Abstract
With each heartbeat, Connexin43 (Cx43) cell-cell communication gap junctions are needed to rapidly spread and coordinate excitation signals for an effective heart contraction. The correct formation and delivery of channels to their respective membrane subdomain is referred to as protein trafficking. Altered Cx43 trafficking is a dangerous complication of diseased myocardium which contributes to the arrhythmias of sudden cardiac death. Cx43 has also been found to regulate many other cellular processes that cannot be explained by cell-cell communication. We recently identified the existence of up to six endogenous internally translated Cx43 N-terminal truncated isoforms from the same full-length mRNA molecule. This is the first evidence that alternative translation is possible for human ion channels and in human heart. Interestingly, we found that these internally translated isoforms, more specifically the 20 kDa isoform (GJA1-20k), is important for delivery of Cx43 to its respective membrane subdomain. This review covers recent advances in Cx43 trafficking and potential importance of alternatively translated Cx43 truncated isoforms.
1. Introduction
Connexins are ubiquitous transmembrane proteins which are encoded by over 20 different genes in human with connexin 43 (Cx43) being the most commonly expressed in all organ systems, particularly in the heart [1, 2]. All connexins share a similar structural organization, which includes four transmembrane domains, two extracellular and three cytosolic subdomains with the N and C terminal ends facing the cytosol [3, 4]. The N terminus is mainly conserved between the different connexins and is capable of self-assembly and hexamer formation while the carboxy terminal cytosolic tail is the most variable in terms of both length and composition [5]. An extensively studied and well appreciated function of connexins is their ability to form gap junctions. To form a gap junction, six connexin monomers from one cell oligemarize to form a transmembrane channel referred to as a connexon or hemichannel. The connexons from one cell then dock and couple with apposing connexons on neighboring cells and coalesce into dense gap junction plaques [6-8].
Gap junctions are specialized channels that aid in the intercellular exchange of small metabolites, secondary messengers and ions carrying electrical signals between neighboring cells, therefore allowing cells to cooperate both electrically and metabolically [6, 9]. Examples of Cx43 gap junction mediated processes include the synchronous contraction of cardiomyocytes during each heart beat [10-12] as well as the contraction of smooth muscle cells in the uterus during labor [13]. Cx43 gap junction mediated intercellular coupling has also been recognized as a key regulator of cellular development, growth and differentiation [3]. Furthermore, the importance of Cx43 hemichannels and gap junctions in mediating ischemia/reperfusion injury, cardioprotection and neuroprotection has been extensively studied (reviewed recently by Schulz et al. 2015 [4]).
During the average human lifetime, a heart beats more than 3 billion times. For each of those heartbeats to be effective, each second, several billion heart cells need to contract in synchrony. Cx43 gap junctions play a crucial role as they provide the intercellular coupling that is necessary for rapid action potential propagation through the myocardium thus triggering a synchronized heart contraction [10-12]. Altered Cx43 localization and losses in cell-cell gap junction coupling occur during cardiac disease [14] and contribute to abnormal impulse propagation and arrhythmogenic substrates leading to sudden cardiac death [15-21]. In addition, a large number of studies in recent years have demonstrated a decrease in expression and/or lateralization and heterogeneous distribution of Cx43 in the myocardium of patients with hypertrophic cardiomyopathies [22-24], dilated cardiomyopathies [25, 26], ischemic cardiomyopathies [23-25] as well as clinical congestive heart failure [27]. To generalize, altered Cx43 localization is a result of diseased myocardium, with consequences including lethal arrhythmias. The altered Cx43 localization during disease reflects impaired trafficking. To preserve rapid and organized propagation of electrical signals, researchers are now focusing on the mechanisms of normal Cx43 trafficking and the changes with disease. This review discusses recent advances in understanding Cx43 trafficking.
2. Cx43 Forward Trafficking
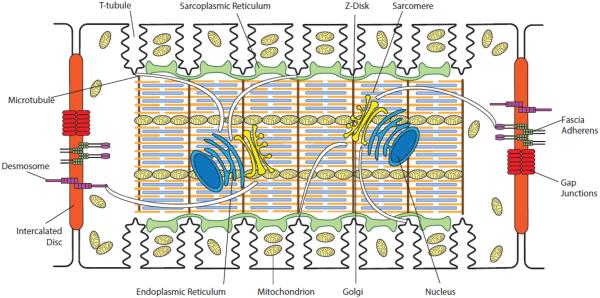
Cardiomyocytes use common intracellular organelles to produce Cx43 and shuttle Cx43 hexameric channels to the intercalated discs. After gene transcription in nuclei, Cx43 is translated and subjected to post-translational modification in the ER and then further modified and sorted in the Golgi apparatus prior to delivery to its subcellular destination at intercalated discs. The intercalated discs are located at the longitudinal ends of cardiomyocytes, perpendicular to myofibrils, and help couple cardiomyocytes both mechanically and electrically [7]. Mechanical coupling of cardiomyocytes is achieved through desmosome and fascia adherens complexes connecting the intercalated disc to structural components of the cytoskeleton such as intermediate filaments and F-actin (Figure 1). Gap junctions are primarily responsible for electrical coupling of the cardiomyocytes as they allow direct communication between the cytoplasm of adjacent cells, permitting free and voltage driven diffusion of ions. The Golgi complex is usually found adjacent to the lateral side of each nucleus in mammalian ventricular cardiomyocytes. Co-localized with each Golgi is the centrosome at which microtubules are nucleated and extend throughout the cell [28]. Sorting of proteins mainly takes place at the trans Golgi network (TGN) [29].
Figure 1. Organization of an adult ventricular cardiomyocyte.
Intercalated discs are located at the longitudinal sides of each ventricular cardiomyocyte to mediate cell-to-cell mechanical and electrical coupling. Mechanical coupling of cardiomyocytes is achieved through desmosomes and fascia adherens complexes. Gap junctions are primarily responsible for electrical coupling of the cardiomyocytes. T-tubules, which are rich in voltage-gated L-type calcium channels, are positioned closely to the sarcoplasmic reticulum, the internal calcium store. Sarcomeres form myofibrils, which are responsible for cardiomyocyte contraction upon intracellular calcium release. The Golgi apparatus and microtubules serve as the “loading dock” and “highways”, respectively, to deliver ion channels to specific subdomains on the plasma membrane. Mitochondria provide the energy needed for the contraction of cardiomyocytes.
2.1 Targeted Delivery
It is at the TGN that Cx43 oligomerizes into hemichannels. This is relatively late for such an event to occur, as other connexins oligomerize in the ER, but it may represent a means of controlling heteromeric hemichannel formation with other connexin isoforms [12]. Upon exiting the TGN, vesicles containing Cx43 hemichannels must navigate the complex cardiomyocyte intracellular environment, a feat they achieve by trafficking along dynamic microtubules.
Cargo proteins are sorted into post-Golgi carriers, which are docked onto molecular motors and delivered to the cell periphery along microtubules [30]. These extending microtubules form an intricate and dynamic outgoing network capable of shuttling Cx43 containing vesicles to their destinations [31-35]. In the context of trafficking, one can consider the Golgi to be the “loading dock” and microtubules the “highways” along which packets of channels are delivered to the plasma membrane. Along the microtubule highway, cytoplasmic and cortical actin cytoskeleton provides rest stops [36] to guide and redirect moving microtubules thus facilitating and tailoring en route cargo delivery as well as protein insertion into sarcolemma surface destination.
The mechanisms by which microtubules exert their specificity in interacting with membrane subdomains are now being elucidated. Our report in 2007 [33] and subsequent studies [37-39] have led to the Targeted Delivery model of channel delivery including Cx43. Targeted Delivery is the understanding that channels, once formed and exiting the Golgi, can be rapidly directed across the cytoplasm to their respective specific membrane subdomains. The highways for transport are microtubules whose negative ends originate at Golgi oriented microtubule-organizing centers and whose positive ends are growing outward and can be captured at the plasma membrane by membrane anchor proteins and complexes. Specificity of delivery is a combination of the individual channel, the plus-end-tracking proteins at the positive ends of microtubules which guide microtubule growth and capture, and the membrane bound anchor complex which captures the microtubule, completing the highway for channel delivery (Figure 2). Actin cytoskeleton serves as en route rest-stop stations to redirect microtubules [36], providing additional sorting site.
