0.05). Compared to other racial/ethnic groups, NH Whites were more likely to have severe symptoms of palpitation (0.59±1.13, range 0 – 5), and shoulder pain (1.75±1.73, range 0–5). Hispanics were more likely to have severe joint swelling (0.63±1.44, range 0–5). NH Asians were less likely to have severe symptoms of palpitation (0.21±0.77), shoulder pain (1.10±1.50, range 0–5), feel hot or cold (0.97± 1.31, range 0–5), hot flushes (0.53±1.18, range 0–5), and exhaustion (0.82±1.50, range 0–5) (Table 4).
Table 4.
Severity scores of cardiovascular symptoms by racial/ethnic group (ANOVA)(N=466).
| Total | NH White | Hispanic | NH AA | NH Asian | F (p) | |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Neck pain | 1.23 (1.54) | 1.51 (1.65)b | 1.40 (1.55)b | 0.97 (1.45)a | 0.98 (1.39)a | 4.036 (.008) |
| Palpitation | 0.39 (0.97) | 0.59 (1.13)b | 0.36 (0.96)ab | 0.34 (0.90)ab | 0.21 (0.77)a | 3.290 (.021) |
| Joint swelling | 0.36 (1.13) | 0.20 (0.84)a | 0.63 (1.44)b | 0.50 (1.33)b | 0.18 (0.76)a | 4.401 (.005) |
| Shoulder pain | 1.45 (1.68) | 1.75 (1.73)b | 1.46 (1.75)ab | 1.39 (1.67)ab | 1.10 (1.50)a | 3.100 (.027) |
| Night sweats | 0.60 (1.30) | 0.80 (1.49)b | 0.45 (1.20)a | 0.81 (1.36)b | 0.25 (0.93)a | 5.208 (.002) |
| Feeling hot/cold |
1.45 (1.54) | 1.65 (1.55)b | 1.35 (1.50)ab | 1.75 (1.64)b | 0.97 (1.31)a | 6.056 (<.001) |
| Hot flushes | 1.10 (1.57) | 1.24 (1.67)bc | 1.06 (1.57)b | 1.48 (1.63)c | 0.53 (1.18)a | 7.688 (<.001) |
| Exhaustion | 1.22 (1.70) | 1.50 (1.74)b | 1.42 (1.85)b | 1.08 (1.62)ab | 0.82 (1.50)a | 4.053 (.007) |
| Total severity | 16.10 (16.45) |
18.03 (16.29)b |
17.62 (18.00)b |
16.58 (15.61)b |
11.64 (15.39)a |
3.644 (0.013) |
Notes. Post hoc tests by Duncan (a ≤ab ≤b ≤bc ≤c).
CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American
In the multinomial logistic regression analyses, Hispanics were more likely to report severe joint swelling (OR=1.78, 95% CI=1.33–2.38), whereas they were less likely to report severe shoulder pain (OR=0.80, 95% CI=0.64–0.99) than NH Whites. NH African Americans were more likely to report severe joint swelling (OR=1.53, 95% CI=1.15–2.04) and less likely to report severe neck pain (OR=0.80, 95% CI=0.64–0.99) and severe exhaustion (OR=0.83, 95% CI=0.69–1.00) compared to NH Whites (Table 5).
Table 5.
Total severity scores of cardiovascular symptoms by racial/ethnic group (multinomial logistic regression analysis)(N=466).
| Hispanics | NH AA | NH Asian | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 0.97 (0.93–1.02) | 0.99 (0.94–1.04) | 0.98 (0.93–1.03) |
| BMI (Kg/m2) | 1.05 (1.01–1.10)* | 1.05 (1.01–1.10)* | 0.80 (0.75–0.86)*** |
| Menopause (post) | |||
| Pre- | 1.38 (0.69–2.74) | 1.21 (0.60–2.43) | 1.40 (0.68–2.85) |
| Peri- | 1.56 (0.71–3.47) | 1.30 (0.61–2.79) | 1.91 (0.83–4.37) |
| CVD (no) | 0.66 (0.41–1.76) | 0.45 (0.23–0.88)* | 0.60 (0.26–1.37) |
| Neck pain | 1.06 (0.85–1.33) | 0.80 (0.64–0.99)* | 1.01 (0.80–1.28) |
| Palpitation | 0.89 (0.66–1.20) | 0.83 (0.63–1.11) | 0.73 (0.51–1.04) |
| Joint swelling | 1.78 (1.33–2.38)*** | 1.53 (1.15–2.04)* | 1.34 (0.91–1.97) |
| Shoulder pain | 0.80 (0.64–0.99)* | 0.88 (0.72–1.08) | 0.85 (0.68–1.07) |
| Night sweats | 0.78 (0.59–1.02) | 1.00 (0.79–1.27) | 0.79 (0.56–1.09) |
| Feeling hot/cold | 0.92 (0.73–1.16) | 1.10 (0.88–1.37) | 0.90 (0.70–1.14) |
| Hot flushes | 1.08 (0.85–1.39) | 1.12 (0.89–1.42) | 0.88 (0.66–1.16) |
| Exhaustion | 0.95 (0.78–1.15) | 0.83 (0.69–1.00)* | 1.07 (0.86–1.33) |
Notes. Cox & Snell R2 = 0.34, Nagelkerke R2 = 0.36, Likelihood ratio χ2 (p) = 194.19 (p < 0.001).
p < 0.05,
p < 0.01,
p < 0.001.
