Abstract
Genetic counselors believe fertility preservation and preimplantation genetic diagnosis (PGD) discussions to be a part of their role when counseling BRCA1/2 mutation-positive patients. This study is the first to explore reproductive endocrinologists’ (REI) practices and attitudes regarding involvement of genetic counselors in the care of BRCA1/2 mutation carriers seeking fertility preservation and PGD. A survey was mailed to 1000 REIs from Reproductive Endocrinology & Infertility (SREI), an American Society for Reproductive Medicine (ASRM) affiliate group. A 14.5 % response rate was achieved; data was analyzed using SPSS software. The majority of participating REIs were found to recommend genetic counseling to cancer patients considering fertility preservation (82 %) and consult with a genetic counselor regarding PGD for hereditary cancer syndromes (92 %). Additionally, REIs consult genetic counselors regarding PGD patient counseling (88 %), genetic testing (78 %), and general genetics questions (66 %). Two areas genetic counselors may further aid REIs are: elicitation of family history, which is useful to determine fertility preservation and PGD intervention timing (32 % of REIs utilize a cancer family history to determine intervention timing); and, interpretation of variants of uncertain significance (VOUS) as cancer panel genetic testing becomes more common (36 % of REIs are unfamiliar with VOUS). Given our findings, the Oncofertility Consortium® created an online resource for genetic counselors focused on fertility preservation education and communication strategies.
Keywords: Oncofertility, Fertility preservation, BRCA1/2, Preimplantation genetic diagnosis, Genetic counseling
Introduction
A great deal of progress has been made in the past decade in terms of improving clinician-patient education, communication, and decision support with regard to oncofertility- a medical subfield concerned with young patients whose disease or its treatment may affect future fertility (Jeruss and Woodruff 2009; Loren et al. 2013; Quinn et al. 2010a). However, it remains unclear whether the oncofertility field is adequately addressing the unique and complex issues of fertility loss in patients with a BRCA1/2 mutation (Goetsch et al. 2014; Llarena and Jeruss 2014). Women with a BRCA1/2 mutation are at high risk to develop hereditary breast and ovarian cancer and therefore may be interested in fertility preservation options, and/or preimplantation genetic diagnosis (PGD) to reduce the risk of passing on a BRCA1/2 mutation to their children.
Women with Hereditary Breast and Ovarian Cancer (HBOC) syndrome, caused by deleterious mutations in BRCA1/2, have significantly greater lifetime risks of developing breast and ovarian cancer than the general population. Women with BRCA1 mutations face a 47.0–66.0 % risk of breast cancer and a 35.0–46.0 % risk of ovarian cancer; similarly, women with BRCA2 mutations face a 40.0–57.0 % risk of breast cancer and a 12.0–23.0 % risk of ovarian cancer (Chen and Parmigiani 2007). In comparison, the general population risk of breast cancer is 12.5 % and risk of ovarian cancer is 1.4 %(American Cancer Society 2013). Additionally, the average age of hereditary breast or ovarian cancer diagnosis in women with BRCA1/2 mutations is significantly lower than that in the general population (Miesfeldt et al. 2013).
The National Comprehensive Cancer Network (NCCN) strongly recommends that women at high risk for HBOC have genetic counseling when genetic testing is offered and after results are disclosed (National Comprehensive Cancer Network 2013). BRCA1/2 genetic testing can be performed by either traditional Sanger sequencing or as part of a Next-Generation sequencing cancer panel genetic test. Next-Generation sequencing cancer panels include genes in addition to BRCA1/2 that are associated with an increased risk of cancer. With any sequence-based genetic test, there are three possible results that can be reported after BRCA1/2 genetic testing: 1) negative, no mutation in the DNA sequence was detected; 2) positive, a deleterious mutation in the DNA sequence was detected that confers increased risk of developing cancer; and, 3) uncertain, in which a “variant of uncertain significance” (VOUS), a variation in a genetic sequence whose association with disease risk is unknown, was detected (Plon et al. 2008).
The NCCN also recommends that women with HBOC have risk-reducing prophylactic bilateral salpingo oophorectomy (PBSO)- ideally between age 35 and 40 years, after completion of child bearing, or individualized based on earliest age of onset of ovarian cancer in the family (National Comprehensive Cancer Network 2013). Studies have shown that to achieve the greatest reduction in risk for breast and ovarian cancer, BRCA1 mutation positive women should undergo PBSO by the age of 35 and BRCA2 mutation positive women should undergo PBSO by the age of 40 (Eisen et al. 2005; Finch et al. 2014). Women with strong family histories of cancer often elect risk-reducing PBSO at younger ages (Quinn et al. 2010a). Additionally, BRCA1/2 mutation-positive status and the associated greater lifetime cancer risk does not seem to affect the decision to have a child (Dekeuwer and Bateman 2013), and although BRCA1/2-positive women can pursue other possible avenues to parenthood, such as adoption and third-party reproduction, the majority of individuals surveyed prefer to have biological offspring (Crockin 2005; Schover 2009). Therefore, women with BRCA1/2 mutations may have increased interest in fertility preservation after a cancer diagnosis or prophylactically due to the increased risk of developing cancer.
