Abstract
Objective
To measure the quality of life and clinical–functional results from patients diagnosed with osteoarthrosis of the distal radioulnar joint who underwent surgical treatment using the technique of total arthroplasty of the ulna, with a total or partial Ascension® prosthesis of the distal ulna.
Methods
Ten patients were evaluated after 12 months of follow-up subsequent to total or partial arthroplasty of the distal ulna. All of them presented post-traumatic osteoarthrosis and/or chronic symptomatic instability of the distal radioulnar joint. The study was prospective. Seven patients had previously undergone wrist procedures (two cases with Darrach, three with Sauvé–Kapandji and two with ligament reconstruction of the fibrocartilage complex) and three presented fractures of the distal ulna that evolved with pain, instability and osteoarthrosis of the distal radioulnar joint. The following were assessed: quality of life (DASH scale); percentage degree of palm grip strength (kgf) and pronosupination range of motion in relation to the unaffected side; pain (VAS); return to work; subjective evaluation of radiography; and complications.
Results
The patients presented a mean range of motion of 174.5° (normal side: 180°). Quality of life was analyzed by applying the DASH questionnaire and the mean value found was 5.9. The mean pain score using the VAS was 2.3. The mean degree of palm grip strength (kgf) was 50.7, which represented 90.7% of the strength on the unaffected side. The complication rate was 10%: this patient presented slight dorsal instability of the ulna and persistent pain, and did not return to work. This patient is still being followed up in the outpatient clinic and occupational therapy sector, with little improvement. He does not wish to undergo a new procedure. The mean length of follow-up was 16.8 months, with a minimum of 10 and maximum of 36 months.
Conclusion
This concept is subject to the test of time. Implantation of a prosthesis is a very interesting addition to the surgical arsenal for those who are specialists in hand surgery. Arthroplasty of the distal ulna is a safe and effective method with clinical–functional and quality-of-life improvements for patients and presents a low complication rate.
Keywords: Arthroplasty, Fractures of the radius, Fractures of the ulna, Joint prosthesis
Resumo
Objetivo
Mensurar a qualidade de vida e os resultados clínico-funcionais dos pacientes com diagnóstico de osteoartrose da radioulnar distal submetidos ao tratamento cirúrgico pela técnica de artroplastia total da ulna com a prótese total ou parcial Ascension® da ulna distal.
Métodos
Foram avaliados 10 pacientes com 12 meses de seguimento de artroplastia total ou parcial de ulna distal. Todos apresentavam osteoartrose pós-traumática e ou instabilidade crônica e sintomática da articulação radioulnar distal. O estudo foi prospectivo. Sete pacientes tinham procedimentos prévios no punho (2-darrach, 3-Sauvé-kapandji, 2-reconstruções ligamentares do complexo da fibrocartilagem) e três apresentaram fraturas da ulna distal que evoluíram com dor, instabilidade e osteoartrose da radioulnar distal. Foram analisados a qualidade de vida (DASH), a porcentagem do grau de força de preensão palmar (kgf) e o arco de movimento de pronossupinação em relação ao lado não afetado, a dor (VAS), o retorno ao trabalho e a avaliação subjetiva da radiografia e das complicações.
Resultados
Os pacientes apresentaram, em média, o arco de movimento de 174,5° e o lado normal 180°. A qualidade de vida foi analisada pela aplicação do questionário DASH e o valor médio encontrado foi 5,9. A avaliação da dor, com o uso da escala VAS, foi de 2,3, em média. O grau de força de preensão palmar (kgf) foi de 50,7, em média, o que representa 90,7% da força do lado não acometido. A taxa de complicações foi de 10%. Esse paciente apresentou discreta instabilidade dorsal da ulna, dor persistente e não retornou ao trabalho. Esse paciente segue no ambulatório e no setor de terapia ocupacional, com pouca melhoria. Não deseja fazer novo procedimento. O tempo de seguimento, em média, foi de 16,8 meses, com mínimo de 10 e máximo de 36 meses.