Reference group = NH Whites, CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American, OR = Odd ratio, 95% CI = 95% confidence interval.
Covariates included in the model: age, BMI, menopause, and CVD
Racial/Ethnic Differences in Cardiovascular Symptoms by Menopausal Status (Aim #2)
Pre-menopausal women had lower total numbers and total severity scores than peri- and post-menopausal women across racial/ethnic groups. NH Asians had significantly lower total numbers and total severity scores of cardiovascular symptoms than Hispanics and NH Whites. The main effects of race/ethnicity were not significant (p>0.05), while the main effects of menopausal status were significant for both total numbers and total severity scores of cardiovascular symptoms (p<0.05). Interaction between race/ethnicity and menopausal status was significant for the total severity scores of cardiovascular symptoms (p<0.05) (Table 6).
Table 6.
Total numbers and total severity scores of cardiovascular symptoms by menopausal status and racial/ethnic groups.
| Total numbers | Menopausal Status | F (p) | |||
|---|---|---|---|---|---|
| Prea | Perib | Postb | |||
| M (SD) | M (SD) | M (SD) | |||
| NH White | 4.31 (4.15) | 7.76 (5.90) | 6.50 (4.58) | Ethnicity | 2.06 (0.105) |
| Hispanic | 4.05 (3.39) | 4.69 (4.57) | 7.32 (5.69) | Menopause | 7.62 (0.001) |
| NH AA | 5.17 (4.25) | 5.84 (4.62) | 5.85 (4.93) | Ethnic * meno | 1.81 (0.095) |
| NH Asian | 3.02 (3.62) | 6.53 (5.68) | 4.07 (4.50) | ||
| Total severity |
Menopause | F (p) | |||
| Prea | Perib | Postb | |||
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| NH Whiteb | 12.86 (13.57) | 24.62 (19.79) | 18.55 (15.87) | Ethnicity | 1.90 (0.129) |
| Hispanicb | 10.94 (10.27) | 13.44 (13.29) | 23.27 (21.29) | Menopause | 6.96 (0.001) |
| NH AAab | 15.52 (14.89) | 15.95 (14.60) | 17.18 (16.31) | Ethnic * meno | 2.18 (0.044) |
| NH Asiana | 8.00 (11.77) | 19.53 (20.02) | 12.05 (15.37) | ||
Notes. Post hoc tests by Bonferroni (a < b).
Covariates included in the model: financial strain, BMI, and CVD.
CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American
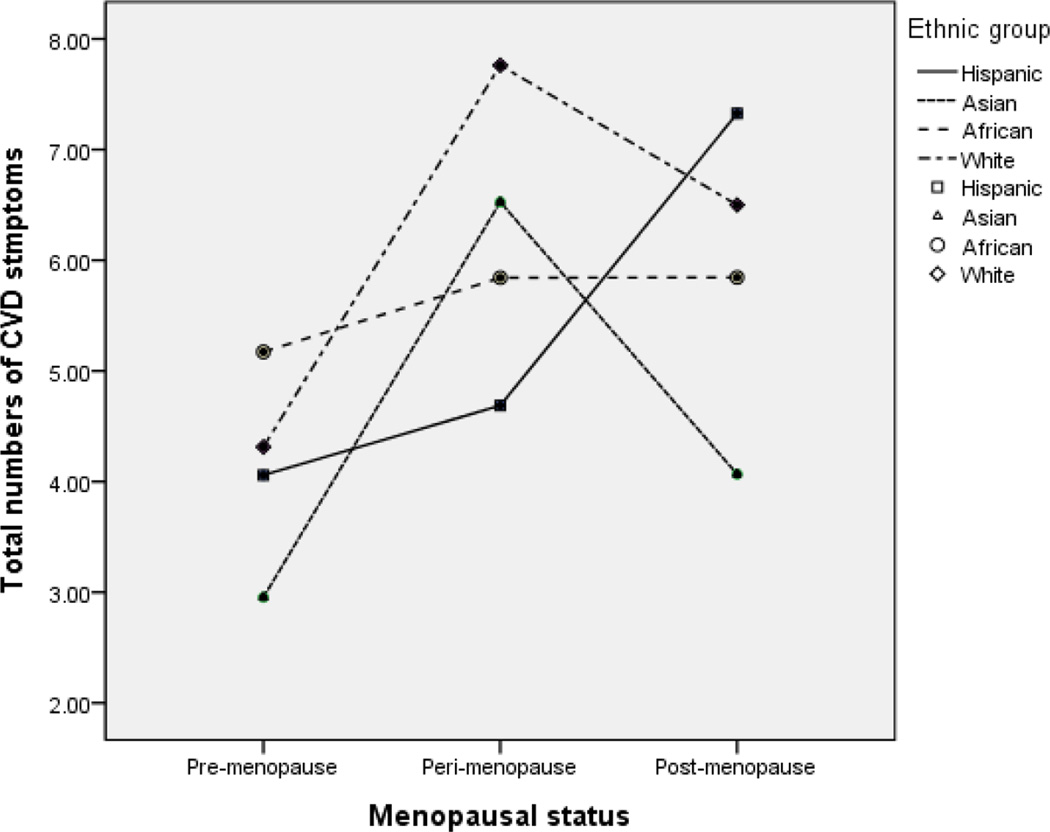
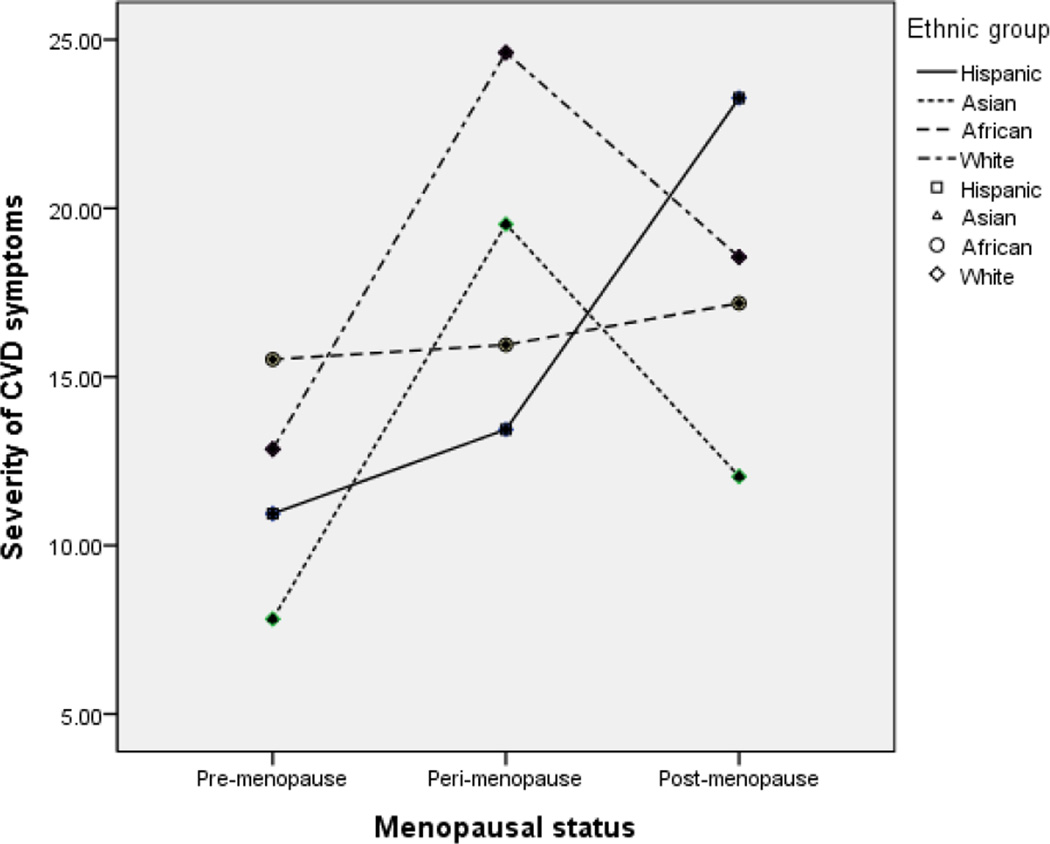