BRCA1/2 mutation positive women may be more prone to chemotherapy-induced infertility given their low ovarian reserve and high likelihood of low response to ovulation induction than women without BRCA1/2 mutations (Loren et al. 2013), and thus may have greater interest in and benefit from fertility preservation. The established fertility preservation procedures available to women with HBOC are embryo cryo-preservation (Quinn et al. 2010a) and oocyte cryopreservation (ACOG 2008). Ovarian tissue cryopreservation is not advisable in BRCA1/2 mutation carriers given the increased risk of ovarian cancer in this population; however, at the time of oophorectomy, women with BRCA1/2 mutations may consider ovarian tissue harvesting for the option of experimental in vitro maturation of oocytes or follicles (Practice Committee of American Society for Reproductive, M 2013).
In addition to fertility preservation and intervention, women with BRCA1/2 mutations may have additional concerns about passing on hereditary cancer susceptibility to future children (Quinn et al. 2010a). To reduce this risk, patients may pursue preimplantation genetic diagnosis (PGD) and embryo selection, which has been used in conjunction with in vitro fertilization (IVF) to screen for BRCA1/2 mutations since 2006 (Quinn et al. 2010a). Couples considering PGD are required by the American Society for Reproductive Medicine (ASRM) Practice Committee to have genetic counseling to ensure that patients fully understand the risk for having an affected child, the impact of the disease on an affected child, and the limitations of available options that may help to avoid the birth of an affected child (Practice Committee of Society for Assisted Reproductive, T., and Practice Committee of American Society for Reproductive, M 2008).
This study aims to assess REIs’, who perform fertility preservation and PGD procedures, utilization of genetic counselors for assistance with the care of BRCA1/2 mutation positive oncofertility patients, including women with recent cancer diagnoses and women at increased risk to develop cancer. The specific objectives include: assess REIs’ experience with obtaining family history information and determination of intervention timing (the age at which fertility preservation or PGD would be appropriate for a patient given the age of cancer diagnosis in relatives); assess REIs’ experience with genetic testing for BRCA1/2 mutations; and, assess REIs’ relationships with genetic counselors- particularly regarding which aspects of patient care REIs utilize genetic counselors.
Methods
Sample
An introductory letter, survey in paper format, and prepaid return envelope were mailed to 1000 members of the Society for Reproductive Endocrinology & Infertility (SREI), an ASRM affiliate, using a random number generator to select addresses from the purchased list. Those who received the mailing were invited to participate in the study if they met the following inclusion criteria:
Participants must be board certified by the American Board of Obstetrics and Gynecology in both obstetrics and gynecology and the subspecialty of reproductive endocrinology;
Or, participants must be in the process of completing fellowship training in reproductive endocrinology and waiting to complete the subspecialty board examination process.
No reminder letter or incentives were provided. Responses were accepted between November 12, 2013 and January 13, 2014. Of the 1000 surveys that were mailed to REIs 141 complete, 27 return-to-sender, and two blank surveys were received, for an approximate response rate of 14.5 %.
Northwestern University IRB approved the study. Before answering survey questions, all the participants were instructed that the study was anonymous and return of the survey implied their consent in the study.
Instrumentation
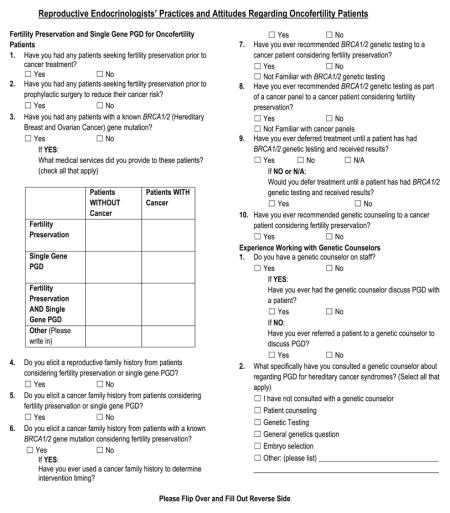
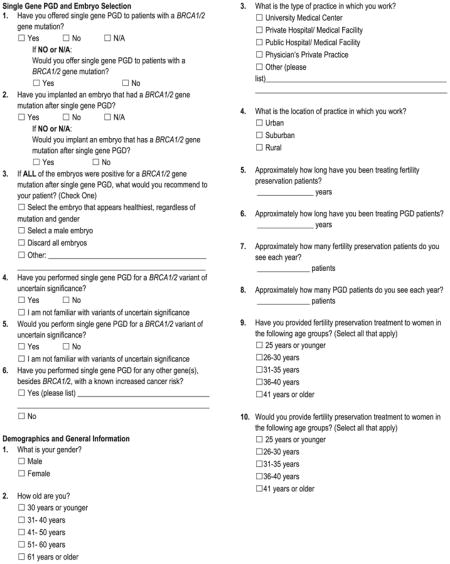
The survey instrument was developed based on published literature and clinical experience (Quinn et al. 2012; Quinn et al. 2010b; Vadaparampil et al. 2009; Menon et al. 2007). It was designed to explore the attitudes and practices of REIs’ towards BRCA1/2 gene mutation positive oncofertility patients, that is, women who have been recently diagnosed with cancer or women whom prophylactically act to preserve their fertility given the increased risk of cancer and earlier age of onset associated with HBOC. Survey questions and statements fell within the overall themes of experience with fertility preservation and PGD patients, experience with BRCA1/2 gene mutation positive patients, elicitation of family history, experience with genetic testing, and relationships with genetic counselors. Demographic data including clinician gender, age, location of practice, practice type, years practicing, and approximate number of patients seen per year were included at the end of the survey. The survey contained 34 questions; primarily multiple-choice and some clarifying free response questions. The survey took approximately 10–15 min to complete. The complete survey can be found in Appendix.