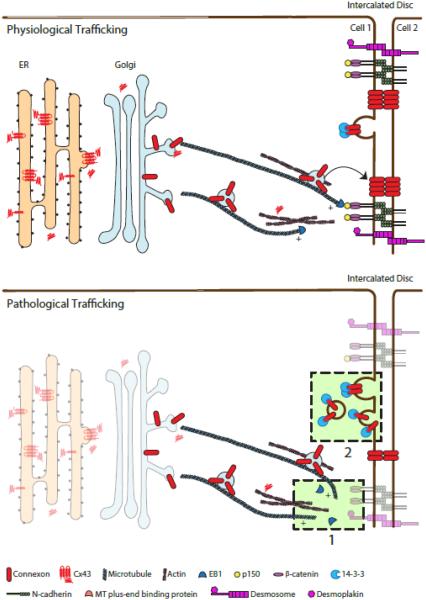
Figure 2. Channel trafficking in healthy and failing hearts.
Cx43 proteins are synthesized by ribosomes and multiple isoforms are produced as a result of alternative translation. (Top) The interaction between EB1, a microtubule plus-end binding protein, and the adherens junction complex ensures the targeted delivery of Cx43 hemichannels to the intercalated discs. Cx43 gap junctions on the plasma membrane undergo internalization for degradation. (Bottom) In failing cardiomyocytes, expression of Cx43 gap junctions on the cell surface is altered. As highlighted in the light green boxed areas, possible mechanisms underlying this change include (1) dissociation of microtubule plus-end binding proteins from microtubules; and (2) increased internalization of Cx43 gap junctions. Under oxidative stress EB1 dissociates from the tip of microtubules, impairing the attachment of microtubules to the adherens junction and the delivery of Cx43 to the intercalated discs. During acute cardiac ischemia 14-3-3 mediated internalization of Cx43 is increased, diminishing the amount of Cx43 channels on the plasma membrane.
A major plus-end binding protein, EB1, is known to be necessary for targeted delivery of connexons to adherens junction complexes [33]. Through interaction with another plus-end protein, p150GLUED, the EB1-tipped microtubule complexes specifically with β-catenin molecules at the fascia adherens of intercalated discs. Vesicular cargo is unloaded and subsequently inserted into the plasma membrane at nearby gap junctions. Other reports propose a less specific paradigm of connexin delivery, whereby connexons are inserted indiscriminately into the lateral membrane of the cell and freely diffuse to gap junction structures [6]. Both models can exist in parallel. However, the inefficiency of lateral diffusion to a few specific subdomains, the short half-life of connexins (1-3 hours in the myocardium) [40, 41], and the complex interactions between a single cell with multiple neighboring cardiomyocytes, all suggest directed targeting can be a more effective form of connexon localization to the intercalated disc.
In Targeted Delivery, specificity of delivery occurs near the membrane, in which a key aspect is the differential membrane bound anchor proteins at distinct membrane subregions. Membrane anchors are critical in capturing with specificity a subgroup of microtubules allowing channel delivery directly to regions of membrane that happen to contain the particular anchor. For Cx43 delivery to the intercalated disc, EB1-tipped microtubules bind to N-Cadherin associated β-catenin and also p150GLUED [33]. Desmoplakin may also be involved in capturing the EB1-tiped microtubule for Cx43 delivery [42], although the transmembrane domain still appears to be N-Cadherin rather than desmosomal desmoglein [43].
The Targeted Delivery model has since been supported by multiple subsequent reports [38, 44-47]. At the same time, important details of this delivery paradigm still continue to be elucidated, for instance Patel et al. recently reported that the desmosome associated linker protein desmoplakin binds to EB1, and is involved in targeted delivery of Cx43 to intercalated discs [42]. Non-sarcomeric actin has been shown to be necessary for Cx43 forward delivery [36, 48]. It remains to be determined how actin interacts with channels and the microtubule apparatus. At any given point in time, the majority of intracellular Cx43 channels are not moving rapidly on microtubules, but rather are stationary and associated with non-sarcomeric actin [36, 48].
Other than microtubules, there is increasing appreciation for the involvement of non-sarcomeric actin cytoskeleton in Targeted Delivery of Cx43. The fundamental question remains with regard to why actin is involved in Cx43 trafficking. If vesicles containing Cx43 can depart the Golgi and ride a microtubule highway straight to its proper subdomain, is there a need for actin filaments which appear to slow down vesicle transport? Actin can have at least two important roles in forward delivery of Cx43. The first is to help contribute specificity to delivery. Vesicles transported along microtubules on kinesin motors move rapidly, at a rate of about 1 micron per second [33]. Thus delivery to most locations at a cell membrane can occur within a minute. Association with important accessory proteins and post-translational modification of channels, both of which can affect delivery destination, probably also happen en route between the Golgi and membrane. Hopping off the microtubule highway on an actin “way station”, which is analogous to a highway rest stop with convenience stores, could allow Cx43 and the vesicle containing it to pick up accessory proteins and allow for needed post-translational modification. Such rest stops would occur at Z-disc, subcortical locations, or other important cytoskeleton intersections in the cytoplasm. These actin rest stops could also allow the Cx43 containing vesicles to use multiple microtubule highways in their delivery path. The Golgi exiting microtubule could be destined for an actin rest stop, allowing for a different membrane domain specific microtubule to finish the delivery. The second potential role for actin in microtubule based forward delivery pertains to the microtubules themselves. In non-myocyte systems, actin can help stabilize and guide microtubules [49, 50]. Actin could be the blueprint along and across which microtubule highways are patterned. In this respect, actin involvement could be an upstream to microtubules in determining location of Cx43 delivery.
2.2 Altered Cx43 Trafficking in Disease
Recent studies have explored forward trafficking of cardiac ion channels in different disease states. A difficulty with such studies is that the short life spans of individual channels (hours) are dwarfed by the chronicity (months, years and decades) of most failing hearts. A further complication is that dynamic channel behavior is best studied with in vitro cellular studies, well removed from intact animals and humans. A simple knockout mouse model establishes the importance of a channel or trafficking partner, but does not reveal the signaling interplay that occurs with other proteins during protein movements.
Trafficking related channel studies need to occur with cardiomyocytes intact, yet in environmental conditions that mimic those of failing heart. One important such condition is oxidative stress that occurs in ischemia-reperfusion injury as well as ischemic and non-ischemic heart failure. When isolated cardiomyocytes are subjected to oxidative stress, Cx43 gap junction delivery to intercalated discs is impaired due to disruption of the forward trafficking machinery [39]. Specifically, oxidative stress causes the microtubule plus-end protein EB1 to disassociate from the tips of microtubules, impairing microtubule attachment to adherens junction structures and subsequent delivery of Cx43 hemichannels to plasma membrane [39] (Figure 2). Manipulation of EB1 as well as the upstream regulators of EB1 localization at microtubules could potentially preserve or enhance gap junction coupling during stress. As many ion channels rely on microtubules for their transport, it is likely that such disruption of microtubule trafficking machinery inhibits delivery of many essential channels to the sarcolemma.
Such studies provide evidence that forward trafficking of Cx43 is impaired in acquired heart failure. At present we do not know how oxidative stress causes EB1 displacement and disassembly of the forward trafficking apparatus. We have preliminary investigations on the role of actin in maintaining EB1 based microtubule integrity, and the response of these cytoskeletal fibers to stress conditions. This remains an active area of investigation.
3. The Cx43 C-Terminal Carboxyl Tail
Ion channel function and trafficking are usually dependent and regulated by auxiliary protein subunits [51]. With regard to accessory proteins, Cx43 hemichannels are notable for, despite extensive examination, not being associated with their own unique β-subunits that assist in their trafficking. It turns out that Cx43 mRNA, through alternative translation, encodes its own trafficking subunits [52] which are N-terminal truncations of the full protein. These isoforms have potential roles in non-canonical functions of Cx43 as well.
3.1 The C-terminus and Non-canonical Roles of Cx43
The non-canonical roles of Cx43 include regulation of cellular processes such as gene expression, proliferation, migration, apoptosis, differentiation and cell survival [3, 53-55]. Interestingly, many of these channel-independent roles of Cx43 have been specifically attributed to its C-terminal domain. The cytosolic C-terminal tail of Cx43 (Cx43-CT) is the site of protein–protein interactions, contains multiple phosphorylation sites, and plays an important regulatory role in gap junction functions [3]. Cx43-CT has been shown to be effective in suppressing the growth of several cell types including Neuro2a [56], Hela [57], HEK293 [58] and primary cardiomyocytes [3]. In Hela cells, overexpressed Cx43-CT was observed to be enriched in the cytosol as well as the nucleus and thus it was suggested that the Cx43-CT may be able to exert its effects on gene expression directly [57]. Expression of Cx43-CT in U2OS cells was also shown to decrease cellular proliferation via suppressing Skp2 expression and thus increasing the levels of the cell cycle inhibitor p27 [59, 60]. In line with these findings, ectopic expression of a Cx43-CT fragment (aa 243-382 or CT243) in isolated cardiomyocytes led to upregulation of the tumor suppressor p53 and rendered the cardiomyocytes susceptible to mild ischemic conditions leading to increased cell death [3]. Interestingly however, expressing a slightly longer Cx43-CT fragment (aa 228-382 or CT228) in isolated cardiomyocytes did not cause upregulation of p53 unlike the CT243 fragment [3]. Thus it would be of interest to further examine the differences between these two CT fragments to better understand the variable functions of the Cx43-CT. Perhaps more importantly, fragments of Cx43-CT have been recently shown to be endogenously generated by alternative translation [52].