Conclusão
Esse conceito está a teste do tempo. A implantação de uma prótese é uma adição muito interessante ao arsenal cirúrgico para aqueles que são especializados em cirurgia da mão. A artroplastia de ulna distal é um método seguro, eficaz, com melhoria clínico-funcional e da qualidade de vida dos pacientes e apresenta baixo índice de complicações.
Palavras-chave: Artroplastia, Fraturas do rádio, Fraturas da ulna, Prótese articular
Introduction
Fractures of the distal portions of the radius and ulna, ligament injuries of the triangular fibrocartilage complex, Essex-Lopresti fractures and degenerative osteoarthrosis due to rheumatoid arthritis are the main primary causes of disarray of the distal radioulnar joint. The integrity of this joint is the critical point for maintaining the stability and functionality of the upper arm and forearm. Chronic instability and osteoarthrosis lead to pain and diminished capacity for pronation–supination, grip strength and activities of daily living.1
Several surgical salvage methods for addressing complications of this joint (osteoarthrosis and/or chronic instability) are known,2 and these include the Sauvé and Kapandji,3 Darrach4 and Bowers5 procedures. The limitations of these methods include instability of the distal radioulnar joint, impact of the ulna on the radius and, consequently, residual pain in this wrist.
In seeking integrity of the distal radioulnar joint, with mechanical fulfillment of the relationship between the bones of the forearm along its entire extent, and reinsertion of the main ligament stabilizers of this joint, which enables pronation–supination and load transmission by the ulnar column of the wrist,6, 7, 8, 9, 10 prostheses for the distal ulna have been developed.2
However, this technique is not popular in our setting and no articles describing it exist in the Brazilian literature. For these reasons, we decided to conduct the present study, in which arthroplasty of the distal ulna was used to treat complications of the distal radioulnar joint.
The objective was to measure the quality of life and clinical–functional results of patients with a diagnosis of osteoarthrosis of the distal radioulnar joint who underwent surgical treatment by means of the technique of total ulna arthroplasty using the Ascension® total or partial prosthesis of the ulnar head.
Materials and methods
Between January 2012 and July 2014, 10 patients were attended at the outpatient clinic of the hand sector of our institution (Table 1). All of them had a diagnosis of post-traumatic osteoarthrosis and/or instability of the distal radioulnar joint. They were included in the study and underwent physical examination and simple radiography in posteroanterior (PA), lateral and Lees and Schecker views,11 in order to evaluate the impact of the ulna on the radius in patients who had previously undergone Darrach and Sauvé–Kapandji procedures, and also underwent magnetic resonance imaging of the wrist in T1 and T2 weightings.
Table 1.
Clinical–epidemiological features.
| Identification | Age | Follow-up (months) | Return to work | Complications | Motive |
|---|---|---|---|---|---|
| I | 26 | 36 | Before 6th month | No | Complex fracture |
| II | 59 | 24 | Before 12th month | No | Post-Sauvé–Kapandji impact |
| III | 41 | 12 | No | Yes. Pain and instability | Ligament injury |
| IV | 60 | 10 | Before 6th month | No | Post-Darrach impact |
| V | 64 | 12 | Before 12th month | No | Complex fracture |
| VI | 60 | 14 | Before 12th month | No | Post-Darrach impact |
| VII | 56 | 18 | Before 6th month | No | Post-Sauvé–Kapandji impact |
| VIII | 48 | 15 | Before 12th month | No | Post-Sauvé–Kapandji impact |
| IX | 55 | 13 | Before 12th month | No | Ligament injury |
| X | 34 | 14 | Before 12th month | No | Complex fracture |
Source: Hospital service files.
The inclusion criteria that were established were that the patients needed to be adults between 18 and 65 years of age, of both sexes, with clinical and imaging diagnoses, and that they needed to have filled out a statement of free and informed voluntary consent and a conflict-of-interest protocol, as required by the research ethics committee (CAAE – 12759113.7.0000.0082).
Patients were excluded if they presented distal radioulnar instability without osteoarthrosis or if they abandoned the treatment at any stage.
The functional evaluation was performed by professionals in the hand occupational therapy sector.