Data Analysis
Following survey closure, the data from the survey was compiled, coded, and analyzed using IBM SPSS Statistics 20 predictive analytics software (Statistics Package for the Social Sciences, Chicago, IL). A response was not required for each question in the survey, leading to different total number (n) of responses for each question. All data, regardless of the total n, was analyzed. Descriptive statistics, including frequencies, means, medians, and percentage of respondents, were calculated for each individual survey question. Chi-square statistics (or Fisher’s exact test) and p-values (p<0.05) were used to compare categorical variables and determine what, if any, statistical significance or associations existed between responses.
Results
Demographics
As shown in Table 1, the majority of the study participants were between 41 and 60 years of age (n=86, 62.3 %), and were in private practice (n=66, 46.8 %) or practiced at university medical centers (n=55, 39.0 %) in both urban (n=80, 57.1 %) and suburban (n=59, 42.1 %) locations. As shown in Table 2, respondents had a median of 8 years treating fertility preservation and/or PGD patients, and reported treating a median of 10 fertility preservation patients per year and 15 PGD patients per year. Additionally, 98.6 % (n=138) of participants reported experience providing fertility preservation to patients prior to undergoing cancer treatment and 43.5 % (n=60) of participants reported experience providing fertility preservation to patients prior to prophylactic surgery to reduce cancer risk. Furthermore, 65.7 % (n=92) of participants reported they have treated patients with a known BRCA1/2 gene mutation. As shown in Table 3, the most common treatment provided by participating REIs (n=69, 75.0 %) to BRCA1/2 positive patients is fertility preservation in women with cancer. Additionally, we discovered 30.3 % (n=40, N=132) of our participants have performed PGD for hereditary cancer predisposition syndromes other than HBOC; results are summarized in Table 4.
Table 1.
Demographic characteristics of study participants
| Category | n | % |
|---|---|---|
| Gender | ||
| Male | 78 | 56.9 |
| Female | 59 | 43.1 |
| Total | 137 | |
| Age | ||
| 30 and under | 4 | 2.9 |
| 31–40 | 30 | 21.7 |
| 41–50 | 34 | 24.6 |
| 51–60 | 52 | 37.7 |
| Over 60 | 18 | 13.0 |
| Total | 138 | |
| Type of practice | ||
| University Medical Center | 55 | 39.0 |
| Private Hospital | 15 | 10.6 |
| Public Hospital | 2 | 1.4 |
| Private Practice | 66 | 46.8 |
| Other | 3 | 2.1 |
| Total | 141 | |
| Location of practice | ||
| Urban | 80 | 57.1 |
| Suburban | 59 | 42.1 |
| Rural | 1 | 0.7 |
| Total | 140 | |
Table 2.
Clinical experience of study participants
| Years treating fertility preservation patients | Years treating PGD patients | Fertility preservation patients seen per year | PGD patients seen per year | |
|---|---|---|---|---|
| n | 141 | 141 | 140 | 140 |
| Mean | 10.9 | 8.2 | 27.2 | 26.9 |
| Median | 8.0 | 8.0 | 10.0 | 15.0 |
| Mode | 10.0 | 10.0 | 10.0 | 10.0 |
| Range | 45.0 | 24.0 | 500.0 | 250.0 |
PGD Preimplantation Genetic Diagnosis
Table 3.
Services provided by participating REIs to BRCA1/2 mutation positive oncofertility patients
| Category | n | % |
|---|---|---|
| Women with cancer diagnosis | ||
| Fertility preservation | 69 | 75.0 |
| PGD | 36 | 39.1 |
| Fertility preservation and PGD | 37 | 40.2 |
| Women without cancer diagnosis | ||
| Fertility preservation | 58 | 63.0 |
| PGD | 56 | 60.9 |
| Fertility preservation and PGD | 41 | 44.6 |
| Total | 92 | |
PGD Preimplantation Genetic Diagnosis
Table 4.
Hereditary cancer predispositions syndromes other than HBOC for which participating Reproductive Endocrinologists have Preimplantation Genetic Diagnosis (PGD) experience
| Syndrome | n | % |
|---|---|---|
| Lynch syndrome | 11 | 40.8 |
| Retinoblastoma | 5 | 18.5 |
| Li-Fraumeni syndrome | 4 | 14.8 |
| Familial adenomatous polyposis (FAP) | 3 | 11.1 |
| Multiple endocrine neoplasia type 2 (MEN2) | 3 | 11.1 |
| Peutz-Jeghers syndrome | 1 | 3.7 |
| Total | 27 |
Elicitation of Family History
Although the majority of participants reported they obtain a reproductive family history (97.9 %, 137/140) and a cancer family history (96.4 %, 134/139) from their patients, only 32.2 % (37/115) of respondents who have treated BRCA1/2 positive patients reported they have utilized a BRCA1/2 positive patient’s cancer family history to determine intervention timing (the age at which fertility preservation or PGD would be appropriate for a patient given the age of cancer diagnosis in relatives).
