Abstract
Purpose:
Low temporal latency between a gating ON/OFF signal and the LINAC beam ON/OFF during respiratory gating is critical for patient safety. Here the authors describe a novel method to precisely measure gating lag times at high temporal resolutions.
Methods:
A respiratory gating simulator with an oscillating platform was modified to include a linear potentiometer for position measurement. A photon diode was placed at linear accelerator isocenter for beam output measurement. The output signals of the potentiometer and diode were recorded simultaneously at 2500 Hz with an analog to digital converter for four different commercial respiratory gating systems. The ON and OFF of the beam signal were located and compared to the expected gating window for both phase and position based gating and the temporal lag times extracted.
Results:
For phase based gating, a real-time position management (RPM) infrared marker tracking system with a single camera and a RPM system with a stereoscopic camera were measured to have mean gate ON/OFF lag times of 98/90 and 86/44 ms, respectively. For position based gating, an AlignRT 3D surface system and a Calypso magnetic fiducial tracking system were measured to have mean gate ON/OFF lag times of 356/529 and 209/60 ms, respectively.
Conclusions:
Temporal resolution of the method was high enough to allow characterization of individual gate cycles and was primary limited by the sampling speed of the data recording device. Significant variation of mean gate ON/OFF lag time was found between different gating systems. For certain gating devices, individual gating cycle lag times can vary significantly.
Keywords: respiratory gating, time delay, gated radiotherapy
1. INTRODUCTION
Respiratory motion management is recommended when a target receiving radiation therapy is likely to have intrafraction motion of more than 5 mm.1 One method of achieving motion management is through respiratory gating, which can potentially reduce the planning target volume (PTV) margin and therefore reduce normal tissue toxicity. With a respiratory gating system, its ability to turn a linear accelerator (LINAC) ON and OFF accurately at a certain point of a respiratory cycle is required in order to avoid any risk of missing the target.
The American Association of Physicists in Medicine (AAPM) Task Group 142 recommends annual measurements of temporal resolution when the LINAC beam ON and OFF timing is triggered by an external tracking mechanism.2 The temporal accuracy of the measurement should be able to distinguish a value that is within 100 ms from a baseline value determined at commissioning. Current methods of determining a gating system’s temporal characteristics have relied on the use of a moving phantom and radiographic film.3–6 However, such methods are highly susceptible to error as they rely on visual identification of gated treatment field edges on film. Depending on the speed at which the motion phantom moves the film, significant blurring of field edges can occur. Additionally, beam penumbra, film processing, and the skill of the user in measuring edge positions can make the process highly qualitative. Also, depending on film sensitivity, exposure of the film to several beam gating cycles may be necessary to increase contrast to sufficient levels as to make edge identification possible. In this case, only the mean gating response time of the system is given, leading to loss of information on the timing response of individual gate cycles which may deviate significantly from the mean.
We present a novel method to precisely measure end-to-end gating response times (gating system + LINAC system) at high temporal resolutions. The method is demonstrated for both phase and position based gating using four commercial gating systems. The method can be easily generalized to perform temporal lag measurements on any system where a radiation beam is triggered based on external tracking measurements of patient motion.
2. METHODS
A commercial motion platform (Standard Imaging, WI) was modified by fixing a 10 kΩ potentiometer with 100 mm of travel (PTF01-152A-103B2, Bourns, Riverside, CA) to its side (Fig. 1). The position of the motion phantom was determined by converting mechanical motion to a voltage signal through use of this potentiometer. The potentiometer was incorporated into a Wheatstone bridge circuit in order to null out its baseline voltage for better dynamical range before connection to channel 1 of an oscilloscope (Tektronix, Beaverton, OR). The potentiometer was calibrated by manually moving the platform to several positions and recording the resultant voltage and position using the oscilloscope and a digital caliper (Mitutoyo, Japan). The potentiometer was found to be highly linear with a slope corresponding to 3.875 mV/mm and a R2 value of 0.999. The platform was then set to produce sinusoidal motion with a peak-to-peak amplitude of 39.25 mm and a 6 s period. To measure the gated LINAC beam, a photon diode (IBA Dosimetry America, TN) was placed at the radiation isocenter (Fig. 1) and connected to channel 2 of the oscilloscope. The field size of the 6 MV photon beam was set at 10 × 10 cm2.