The clinical–functional measurements consisted of measuring the range of motion (ROM) of wrist pronation–supination in degrees, using a single specific goniometer. The clinical analysis on pain was performed using a visual analog scale (VAS) from one to ten, for subjective assessment.
The quality-of-life assessment was made using the DASH questionnaire, which is an instrument validated for the upper limbs, and also according to whether the patient returned to work (or not).
The postoperative radiographic evaluation on the wrist was performed serially, at outpatient consultations, in order to check on the positioning of the prosthesis. The complication rate was analyzed throughout the follow-up.
The distal ulna prostheses used were the First Choice Ascension® (partial cases) and the Modular Ulnar Head (MUH) Ascension® (total cases). Both of these are modular endoprosthesis that consist of a head of hemispherical shape (total or partial), made of chromium–cobalt, which is connected by means of a neck, also made of chromium–cobalt, with specific orifices in its distal component. This fits into the proximal portion, which is an intramedullary nail covered with pure titanium, in a press-fit system, which is accommodated in the diaphysis of the ulna. Several sizes or head, neck and nail are available, and these can be combined according to the size of the patient's ulna. The head has orifices to enable passage of suturing thread from the triangular fibrocartilage complex.
Description of the surgical technique
-
1.
Usual orthopedic preparation for the patient, in the supine position.
-
2.
The access route is dorsal and arc-shaped in the wrist, under the distal radioulnar joint, outlining the ulnar head, of length approximately 7 cm.
-
3.
All layers are dissected, under the V extensor tunnel.
-
4.
The dorsal capsule is opened and arthrotomy of the distal radioulnar joint is performed.
-
5.
Replacement arthroplasty is performed, with removal of the ulnar head (partially or totally), using a specific microsaw.
-
6.
The distal and proximal components are placed after measurement using specific guides and milling cutters, with the aid of radioscopy.
-
7.
Reinsertion of the triangular fibrocartilage complex in the distal prosthesis.
-
8.
Revision of hemostasis, local cleaning and suturing in layers, including the dorsal capsule and the sheath of the ulnar extensor of the carpus, under the prosthesis.
-
9.
Suturing of the retinaculum of the extensors, subcutaneous cellular tissue and skin.
-
10.
Release of the tourniquet and preparation of dressings.
After the procedure, the patients were kept immobilized by means of a plaster-cast splint from the axilla to the palm, for up to six weeks. Subsequently, the patient underwent rehabilitation in the occupational sector of this institution, using a preestablished specific protocol.
Results
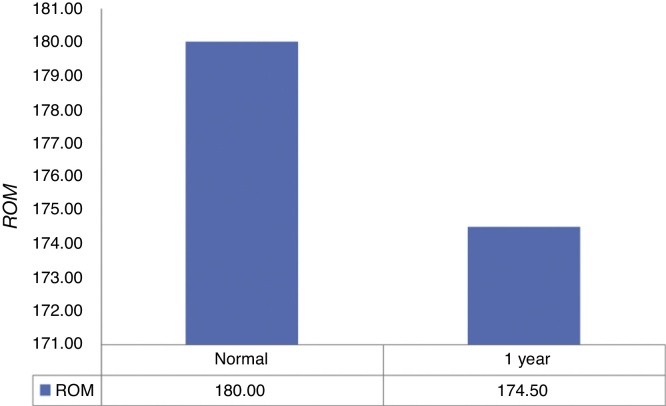
The patients presented a mean range of motion of 174.5°, while the normal side was 180° (Fig. 1).
Fig. 1.
Comparison of the range-of-motion (ROM) variable from before to after the operation.
Quality of life was analyzed by applying the DASH questionnaire, which ranges from 1 to 100, and the mean value found was 5.9.