Experience with BRCA1/2 Genetic Testing
Participants were surveyed about their experience and familiarity with BRCA1/2 genetic test results, independently and as part of Next-Generation sequencing cancer panel testing. It was not assessed if participants were the ordering provider for genetic tests. As shown in Table 5, 64.0 % (n=89) of participants have recommended BRCA1/2 genetic testing to their patients seeking fertility preservation after a cancer diagnosis. Of the study participants, 44.6 % (n=62) reported that they have recommended BRCA1/2 genetic testing as part of a Next-Generation sequencing cancer panel to their patients. A greater percentage of participants (11.5 %, 16/139) reported that they were unfamiliar with cancer panel genetic testing as compared to single gene BRCA1/2 testing (0.75 %, 1/139). Additionally, 26.1 % (n=36) of participants have delayed oncofertility treatment until a patient’s BRCA1/2 genetic test results were available. Of those who have not delayed oncofertility treatment in the past, 45.7 % (n=37) reported they would be willing to delay treatment pending results in the future. Therefore, 52.9 % (n= 73) of respondents have or would defer oncofertility treatment until a patient’s BRCA1/2 genetic test results were available.
Table 5.
Participating REI experiences with genetic testing for BRCA1/2 mutations
| Characteristics and behaviors | n | % |
|---|---|---|
| Have you recommended BRCA1/2 genetic testing to a cancer patient considering fertility preservation? | ||
| Yes | 89 | 64.0 |
| No | 49 | 35.3 |
| Not Familiar with BRCA1/2 genetic testing | 1 | 0.7 |
| Total | 139 | |
| Have you ever recommended BRCA1/2 genetic testing as part of a cancer panel to a cancer patient considering fertility preservation? | ||
| Yes | 62 | 44.6 |
| No | 61 | 43.9 |
| Not familiar with cancer panels | 16 | 11.5 |
| Total | 139 | |
| Have you ever deferred treatment until a patient has had BRCA1/2 genetic testing and received results? | ||
| Yes | 36 | 26.1 |
| No | 74 | 53.6 |
| N/A | 28 | 20.3 |
| Total | 138 | |
| If No or N/A: Would you defer treatment until a patient has had BRCA1/2 genetic testing hand received results? | ||
| Yes | 37 | 45.7 |
| No | 74 | 54.3 |
| Total | 81 | |
The participants were also surveyed about their familiarity and experience with VOUS genetic test results. Of the study participants, 2.9 % (4/140) reported they have performed PGD for a VOUS and 36.3 % (49/135) of those who have not, would perform PGD for a VOUS. A total of 35.6 % (48/135) reported they were unfamiliar with VOUS.
Experience Working with Genetic Counselors
Participants were asked a series of questions in order to assess if REIs seek out genetic counselors for additional information regarding BRCA1/2 mutations as well as assistance with patient counseling and embryo selection based on molecular test results. Of study participants, 42.4 % (n=61) reported that they have a genetic counselor on staff, and of those who do, 91.8 % (56/61) have had their genetic counselor discuss PGD with patients. Of those participants who do not have a genetic counselor on staff (n=80, 57.6 %), 80.8 % (59/73) refer patients to genetic counselors to discuss PGD. And 81.6 % (n=111) of all participants reported that they have recommended genetic counseling to their cancer patients considering fertility preservation. REIs reported consulting with genetic counselors about PGD for hereditary cancer syndromes regarding the topics summarized in Table 6. The primary reasons REIs reported consulting with genetic counselors regarding PGD for hereditary cancer syndromes were: patient counseling (n=122, 88.4 %), genetic testing (n=107, 77.5 %), and general genetics questions (n=91, 65.9 %).
Table 6.
Aspects of patient care and genetics that reproductive endocrinologists report they have consulted with a genetic counselor for patients with hereditary cancer syndromes interested in Preimplantation Genetic Diagnosis (PGD)
| Options | n | % |
|---|---|---|
| Not consulted a genetic counselor | 11 | 8.0 |
| Patient counseling | 122 | 88.4 |
| Genetic testing | 107 | 77.5 |
| General genetics questions | 91 | 65.9 |
| Embryo selection | 26 | 18.8 |
| Other | 6 | 4.3 |
| Total | 138 |
REIs who work in university medical centers (Fisher’s exact, p=0.000) and private practice (Fisher’s exact, p=0.000) were found to be significantly associated with having a genetic counselor on staff. All participant demographic variables were analyzed with respect to all questions pertaining genetic counselors and no additional statistical associations involving the relationship between REIs and genetic counselors were found.
Discussion
This study was the first to examine and quantify REI practices and attitudes regarding BRCA1/2 mutation positive oncofertility patients with respect to elicitation of family history information, determination of intervention timing, experience with genetic testing and VOUS, and relationships with genetic counselors. This study establishes the majority of participating REIs utilize genetic counselors for hereditary cancer syndrome PGD patient counseling, genetic testing, and general genetics questions, as well as recommend genetic counseling to patients interested in fertility preservation after a cancer diagnosis.