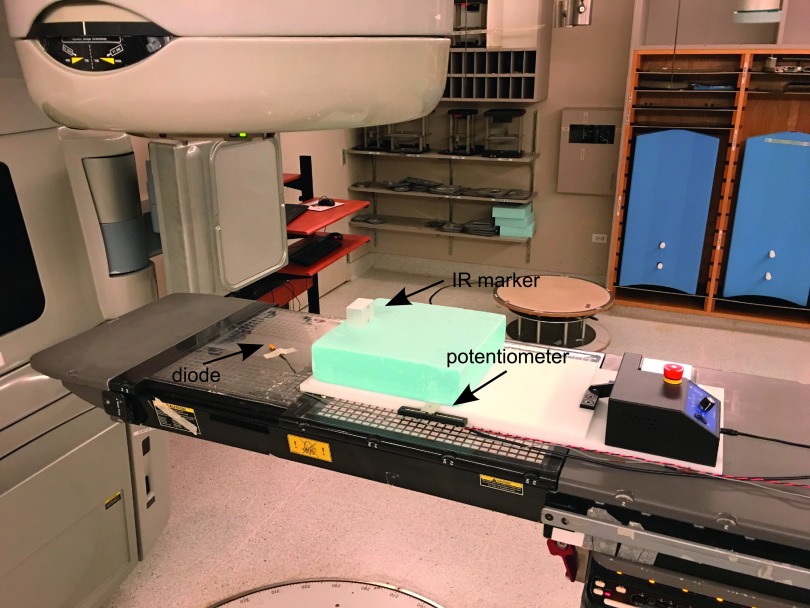
FIG. 1.
Experimental setup showing a photon diode placed at isocenter and a motion platform with an IR marker block. Platform motion is monitored using a linear potentiometer fixed to the side. Both potentiometer and diode signals are measured simultaneously using an oscilloscope.
Phase based gating was investigated using two different models of the real-time position management (RPM) gating system (Varian Medical Systems, CA). The first RPM system consisted of a single infrared (IR) camera and a patient marker block with two reflective IR stickers. The second RPM system used a stereoscopic IR camera with a marker block containing four reflective IR spheres. A gating window covering the 40%–60% phase of the breathing cycle was chosen as it corresponds to the clinically used exhale phase. To track motion, the IR marker block was placed on the motion platform (Fig. 1). Position based gating was investigated using an AlignRT 3D surface tracking system (VisionRT, UK) and a Calypso magnetic marker tracking system (Varian Medical Systems, CA) with a gating window covering a ±5 mm tolerance from the zero target position. To establish the zero reference position of the target, the motion platform was switched OFF and manually moved to the zero amplitude position. This position was then acquired by the gating system and used as its zero reference position. In addition, this position was recorded by the potentiometer for approximately 40 s in order to average out any noise. In all cases, the potentiometer and diode were measured simultaneously with the oscilloscope at 2500 Hz (0.4 ms sampling interval) for 40 s. The measurement was repeated three times in order to acquire approximately 20 or more respiratory cycles.
The phantom motion and beam ON/OFF gating windows were located using in-house software written in python. For phase based gating, it is necessary to determine the peak position of each cycle before the expected gating window can be calculated. To locate peak positions, motion greater than 80% of its maximum value was first isolated using a threshold function. Each peak was then individually fitted to a polynomial function using a least squares approach and the maximum point identified. These points therefore indicate the 0% phase for each cycle and allow for calculation of the period. The 40% and 60% gating window phase was then determined for each cycle based on its period. For position based gating, the expected gating window was determined by locating the intersection point between the motion signal and the set tolerance ranges based on the zero position reference signal. Beam ON regions of the diode signal were located by determining the times at which the diode signal increased to more than 30% of its maximum value, while the beam OFF regions were determined as the times at which the signal fell below 80% of its maximum value. The beam ON and OFF regions of the diode signal were then compared to the expected gating window.