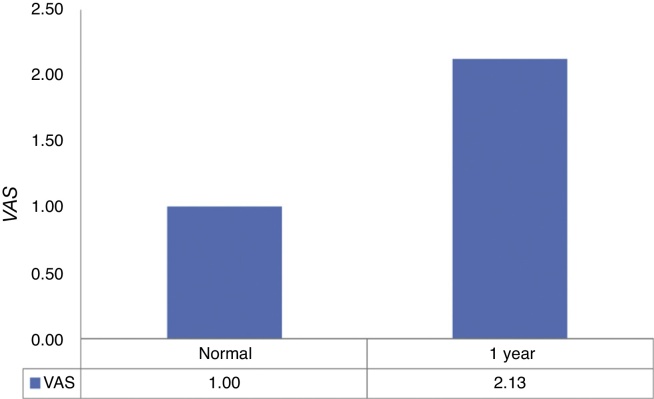
The pain evaluation using the VAS (Fig. 2) showed a mean value of 2.3.
Fig. 2.
Comparison of the visual analog scale (VAS) variable from before to after the operation.
The mean palmar grip strength (kgf) was 50.7. This represented 90.7% of the strength of the unaffected side.
The complication rate was 10%. This patient presented slight dorsal instability of the ulna and persistent pain, and did not return to work. This patient continues to attend the outpatient clinic and occupational therapy sector, with little improvement. He does not wish to undergo another procedure (Fig. 3, Fig. 4, Fig. 5).
Fig. 3.
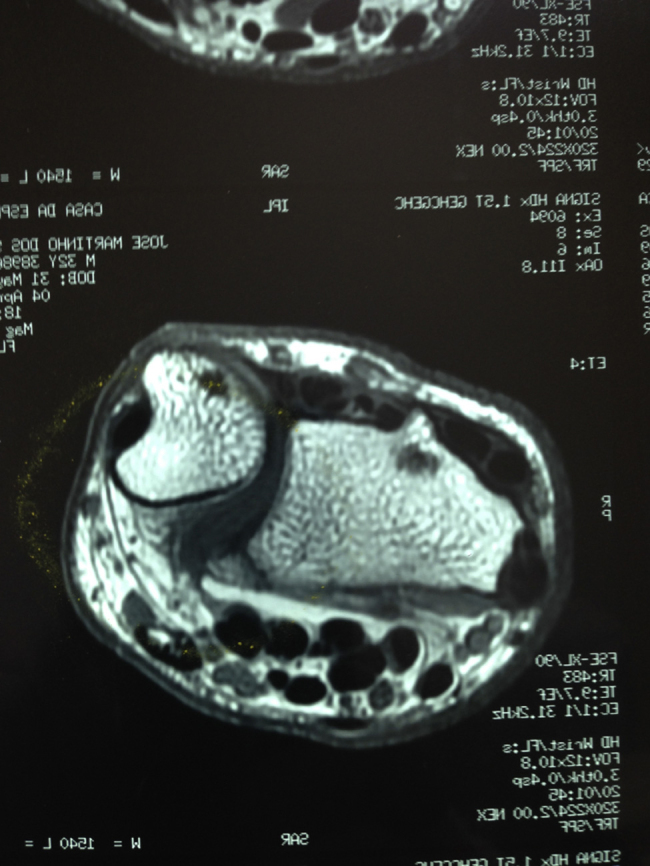
Magnetic resonance imaging of patient III, in axial slice showing joint incongruence of the distal radioulnar joint even after ligament reconstruction.
Fig. 4.

Radiographic appearance of the wrist in lateral view, six months after the operation, showing dorsal subluxation of the prosthesis of the distal ulna (patient III).
Fig. 5.

Radiographic appearance of the wrist in anteroposterior view, six months after the operation, showing the prosthesis of the distal ulna aligned and without signs of loosening or remodeling (patient III).
The mean length of follow-up was 16.8 months, with a minimum of 10 and maximum of 36 months.
Statistical analysis
For the statistical analyses, we used the significance level of 5% (0.050) for applying the statistical tests. In other words, when the calculated significance value (p) was less than 5% (0.050), there would be a statistically significant difference (in the case of comparisons) or a statistically significant relationship (in the case of relationships), i.e. an “effective difference” in the case of comparisons or a “strong relationship” in the case of relationships, respectively. When the calculated significance value (p) was greater than or equal to 5% (0.050), there would be a statistically non-significant difference (in the case of comparisons) or a statistically non-significant relationship (in the case of relationships), i.e. a “similarity” in the case of comparisons or a “weak relationship” in the case of relationships, respectively. We used the Microsoft Excel electronic spreadsheet (MS-Office 2010 version) to organize the data and the IBM SPSS software (Statistical Package for the Social Sciences), version 22.0, in order to obtain the results.