Subsequent ANOVA and post hoc tests by Duncan were performed to identify changes in the total numbers and severity scores of cardiovascular symptoms by menopausal transition status. The results showed that, among NH Whites and NH Asians, the total numbers and severity scores peaked in the peri-menopausal period and decreased in the post-menopausal period (p<0.05)(see Figures 1 and 2). Among Hispanics, the total numbers and severity scores continued to increase throughout the menopausal transition, and post-menopausal women had the highest total numbers and severity scores (p<0.05). Among NH African Americans, the total numbers and severity scores of cardiovascular symptoms were not significantly different across the menopausal transition (p>0.05)(Figures 1 & 2).
Figure 1.
Total numbers of cardiovascular symptoms by menopausal status and race/ethnicity
Figure 2.
Total severity scores of cardiovascular symptoms by menopausal status and race/ethnicity
Factors Associated with the Total Number of Cardiovascular Symptoms (Aim #3)
Across the racial/ethnic groups, education (no college degree), financial strain (very low and somewhat low), BMI, peri-menopausal status, and the use of medication were positively associated with the total number of cardiovascular symptoms while pre-menopausal status was negatively associated with them (p<0.05). For every one unit increases in independent variables (e.g., BMI), the log count of the total numbers of cardiovascular symptoms was expected to increase by the regression coefficients (β= 0.01 for BMI). Among NH Whites, education (no college degree), high financial strain, employment, BMI, and the use of medication were positively associated with the total number of cardiovascular symptoms while age and pre-menopausal status were negatively associated (p<0.05). Among Hispanics, somewhat high financial strain, BMI, and the use of medication were positively associated with the total number of cardiovascular symptoms, while marital status (married/partnered) and employment were negatively associated (p<0.05). Among NH African Americans, very high and somewhat high financial strain were positively associated with the total number of cardiovascular symptoms. Among NH Asians, age, very high financial strain, peri-menopausal status, and the use of medication were positively associated with the total number of cardiovascular symptoms, whereas employment was negatively associated (p<0.05) (Table 7).