3. RESULTS
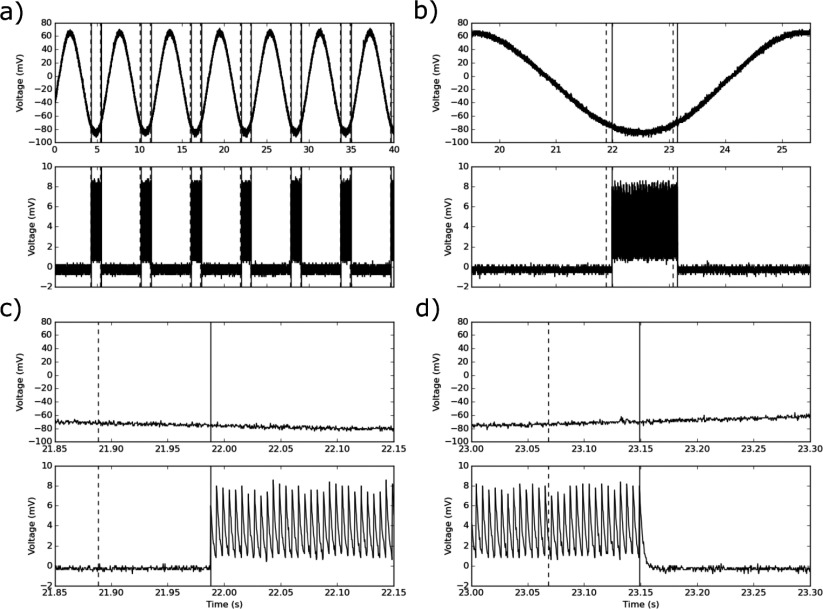
The measured outputs from the potentiometer and diode were examined for both the phase based case (Fig. 2) and the phase based case (Fig. 3). For the phase gating, Fig. 2(a) displays a sample of the synchronized signals captured from the potentiometer sensor mounted on the respiratory gating phantom and the photon diode. Figure 2(b) presents a zoomed in region around a single breathing cycle where the expected (dashed lines) versus the actual (solid lines) beam ON and OFF times for a 40% and 60% breathing phase have been indicated. Figures 2(c) and 2(d) further magnify on the start of gate and end of gate regions of the breathing cycle. Here it can be seen that the analysis algorithm correctly identifies the start and end of the gating window. Additionally, one can observe that the temporal resolution is high enough to distinguish individual LINAC beam pulses.
FIG. 2.
(a) Plot of phantom-simulated respiratory motion (top) and gated beam output signals (bottom) for a 40%–60% phase window of a RPM monoscopic camera gating system. (b) Magnified region showing expected (dashed lines) versus actual (solid lines) gate ON and OFF times for an individual cycle. (c) Magnified region at the start of gate. (d) Magnified region at the end of gate.
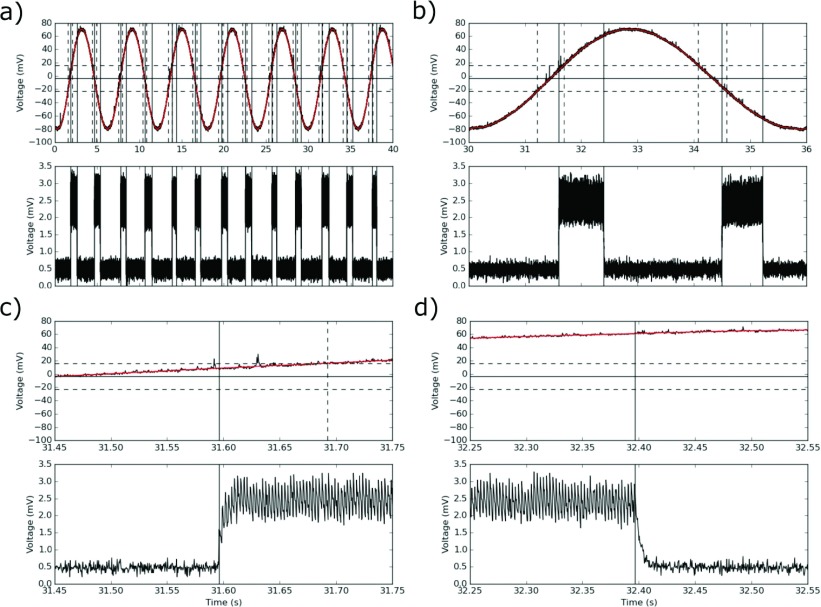
FIG. 3.