The National Society of Genetic Counselors (NSGC) defines genetic counseling as “the process of helping people understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease”, which integrates interpretation of personal and family medical histories; education about inheritance, testing, management, prevention, resources, and research; and counseling to promote informed choices (National Society of Genetic Counselors’ Definition Task et al. 2006). Genetic counselors possess the necessary skills to address fertility preservation and PGD with oncofertility patients and should be utilized in oncofertility and PGD care. Additionally, genetic counselors are different than other health professionals with genetics expertise because they focus on the psychosocial adaption to genetic conditions or genetic risk (Biesecker and Peters 2001). In fact, the complexity of the psychological, social, and scientific issues associated with PGD resulted in the Ethics Committee of the ASRM stressing the importance of involving experienced genetic counselors in PGD discussions (Ethics Committee of American Society for Reproductive Medicine 2013). In accordance with the Ethics Committee of the ASRM, the majority of participating REIs in this study reported they have genetic counselors (either on staff or by referral) discuss PGD with their patients and have recommended genetic counseling to their patients interested in fertility preservation. Therefore, REIs appear to utilize genetic counselors and their services to assist with the care of their patients interested in PGD and fertility preservation.
In addition to having genetic counselors counsel their patients interested in fertility preservation and PGD, the majority of REIs in this study reported that they also consult with genetic counselors about genetic testing for hereditary cancer syndromes and general genetics questions regarding hereditary cancer syndromes. The majority of participants reported recommending genetic testing of embryos for BRCA1/2 mutations to their patients and consulting with genetic counselors regarding genetic testing.
Genetic testing for mutations in BRCA1/2 results in a VOUS in approximately 5 % of patients (Vallee et al. 2012), although the likelihood of a variant result is even higher for individuals in understudied populations (John et al. 2007; McKean-Cowdin et al. 2005). Our study found greater than one third of participants were unfamiliar with VOUS; this unfamiliarity is consistent with a study assessing referring physicians understanding of BRCA1/2 VOUS, which showed an inappropriate referral pattern after VOUS identification (Richter et al. 2013). VOUS results are a more frequent outcome of panel-based genetic testing compared to BRCA1/2 testing; analysis of the first 100 Ambry Genetics BreastNext™ panels reported a VOUS in 33 % of patients (Ambry Genetics 2013). Given that 44.6 % (n=62) of participating REIs have recommended BRCA1/2 genetic testing as part of a Next-Generation sequencing cancer panel to their patients, REIs may see an increase in their patient population with VOUS results, and in turn need additional assistance from genetic counselors with the interpretation and explanation of VOUS. Genetic counselors have also been shown to accurately predict the difficulties patients would have with a VOUS result and have identified the need for BRCA1/2 VOUS management guidelines (Richter et al. 2013). Therefore genetic counselors may provide further assistance to REIs by providing additional information about VOUS genetic test results for patients considering fertility preservation and/or PGD, especially as the uptake of cancer panel genetic testing increases.
Traditionally, genetic counselors have used personal and family medical histories to develop a differential diagnosis, identify and quantify risk for family members, and select the appropriate proband to test (Ormond 2013; Pyeritz 2012). However, age of cancer onset in the family history contributes to risk-reducing PBSO decision in patients with BRCA1/2 gene mutations, and as such, cancer family history should also be considered when discussing intervention timing for fertility preservation and PGD. Although 93.0 % of participating REIs reported they elicit a cancer family history from their BRCA1/2 mutation positive patients, only 32.2 % of REIs have utilized a BRCA1/2 positive patient’s cancer family history to determine intervention timing. Genetic counselors are capable of further aiding REIs by eliciting detailed family histories per NSGC and NCCN guidelines. Both NSGC and NCCN guidelines regarding cancer risk assessment for HBOC highlight the importance of family history information in genetic assessment and management recommendations (Berliner et al. 2013; National Comprehensive Cancer Network 2013). Additionally, The Practice Committee of the ASRM promotes interdisciplinary communication among providers, including genetic counselors, given that it is “critical to determine the optimal strategy and timing of fertility-preservation techniques” (Practice Committee of American Society for Reproductive, M 2013). Genetic Counselors could assist REIs in the determination of intervention timing for oncofertility patients by eliciting detailed family history information.
Previous studies have assessed hereditary cancer syndrome carriers’ attitudes towards fertility preservation and/or PGD and two main themes have emerged from the literature: 1) there is an oncofertility and PGD information gap in the HBOC population (Quinn et al. 2012; Quinn et al. 2010b; Vadaparampil et al. 2009), and 2) once informed about the use and availability of PGD, it is considered an acceptable option for individuals with HBOC (Menon et al. 2007; G. P. Quinn et al. 2012; Vadaparampil et al. 2009). Women with BRCA1/2 mutations also express a strong desire for assistance with decision making in oncofertilty and PGD and report the need for health care professionals with expertise across a variety of topics including BRCA1/2 risk management, fertility, and psychosocial counseling (Quinn et al. 2010c). Genetic counselors, who possess expertise in all three areas, were identified as BRCA1/2 mutation positive patients preferred professionals with whom to discuss reproductive options (Quinn et al. 2009). Reproductive options discussions regarding fertility preservation are believed by cancer genetic counselors to be a part of their role and 61 % reported having a patient raise the issue of fertility preservation (Volk et al. 2012). Similarly, most genetic counselors believe PGD should be discussed with every BRCA1/2 mutation positive patient (Morrison et al. 2010). The Ethics Committee of the ASRM has also stressed the importance of involving an experienced genetic counselor before patients undertake PGD, given the complexity of the scientific, psychological, and social issues involved in this arena (Ethics Committee of American Society for Reproductive Medicine 2013).
