Abstract
Changes in left coronary artery flow pattern in anomalous left coronary from pulmonary artery can provide valuable insight into pathology and natural history of disease. We wish to discuss a case with pre and post operative left coronary flow pattern with mid term follow up.
Keywords: Congenital heart disease, coronary anomalies, left ventricular dysfunction
CASE PRESENTATION
A girl (3-year-old, 11 Kg) presented with poor effort tolerance, easy fatigability, and depressed left ventricular ejection fraction (LVEF) [9% by three-dimensional (3D) echocardiography]. The anomalous left coronary artery (LCA) was arising from the posterior facing sinus of pulmonary artery (ALCAPA). Collaterals feeding the LCA in the interventricular septum could not be appreciated on echocardiography. Basal and mid segments were severely hypokinetic. Apical segments were dyskinetic along with a positive strain and postsystolic shortening. There was significant endomyocardial fibroelastosis and moderate mitral regurgitation.
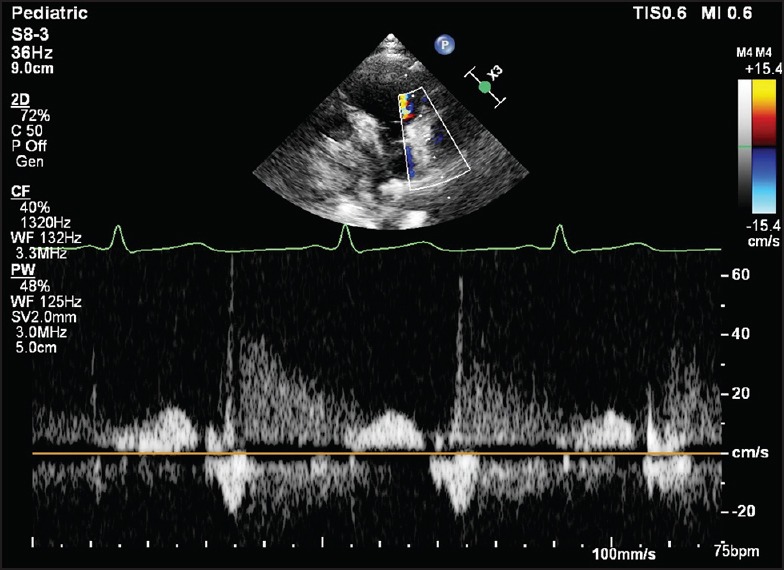
Preoperative pulse wave Doppler (PWD) findings are shown in Figure 1. The wall filter was set at low levels and Nyquist limits were, in addition, set as low as possible for optimal visualization in modified short axis view. In mid left anterior descending (LAD) artery, there was systolic and diastolic flow reversal with brief interruption by forward flow during the early part of diastole. The signal during mid and late diastole was very weak. Due to abnormal orientation, right coronary artery (RCA) flow could not be consistently captured.
Figure 1.
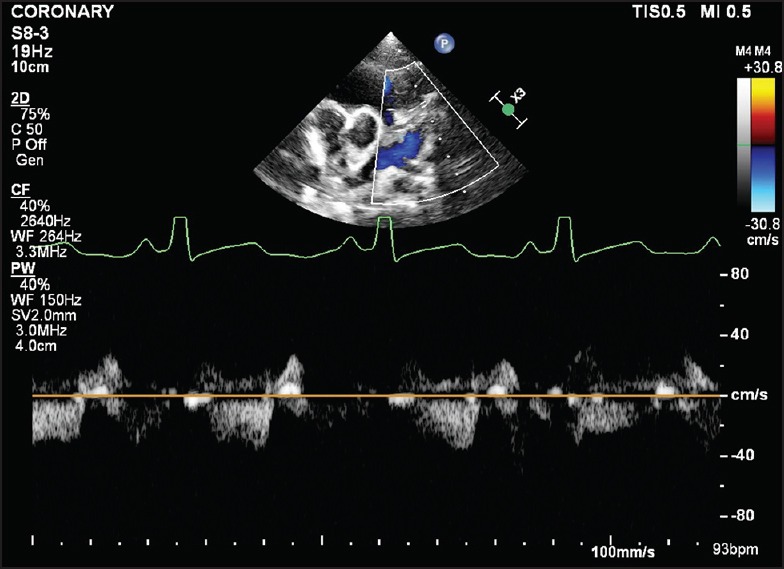
Presurgical pulse wave in Mid-left anterior descending artery
In view of very poor baseline left ventricular function, cardioplegia and aortic cross-clamp was avoided because of concerns of further insult to the already sick myocardium. She underwent left internal mammary artery (LIMA) to LAD (off pump) graft. Site of anastomosis between LIMA and LAD was fashioned close to left main coronary artery (LMCA) bifurcation so as to allow adequate circumflex perfusion. LMCA was ligated close to the pulmonary end. She had an uneventful postoperative recovery.