Table 7.
Factors associated with the total number of cardiovascular symptoms by racial/ethnic group.
| Factors | Total (N=466) |
NH White (n=138) |
Hispanic (n=102) |
NH AA (n=119) |
NH Asian (n=107) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | p | B | p | B | p | B | p | B | p | |
| Age | 0.00 | 0.971 | −0.02 | 0.003 | 0.02 | 0.068 | 0.01 | 0.143 | 0.03 | 0.002 |
| Education (no college) | 0.10 | 0.030 | 0.21 | 0.010 | −0.02 | 0.871 | 0.12 | 0.206 | −0.04 | 0.751 |
| Marital status (married) | −0.01 | 0.844 | 0.12 | 0.171 | −0.19 | 0.039 | −0.08 | 0.339 | 0.25 | 0.079 |
| Financial strain (not high) |
||||||||||
| Very high | 0.44 | <0.001 | 0.50 | <0.001 | 0.02 | 0.889 | 0.27 | 0.042 | 1.03 | <0.001 |
| Somewhat high | 0.22 | <0.001 | 0.16 | 0.110 | 0.25 | 0.011 | 0.31 | 0.001 | 0.21 | 0.090 |
| Employment (yes) | −0.06 | 0.184 | 0.18 | 0.041 | −0.32 | 0.003 | 0.10 | 0.366 | −0.25 | 0.024 |
| BMI (kg/m2) | 0.01 | 0.001 | 0.01 | 0.027 | 0.02 | 0.014 | 0.00 | 0.796 | 0.02 | 0.357 |
| Menopause (post) | ||||||||||
| Pre | −0.28 | <0.001 | −0.36 | <0.001 | −0.23 | 0.054 | 0.01 | 0.961 | −0.10 | 0.459 |
| Peri | 0.12 | 0.025 | 0.15 | 0.119 | −0.04 | 0.806 | 0.02 | 0.860 | 0.74 | <0.001 |
| CVD (no) | −0.09 | 0.074 | −0.04 | 0.679 | −0.04 | 0.688 | −0.14 | 0.143 | −0.07 | 0.640 |
| Medication (no) | −0.35 | <0.001 | −038 | <0.001 | −0.65 | <0.001 | 0.02 | 0.856 | −0.32 | 0.006 |
| Acculturation | 0.01 | 0.177 | −0.01 | 0.863 | 0.01 | 0.321 | 0.03 | 0.246 | −0.01 | 0.602 |
| Log likelihood | −1538.01 | −428.65 | −309.12 | −404.71 | −322.63 | |||||
| LR χ2 | 299.23*** | 121.18*** | 138.93*** | 27.62*** | 102.49*** | |||||
Notes. CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American, BMI = body mass index.
Factors Associated with the Severity of Cardiovascular Symptoms (Aim #3)
Participants were divided into two groups using the mean total severity scores of individual racial/ethnic group. Based on the mean severity scores, we divided the total group and each racial/ethnic group into two groups (low versus high CVD symptom severity groups). For example, the mean severity score of CVD symptoms was 18.03 for NH Whites. Thus, those with the mean severity scores of at least 19 were categorized into the high CVD symptom severity group, and those with the mean severity scores of less than or equal to 18 were categorized into the low CVD symptom severity group. The CVD symptom severity scores for all participants were whole numbers. Multiple logistic regression analyses revealed that among all participants, very high (OR=3.71, 95% CI=1.97–6.99) and somewhat high financial strain (OR=1.84, 95% CI=1.14–2.97) and no medication (OR=0.43, 95% CI= 0.27–0.69) were significantly positively and negatively, respectively, associated with the total severity scores of cardiovascular symptoms. Among NH Whites, very high financial strain (OR=4.39, 95% CI=1.38–14.01) and no medication (OR=0.29, 95% CI=0.12–0.72) were significantly positively and negatively, respectively, associated with total severity scores. Among Hispanics, employment (OR=0.19, 95% CI=0.04–0.83) was significantly negatively associated. Among NH Asians, very high financial strain (OR=7.82, 95% CI=1.30–47.10) and peri-menopausal status (OR=4.55, 95% CI= 1.08–19.11) were significantly positively associated with severity scores for cardiovascular symptoms. Among NH African Americans, none of the variables was significantly associated with the total severity scores of cardiovascular symptoms (p>0.05). The Hosmer and Lemeshow goodness of fit tests indicated that all the logistic regression models had an acceptable fit (p>0.05), except for NH Whites and Hispanics (Table 8).