3.2 Alternative Translation of Cx43
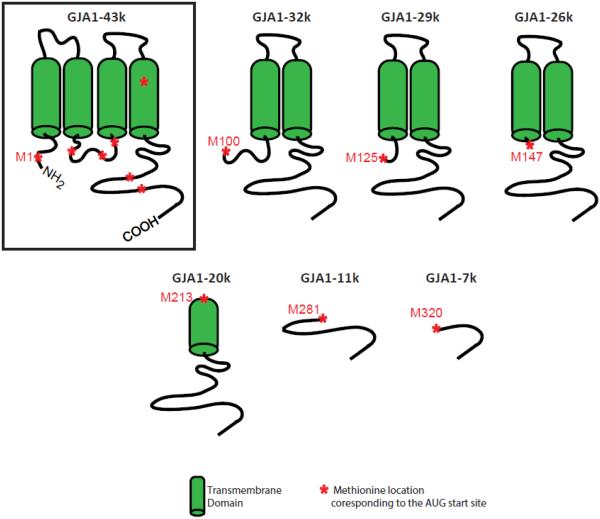
In order to understand alternative translation, it should be recognized that traditional translation of mRNA begins with the first coding triplet, which is always an AUG (Methionine). Most transcribed genes (mRNA strands) have other AUG sites downstream of the first one. The Cx43 protein has six Methionines, corresponding to the different AUG triplet translation start sites, beyond the first one (Figure 3). Alternative translation occurs when ribosomal translation initiates not at the first triplet, but at a downstream triplet. By initiating translation at downstream sites, alternative translation creates truncated proteins that lack the respective non-translated upstream (N-terminal) portions of the proteins.
Figure 3. Alternatively translated isoforms of Cx43.
Schematic showing the protein structure of full length Cx43 (GJA1-43k) and the structures of its 6 different alternatively translated isoforms (GJA1-32k, GJA1-29k, GJA1-26k, GJA1-20k, GJA1-11k and GJA1-7k). Cx43 alternative translation creates N-terminal truncated proteins lacking the respective non-translated upstream (N-terminal) portions of the Cx43 protein. The Methionine locations corresponding to the respective AUG start sites of the various Cx43 isoforms are marked by asterisks.
A naturally occurring Cx43 C-terminal fragment of around 20kDa in size was shown in cultured cells to be derived from a transcript encoded by the Cx43 gene, GJA1, and to be induced by cyclosporine [61]. This 20 kDa fragment was also observed in hearts of zebrafish together with other different sized fragments of Cx43 in other zebrafish organs [62]. GJA1 consists of two exons: non-coding exon 1 responsible for the 5′-UTR whereas exon 2 encodes the remaining 13 bp of this region, followed by the entire coding region of Cx43 and the 3′-UTR. Interestingly, an IRES element that allows cap independent translation has been found within the non-coding 5′-UTR region of GJA1 mRNA [63]. We have recently reported that the coding region of GJA1 mRNA occurs as a polycistronic molecule and that different N-terminal truncated isoforms of Cx43 protein arise from internal translation of the same mRNA molecule [52]. We have found that the GJA1 mRNA produces the expected full-length 43 kDa protein as well as proteins that are approximately 32 kDa, 29 kDa, 26 kDa, 20 kDa, 11 kDa and 7 kDa in size (Figure 3) with the 20 kDa isoform (GJA1-20k) being the predominate isoform in human heart tissue and several other cell lines [52]. This is the first evidence that alternative translation is possible for human ion channels and in human heart. These results have since been supported by a separate report showing that the GJA1-20k isoform is expressed in many cell lines that express high levels of full length Cx43 [64]. In addition, it has also been reported that this 20 kDa isoform is induced by hypoxic stimuli in the mouse brain and is the result of internal translation from an IRES element [65].
To explore the mechanism through which these Cx43 isoforms are generated, we performed a series of mutagenesis experiments of the internal AUG initiation codons and found that we were able to successfully abrogate the expression of the corresponding Cx43 protein isoform [52]. Furthermore, we found that inhibition of the PI3k/AKT signaling pathway or inhibition of the mammalian target of rapamycin (mTOR) pathway increased internal translation and protein levels of the GJA1-20k isoform. Since the mTOR pathway promotes cap-dependent translation [66], our data suggests that translation from internal Cx43 AUGs may follow a cap-independent mechanism [52]. In support of our data, Ul-Hussain et al. suggested the presence of an IRES element in the coding sequence of Cx43 at nucleotides 442–637 which is just before where the putative AUG of the 20-kDa fragment starts at nucleotide 638 [53, 65]. However, a report by Salat-Canela et al. suggests that unlike typical IRES sequences, the internal translation of GJA1 is not mediated through a bona fide IRES sequence alone, and the presence of an intact classical 5′ methylated cap structure appears to be required. Furthermore, in addition to capped RNA, upstream active translation or ribosomal scanning is required for efficient internal translation [53, 67]. Also, they showed that the Mnk1/2 kinase pathway, responsible for the phosphorylation of the translation initiation factor eIF4E, plays a role in regulating internal translation of the Cx43 transcript [67].
3.3 GJA1-20k as a Chaperone Protein in Targeted Delivery
We have found that at least one of the alternatively translated isoforms, GJA1-20k, is important for increasing the trafficking of Cx43 to the plasma membrane. Loss of all four of the following Cx43 isoforms; GJA1-32k, GJA1-29k, GJA1-26k and GJA1-20k, severely abrogated the formation of Cx43 gap junctions at the membrane [52]. Interestingly, reintroduction of the GJA1-20k isoform was sufficient to rescue the transport of Cx43 to the cell surface. The majority of ectopically expressed GJA1-20K remained localized primarily at cytoplasmic reticular structures which were confirmed to be the ER/Golgi network. The interaction between full length GJA1-43k and GJA1-20k in the ER was confirmed using co-immunoprecipitation assays where Brefeldin A (an inhibitor of protein transport from the ER to the Golgi) resulted in increased interactions between these two peptides. This data suggests a role of GJA1-20k isoform early in the Cx43 vesicular transport pathway and that this isoform may function as a cytoplasmic chaperone auxiliary protein for trafficking of de novo GJA1-43k molecules through the ER/Golgi complex to the membrane [52]. It remains to be determined how GJA1-20k contributes specificity to trafficking delivery. We expect that GJA1-20k is involved in cytoskeleton organization.
3.4 mTOR Signaling is a Regulator of GJA1-20K Expression and Cx43 Trafficking
The mTOR signaling pathway increases expression of the GJA1-20K isoform and Cx43 trafficking [52]. Our findings are that inhibiting the mTOR kinase activity in neonatal mouse ventricular cardiomyocytes not only resulted in upregulated GJA1-20k protein levels but also increased gap junction plaque size at the cardiomyocyte cell-cell border [52]. The mTOR pathway has already been implicated in cardiovascular physiology and pathology and the available evidence suggests that partial and selective inhibition of mTORC1 is cardioprotective during aging and cardiac stress. Inhibition of mTORC1 has also been shown to extend the life span of mice [68-70], to reduce cardiac hypertrophy and improve cardiac function in the presence of pressure overload [71-74] and genetic cardiomyopathies [75, 76] and to reduce ischemic injury after acute [77, 78] and chronic myocardial infarction [74, 79, 80]. Finally, the inhibition of mTORC1 reactivates cardiac autophagy, which is impaired in the presence of obesity and metabolic syndrome [77]. Because of the link between mTOR signaling and GJA1-20k, it would be interesting to examine the biological function of GJA1-20k in regulating these disease related processes.
4. Cx43 Internalization
Endocytosis of Cx43 can occur either through internalization of uncoupled hemichannels or entire gap junctions, which requires engulfment of gap junctions from the opposing neighboring cell plasma membrane as well. The internalized double-membrane intracellular structures are known as nonfunctional annular gap junctions. Both the lysosome and the proteasome have been implicated in degradation of Cx43 and interestingly, autophagy is now known to be involved in degradation of annular gap junctions in failing hearts [81]. Studies have shown that recycling of gap junctions occur during cell cycle progression in cell lines [82], but whether gap junctions are recycled in cardiomyocytes remains a controversial issue. It is exciting to consider the possibility that there exists a delicate balance and competition between the various posttranslational modification processes of Cx43 including phosphorylation [41, 83, 84], ubiquitination [85-87] and SUMOylation [88] that may act as checkpoints within the same connexin molecule, or connexon hemichannel to allow specific series of events to permit internalization and degradation of the hemichannel, or annular gap junction.