Early postsurgical PWD findings in the LCA were as follows [Figures 2–4]: There was holodiastolic forward flow that had an early peak and decline. During systole there was flow reversal. The site of anastomosis was evident by flow turbulence noted in proximal LAD and a portion of LAD and left circumflex upstream to the anastomosis was having blue flow while mid/distal LAD was showing red flow (usual color conventions of color Doppler flow assessment).
Figure 2.
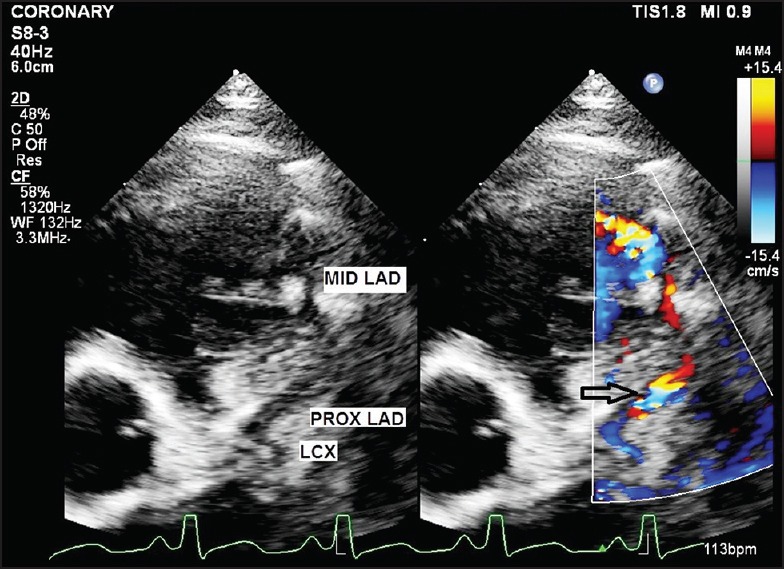
Post LIMA to LAD bypass graft: Color Doppler of LAD and LCX. Turbulence in LAD suggests site of anastomosis (open arrow) (P LAD: Proximal left anterior descending artery, M LAD: Mid-left anterior descending artery, LCX: Left circumflex artery)
Figure 4.
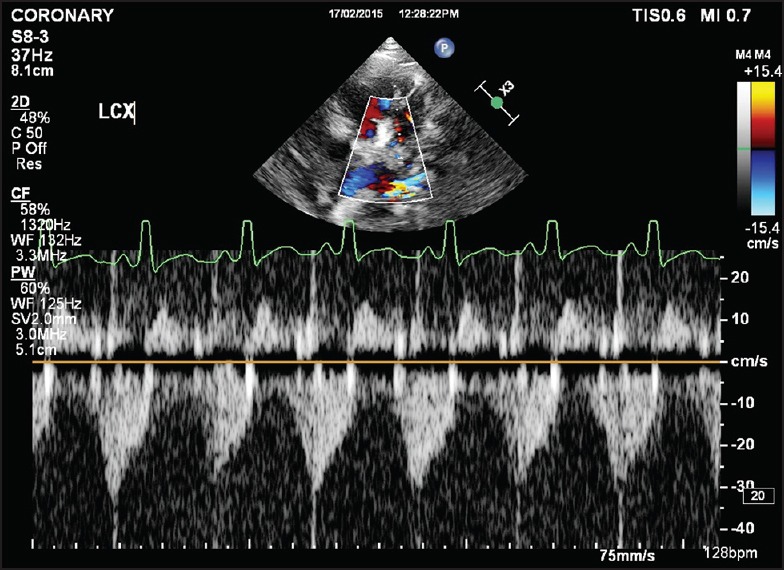
Postoperative Pulse wave of LCX
Figure 3.