The Wilcoxon signed-rank test was applied with the aim of investigating possible differences between the two observation times (Table 2), for each variable of interest.
Table 2.
Comparison of the variables of interest between the pre and postoperative times of observation.
| Pair of variables | n | Mean | Standard deviation | Minimum | Maximum | 25th percentile | 50th percentile (median) | 75th percentile | Significance (p) |
|---|---|---|---|---|---|---|---|---|---|
| Normal ROM | 10 | 180.00 | 0.00 | 180.00 | 180.00 | 180.00 | 180.00 | 180.00 | 0.068 |
| ROM after 1 year | 10 | 174.50 | 7.15 | 160.00 | 180.00 | 170.50 | 177.00 | 180.00 | |
| Normal DASH | 10 | 1.00 | 0.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.068 |
| DASH after 1 year | 10 | 5.9 | 14.32 | 1.00 | 35 | 30.00 | 33.00 | 40.50 | |
| Normal VAS | 10 | 1.00 | 0.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.066 |
| VAS after 1 year | 10 | 2.13 | 1.46 | 1.00 | 5.00 | 1.00 | 1.50 | 3.00 | |
| Normal strength | 10 | 56.1 | 5.28 | 1.9 | 10.1 | 1.9 | 5.5 | 5.9 | |
| Strength after 1 year | 10 | 50.7 | 5.44 | 1.7 | 10.7 | 2.7 | 5.3 | 8.0 | 0.058 |
Source: Hospital service files.
There were similar results for all the variables analyzed, thus showing that the operated side was similar to the normal side.
Discussion
There is no unanimity regarding the procedure of arthroplasty of the distal ulna in our setting and no Brazilian articles have yet been published. However, in seeking stabilization of the distal radioulnar joint, especially after salvage procedures2, 3, 4, 5 that improve pronation–supination but lead to the ulna impacting on the radius in a symptomatic manner1 while still maintaining radioulnar joint instability, we applied a distal ulna prosthesis in order to attempt to resolve these complications.
Biomechanical studies have presented statistically significant evidence showing that the prosthesis favors stability, diminishes impaction on the radius and recovers pronation–supination, in comparison with other salvage techniques cited above.8, 12
In comparing the results from our study with those from other case series in which the Sauvé and Kapandji procedure apud Carter and Stuart13 was applied to disorders of the distal radioulnar joint, we observed that there was better recovery of range of motion (174.5° versus 172°) and a lower complication rate (10% versus 33.5%) in our present series.
Van Schoonhoven et al.14 published a multicenter study with long-term results (41 months of follow-up) from 23 patients who were treated using the Herbert UHP® prosthesis. All the patients presented stable distal radioulnar joints, none of the patients was reoperated and the VAS pain measurement was 2.2. The pronation–supination range of motion was 175° and the palmar grip strength recovered to 81% in relation to the unaffected side. All the patients presented bone absorption in the most proximal region of the nail (stress shielding) and remodeling of the sigmoid fossa of the radius. There was no loosening or fracturing of the implants, and these radiographic findings did not show any clinical symptoms. Our study presented one case of instability and residual pain in the distal radioulnar joint, with strength recovery of 90%, VAS of 2.3 and range of motion of 174.5°. We also did not observe any radiographic alterations in our patients. Our results were similar to those of the above study, even with a shorter follow-up (16.8 months versus 41 months).