4.1 Internalization in Healthy Myocytes
Since Cx43 proteins are short lived and dynamically replaced, channel internalization from the plasma membrane also represents an important regulatory step in determining the level of gap junction coupling. Gap junction internalization can be induced by different posttranslational modifications such as ubiquitination, SUMOylation, acetylation, and phosphorylation. In the case of Cx43, phosphorylation is most well studied, and the importance of phosphorylation has been highlighted by recent findings that casein kinase-dependent phosphorylation alters gap junction remodeling and decreases arrhythmic susceptibility [83]. Many residues on the C-terminus of Cx43, specifically 22 serines, 5 tyrosines, and 4 threonines, are potentially subjected to phosphorylation. To make matters even more complex, Cx43 exists as a hexamer on the plasma membrane, and it is currently not known how phosphorylation differs between individual connexins of the same connexon. It is likely that a cascade of phosphorylation events occurs preceding ubiquitination of Cx43, which then leads to channel internalization and degradation [84, 89]. For example, it has been shown that Cx43 phosphorylation by EGF (epidermal growth factor) and TPA (12-O-tetradecanoylphorbol-13-acetate) promotes interaction between Cx43 and the E3 ubiquitin ligase Nedd4 (neuronal precursor cell-expressed developmentally down-regulated 4) leading to the subsequent ubiquitination of Cx43 [90, 91].
There is increasing evidence that Cx43 ubiquitination plays an important role in regulating gap junction internalization and degradation and several E3 ubiquitin ligases have been shown to regulate Cx43 internalization from the plasma membrane including TRIM21 [92], Smurf2 [93], and Nedd4 [94, 95]. Since these studies were done in cell culture systems, it still remains largely unclear how Cx43 ubiquitination is regulated in the cardiomyocytes. Nedd4 was the first described E3 ubiquitin ligase to be implicated in regulating Cx43 ubiquitination, internalization and autophagic degradation through a mechanism involving recruitment of the endocytotic adaptor Eps15 (epidermal growth factor receptor substrate 15) and the autophagic receptor p62 in cell lines [94, 96]. In neonatal rat cardiomyocytes, Nedd4 has also been reported to interact with Cx43 possibly regulating its ubiquitination and internalization in response to norepinephrine [97]. Further evidence implicating the role of Nedd4 in regulating Cx43 in myocytes was recently reported showing that only under basal conditions, silencing of Nedd4 in the HL-1 mouse atrial cell line led to increased Cx43 protein with a decrease in its ubiquitination levels [86]. Wwp1, which is a close family member to Nedd4, has been recently shown to interact with, ubiquitinate and degrade Cx43 in cell lines [87]. In addition, cardiomyocyte specific overexpression of Wwp1 in an inducible transgenic mouse model led to a significant reduction in Cx43 protein levels in the heart thus highlighting the importance of Wwp1 in regulating Cx43 turn over in the myocardium [87].
To add to the complexity of posttranslational regulation of Cx43, ubiquitinated Cx43 can also undergo reverse modification with the help of AMSH (associated molecule with the SH3 domain of STAM) which is a deubiquitinating enzyme or a deubiquitylase [98]. AMSH was found to interact with Cx43 in HEK293 cells, catalyzing the removal of ubiquitin which is preferentially attached to Cx43 through the K-63 ubiquitin chain linkage. In addition, AMSH was found to colocalize with Cx43 at gap junction plaque sites where it mediated the deubiquitination of Cx43 thus stabilizing the protein at the plasma membrane and protecting it from internalization and degradation [98]. Although deubiquitination seems to play an important role in regulating Cx43 stability in cell lines, its role in the cardiomyocytes has yet to be elucidated.
In addition to ubiquitination, Cx43 has also been reported to be covalently modified by SUMOylation in Hela cells [88]. The conjugation of SUMO molecules, which are ubiquitin like modifiers, to lysine residues 144 and 237 found in the cytoplasmic loop and the C-terminal tail of Cx43 respectively led to increased levels of Cx43 protein and more gap junctions forming at the plasma membrane [88]. Interestingly, the majority of the SUMOylated Cx43 was found in the triton soluble fraction, which includes non-junctional Cx43, thus the authors of that study suggested that SUMOylation of Cx43 may occur during its route to form gap junctions or after it has been internalized [88]. The effect of SUMOylation on Cx43 life cycle and internalization is still not well understood and it would be interesting to further examine this process particularly in cardiomyocytes.
4.2 Internalization in Disease Myocytes
The short half-life of Cx43 in the myocardium (1-3 hours) [40, 41], suggests an intricate and sequential interplay between phosphorylation, ubiquitination, SUMOlyation and their reverse modifications in order to help maintain regulation of Cx43 turnover in the healthy heart and which might otherwise lead to cardiac disease. Our experience with Cx43 protein is that post-translational modification preferentially affects ion channel internalization. Pathological gap junction remodeling is strongly associated with altered phosphorylation of Cx43 [12, 99, 100]. Rather than individual independent phosphorylation events of singular residues at the C-terminus, it is likely that internalization results from a sophisticated cascade of posttranslational modifications. The Cx43 C-terminus contains a phosphorylation-dependent 14-3-3 binding motif at Serine 373 (within 10 amino acids of the end of the protein). 14-3-3 proteins are known to regulate protein transport and have been implicated in facilitating de novo Cx43 transport from ER to Golgi apparatus [101, 102]. Phosphorylation of Ser373 and subsequent 14-3-3 binding provide a gateway to a signaling cascade of downstream phosphorylation of Ser368, leading to gap junction ubiquitination, internalization and degradation during acute cardiac ischemia [41].
The C-terminus of Cx43 is the main protein-protein interaction domain responsible for Cx43 binding to its partners within the cell [103]. In close proximity to the Cx43 14-3-3 binding motif is a PDZ domain at the distal end of the C-terminus. It is through this PDZ domain that Cx43 interacts with ZO-1 [104], and this interaction has been demonstrated to regulate Cx43 gap junction plaque size and assembly [105, 106]. Disruption of Cx43/ZO-1 complexing has been reported to increase gap junction plaque size in cultured cells [107, 108]. Phosphorylation of Cx43 Serine373 can disrupt interaction with ZO-1 [109], and indeed it would be sterically unlikely for both 14-3-3 and ZO-1 to bind the same Cx43 protomer simultaneously. However, increased Cx43/ZO-1 interaction has also been associated with gap junction remodeling, highlighting the complex nature of these dynamic posttranslational and protein complexing events [110, 111].
Acute cardiac ischemic injury in isolated rat hearts has been shown to cause increased ubiquitination of Cx43 at the intercalated discs accompanied by increased interaction between Cx43 and Nedd4 [85]. However, silencing of Nedd4 in HL-1 mouse atrial cells subjected to ischemic conditions did not have any significant effect on Cx43 ubiquitination nor degradation and only under basal conditions did the knockdown of Nedd4 prevent ubiquitination and degradation of Cx43 [86]. This suggests that other E3 ubiquitin ligases besides Nedd4 may regulate Cx43 ubiquitination and degradation in cardiac injury. Indeed it has been recently reported that cardiomyocyte specific overexpression of Wwp1 in an inducible transgenic mouse model caused a significant reduction in Cx43 protein levels in the heart leading to the development of lethal left ventricular arrhythmias [87].
5. Conclusions
The individual cardiomyocyte is a highly complex and dynamic system with internal organization designed to maintain efficient cell-cell communication. To maintain intracellular homeostasis as well as overall synchrony across the myocardium, cardiomyocytes regulate Cx43 intracellular movement and localization through highly sophisticated and highly efficient protein trafficking machineries. The short life span of Cx43 suggests that there needs to be efficiency in its life-cycle and movements which follow the order of: formation, delivery to the correct subdomain on plasma membrane, and internalization back into the cell. In diseased hearts, cardiomyocyte structures and organization are negatively affected by environmental conditions of stress thus impacting Cx43 channel trafficking and function. As the physiologic movements of cardiac Cx43 are elucidated, and then disease related changes of these movements are understood, interventions can be designed to promote positive intracellular remodeling. Identification of intracellular pathways critical in stress response during heart failure progression will provide new targets for development of interventions to help restore normal myocyte function. Therefore, the newly appreciated role of the Cx43 internally translated isoforms in protein trafficking provide a new insight into the trafficking regulatory mechanism of Cx43 which potentially opens the door for new models of targeted therapies and therapeutic interventions.
Highlights.