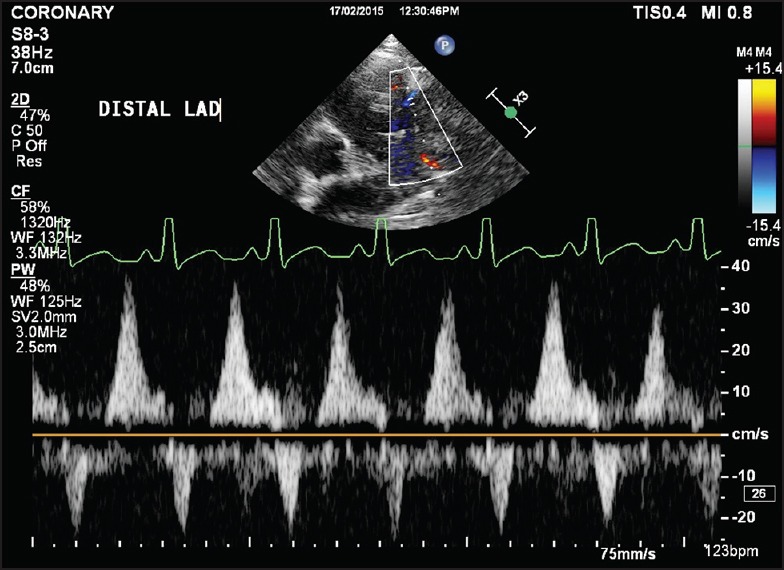
Postoperative Pulse wave of mid LAD
After 6 months, LVEF improved to 30% [Videos 1 and 2]. Basal segments had significant improvement in contractility. The entire apex remained dyskinetic. There was diastolic and systolic forward flow in mid LAD with the former being of a higher velocity [Figure 5].
Figure 5.
Pulse wave of LAD at 6 month follow-up
As a result of ischemia in ALCAPA, there is development of collaterals from the RCA and they feed LAD. The recipient vessel had systolic and diastolic flow reversal. Epicardial collaterals are responsible for systolic flow reversal in the LCA and characteristic higher systolic flow in the RCA. The myocardial collaterals feed the LCA mainly during diastole as they are compressed by contracting myocardium. Long standing ischemia ultimately leads to myocardial infarction and fibrosis. Poor systolic flow reversal may be the result of postinfarction fibrotic obliteration of intramyocardial collaterals. Short early diastolic forward flow may be the result of pulmonary hypertension. Thus, poor diastolic flow reversal in LAD may be an indicator of infarcted myocardium and poor recovery of LVEF after surgery. However, the survival with preserved LV function of a selected few patients well into adulthood remains unexplained.[1,2,3,4,5,6]
Videos available on www.annalspc.com
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yau JM, Singh R, Halpern EJ, Fischman D. Anomalous origin of the left coronary artery from the pulmonary artery in adults: A comprehensive review of 151 adult cases and a new diagnosis in a 53-year-old woman. Clin Cardiol. 2011;34:204–10. doi: 10.1002/clc.20848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrindle BW, Li JS, Minich LL, Colan SD, Atz AM, Takahashi M, et al. Pediatric Heart Network Investigators. Coronary artery involvement in children with Kawasaki disease: Risk factors from analysis of serial normalized measurements. Circulation. 2007;116:174–9. doi: 10.1161/CIRCULATIONAHA.107.690875. [DOI] [PubMed] [Google Scholar]
- 3.Tian Z, Fang LG, Liu YT, Zhang SY. Anomalous origin of the left coronary artery from the pulmonary artery detected by echocardiography in an asymptomatic adult. Intern Med. 2013;52:233–6. doi: 10.2169/internalmedicine.52.7643. [DOI] [PubMed] [Google Scholar]
- 4.Drinkovic N, Margetic E, Smalcelj A, Brida V. Echocardiographic diagnosis of anomalous origin of the left coronary artery from the pulmonary artery. Eur J Echocardiogr. 2008;9:309–10. doi: 10.1016/j.euje.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Varghese M, Kothari S. The caveats in the diagnosis of anomalous origin of left coronary artery from pulmonary artery (ALCAPA) Images Paediatr Cardiol. 2010;12:3–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Lange R, Vogt M, Hörer J, Cleuziou J, Menzel A, Holper K, et al. Long-term results of repair of anomalous origin of the left coronary artery from the pulmonary artery. Ann Thorac Surg. 2007;83:1463–71. doi: 10.1016/j.athoracsur.2006.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