In summary, BRCA1/2 mutation carriers consider PGD an acceptable reproductive option and prefer discussing reproductive options with genetic counselors. Additionally, genetic counselors believe they should discuss fertility preservation and PGD with HBOC patients and the ASRM has recognized the importance of genetic counselors in PGD discussions. In combination with this study, which found that REIs utilize genetic counselors for the care and treatment of BRCA1/2 mutation-positive patients interested in fertility preservation and PGD, it appears that genetic counselors have a role in oncofertility and PGD discussions.
The study was limited by a response rate of 14.5 %. Due to budgetary restrictions, no incentives or reminder letters were provided to participants to increase response rate. The limited responses made it difficult to make data comparisons. However, the response rate is comparable with the 10.2–20.0 % response rate range of previous studies that have surveyed similar populations (Abdel-Rahman et al. 2012; Freedman et al. 2013; Tambor et al. 1993).
The study requested participants to answer questions regarding their practices and attitudes regarding BRCA1/2 positive oncofertility patients. Individuals who are not treating oncofertility patients, or are not familiar with BRCA1/2 mutations, may not have taken the survey. This may have potentially skewed the data towards those that are familiar with oncofertility and interested in PGD for hereditary cancer predisposition syndromes, and therefore may not be representative of the entire United States REI population. Additionally, we did not ask study participants if they were ordering BRCA1/2 genetic testing for their patients, therefore we do not know if study participants have personal experience with this testing or if patients typically have testing with an alternative provider (e.g., genetic counselor, oncologist, gynecologist).
Finally, this survey looked primarily at the practice of fertility preservation and PGD in women with known BRCA1/2 gene mutations; therefore discussions and perceptions may be different across different cancer syndromes, genders, and age groups. However, results may also be generalizable to other hereditary cancer predisposition syndromes, as many study participants have performed PGD for hereditary cancer predisposition syndromes besides HBOC. Additionally, hereditary cancer predisposition syndromes share the common characteristic of not causing a disease but instead conferring an increased risk to develop cancer. However, the specific risk or penetrance among offspring may differ with respect to underlying genetic etiology and gender.
Conclusions
Previous studies have shown genetic counselors have a role in both oncofertility and PGD patient discussions given BRCA1/2 mutation carriers consider PGD an acceptable reproductive option; BRCA1/2 mutation carriers prefer discussing reproductive options with genetic counselors; genetic counselors believe they should discuss fertility preservation and PGD with HBOC patients; and the ASRM has recognized the importance of genetic counselors in PGD discussions. Furthermore, the majority of REIs in this study reported they have genetic counselors, either on staff or by referral, discuss PGD with their patients as well as reported they recommend genetic counseling to patients newly diagnosed with cancer considering fertility preservation. Genetic counselors appear to be a utilized resource by REIs and may be able to provide further assistance regarding Next-Generation sequencing cancer panel testing, provide information about variants of uncertain significance, and elicit detailed cancer family history information from patients which REIs can use to help determine intervention timing.
Given the study findings, the Oncofertility Consortium® created an online resource specifically for genetic counselors that focuses on oncofertility education and communication strategies (accessible: http://oncofertility.northwestern.edu/genetic-counselors). The resource summarizes genetic counselors’ role in oncofertility care and provides access to many educational materials, including the Oncofertility Decision Tool Web Portal- an online library of existing oncofertility decision aids designed to help genetic counselors stay current on fertility preservation techniques and technology; learn communication strategies for discussing fertility preservation options with patients of all ages and their family members; access clinical guidelines and recommendations; and, access print and online patient educational resources.
Many Oncofertility Consortium® tools are specific to the high-risk patient population, and therefore are particularly helpful for genetic counselors, as they may be the first health care provider with an opportunity to address future fertility concerns with young women concerned about future cancer risk. The Oncofertility Consortium® also assists genetic counselors with patient referrals- via the FERTline (866-708-FERT (3378)), a hotline for providers and patients who have fertility preservations concerns and questions, or need a referral for a fertility preservation consultation. Finally, the Oncofertility Consortium® provides quick links to insurance and billing information regarding fertility preservation, as well as provider pocket guides and patient fact sheets available for no charge online at http://www.savemyfertility.org or via iSaveFertility, a smartphone application. The Oncofertility Consortium® online resource for genetic counselors was designed to educate and further integrate genetic counselors into the exciting field of oncofertility with targeted resources specific to the genetic counselors’ high risk patient population.
Future directions include additional research studies designed to expand our knowledge and understanding of genetic counselor involvement in fertility preservation discussions with respect to gender, additional hereditary cancer predisposition syndromes, and non-malignant genetic conditions know to impair fertility. Additionally, we hope to increase accessibility of the Oncofertility Consortium®’s free resources with providers and patients with the goal of establishing fertility preservation discussion as standard medical care.
Acknowledgments
The authors would like to thank the study participants for their involvement; Jacqueline S. Jeruss, MD, Eve C. Feinberg, MD, and Taya Fallen, MS for their assistance and input; Northwestern University’s Graduate Program in Genetic Counseling for their support; and NIH/NICHD grant P50HD076188.
Appendix
Footnotes
Compliance with Ethical Standards
Human Studies and Informed Consent No human studies were carried out by the authors for this article
Animal Studies No animal studies were carried out by the authors for this article
Disclaimer Note that the data analyzed in this paper represents a portion of the primary data collected and that two analyses were conducted independently.