Major Changes in the Revised Manuscript are:
1) New detailed information regarding Cx43 ubiquitination, deubiquitination, and SUMOylation have been added to sections 4.1 and 4.2.
2) The concept of alternative translation is now introduced at the beginning of section 3.2 to help familiarize the readers with the general process before getting into the specifics of Cx43 alternative translation.
3) New Figure 3 has been added which includes a schematic showing the protein structure of full length Cx43 and the structures of all of its detected alternatively translated isoforms.
Acknowledgments
We thank our funding sources American Heart Association (Shaw, Fu, 13EIA4480016) and National Institute of Health / National Heart, Lung, and Blood Institute (NIH/NHLBI, Shaw, R01-HL094414).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Willecke K, Eiberger J, Degen J, Eckardt D, Romualdi A, Guldenagel M, Deutsch U, Sohl G. Structural and functional diversity of connexin genes in the mouse and human genome. Biol Chem. 2002;383:725–737. doi: 10.1515/BC.2002.076. [DOI] [PubMed] [Google Scholar]
- [2].Beyer EC. Gap junctions. International review of cytology. 1993;137C:1–37. [PubMed] [Google Scholar]
- [3].Kardami E, Dang X, Iacobas DA, Nickel BE, Jeyaraman M, Srisakuldee W, Makazan J, Tanguy S, Spray DC. The role of connexins in controlling cell growth and gene expression. Prog Biophys Mol Biol. 2007;94:245–264. doi: 10.1016/j.pbiomolbio.2007.03.009. [DOI] [PubMed] [Google Scholar]
- [4].Schulz R, Gorge PM, Gorbe A, Ferdinandy P, Lampe PD, Leybaert L. Connexin 43 is an emerging therapeutic target in ischemia/reperfusion injury, cardioprotection and neuroprotection. Pharmacology & therapeutics. 2015;153:90–106. doi: 10.1016/j.pharmthera.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Evans WH, Martin PE. Gap junctions: structure and function (Review) Mol Membr Biol. 2002;19:121–136. doi: 10.1080/09687680210139839. [DOI] [PubMed] [Google Scholar]
- [6].Laird DW. Life cycle of connexins in health and disease. Biochem J. 2006;394:527–543. doi: 10.1042/BJ20051922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Noorman M, van der Heyden MA, van Veen TA, Cox MG, Hauer RN, de Bakker JM, van Rijen HV. Cardiac cell-cell junctions in health and disease: Electrical versus mechanical coupling. J Mol Cell Cardiol. 2009;47:23–31. doi: 10.1016/j.yjmcc.2009.03.016. [DOI] [PubMed] [Google Scholar]
- [8].Unwin PN, Zampighi G. Structure of the junction between communicating cells. Nature. 1980;283:545–549. doi: 10.1038/283545a0. [DOI] [PubMed] [Google Scholar]
- [9].Saez JC, Berthoud VM, Branes MC, Martinez AD, Beyer EC. Plasma membrane channels formed by connexins: Their regulation and functions. Physiological Reviews. 2003;83:1359–1400. doi: 10.1152/physrev.00007.2003. [DOI] [PubMed] [Google Scholar]
- [10].Rohr S. Role of gap junctions in the propagation of the cardiac action potential. Cardiovasc Res. 2004;62:309–322. doi: 10.1016/j.cardiores.2003.11.035. [DOI] [PubMed] [Google Scholar]
- [11].Shaw RM, Rudy Y. Ionic mechanisms of propagation in cardiac tissue. Roles of the sodium and L-type calcium currents during reduced excitability and decreased gap junction coupling. Circulation research. 1997;81:727–741. doi: 10.1161/01.res.81.5.727. [DOI] [PubMed] [Google Scholar]
- [12].Hesketh GG, Van Eyk JE, Tomaselli GF. Mechanisms of gap junction traffic in health and disease. J Cardiovasc Pharmacol. 2009;54:263–272. doi: 10.1097/FJC.0b013e3181ba0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Doring B, Shynlova O, Tsui P, Eckardt D, Janssen-Bienhold U, Hofmann F, Feil S, Feil R, Lye SJ, Willecke K. Ablation of connexin43 in uterine smooth muscle cells of the mouse causes delayed parturition. J Cell Sci. 2006;119:1715–1722. doi: 10.1242/jcs.02892. [DOI] [PubMed] [Google Scholar]
- [14].Saffitz JE, Hames KY, Kanno S. Remodeling of gap junctions in ischemic and nonischemic forms of heart disease. J Membr Biol. 2007;218:65–71. doi: 10.1007/s00232-007-9031-2. [DOI] [PubMed] [Google Scholar]
- [15].Gutstein DE, Morley GE, Vaidya D, Liu F, Chen FL, Stuhlmann H, Fishman GI. Heterogeneous expression of Gap junction channels in the heart leads to conduction defects and ventricular dysfunction. Circulation. 2001;104:1194–1199. doi: 10.1161/hc3601.093990. [DOI] [PubMed] [Google Scholar]
- [16].van Rijen HV, van Veen TA, Gros D, Wilders R, de Bakker JM. Connexins and cardiac arrhythmias. Adv Cardiol. 2006;42:150–160. doi: 10.1159/000092567. [DOI] [PubMed] [Google Scholar]
- [17].Danik SB, Liu F, Zhang J, Suk HJ, Morley GE, Fishman GI, Gutstein DE. Modulation of cardiac gap junction expression and arrhythmic susceptibility. Circulation research. 2004;95:1035–1041. doi: 10.1161/01.RES.0000148664.33695.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lerner DL, Yamada KA, Schuessler RB, Saffitz JE. Accelerated onset and increased incidence of ventricular arrhythmias induced by ischemia in Cx43-deficient mice. Circulation. 2000;101:547–552. doi: 10.1161/01.cir.101.5.547. [DOI] [PubMed] [Google Scholar]
- [19].Poelzing S, Rosenbaum DS. Altered connexin43 expression produces arrhythmia substrate in heart failure. American Journal of Physiology-Heart and Circulatory Physiology. 2004;287:H1762–H1770. doi: 10.1152/ajpheart.00346.2004. [DOI] [PubMed] [Google Scholar]
- [20].Lo CW. Role of gap junctions in cardiac conduction and development: insights from the connexin knockout mice. Circulation research. 2000;87:346–348. doi: 10.1161/01.res.87.5.346. [DOI] [PubMed] [Google Scholar]
- [21].Saffitz JE. Arrhythmogenic cardiomyopathy and abnormalities of cell-to-cell coupling. Heart Rhythm. 2009;6:S62–65. doi: 10.1016/j.hrthm.2009.03.003. [DOI] [PubMed] [Google Scholar]
- [22].Sepp R, Severs NJ, Gourdie RG. Altered patterns of cardiac intercellular junction distribution in hypertrophic cardiomyopathy. Heart. 1996;76:412–417. doi: 10.1136/hrt.76.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Peters NS. New insights into myocardial arrhythmogenesis: Distribution of gap-junctional coupling in normal, ischaemic and hypertrophied human hearts - Glaxo/MRS Young Investigator Prize. Clinical science. 1996;90:447–452. doi: 10.1042/cs0900447. [DOI] [PubMed] [Google Scholar]
- [24].Jongsma HJ, Wilders R. Gap junctions in cardiovascular disease. Circulation research. 2000;86:1193–1197. doi: 10.1161/01.res.86.12.1193. [DOI] [PubMed] [Google Scholar]
- [25].Kostin S, Rieger M, Dammer S, Hein S, Richter M, Klovekorn WP, Bauer EP, Schaper J. Gap junction remodeling and altered connexin43 expression in the failing human heart. Mol. Cell. Biochem. 2003;242:135–144. [PubMed] [Google Scholar]
- [26].Kitamura H, Ohnishi Y, Yoshida A, Okajima K, Azumi H, Ishida A, Galeano EJ, Kubo S, Hayashi Y, Itoh H, Yokoyama M. Heterogeneous loss of connexin43 protein in nonischemic dilated cardiomyopathy with ventricular tachycardia. J Cardiovasc Electrophysiol. 2002;13:865–870. doi: 10.1046/j.1540-8167.2002.00865.x. [DOI] [PubMed] [Google Scholar]
- [27].Dupont E, Matsushita T, Kaba RA, Vozzi C, Coppen SR, Khan N, Kaprielian R, Yacoub MH, Severs NJ. Altered connexin expression in human congestive heart failure. J Mol Cell Cardiol. 2001;33:359–371. doi: 10.1006/jmcc.2000.1308. [DOI] [PubMed] [Google Scholar]
- [28].de Forges H, Bouissou A, Perez F. Interplay between microtubule dynamics and intracellular organization. Int J Biochem Cell Biol. 2012;44:266–274. doi: 10.1016/j.biocel.2011.11.009. [DOI] [PubMed] [Google Scholar]
