Abstract
Objective
To analyze the radiographic positioning of the femoral tunnel and correlate this with the postoperative clinical results among patients undergoing reconstruction of the medial patellofemoral ligament (MPFL) alone.
Method
This was a retrospective study in which 30 knees of 26 patients with recurrent dislocation of the patella that underwent MPFL reconstruction were evaluated. The femoral insertion point of the graft and the postoperative clinical condition were analyzed and correlated using the Kujala and Lysholm scales.
Results
22 knees presented a femoral tunnel in the anatomical area (group A) and 8 outside of this location (group B). In group A, the mean score on the Kujala scale was 89.68 points and on the Lysholm scale was 92.45 points. In group B, the mean score on the Kujala scale was 84.75 points and on the Lysholm scale was 92 points. The difference between the means was not significant on either of the two scales.
Conclusion
Correlation with the clinical results did not show any difference in relation to the positioning of the femoral insertion of the graft.
Keywords: Patellar dislocation, Patellar ligament, Reconstruction
Resumo
Objetivo
Analisar o posicionamento radiográfico do túnel femoral e correlacioná-lo com os resultados clínicos no pós-operatório em pacientes submetidos à reconstrução isolada do ligamento patelofemoral medial (LPFM).
Método
Estudo retrospectivo, em que foram avaliados 30 joelhos de 26 pacientes com quadro de luxação recidivante da patela submetidos à reconstrução do LPFM, analisados e correlacionados o ponto de inserção femoral do enxerto e o quadro clínico pós-operatório pelas escalas de Kujala e Lysholm.
Resultados
Apresentaram túnel femoral na área anatômica (grupo A) 22 joelhos e oito fora desse local (grupo B). No grupo A, a pontuação média pela escala de Kujala foi de 89,68 e pela de Lysholm foi de 92,45. No grupo B, a pontuação média pela escala de Kujala foi de 84,75 e pela de Lysholm foi de 92. A diferença entre as médias não foi significativa nas duas escalas.
Conclusão
Não houve diferença de resultados clínicos correlacionados ao posicionamento da inserção femoral do enxerto.
Palavras-chave: Luxação patelar, Ligamento patelar, Reconstrução
Introduction
The medial patellofemoral ligament (MPFL) is a strip of retinacular tissue that connects the medial epicondyle of the femur to the medial border of the patella. Several studies have shown that the MPFL is the primary restrictor of lateral patellar displacement and the main agent responsible for avoiding patellar dislocation, thus contributing 50–80% of the medial containment.1, 2 According to Amis et al.,3 the MPFL has mean tensile strength of 208 N, although, as demonstrated by Mountney et al.,4 its limited capacity for stretching results in total rupture in cases of complete patellar dislocation.
In cases of recurrent dislocation of the patella, surgical treatment is indicated, given that anatomical reconstruction of the MPFL is essential for restoration of patellar stability.3, 5, 6, 7 Thus, several techniques for MPFL reconstruction have been developed, mostly with replacement of the torn ligament by a tendon graft.8, 9, 10
Several studies have identified the location of the MPFL3, 11, 12 and it is believed that anatomical restoration is essential for reproducing the normal isometry and function of the ligament.13, 14 Bone and radiographic parameters may help the surgeon to adequately verify the positioning of the reconstructed ligament.
The femoral isometric point makes the greatest contribution towards the isometry of the MPFL and is the most important factor for success of the surgery. However, its reproduction is more difficult and more subject to failure.3, 15
Nonetheless, there are few reports correlating the positioning of the femoral tunnel and the clinical condition after the reconstruction. Through a retrospective study on patients who underwent MPFL reconstruction, we aimed to analyze the positioning of the femoral tunnel, by means of radiographs, and to correlate this with the clinical results and functional scores.
Sample and method
Between January 2008 and February 2013, MPFL reconstruction was performed on 30 knees in 26 patients (9 men and 17 women) presenting a condition of recurrent dislocation of the patella. The patients’ mean age at the time of the surgery was 25.8 years, with a range from 16 to 46 years. The right knee was affected in 13 cases, while the left knee was affected in 17. The minimum follow-up was seven months and the maximum was 62 months, with a mean of 24.3 months. A correlation was made between the femoral insertion point of the graft (assessed by means of simple radiography of the knee) and the postoperative clinical condition (assessed by means of the Kujala and Lysholm scales.