Conflict of Interest Allison L Goetsch, Catherine Wicklund, Marla Clayman, and Teresa K Woodruff declare that they have no conflict of interest.
References
- Abdel-Rahman M, Jackson L, Rodewald K, Abdellah M, Ismail S, Hurd W. Polycystic ovary syndrome and diabetes screening: a survey of gynecologists and reproductive endocrinologists. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2012;162(2):178–181. doi: 10.1016/j.ejogrb.2012.03.007. [DOI] [PubMed] [Google Scholar]
- ACOG. ACOG committee opinion No. 413: age-related fertility decline. Obstetrics and Gynecology. 2008;112:409–411. doi: 10.1097/AOG.0b013e318183fbe6. [DOI] [PubMed] [Google Scholar]
- Ambry Genetics. The case for clinical adoption of hereditary breast cancer panel testing. Ambry Genetics; 2013. http://www.ambrygen.com/sites/default/files/BreastNext_WhitePaper_112812_0.pdf. [Google Scholar]
- American Cancer Society. Cancer facts & figures 2013. Atlanta: American Cancer Society; 2013. [Google Scholar]
- Berliner JL, Fay AM, Cummings SA, Burnett B, Tillmanns T. NSGC practice guidelines: risk assessment and genetic counseling for hereditary breast and ovarian cancer. Journal of Genetic Counseling. 2013;22:155–163. doi: 10.1007/s10897-012-9547-1. [DOI] [PubMed] [Google Scholar]
- Biesecker BB, Peters KF. Process studies in genetic counseling: peering into the black box. American Journal of Medical Genetics. 2001;106(3):191–198. doi: 10.1002/ajmg.10004. [DOI] [PubMed] [Google Scholar]
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. Journal of Clinical Oncology. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crockin S. Legal isses related to parenthood after cancer. Journal of the National Cancer Institute Monographs. 2005;34:111–112. doi: 10.1093/jncimonographs/lgi024. [DOI] [PubMed] [Google Scholar]
- Dekeuwer C, Bateman S. Much more than a gene: hereditary breast and ovarian cancer, reproductive choices and family life. Medicine, Health Care and Philosophy. 2013;16(2):231–244. doi: 10.1007/s11019-011-9361-9. [DOI] [PubMed] [Google Scholar]
- Eisen A, Lubinski J, Klijn J. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers: an international case–control study. Journal of Clinical Oncology. 2005;23:7491–7496. doi: 10.1200/JCO.2004.00.7138. [DOI] [PubMed] [Google Scholar]
- Ethics Committee of American Society for Reproductive Medicine. Use of preimplantation genetic diagnosis for serious adult onset conditions: a committee opinion. Fertility and Sterility. 2013;100(1):54–57. doi: 10.1016/j.fertnstert.2013.02.043. [DOI] [PubMed] [Google Scholar]
- Finch APM, Lubinski J, Moller P, Singer CF, Karlan B, Senter L, Maehle L. Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. Journal of Clinical Oncology. 2014 doi: 10.1200/JCO.2013.53.2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman B, Steffen G, Wicklund C, Besser A, Pavone M, Dungan J. Preimplantation genetic diagnosis for adult-onset and susceptibility diseases: perspectives of reproductive endocrinologists. Northwestern University; 2013. Unpublished manuscript. [Google Scholar]
- Goetsch A, Volk A, Woodruff TK. Genetic counselors: bridging the oncofertility information gap. In: Woodruff TK, Clayman M, editors. Oncofertility communication sharing information building relationships across disciplines. Springer Science+ Business Media, LLC; 2014. [Google Scholar]
- Jeruss JS, Woodruff TK. Preservation of fertility for cancer patients. The New England Journal of Medicine. 2009;360:902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John E, Miron A, Gong G, Phipps A, Felberg A, Li F, Whittemore A. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298(24):2869–2876. doi: 10.1001/jama.298.24.2869. [DOI] [PubMed] [Google Scholar]
- Llarena NC, Jeruss JS. Fertility communication and high risk patients. In: Woodruff TK, Clayman ML, Waimey KE, editors. Oncofertility communication. Springer; New York: 2014. pp. 61–72. [Google Scholar]
- Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH American Society of Clinical O. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology. 2013;31(19):2500–2510. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKean-Cowdin R, Spencer Feigelson H, Xia LY, Pearce CL, Thomas DC, Stram DO, Henderson BE. BRCA1 variants in a family study of African-American and Latina women. Human Genetics. 2005;116(6):497–506. doi: 10.1007/s00439-004-1240-5. [DOI] [PubMed] [Google Scholar]
- Menon U, Harper J, Sharma A, Fraser L, Burnell M, ElMasry K, Jacobs I. Views of BRCA gene mutation carriers on pre-implantation genetic diagnosis as a reproductive option for hereditary breast and ovarian cancer. Human Reproduction. 2007;22(6):1573–1577. doi: 10.1093/humrep/dem055. [DOI] [PubMed] [Google Scholar]
- Miesfeldt S, Lamb A, Duarte C. Management of genetic syndromes predisposing to gynecologic cancers. Current Treatment Options in Oncology. 2013;14:34–50. doi: 10.1007/s11864-012-0215-3. [DOI] [PubMed] [Google Scholar]