In comparing studies that used different total prostheses in 2009, Yen Shipley et al.15 presented a series of 22 wrists in 20 patients (14 UHPs® and 7 uHeads®) with a follow-up of 53.4 months. Ten patients presented excellent and good results after treatment for osteoarthrosis consisting of a primary prosthesis, without any previous procedure. Among the other 12 patients who had undergone other treatments prior to the prosthesis, 75% of the results were good or excellent. Their complication rate was 13% (three patients): two patients evolved with dorsal subluxation and were subsequently treated by means of ligament reconstruction; and one patient presented post-traumatic fracturing of the ulnar diaphysis. These three patients also evolved with good or excellent results. Our complication rate was 10%, comprising one patient with instability and dorsal subluxation of the prosthesis that remains unresolved.
We had a single patient with a partial prosthesis (II), who presented osteoarthrosis only of the radial ulna, after chronic ligament injury of the triangular fibrocartilage complex. Twenty-four months after arthroplasty, range of motion of 180° was obtained, with VAS and DASH of 1 and recovery of 96% of the palmar grip strength. Garcia-Elias16 conducted a study on three patients with 11 months of follow-up, in which an Eclypse® partial prosthesis made of pyrocarbon was used. So far, these patients remain free from pain: they can lift 4 kg weight with their wrist and do not present any instability of the distal radioulnar joint.
Another series published by Fernandez et al.17 presented 10 patients with a follow-up of 2.6 years. All of them were treated using a spherical prosthesis proximal to the ulnar head and sigmoid fossa of the radius. All the patients presented failure of the Sauvé–Kapandji procedure and this prosthesis was placed at the pseudarthrosis of the ulna, without removing its head, and was connected to the region just below the sigmoid fossa of the radius and, superiorly, to the most proximal part of the ulnar head. All the patients’ pain and impaction of the ulna on the radius improved, and their degree of palmar grip strength recovered from 27% before the surgery to 55% after the surgery, in relation to the unaffected side. The range of motion recovered totally in seven patients, partially in two and not at all in one. 90% of the patients returned to work. The complication rate was 10%, and this patient continued to present pain and did not recover his pronation–supination movement. None of the patients presented instability of the prosthesis. In our setting, use of the Sauvé–Kapandji technique is very common and complication rates of 13–39% have been reported in the literature. This prosthesis is well indicated in such cases: it is stable and does not alter the relationship between the ulnar and the carpus.
Savvidou et al.18 showed long-term results (five years of follow-up) from 35 patients who underwent total arthroplasty of the distal radius using the Aptis DRUJ® semi-constricted prosthesis. This prosthesis is indicated for treatment of cases of failure of primary arthroplasty, and for pathological conditions that affect the ligament stabilization system of the distal radioulnar joint distal, such as congenital, traumatic, degenerative and autoimmune pathological conditions. It presents not only proximal and distal ulnar components but also a radial component that covers the sigmoid fossa. This functions as a bipolar prosthesis and is used in pathological conditions of the hip. Most of those authors’ patients presented a functional range of motion for pronation–supination, recovered their palmar grip strength and were able to do their activities of daily living (ADLs) in a satisfactory manner, without pain. Twelve patients presented complications before the surgery. Among these, there were cases of tendinopathy and insufficiency of the ulnar extensor of the carpus, heterotopic ossification, bone reabsorption with loosening of the primary prosthesis and infection. The total Aptis DRUJ® prosthesis was shown to be a safe option that promoted improvement of pronation–supination, palmar grip strength and return to activities of daily living. That study showed solutions for failure of primary arthroplasty of the distal ulna.
Conclusion
This concept is subject to the test of time. Implantation of a prosthesis is a very interesting addition to the surgical arsenal for those who are specialists in hand surgery. Arthroplasty of the distal ulna is a safe and effective method with clinical–functional and quality-of-life improvements for patients and presents a low complication rate.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed in the Hand Sector, Department of Orthopedics and Traumatology, Faculdade de Medicina do ABC (FMABC), Santo André, SP, Brazil.