Table 8.
Factors associated with total severity scores of cardiovascular symptoms by racial/ethnic group.
| Total (N=466) |
NH White (n=138) |
Hispanic (n=102) |
NH AA (n=119) |
NH Asian (n=107) |
|
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age (years) | 1.01 (0.97–1.05) | 0.96 (0.89–1.02) | 1.03 (0.94–1.14) | 1.05 (0.97–1.13) | 1.10 (0.99–1.21) |
| Education (≥ college) | |||||
| ≤ High school | 1.19 (0.75–1.89) | 2.29 (0.90–5.82) | 0.87 (0.27–2.83) | 1.33 (0.53–3.36) | 1.73 (0.47–6.28) |
| Marital status (single) | |||||
| Married/partnered | 0.79 (0.51–1.23) | 1.13 (0.45–2.84) | 0.63 (0.22–1.80) | 0.65 (0.28–1.48) | 1.35 (0.37–5.02) |
| Financial strain | |||||
| (sufficient) | 3.71 (1.97–6.99)*** | 4.39 (1.38–14.01)* | 0.90 (0.16–5.24) | 2.80 (0.72–10.89) | 7.82 (1.30–47.10)* |
| Very high | 1.84 (1.14–2.97)* | 1.72 (0.61–4.90) | 2.51 (0.82–7.73) | 2.03 (0.82–5.04) | 0.96 (0.29–3.19) |
| Somewhat high | |||||
| Employment (yes) | 0.70 (0.42–1.16) | 1.47 (0.54–3.99) | 0.19 (0.04–0.83)* | 1.50 (0.48–4.69) | 0.80 (0.27–2.34) |
| BMI (≥ 25 Kg/m2) | |||||
| < 25 Kg/m2 | 0.70 (0.44–1.11) | 0.51 (0.22–1.15) | 0.20 (0.04–1.14) | 1.78 (0.65–4.86) | 1.02 (0.32–3.25) |
| Menopause (post) | |||||
| Pre- | 0.65 (0.38 – 1.12) | 0.74 (0.27–2.06) | 0.49 (0.13–1.90) | 1.61 (0.54–4.80) | 0.54 (0.15–1.91) |
| Peri- | 1.24 (0.69 – 2.23) | 0.95 (0.30 – 2.99) | 1.41 (0.32 – 6.13) | 0.98 (0.30–3.22) | 4.55 (1.08–19.11)* |
| Cardiology (no) | 0.89 (0.52–1.52) | 0.89 (0.31–2.55) | 0.57 (0.16–2.04) | 1.05 (0.40–2.76) | 1.61 (0.33–7.76) |
| Medication (no) | 0.43 (0.27 – 0.69)*** | 0.29 (0.12 – 0.72)** | 0.38 (0.11 – 1.33) | 0.76 (0.28 – 2.02) | 0.75 (0.24 – 2.32) |
| Acculturation | 1.03 (0.98 – 1.09) | 1.34 (0.66 – 2.72) | 1.03 (0.92 – 1.16) | 1.09 (0.82 – 1.44) | 0.93 (0.84 – 1.03) |
| Cox & Snell R2 | .13 | .18 | .27 | .08 | .21 |
| Nagelkerke R2 | .18 | .26 | .37 | .10 | .30 |
| Hosmer/Lemeshow χ2 (p) | 13.93(.084) | 18.35(.019) | 18.22(.020) | 4.17(.842) | 3.36(.910) |
Notes. CVD = Cardiovascular disease, NH = Non-Hispanic, AA = African American, BMI = body mass index.
Groups were divided using the mean CVD symptom severity score for each racial/ethnic group: Asians (11 ≥ low CVD symptom severity, 11 < high CVD symptom severity); Total group and African Americans (16 ≥ low CVD symptom severity, 16 < high CVD symptom severity); and Hispanics (17 ≥ low CVD symptom severity, 17 < high CVD symptom severity), and Whites (18 ≥ low CVD symptom severity, 18 < high CVD symptom severity).
p < 0.05,
p < 0.01,
p < 0.001
Discussion
The findings of this study agree with those in the literature; significant racial/ethnic differences were observed in the total numbers and total severity scores of cardiovascular symptoms experienced during the menopausal transition, and significant interactions were observed between race/ethnicity and menopausal status in their relations to cardiovascular symptoms. Indeed, the literature supported significant racial/ethnic differences in the prevalence and mortality rates of CVDs and/or CVD risk factors (Frank et al. 2013). Our findings suggest significant racial/ethnic differences in cardiovascular symptoms that midlife women might experience during the menopausal transition. Some studies also indicated racial/ethnic differences in hormone trajectories during menopausal transition (Richard-Davis and Wellons 2013; Weiss et al. 2004; Randolph et al 2003), which may partially explain racial/ethnic differences in cardiovascular symptoms experienced by midlife women.