- Morrison S, Hiller E, Gabree M, Roche P. Opinions, knowledge, and attitudes of genetic counselors in the United States about preimplantation genetic diagnosis for BRCA1/2 mutation carriers. Brandeis University; 2010. Unpublished manuscript. [Google Scholar]
- National Comprehensive Cancer Network. 2013 Genetic/familial high-risk assessment: breast and ovarian. 2014. [Google Scholar]
- National Society of Genetic Counselors’ Definition Task F. Resta R, Biesecker BB, Bennett RL, Blum S, Hahn SE, Williams JL. A new definition of Genetic Counseling: National Society of Genetic Counselors’ Task Force report. Journal of Genetic Counseling. 2006;15(2):77–83. doi: 10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- Ormond KE. From genetic counseling to “genomic counseling”. Molecular Genetics & Genomic Medicine. 2013;1(4):189–193. doi: 10.1002/mgg3.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plon SE, Eccles DM, Easton D, Foulkes WD, Genuardi M, Greenblatt MS, Group IUGVW. Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Human Mutation. 2008;29(11):1282–1291. doi: 10.1002/humu.20880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Practice Committee of American Society for Reproductive M. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertility and Sterility. 2013;100(5):1214–1223. doi: 10.1016/j.fertnstert.2013.08.012. [DOI] [PubMed] [Google Scholar]
- Practice Committee of Society for Assisted Reproductive T, Practice Committee of American Society for Reproductive M. Preimplantation genetic testing: a Practice Committee opinion. Fertility and Sterility. 2008;90(5 Suppl):S136–S143. doi: 10.1016/j.fertnstert.2008.08.062. [DOI] [PubMed] [Google Scholar]
- Pyeritz RE. The family history: the first genetic test, and still useful after all those years? Genetics in Medicine. 2012;14(1):3–9. doi: 10.1038/gim.0b013e3182310bcf. [DOI] [PubMed] [Google Scholar]
- Quinn G, Vadaparampil S, Wilson C, King L, Choi J, Miree C, Friedman S. Attitudes of high-risk women toward preimplantation genetic diagnosis. Fertility and Sterility. 2009;91(6):2361–2368. doi: 10.1016/j.fertnstert.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Quinn GP, Pal T, Murphy D, Vadaparampil ST, Kumar A. High-risk consumers’ perceptions of preimplantation genetic diagnosis for hereditary cancers: a systematic review and meta-analysis. Genetics in Medicine. 2012;14(2):191–200. doi: 10.1038/gim.0b013e31822ddc7e. [DOI] [PubMed] [Google Scholar]
- Quinn GP, Vadaparampil S, Jacobsen P, Knapp C, Keefe D, Bell G. Frozen hope: fertility preservation for women with cancer. Journal of Midwifery & Women’s Health. 2010a;55:175–180. doi: 10.1016/j.jmwh.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Quinn GP, Vadaparampil ST, Miree CA, Lee JH, Zhao X, Friedman S, Mayer J. High risk men’s perceptions of pre-implantation genetic diagnosis for hereditary breast and ovarian cancer. Human Reproduction. 2010;25(10):2543–2550. doi: 10.1093/humrep/deq207. [DOI] [PubMed] [Google Scholar]
- Quinn GP, Vadaparampil ST, Tollin S, Miree CA, Murphy D, Bower B, Silva C. BRCA carriers’ thoughts on risk management in relation to preimplantation genetic diagnosis and childbearing: when too many choices are just as difficult as none. Fertility and Sterility. 2010c;94(6):2473–2475. doi: 10.1016/j.fertnstert.2010.03.064. [DOI] [PubMed] [Google Scholar]
- Richter S, Haroun I, Graham TC, Eisen A, Kiss A, Warner E. Variants of unknown significance in BRCA testing: impact on risk perception, worry, prevention and counseling. Annals of Oncology. 2013;24(Suppl 8):viii69–viii74. doi: 10.1093/annonc/mdt312. [DOI] [PubMed] [Google Scholar]
- Schover LR. Patient attitudes toward fertility preservation. Pediatric Blood & Cancer. 2009;53(2):281–284. doi: 10.1002/pbc.22001. [DOI] [PubMed] [Google Scholar]
- Tambor E, Chase G, Faden R. Improving response rates through incentive and follow-up: the effect on a survey of physicians’ knowledge of genetics. American Journal of Public Health. 1993;83:1599–1603. doi: 10.2105/ajph.83.11.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadaparampil ST, Quinn GP, Knapp C, Malo TL, Friedman S. Factors associated with preimplantation genetic diagnosis acceptance among women concerned about hereditary breast and ovarian cancer. Genetics in Medicine. 2009;11(10):757–765. doi: 10.1097/GIM.0b013e3181b3f451. [DOI] [PubMed] [Google Scholar]
- Vallee MP, Francy TC, Judkins MK, Babikyan D, Lesueur F, Gammon A, Tavtigian SV. Classification of missense substitutions in the BRCA genes: a database dedicated to Ex-UVs. Human Mutation. 2012;33(1):22–28. doi: 10.1002/humu.21629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volk A, Aufox S, Fallen T, Beaumont J, Woodruff TK. Genetic counselor attitudes, knowledge and discussions of fertility preservation in the hereditary breast and ovarian cancer clinc. Northwestern University; 2012. Unpublished manuscript. [Google Scholar]