References
- 1.Willis A.A., Berger R.A., Cooney W.P., 3rd Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg Am. 2007;32(2):177–189. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Gordon K.D., Dunning C.E., Johnson J.A., King G.J. Kinematics of ulnar head arthroplasty. J Hand Surg Br. 2003;28(6):551–558. doi: 10.1016/s0266-7681(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 3.Sauve L., Kapandji M. Nouvelle technique de traitement chirurgical des luxations récidivantes isoleés de l’extremité inferičure du cubitus. J Chir. 1936;47:589. [Google Scholar]
- 4.Darrach W. Anterior dislocation of the head of the ulna. Ann Surg. 1912;56:802–803. [Google Scholar]
- 5.Bowers W.H. Distal radioulnar joint arthroplasty. Current concepts. Clin Orthop Relat Res. 1992;275:104–109. [PubMed] [Google Scholar]
- 6.Rotsaert P., Cermak K., Vancabeke M. Case report: revision of failed Sauvé–Kapandji procedure with an ulnar head prosthesis. Chir Main. 2008;27(1):47–49. doi: 10.1016/j.main.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 7.De Smet L., Peeters T. Salvage of failed Sauvé–Kapandji procedure with an ulnar head prosthesis: report of three cases. J Hand Surg Br. 2003;28(3):271–273. doi: 10.1016/s0266-7681(02)00309-1. [DOI] [PubMed] [Google Scholar]
- 8.Palmer A.K., Werner F.W. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26–35. [PubMed] [Google Scholar]
- 9.Sauerbier M., Fujita M., Hahn M.E., Neale P.G., Berger R.A. The dynamic radioulnar convergence of the Darrach procedure and the ulnar head hemiresection interposition arthroplasty: a biomechanical study. J Hand Surg Br. 2002;27(4):307–316. doi: 10.1054/jhsb.2002.0763. [DOI] [PubMed] [Google Scholar]
- 10.Masaoka S., Longsworth S.H., Werner F.W., Short W.H., Green J.K. Biomechanical analysis of two ulnar head prostheses. J Hand Surg Am. 2002;27(5):845–853. doi: 10.1053/jhsu.2002.34010. [DOI] [PubMed] [Google Scholar]
- 11.Lees V.C., Scheker L.R. The radiological demonstration of dynamic ulnar impingement. J Hand Surg Br. 1997;22:448–450. [Google Scholar]
- 12.Sauerbier M., Arsalan-Werner A., Enderle E., Vetter M., Vonier D. Ulnar head replacement and related biomechanics. J Wrist Surg. 2013;2(1):27–32. doi: 10.1055/s-0032-1333464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter P.B., Stuart P.R. The Sauve–Kapandji procedure for post-traumatic disorders of the distal radio-ulnar joint. J Bone Joint Surg Br. 2000;82(7):1013–1018. doi: 10.1302/0301-620x.82b7.10674. [DOI] [PubMed] [Google Scholar]
- 14.van Schoonhoven J., Mühldorfer-Fodor M., Fernandez D.L., Herbert T.J. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. J Hand Surg Am. 2012;37(7):1372–1380. doi: 10.1016/j.jhsa.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 15.Yen Shipley N., Dion G.R., Bowers W.H. Ulnar head implant arthroplasty: an intermediate term review of one surgeon's experience. Tech Hand Up Extrem Surg. 2009;13(3):160–164. doi: 10.1097/BTH.0b013e3181b4c52d. [DOI] [PubMed] [Google Scholar]
- 16.Garcia-Elias M. Eclypse: partial ulnar head replacement for the isolated distal radio-ulnar joint arthrosis. Tech Hand Up Extrem Surg. 2007;11(1):121–128. doi: 10.1097/bth.0b013e31803261e2. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez D.L., Joneschild E.S., Abella D.M. Treatment of failed Sauvé–Kapandji procedures with a spherical ulnar head prosthesis. Clin Orthop Relat Res. 2006;445:100–107. doi: 10.1097/01.blo.0000205901.13609.70. [DOI] [PubMed] [Google Scholar]
- 18.Savvidou C., Murphy E., Mailhot E., Jacob S., Scheker L.R. Semiconstrained distal radioulnar joint prosthesis. J Wrist Surg. 2013;2(1):41–48. doi: 10.1055/s-0032-1333466. [DOI] [PMC free article] [PubMed] [Google Scholar]