The directions of the racial/ethnic differences that were found in this study, however, were somewhat different from those in the literature. In most studies, ethnic minority groups tended to have higher prevalence and mortality rates of CVDs and/or CVD risk factors (Frank et al. 2013). From these findings, it can be inferred that ethnic minorities would have higher frequencies and severity of cardiovascular symptoms during the menopausal transition. Yet, in these secondary analyses, the racial/ethnic differences in the cardiovascular symptoms totally depended on the types of symptoms. In some symptoms, NH Whites tended to have higher frequencies and severity compared with other racial/ethnic groups, while they tended to have lower frequencies and severity in other symptoms. However, these findings have largely been missing in the literature, which necessitates further exploration on racial/ethnic differences in cardiovascular symptoms that are experienced during the menopausal transition.
The finding that NH Asian women tended to have lower frequencies and severity of cardiovascular symptoms agrees with the literature (Frank et al. 2013) but has rarely been reported. In the study of Frank et al. (2013), compared with NH Whites, all racial/ethnic minority groups tended to have a higher prevalence of low HDL-C, except for Japanese Americans and African Americans. Also, literature reveals that NH Asians experienced lower frequencies and severity of menopausal symptoms than other racial/ethnic groups (Im 2003; Gold et al., 2006). Richard-Davis and Wellons (2013) reported that NH Asian women’s estradiol levels were significantly lower than NH White women, which implies that their cardiovascular symptoms could be less frequent and less severe compared with NH White women. Randolph et al. (2003) also reported that Chinese women had lower unadjusted serum estradiol and sex hormone-binding globulin levels than other racial/ethnic groups even after adjusting for body size.
The finding that the total numbers and severity scores peaked in the peri-menopausal period and decreased in the post-menopausal period agrees with the literature (Pérez et al. 2009). Also, the finding that pre-menopausal women had lower total numbers and total severity scores than peri- and post-menopausal women across racial/ethnic groups concurs with the literature. As mentioned above, the menopausal transition brings about several biological and psychosocial changes that are frequently linked to increased cardiovascular risks, subsequently making midlife women experience cardiovascular symptoms that they did not experience previously (Pérez et al. 2009). Changes in estrogen levels are reportedly associated with hardening of the arteries, elevations in LDL cholesterol, and elevated triglycerides, subsequently increasing CVD risks (Rosano et al. 2007). Thus, peri-menopausal women with estrogen fluctuation would be the group who are more likely to experience cardiovascular symptom compared with others.
The factors associated with cardiovascular symptoms were different in each racial/ethnic group, although education, financial strain, BMI, and use of medication were significantly related to symptom reporting in all participants. Only financial strain was significantly associated with the total number of cardiovascular symptoms in all racial/ethnic groups. This finding agrees with the literature, which indicates socioeconomic status is a significant factor associated with CVDs, CVD risk factors, and cardiovascular symptoms. Shaw et al. (2008) indicated that income was significantly associated with CVD outcomes of women with chest pain symptoms. Wang et al. (2013) reported significant differences between midlife women with CVD and those without CVD in several demographic characteristics, including family income. Shishehbor et al. (2006) also reported that socioeconomic status was significantly associated with functional capacity and heart rate recovery. However, the factors associated with cardiovascular symptoms in each racial/ethnic group have not been clearly determined yet.
Some significant differences by racial/ethnic group were not significant after controlling age, BMI, menopausal status, and the diagnosis of CVDs, which suggests that health covariates account for some of the racial/ethnic differences in cardiovascular symptoms experienced by midlife women during the menopausal transition. However, because of the inherent nature of a secondary analysis, no further analysis and/or interpretation were possible in this study.
A plausible reason for the racial/ethnic differences in CVDs has been postulated as the racial/ethnic minorities’ unique cultural attitudes toward CVDs. As recent studies among ethnic minorities have shown, culture can shape their attitudes toward CVDs, and they can define their own experience of CVDs differently according to their culture (Tindle, Davis, and Kuller 2010). For example, in Korean culture, a heart attack is perceived as a disease of higher social class people who eat meats more frequently than lower social class people. These cultural attitudes have been influenced by Western culture, and migrations to the U.S. have assimilated Korean Americans to the U.S. culture. However, these attitudes still continue among Korean Americans, especially middle-aged and elderly populations. Not taking this cultural attitude into account may frustrate the promotion of cardiovascular health among Korean Americans. Likewise, the racial/ethnic differences in individual cardiovascular symptoms may need to be interpreted while considering the cultural contexts and attitudes related to CVDs in different cultures.
This study had several limitations. First of all, the generalizability of the findings was limited because the participants tended to be highly educated, married, and employed women. Some potential bias was also possible from participants being a member in an Internet community/group. Furthermore, the participants might not represent all the sub-ethnic groups within each of the major racial/ethnic groups. Because only those who could engage in all possible forms of physical activity were included, more severely ill individuals who could be disproportionally from racial/ethnic minority groups might have been excluded. In addition, some unauthentic cases might have been included although several measures were adopted to prevent unauthentic cases. Since only self-reports were used to collect the data, no objective validation of the self-reports was available, which could have resulted in misclassification of symptoms and diseases. Furthermore, the acculturation scale used was originally developed for Asian populations, although it was used in multiple ethnic groups of midlife women in previous studies. Also, the symptom item of feeling hot or cold in the CSIMW could have some conceptual overlap with hot flushes. Additionally, the statistically significant racial/ethnic differences that were reported in this paper need to be carefully interpreted because the clinical meanings of the racial/ethnic differences are not clear at this point. Finally, the cross-sectional design of the original study did not permit assessment of temporal and thus potentially causal relations of demographic, behavioral, and health factors to symptoms and diseases reported.