(a) Plot of phantom-simulated respiratory motion (top) and gated beam output signals (bottom) for a ±5 mm position window for the AlignRT gating system. (b) Magnified region showing expected (dashed lines) versus actual (solid lines) gate ON and OFF times for an individual cycle. (c) Magnified region at the start of gate. (d) Magnified region at the end of gate.
Figure 3 displays synchronized signals captured from the potentiometer and the photon diode for the case of position-based gating for the AlignRT gating system. Variation of actual beam ON times can be seen for different breathing cycles. Figure 3(b) presents a magnified region around a single cycle where the expected (dashed lines) versus the actual (solid lines) beam ON and OFF times for a ±5 mm breathing window (horizontal dashed lines) have been indicated. Here it was found that gate OFF lag times were longer than gate ON times. Figures 3(c) and 3(d) magnify further on both the start and end of gate regions of the breathing cycle, respectively.
Table I presents a summary of gate timing results for both phase and position gating systems. Statistics are calculated based on the breathing cycles as shown in Figs. 2 and 3.
TABLE I.
Summary of results for gate lag times in milliseconds.
| Gate ON (ms) | Gate OFF (ms) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Device | Type | Mean | Max | Min | SD | Mean | Max | Min | SD |
| AlignRT | Position | 356 | 449 | 265 | 60 | 529 | 704 | 432 | 81 |
| Calypso | Position | 209 | 242 | 171 | 21 | 60 | 109 | 26 | 21 |
| RPM mono | Phase | 98 | 118 | 99 | 11 | 90 | 109 | 78 | 11 |
| RPM stereo | Phase | 86 | 116 | 59 | 16 | 44 | 59 | 11 | 10 |
4. DISCUSSION
A high temporal resolution gating characterization method was demonstrated for both phase and positional gating modalities for the first time. The method was used to characterize the temporal performance of several clinically used gating systems. For patient safety, it is important to know exactly when the gating window begins and ends. TG-142 recommends that a gating device should gate the beam within 100 ms from the expected window. Referring to Table I, both RPM systems investigated were found to have mean start and end of gate lag times that met this recommendation. For position based gating, both the AlignRT and Calypso system had mean start of gate lag times that did not meet TG-142 recommendations. For end of gate times, it was found that the Calypso system lag time of 60 ms was within recommendations, whereas, the AlignRT system lag time of 529 ms was not. In terms of patient safety, it can be argued that the most important quantity is the end of gate time, as this will occur outside the gate window given positive lag times. The start of gate time, on the other hand, will occur inside the safety of the gate window. In this case the RPM stereo gating system delivered radiation with the highest spatial accuracy as it turned OFF its beam the fastest.
As shown in Figs. 2 and 3, the temporal resolution of this method is high enough to allow intercomparison of the differences in synchrony from one breathing cycle to the next. Referring to Table I, it can be seen that all gating systems displayed such variation. Here it was found that the Varian RPM systems had the lowest variation with a standard deviation of approximately 10 ms for both start and end of gate time lags. For the Calypso system, variation was similar for both gate ON and gate OFF lag times and equal to approximately 21 ms. The AlignRT system was found to have significant variation between individual gate cycles (Fig. 3). Here gate ON and OFF standard deviations were 60 and 81 ms, respectively. Here it should be noted that both RPM systems required initial sampling of several respiratory cycles before start of gated treatment. This was likely used to train an algorithm that helps judge when to turn the beam ON and OFF. Such an algorithm may also contain predictive filters that take into account mechanical or electrical delays and may explain the lower lag times of the RPM systems over the Calypso or AlignRT systems. It is expected that a tracking algorithm should be able to track 1D sinusoidal motion with high confidence. Therefore, the results reported in Table I should be interpreted as gating performance under a best case scenario. In addition to sinusoidal motion, a gating system should be subjected to a series of well-defined patient recorded breathing trajectories containing irregular motion in terms of amplitude and period. Such an investigation is beyond the scope of this work, however, it should be noted that the basic principles of the method can be expanded to include such an investigation. This would require improvement of the current algorithm to allow identification of highly irregular motion and the use of multidegree of freedom motion phantoms.7,8
The oscilloscope provided a temporal resolution of 0.4 ms/sample. As shown in Fig. 2, this was high enough to resolve individual electron pulses from the LINAC. These LINAC pulses show a sharp delta-like response making temporal location highly accurate. Visual examination of the diode signal versus the software-calculated ON and OFF points showed that the calculated points were within approximately <2 sampling points (or ±0.8 ms) of when the signal showed a steep upward or downward trend. For position based gating, assuming an oscilloscope resolution of 1 mV, the positional calibration is 0.258 mm/mV. Due to the high sampling rate, and ideal sinusoidal motion of the phantom, linear interpolation can be used to resolve a predicted gating window that is submillisecond in accuracy. For phase based gating, identification of the zero phase peak positions was found to be more difficult since the peaks appear flat at millisecond resolutions and noise can lead to the formation of multiple peaks. Here it was necessary to first fit the peak to a high degree polynomial in order to locate the global max peak position.