- [29].Gu F, Crump CM, Thomas G. Trans-Golgi network sorting. Cellular and molecular life sciences : CMLS. 2001;58:1067–1084. doi: 10.1007/PL00000922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Luini A, Mironov AA, Polishchuk EV, Polishchuk RS. Morphogenesis of post-Golgi transport carriers. Histochemistry and cell biology. 2008;129:153–161. doi: 10.1007/s00418-007-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hamm-Alvarez SF, Sheetz MP. Microtubule-dependent vesicle transport: modulation of channel and transporter activity in liver and kidney. Physiol Rev. 1998;78:1109–1129. doi: 10.1152/physrev.1998.78.4.1109. [DOI] [PubMed] [Google Scholar]
- [32].Gaietta G, Deerinck TJ, Adams SR, Bouwer J, Tour O, Laird DW, Sosinsky GE, Tsien RY, Ellisman MH. Multicolor and electron microscopic imaging of connexin trafficking. Science. 2002;296:503–507. doi: 10.1126/science.1068793. [DOI] [PubMed] [Google Scholar]
- [33].Shaw RM, Fay AJ, Puthenveedu MA, von Zastrow M, Jan YN, Jan LY. Microtubule plus-end-tracking proteins target gap junctions directly from the cell interior to adherens junctions. Cell. 2007;128:547–560. doi: 10.1016/j.cell.2006.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Johnson RG, Meyer RA, Li XR, Preus DM, Tan L, Grunenwald H, Paulson AF, Laird DW, Sheridan JD. Gap junctions assemble in the presence of cytoskeletal inhibitors, but enhanced assembly requires microtubules. Exp Cell Res. 2002;275:67–80. doi: 10.1006/excr.2002.5480. [DOI] [PubMed] [Google Scholar]
- [35].Lauf U, Giepmans BN, Lopez P, Braconnot S, Chen SC, Falk MM. Dynamic trafficking and delivery of connexons to the plasma membrane and accretion to gap junctions in living cells. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:10446–10451. doi: 10.1073/pnas.162055899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Smyth JW, Vogan JM, Buch PJ, Zhang SS, Fong TS, Hong TT, Shaw RM. Actin cytoskeleton rest stops regulate anterograde traffic of connexin 43 vesicles to the plasma membrane. Circulation research. 2012;110:978–989. doi: 10.1161/CIRCRESAHA.111.257964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Hong TT, Smyth JW, Chu KY, Vogan JM, Fong TS, Jensen BC, Fang K, Halushka MK, Russell SD, Colecraft H, Hoopes CW, Ocorr K, Chi NC, Shaw RM. BIN1 is reduced and Cav1.2 trafficking is impaired in human failing cardiomyocytes. Heart Rhythm. 2012;9:812–820. doi: 10.1016/j.hrthm.2011.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hong TT, Smyth JW, Gao D, Chu KY, Vogan JM, Fong TS, Jensen BC, Colecraft HM, Shaw RM. BIN1 localizes the L-type calcium channel to cardiac T-tubules. PLoS biology. 2010;8:e1000312. doi: 10.1371/journal.pbio.1000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Smyth JW, Hong TT, Gao D, Vogan JM, Jensen BC, Fong TS, Simpson PC, Stainier DY, Chi NC, Shaw RM. Limited forward trafficking of connexin 43 reduces cell-cell coupling in stressed human and mouse myocardium. J Clin Invest. 2010;120:266–279. doi: 10.1172/JCI39740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Beardslee MA, Laing JG, Beyer EC, Saffitz JE. Rapid turnover of connexin43 in the adult rat heart. Circulation research. 1998;83:629–635. doi: 10.1161/01.res.83.6.629. [DOI] [PubMed] [Google Scholar]
- [41].Smyth JW, Zhang SS, Sanchez JM, Lamouille S, Vogan JM, Hesketh GG, Hong T, Tomaselli GF, Shaw RM. A 14-3-3 mode-1 binding motif initiates gap junction internalization during acute cardiac ischemia. Traffic. 2014;15:684–699. doi: 10.1111/tra.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Patel DM, Dubash AD, Kreitzer G, Green KJ. Disease mutations in desmoplakin inhibit Cx43 membrane targeting mediated by desmoplakin-EB1 interactions. J Cell Biol. 2014;206:779–797. doi: 10.1083/jcb.201312110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Shaw RM. Desmosomal hotspots, microtubule delivery, and cardiac arrhythmogenesis. Developmental cell. 2014;31:139–140. doi: 10.1016/j.devcel.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ligon LA, Holzbaur EL. Microtubules tethered at epithelial cell junctions by dynein facilitate efficient junction assembly. Traffic. 2007;8:808–819. doi: 10.1111/j.1600-0854.2007.00574.x. [DOI] [PubMed] [Google Scholar]
- [45].Levy JR, Holzbaur EL. Special delivery: dynamic targeting via cortical capture of microtubules. Developmental cell. 2007;12:320–322. doi: 10.1016/j.devcel.2007.02.012. [DOI] [PubMed] [Google Scholar]
- [46].Hendricks AG, Lazarus JE, Perlson E, Gardner MK, Odde DJ, Goldman YE, Holzbaur EL. Dynein tethers and stabilizes dynamic microtubule plus ends. Curr Biol. 2012;22:632–637. doi: 10.1016/j.cub.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Chkourko HS, Guerrero-Serna G, Lin X, Darwish N, Pohlmann JR, Cook KE, Martens JR, Rothenberg E, Musa H, Delmar M. Remodeling of mechanical junctions and of microtubule-associated proteins accompany cardiac connexin43 lateralization. Heart Rhythm. 2012;9:1133–1140. doi: 10.1016/j.hrthm.2012.03.003. e1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Zhang SS, Hong S, Kleber AG, Lee LP, Shaw RM. A micropatterning approach for imaging dynamic Cx43 trafficking to cell-cell borders. FEBS Lett. 2014;588:1439–1445. doi: 10.1016/j.febslet.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Bartolini F, Ramalingam N, Gundersen GG. Actin-capping protein promotes microtubule stability by antagonizing the actin activity of mDia1. Mol Biol Cell. 2012;23:4032–4040. doi: 10.1091/mbc.E12-05-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Wittmann T, Bokoch GM, Waterman-Storer CM. Regulation of leading edge microtubule and actin dynamics downstream of Rac1. J Cell Biol. 2003;161:845–851. doi: 10.1083/jcb.200303082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Smyth JW, Shaw RM. Forward trafficking of ion channels: what the clinician needs to know. Heart Rhythm. 2010;7:1135–1140. doi: 10.1016/j.hrthm.2010.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Smyth JW, Shaw RM. Autoregulation of connexin43 gap junction formation by internally translated isoforms. Cell Rep. 2013;5:611–618. doi: 10.1016/j.celrep.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Salat-Canela C, Munoz MJ, Sese M, Ramon y Cajal S, Aasen T. Post-transcriptional regulation of connexins. Biochem Soc Trans. 2015;43:465–470. doi: 10.1042/BST20150033. [DOI] [PubMed] [Google Scholar]
- [54].Aasen T. Connexins: junctional and non-junctional modulators of proliferation. Cell Tissue Res. 2015;360:685–699. doi: 10.1007/s00441-014-2078-3. [DOI] [PubMed] [Google Scholar]
- [55].Zhou JZ, Jiang JX. Gap junction and hemichannel-independent actions of connexins on cell and tissue functions--an update. FEBS Lett. 2014;588:1186–1192. doi: 10.1016/j.febslet.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Moorby C, Patel M. Dual functions for connexins: Cx43 regulates growth independently of gap junction formation. Exp Cell Res. 2001;271:238–248. doi: 10.1006/excr.2001.5357. [DOI] [PubMed] [Google Scholar]
- [57].Dang X, Doble BW, Kardami E. The carboxy-tail of connexin-43 localizes to the nucleus and inhibits cell growth. Mol Cell Biochem. 2003;242:35–38. [PubMed] [Google Scholar]
- [58].Dang X, Jeyaraman M, Kardami E. Regulation of connexin-43-mediated growth inhibition by a phosphorylatable amino-acid is independent of gap junction-forming ability. Mol Cell Biochem. 2006;289:201–207. doi: 10.1007/s11010-006-9162-2. [DOI] [PubMed] [Google Scholar]
- [59].Zhang YW, Kaneda M, Morita I. The gap junction-independent tumor-suppressing effect of connexin 43. Journal of Biological Chemistry. 2003;278:44852–44856. doi: 10.1074/jbc.M305072200. [DOI] [PubMed] [Google Scholar]