Conclusion
This study clearly revealed significant racial/ethnic differences in the total numbers and total severity scores of cardiovascular symptoms that were experienced by midlife women, yet these differences totally depended on the type of symptoms. Also, significant racial/ethnic differences were observed in cardiovascular symptoms by menopausal status. Financial strain was the common factor associated with cardiovascular symptoms across racial/ethnic groups, but specific factors associated with cardiovascular symptoms were somewhat different in each group. Based on the findings, we conclude this paper with the following implications for future research. First, further studies on racial/ethnic differences in cardiovascular symptoms experienced by midlife women and their associated demographic, health, and lifestyle factors are needed with more in-depth cultural studies on possible reasons for the differences. Also, the participants of the original study did not represent sub-ethnic variations in each major racial/ethnic group, and generalizability was limited. Thus, further studies are needed with diverse groups of various sub-ethnic groups, which would give a more generalizable understanding of the racial/ethnic differences.
Acknowledgments
This is a secondary analysis of the data from a larger study funded by the National Institutes of Health (NIH/NINR/NHLBI; R01NR010568). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Authors. Menopausal Symptoms Among Four Major Ethnic Groups in the U.S. Western Journal of Nursing Research. 2010;32:540–565. doi: 10.1177/0193945909354343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avis NE, Stellato R, Crawford S, Bromberger J, Ganz P, Cain V, Kagawa-Singer M. Is There a Menopausal Syndrome? Menopausal Status and Symptoms across Racial/ethnic Groups. Social Science & Medicine. 2001;52:345–356. doi: 10.1016/s0277-9536(00)00147-7. [DOI] [PubMed] [Google Scholar]
- Birru MS, Matthews KA, Thurston RC, Brooks MM, Ibrahim S, Barinas-Mitchell E, Janssen I, Sutton-Tyrrell K SWAN Heart Study. African-American Ethnicity and Cardiovascular Risk Factors Are Related to Aortic Pulse-Wave Velocity Progression. American Journal of Hypertension. 2011;24:809–815. doi: 10.1038/ajh.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, Lee K, et al. Advancing the Science of Symptom Management. Journal of Advanced Nursing. 2001;33:668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- Frank TAH, Zhao B, Jose PO, Azar KMJ, Fortmann SP, Palaniappan LP. Racial/Ethnic Differences in Dyslipidemia Patterns. Circulation. 2013;129:570–579. doi: 10.1161/CIRCULATIONAHA.113.005757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold EB, Colvin A, Avis N, Bromberger J, Greendale GA, Powell L, Sternfeld B, Matthews K. Longitudinal analysis of vasomotor symptoms and race/ethnicity across the menopausal transition. Am J Public Health. 2006;96:1226–1235. doi: 10.2105/AJPH.2005.066936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im EO. Symptoms Experienced during Menopausal Transition: Korean Women in South Korea and the United States. Journal of Transcultural Nursing. 2003;14:321–328. doi: 10.1177/1043659603257160. [DOI] [PubMed] [Google Scholar]
- Im EO. The Midlife Women’s Symptom Index (MSI) Health Care for Women International. 2006;27:268–287. doi: 10.1080/07399330500506600. [DOI] [PubMed] [Google Scholar]
- Im EO, Lee B, Chee W, Brown A, Dormire S. Menopausal Symptoms Among Four Major Ethnic Groups in the U.S. Western Journal of Nursing Research. 2010;32:540–565. doi: 10.1177/0193945909354343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im EO, Shin HJ, Chee W. Characteristics of Midlife Women Recruited through Internet Communities/groups. Computers, Informatics, Nursing. 2008;26:39–48. doi: 10.1097/01.NCN.0000304760.49048.d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indhavivadhana S, Rattanachaiyanont M, Wongvananurak T, Kanboon M, Techatraisak K, Leerasiri P, Tanmahasamut P, Angsuwathana S. Predictors for Metabolic Syndrome in Perimenopausal and Postmenopausal Thai Women. Climacteric. 2011;14:58–65. doi: 10.3109/13697137.2010.481735. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- Khan NA, Daskalopoulou SS, Karp I, Eisenberg MJ, Pelletier R, Tsadok MA, Dasgupta K, Norris CM, Pilote L GENESIS PRAXYTeam. Sex Differences in Acute Coronary Syndrome Symptom Presentation in Young Patients. JAMA Internal Medicine. 2013;173:1863–1871. doi: 10.1001/jamainternmed.2013.10149. [DOI] [PubMed] [Google Scholar]
- McSweeney JC, Leanne LL, Fischer EP, Naylor AJ, Jr, Evans LK. Women’s Prehospital Delay Associated with Myocardial Infarction: Does Race Really Matter? The Journal of Cardiovascular Nursing. 2007;22:279–285. doi: 10.1097/01.JCN.0000278958.98124.6e. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States 2005. Hyattsvile, MD: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- National Heart, Lung, and Blood Institute. What Are the Signs and Symptoms of Heart Disease? 2011 http://www.nhlbi.nih.gov/health/health-topics/topics/hdw/signs.html.