5. CONCLUSION
Temporal resolution of the method was high enough to allow characterization of individual gate cycles and was primarily limited by the sampling speed of the data recording device. Significant variation of gate ON and OFF lag time was found between the tested gating systems. For certain gating devices, individual gating cycle lag time can vary significantly.
ACKNOWLEDGMENTS
This work was funded in part by the National Institutes of Health No. T32-EB002103, Training grant from the National Institute of Biomedical Imaging and Bioengineering, and by American Cancer Society Grant No. RSG-13-313-01-CCE.
CONFLICT OF INTEREST DISCLOSURE
The authors have no COI to report.
REFERENCES
- 1.Keall P. J., Mageras G. S., Balter J. M., Emery R. S., Forster K. M., Jiang S. B., Kapatoes J. M., Low D. A., Murphy M. J., Murray B. R., Ramsey C. R., Van Herk M. B., Vedam S. S., Wong J. W., and Yorke E., “The management of respiratory motion in radiation oncology report of AAPM Task Group 76,” Med. Phys. 33(10), 3874–3900 (2006). 10.1118/1.2349696 [DOI] [PubMed] [Google Scholar]
- 2.Klein E. E., Hanley J., Bayouth J., Yin F.-F., Simon W., Dresser S., Serago C., Aguirre F., Ma L., Arjomandy B., Liu C., Sandin C., Holmes T., and Task Group 142, American Association of Physicists in Medicine, “Task Group 142 report: Quality assurance of medical accelerators,” Med. Phys. 36(9), 4197–4212 (2009). 10.1118/1.3190392 [DOI] [PubMed] [Google Scholar]
- 3.Jin J.-Y. and Yin F.-F., “Time delay measurement for LINAC based treatment delivery in synchronized respiratory gating radiotherapy,” Med. Phys. 32(5), 1293–1296 (2005). 10.1118/1.1896452 [DOI] [PubMed] [Google Scholar]
- 4.Smith W. L. and Becker N., “Time delays in gated radiotherapy,” J. Appl. Clin. Med. Phys. 10(3), 140–154 (2009). 10.1120/jacmp.v10i3.2896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chugh B. P., Quirk S., Conroy L., and Smith W. L., “Measurement of time delays in gated radiotherapy for realistic respiratory motions,” Med. Phys. 41(9), 091702 (6pp.) (2014). 10.1118/1.4890604 [DOI] [PubMed] [Google Scholar]
- 6.Freislederer P., Reiner M., Hoischen W., Quanz A., Heinz C., Walter F., Belka C., and Soehn M., “Characteristics of gated treatment using an optical surface imaging and gating system on an Elekta linac,” Radiat. Oncol. 10, 111–116 (2015). 10.1186/s13014-015-0376-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiersma R. D., Tomarken S. L., Grelewicz Z., Belcher A. H., and Kang H., “Spatial and temporal performance of 3D optical surface imaging for real-time head position tracking,” Med. Phys. 40(11), 111712 (8pp.) (2013). 10.1118/1.4823757 [DOI] [PubMed] [Google Scholar]
- 8.Belcher A. H., Liu X., Grelewicz Z., Pearson E., and Wiersma R. D., “Development of a 6DOF robotic motion phantom for radiation therapy,” Med. Phys. 41(12), 121704 (7pp.) (2014). 10.1118/1.4900828 [DOI] [PMC free article] [PubMed] [Google Scholar]