- [60].Zhang YW, Nakayama K, Nakayama K, Morita I. A novel route for connexin 43 to inhibit cell proliferation: negative regulation of S-phase kinase-associated protein (Skp 2) Cancer Res. 2003;63:1623–1630. [PubMed] [Google Scholar]
- [61].Joshi-Mukherjee R, Coombs W, Burrer C, de Mora IA, Delmar M, Taffet SM. Evidence for the presence of a free C-terminal fragment of cx43 in cultured cells. Cell Commun Adhes. 2007;14:75–84. doi: 10.1080/15419060701402320. [DOI] [PubMed] [Google Scholar]
- [62].Chatterjee B, Chin AJ, Valdimarsson G, Finis C, Sonntag JM, Choi BY, Tao L, Balasubramanian K, Bell C, Krufka A, Kozlowski DJ, Johnson RG, Lo CW. Developmental regulation and expression of the zebrafish connexin43 gene. Dev Dyn. 2005;233:890–906. doi: 10.1002/dvdy.20426. [DOI] [PubMed] [Google Scholar]
- [63].Schiavi A, Hudder A, Werner R. Connexin43 mRNA contains a functional internal ribosome entry site. FEBS Lett. 1999;464:118–122. doi: 10.1016/s0014-5793(99)01699-3. [DOI] [PubMed] [Google Scholar]
- [64].Salat-Canela C, Sese M, Peula C, Ramon YCS, Aasen T. Internal translation of the connexin 43 transcript. Cell communication and signaling : CCS. 2014;12:31. doi: 10.1186/1478-811X-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Ul-Hussain M, Olk S, Schoenebeck B, Wasielewski B, Meier C, Prochnow N, May C, Galozzi S, Marcus K, Zoidl G, Dermietzel R. Internal Ribosomal Entry Site (IRES) Activity Generates Endogenous Carboxyl-terminal Domains of Cx43 and Is Responsive to Hypoxic Conditions. J Biol Chem. 2014;289:20979–20990. doi: 10.1074/jbc.M113.540187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Laplante M, Sabatini DM. mTOR signaling at a glance. J Cell Sci. 2009;122:3589–3594. doi: 10.1242/jcs.051011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Salat-Canela C, Sese M, Peula C, Ramon y Cajal S, Aasen T. Internal translation of the connexin 43 transcript. Cell communication and signaling : CCS. 2014;12:31. doi: 10.1186/1478-811X-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Harrison DE, Strong R, Sharp ZD, Nelson JF, Astle CM, Flurkey K, Nadon NL, Wilkinson JE, Frenkel K, Carter CS, Pahor M, Javors MA, Fernandez E, Miller RA. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Flynn JM, O'Leary MN, Zambataro CA, Academia EC, Presley MP, Garrett BJ, Zykovich A, Mooney SD, Strong R, Rosen CJ, Kapahi P, Nelson MD, Kennedy BK, Melov S. Late-life rapamycin treatment reverses age-related heart dysfunction. Aging Cell. 2013;12:851–862. doi: 10.1111/acel.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Wu JJ, Liu J, Chen EB, Wang JJ, Cao L, Narayan N, Fergusson MM, Rovira, Allen M, Springer DA, Lago CU, Zhang S, DuBois W, Ward T, deCabo R, Gavrilova O, Mock B, Finkel T. Increased mammalian lifespan and a segmental and tissue-specific slowing of aging after genetic reduction of mTOR expression. Cell Rep. 2013;4:913–920. doi: 10.1016/j.celrep.2013.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Shioi T, McMullen JR, Tarnavski O, Converso K, Sherwood MC, Manning WJ, Izumo S. Rapamycin attenuates load-induced cardiac hypertrophy in mice. Circulation. 2003;107:1664–1670. doi: 10.1161/01.CIR.0000057979.36322.88. [DOI] [PubMed] [Google Scholar]
- [72].McMullen JR, Sherwood MC, Tarnavski O, Zhang L, Dorfman AL, Shioi T, Izumo S. Inhibition of mTOR signaling with rapamycin regresses established cardiac hypertrophy induced by pressure overload. Circulation. 2004;109:3050–3055. doi: 10.1161/01.CIR.0000130641.08705.45. [DOI] [PubMed] [Google Scholar]
- [73].Volkers M, Toko H, Doroudgar S, Din S, Quijada P, Joyo AY, Ornelas L, Joyo E, Thuerauf DJ, Konstandin MH, Gude N, Glembotski CC, Sussman MA. Pathological hypertrophy amelioration by PRAS40-mediated inhibition of mTORC1. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:12661–12666. doi: 10.1073/pnas.1301455110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Wu X, Cao Y, Nie J, Liu H, Lu S, Hu X, Zhu J, Zhao X, Chen J, Chen X, Yang Z, Li X. Genetic and pharmacological inhibition of Rheb1-mTORC1 signaling exerts cardioprotection against adverse cardiac remodeling in mice. The American journal of pathology. 2013;182:2005–2014. doi: 10.1016/j.ajpath.2013.02.012. [DOI] [PubMed] [Google Scholar]
- [75].Marin TM, Keith K, Davies B, Conner DA, Guha P, Kalaitzidis D, Wu X, Lauriol J, Wang B, Bauer M, Bronson R, Franchini KG, Neel BG, Kontaridis MI. Rapamycin reverses hypertrophic cardiomyopathy in a mouse model of LEOPARD syndrome-associated PTPN11 mutation. J Clin Invest. 2011;121:1026–1043. doi: 10.1172/JCI44972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Ramos FJ, Chen SC, Garelick MG, Dai DF, Liao CY, Schreiber KH, MacKay VL, An EH, Strong R, Ladiges WC, Rabinovitch PS, Kaeberlein M, Kennedy BK. Rapamycin reverses elevated mTORC1 signaling in lamin A/C-deficient mice, rescues cardiac and skeletal muscle function, and extends survival. Sci Transl Med. 2012;4:144ra103. doi: 10.1126/scitranslmed.3003802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Sciarretta S, Zhai P, Shao D, Maejima Y, Robbins J, Volpe M, Condorelli G, Sadoshima J. Rheb is a critical regulator of autophagy during myocardial ischemia: pathophysiological implications in obesity and metabolic syndrome. Circulation. 2012;125:1134–1146. doi: 10.1161/CIRCULATIONAHA.111.078212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Zhai P, Sciarretta S, Galeotti J, Volpe M, Sadoshima J. Differential roles of GSK-3beta during myocardial ischemia and ischemia/reperfusion. Circulation research. 2011;109:502–511. doi: 10.1161/CIRCRESAHA.111.249532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Buss SJ, Muenz S, Riffel JH, Malekar P, Hagenmueller M, Weiss CS, Bea F, Bekeredjian R, Schinke-Braun M, Izumo S, Katus HA, Hardt SE. Beneficial effects of Mammalian target of rapamycin inhibition on left ventricular remodeling after myocardial infarction. J Am Coll Cardiol. 2009;54:2435–2446. doi: 10.1016/j.jacc.2009.08.031. [DOI] [PubMed] [Google Scholar]
- [80].Volkers M, Konstandin MH, Doroudgar S, Toko H, Quijada P, Din S, Joyo A, Ornelas L, Samse K, Thuerauf DJ, Gude N, Glembotski CC, Sussman MA. Mechanistic target of rapamycin complex 2 protects the heart from ischemic damage. Circulation. 2013;128:2132–2144. doi: 10.1161/CIRCULATIONAHA.113.003638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Hesketh GG, Shah MH, Halperin VL, Cooke CA, Akar FG, Yen TE, Kass DA, Machamer CE, Van Eyk JE, Tomaselli GF. Ultrastructure and regulation of lateralized connexin43 in the failing heart. Circulation research. 2010;106:1153–1163. doi: 10.1161/CIRCRESAHA.108.182147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Boassa D, Solan JL, Papas A, Thornton P, Lampe PD, Sosinsky GE. Trafficking and recycling of the connexin43 gap junction protein during mitosis. Traffic. 2010;11:1471–1486. doi: 10.1111/j.1600-0854.2010.01109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Remo BF, Qu J, Volpicelli FM, Giovannone S, Shin D, Lader J, Liu FY, Zhang J, Lent DS, Morley GE, Fishman GI. Phosphatase-resistant gap junctions inhibit pathological remodeling and prevent arrhythmias. Circulation research. 2011;108:1459–1466. doi: 10.1161/CIRCRESAHA.111.244046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Leithe E, Rivedal E. Ubiquitination and down-regulation of gap junction protein connexin-43 in response to 12-O-tetradecanoylphorbol 13-acetate treatment. J Biol Chem. 2004;279:50089–50096. doi: 10.1074/jbc.M402006200. [DOI] [PubMed] [Google Scholar]