- Osgood DW. Poisson-Based Regression Analysis of Aggregate Crime Rates. Journal of Quantitative Criminology. 2000;16:21–43. [Google Scholar]
- Ouyang X, Lou Q, Gu L, Mo Y, Nan JH, Kong AP, So WY, et al. Cardiovascular Disease Risk Factors Are Highly Prevalent in the Office-Working Population of Nanjing in China. International Journal of Cardiology. 2012;155:212–216. doi: 10.1016/j.ijcard.2010.09.052. [DOI] [PubMed] [Google Scholar]
- Randolph JF, Jr, Sowers MF, Gold EB, Mohr BA, Luborsky J, Santoro N, McConnell DS, et al. Reproductive Hormones in the Early Menopausal Transition: Relationship to Ethnicity, Body Size, and Menopausal Status. The Journal of Clinical Endocrinology and Metabolism. 2003;88:1516–1522. doi: 10.1210/jc.2002-020777. [DOI] [PubMed] [Google Scholar]
- Richard-Davis G, Wellons M. Racial and Ethnic Differences in the Physiology and Clinical Symptoms of Menopause. Seminars in Reproductive Medicine. 2013;31:380–386. doi: 10.1055/s-0033-1348897. [DOI] [PubMed] [Google Scholar]
- Rosano GMC, Vitale C, Marazzi G, Volterrani M. Menopause and Cardiovascular Disease: The Evidence. Climacteric. 2007;10(Suppl 1):19–24. doi: 10.1080/13697130601114917. [DOI] [PubMed] [Google Scholar]
- Shaw LJ, Merz CNB, Bittner V, Kip K, Johnson BD, Reis SE, Kelsey SF, et al. Importance of Socioeconomic Status as a Predictor of Cardiovascular Outcome and Costs of Care in Women with Suspected Myocardial Ischemia. Journal of Women’s Health. 2008;17:1081–1092. doi: 10.1089/jwh.2007.0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shishehbor MH, Litaker D, Pothier CE, Lauer MS. Association of Socioeconomic Status with Functional Capacity, Heart Rate Recovery, and All-Cause Mortality. JAMA. 2006;295:784–792. doi: 10.1001/jama.295.7.784. [DOI] [PubMed] [Google Scholar]
- Sutton-Tyrrell K, Wildman RP, Matthews KA, Chae C, Lasley BL, Brockwell S, Pasternak RC, et al. Sex-Hormone-Binding Globulin and the Free Androgen Index Are Related to Cardiovascular Risk Factors in Multiethnic Premenopausal and Perimenopausal Women Enrolled in the Study of Women Across the Nation (SWAN) Circulation. 2005;111:1242–1249. doi: 10.1161/01.CIR.0000157697.54255.CE. [DOI] [PubMed] [Google Scholar]
- Taechakraichana N, Holinka CF, Haines CJ, Subramaniam R, Tian XW, Ausmanas MK. Distinct Lipid/lipoprotein Profiles and Hormonal Responsiveness in Nine Ethnic Groups of Postmenopausal Asian Women: The Pan-Asia Menopause (PAM) Study. Climacteric: The Journal of the International Menopause Society. 2007;10:225–237. doi: 10.1080/13697130701352375. [DOI] [PubMed] [Google Scholar]
- Thurston RC, Sutton-Tyrrell K, Everson-Rose SA, Hess R, Matthews KA. Hot Flashes and Subclinical Cardiovascular Disease: Findings from the Study of Women’s Health Across the Nation Heart Study. Circulation. 2008;118:1234–1240. doi: 10.1161/CIRCULATIONAHA.108.776823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle H, Davis E, Kuller L. Attitudes and Cardiovascular Disease. Maturitas. 2010;67:108–113. doi: 10.1016/j.maturitas.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical ctivity Guidelines for Americans. [Accessed April 15];2013 http://www.health.gov/paguidelines/guidelines/
- Wang HL, Tai MK, Hung HM, Chen CH. Unique Symptoms at Midlife of Women with Osteoporosis and Cardiovascular Disease in Taiwan. Menopause. 2013;20:315–321. doi: 10.1097/GME.0b013e31826d30f2. [DOI] [PubMed] [Google Scholar]
- Weiss G, Skurnick JH, Goldsmith LT, Santoro NF, Park SJ. Menopause and Hypothalamic-Pituitary Sensitivity to Estrogen. JAMA. 2004;292:2991–2996. doi: 10.1001/jama.292.24.2991. [DOI] [PubMed] [Google Scholar]