- [85].Martins-Marques T, Catarino S, Marques C, Matafome P, Ribeiro-Rodrigues T, Baptista R, Pereira P, Girao H. Heart ischemia results in connexin43 ubiquitination localized at the intercalated discs. Biochimie. 2015;112:196–201. doi: 10.1016/j.biochi.2015.02.020. [DOI] [PubMed] [Google Scholar]
- [86].Martins-Marques T, Catarino S, Zuzarte M, Marques C, Matafome P, Pereira P, Girao H. Ischaemia-induced autophagy leads to degradation of gap junction protein connexin43 in cardiomyocytes. Biochem J. 2015;467:231–245. doi: 10.1042/BJ20141370. [DOI] [PubMed] [Google Scholar]
- [87].Basheer WA, Harris BS, Mentrup HL, Abreha M, Thames EL, Lea JB, Swing DA, Copeland NG, Jenkins NA, Price RL, Matesic LE. Cardiomyocyte-specific overexpression of the ubiquitin ligase Wwp1 contributes to reduction in Connexin 43 and arrhythmogenesis. J Mol Cell Cardiol. 2015;88:1–13. doi: 10.1016/j.yjmcc.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Kjenseth A, Fykerud TA, Sirnes S, Bruun J, Yohannes Z, Kolberg M, Omori Y, Rivedal E, Leithe E. The gap junction channel protein connexin 43 is covalently modified and regulated by SUMOylation. J Biol Chem. 2012;287:15851–15861. doi: 10.1074/jbc.M111.281832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Leithe E, Rivedal E. Epidermal growth factor regulates ubiquitination, internalization and proteasome-dependent degradation of connexin43. Journal of Cell Science. 2004;117:1211–1220. doi: 10.1242/jcs.00951. [DOI] [PubMed] [Google Scholar]
- [90].Leykauf K, Salek M, Bomke J, Frech M, Lehmann WD, Durst M, Alonso A. Ubiquitin protein ligase Nedd4 binds to connexin43 by a phosphorylation-modulated process. J Cell Sci. 2006;119:3634–3642. doi: 10.1242/jcs.03149. [DOI] [PubMed] [Google Scholar]
- [91].Fong JT, Nimlamool W, Falk MM. EGF induces efficient Cx43 gap junction endocytosis in mouse embryonic stem cell colonies via phosphorylation of Ser262, Ser279/282, and Ser368. FEBS Lett. 2014;588:836–844. doi: 10.1016/j.febslet.2014.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Chen VC, Kristensen AR, Foster LJ, Naus CC. Association of Connexin43 with E3 Ubiquitin Ligase TRIM21 Reveals a Mechanism for Gap Junction Phosphodegron Control. J Proteome Res. 2012;11:6134–6146. doi: 10.1021/pr300790h. [DOI] [PubMed] [Google Scholar]
- [93].Fykerud TA, Kjenseth A, Schink KO, Sirnes S, Bruun J, Omori Y, Brech A, Rivedal E, Leithe E. Smad ubiquitination regulatory factor-2 controls gap junction intercellular communication by modulating endocytosis and degradation of connexin43. Journal of Cell Science. 2012;125:3966–3976. doi: 10.1242/jcs.093500. [DOI] [PubMed] [Google Scholar]
- [94].Girao H, Catarino S, Pereira P. Eps15 interacts with ubiquitinated Cx43 and mediates its internalization. Experimental cell research. 2009;315:3587–3597. doi: 10.1016/j.yexcr.2009.10.003. [DOI] [PubMed] [Google Scholar]
- [95].Leykauf K, Salek M, Bomke J, Frech M, Lehmann WD, Durst M, Alonso A. Ubiquitin protein ligase Nedd4 binds to connexin43 by a phosphorylation-modulated process. Journal of Cell Science. 2006;119:3634–3642. doi: 10.1242/jcs.03149. [DOI] [PubMed] [Google Scholar]
- [96].Bejarano E, Girao H, Yuste A, Patel B, Marques C, Spray DC, Pereira P, Cuervo AM. Autophagy modulates dynamics of connexins at the plasma membrane in a ubiquitin-dependent manner. Molecular Biology of the Cell. 2012;23:2156–2169. doi: 10.1091/mbc.E11-10-0844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Mollerup S, Hofgaard JP, Braunstein TH, Kjenseth A, Leithe E, Rivedal E, Holstein-Rathlou NH, Nielsen MS. Norepinephrine inhibits intercellular coupling in rat cardiomyocytes by ubiquitination of connexin43 gap junctions. Cell Commun Adhes. 2011;18:57–65. doi: 10.3109/15419061.2011.611920. [DOI] [PubMed] [Google Scholar]
- [98].Ribeiro-Rodrigues TM, Catarino S, Marques C, Ferreira JV, Martins-Marques T, Pereira P, Girao H. AMSH-mediated deubiquitination of Cx43 regulates internalization and degradation of gap junctions. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2014;28:4629–4641. doi: 10.1096/fj.13-248963. [DOI] [PubMed] [Google Scholar]
- [99].Beardslee MA, Lerner DL, Tadros PN, Laing JG, Beyer EC, Yamada KA, Kleber AG, Schuessler RB, Saffitz JE. Dephosphorylation and intracellular redistribution of ventricular connexin43 during electrical uncoupling induced by ischemia. Circulation research. 2000;87:656–662. doi: 10.1161/01.res.87.8.656. [DOI] [PubMed] [Google Scholar]
- [100].Marquez-Rosado L, Solan JL, Dunn CA, Norris RP, Lampe PD. Connexin43 phosphorylation in brain, cardiac, endothelial and epithelial tissues. Biochim Biophys Acta. 2012;1818:1985–1992. doi: 10.1016/j.bbamem.2011.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Majoul IV, Onichtchouk D, Butkevich E, Wenzel D, Chailakhyan LM, Duden R. Limiting transport steps and novel interactions of Connexin-43 along the secretory pathway. Histochemistry and cell biology. 2009;132:263–280. doi: 10.1007/s00418-009-0617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Batra N, Riquelme MA, Burra S, Jiang JX. 14-3-3theta facilitates plasma membrane delivery and function of mechanosensitive connexin 43 hemichannels. J Cell Sci. 2014;127:137–146. doi: 10.1242/jcs.133553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Giepmans BN. Gap junctions and connexin-interacting proteins. Cardiovasc Res. 2004;62:233–245. doi: 10.1016/j.cardiores.2003.12.009. [DOI] [PubMed] [Google Scholar]
- [104].Giepmans BN, Moolenaar WH. The gap junction protein connexin43 interacts with the second PDZ domain of the zona occludens-1 protein. Curr Biol. 1998;8:931–934. doi: 10.1016/s0960-9822(07)00375-2. [DOI] [PubMed] [Google Scholar]
- [105].Laing JG, Chou BC, Steinberg TH. ZO-1 alters the plasma membrane localization and function of Cx43 in osteoblastic cells. J Cell Sci. 2005;118:2167–2176. doi: 10.1242/jcs.02329. [DOI] [PubMed] [Google Scholar]
- [106].Rhett JM, Jourdan J, Gourdie RG. Connexin 43 connexon to gap junction transition is regulated by zonula occludens-1. Mol Biol Cell. 2011;22:1516–1528. doi: 10.1091/mbc.E10-06-0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Hunter AW, Barker RJ, Zhu C, Gourdie RG. Zonula occludens-1 alters connexin43 gap junction size and organization by influencing channel accretion. Mol Biol Cell. 2005;16:5686–5698. doi: 10.1091/mbc.E05-08-0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Hunter AW, Jourdan J, Gourdie RG. Fusion of GFP to the carboxyl terminus of connexin43 increases gap junction size in HeLa cells. Cell Commun Adhes. 2003;10:211–214. doi: 10.1080/cac.10.4-6.211.214. [DOI] [PubMed] [Google Scholar]
- [109].Chen J, Pan L, Wei Z, Zhao Y, Zhang M. Domain-swapped dimerization of ZO-1 PDZ2 generates specific and regulatory connexin43-binding sites. EMBO J. 2008;27:2113–2123. doi: 10.1038/emboj.2008.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Bruce AF, Rothery S, Dupont E, Severs NJ. Gap junction remodelling in human heart failure is associated with increased interaction of connexin43 with ZO-1. Cardiovasc Res. 2008;77:757–765. doi: 10.1093/cvr/cvm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Kieken F, Mutsaers N, Dolmatova E, Virgil K, Wit AL, Kellezi A, Hirst-Jensen BJ, Duffy HS, Sorgen PL. Structural and molecular mechanisms of gap junction remodeling in epicardial border zone myocytes following myocardial infarction. Circulation research. 2009;104:1103–1112. doi: 10.1161/CIRCRESAHA.108.190454. [DOI] [PMC free article] [PubMed] [Google Scholar]