The inclusion criterion was that the patients selected needed to present objective patellofemoral instability. Patients with an open growth plate, patellofemoral arthrosis or alterations of the anterior tibial tuberosity-trochlear groove (ATT-TG) distance or patellar height that required additional procedures for distal patellar realignment were excluded from the study. Patients with associated lesions on the operated limb that might directly or indirectly influence the final result were also excluded.
Three surgeons (LFBPJ, MHFC and OPN) performed the reconstructions using grafts from the semitendinosus tendon. A transverse tunnel was constructed in the upper-middle third of the patella. The femoral tunnel location was determined by means of palpation of the anatomical marks between the tubercle of the adductors and the medial epicondyle (Nomura point)15 or by means of fluoroscopy, at the intersection of a line tangential to the medial condyle and its perpendicular at the projection of the posterior cortical bone, i.e. the method of Schöttle et al.,16 according to the surgeon's preference. The graft was fixed in the femoral tunnel using a rhombus metal screw or absorbable interference screw, with the knee flexed at 30–45 degrees.
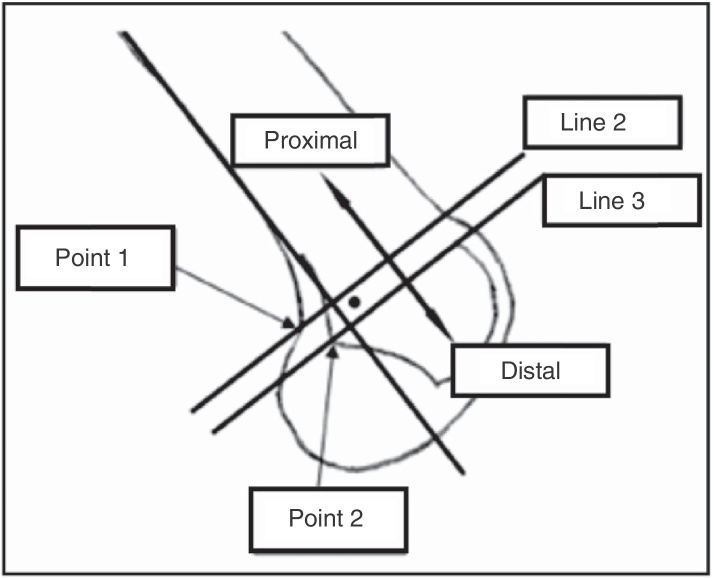
Radiographs of the patella were produced in anteroposterior (AP), lateral and axial views before the operation and at the end of the follow-up. The radiographic method used for evaluating the positioning of the femoral tunnel was the one described in the sagittal plane by Schöttle et al.16 A point 1 mm anterior to the posterior femoral cortical bone, 2.5 mm distal to the origin of the medial femoral condyle and proximal to the Blumensat line was determined as the femoral insertion of the MPFL (Fig. 1). An area of 5 mm in diameter was described. Two groups of patients (A and B) were defined, with their tunnels respectively inside and outside this predetermined anatomical area, according to the radiographic point of the femoral insertion of the graft.
Fig. 1.
Femoral positioning using the method of Schöttle.
In the statistical analysis, to compare the means of the scores obtained by the above groups, the Wilcoxon nonparametric test was used, since this would not need the assumption of normality of the score measurements. Differences between the means were considered to be significant if the p-values obtained were less than 0.05. The analyses were performed in the R free software, version 3.0.1.
This study was approved by our institution's research ethics committee under the number CAAE 19486313.6.0000.5128.
Results
Group A comprised 20 patients and 22 knees. The mean score obtained using the Kujala scale was 89.6 points, with a range from 64 to 100. According to the Lysholm scale, the mean score was 92.4 points, with a range from 77 to 100, which translated as 11 excellent, 8 good and 3 fair results. None of the results were considered poor.
Group B comprised 8 patients and 8 knees. The mean score reached on the Kujala scale was 84.7 points, with a range from 57 to 98. According to the Lysholm scale, the mean score was 92 points, with a range from 76 to 100, which translated as 4 excellent, 3 good and 1 fair result. Just as in group A, none of the results were considered to be poor. The main graft fixation errors were anterior positioning in 37.5% of the cases and superior positioning in 62.5% of the cases.
Table 1 shows the descriptive statistics and p-values of comparison tests on the mean scores obtained via the Lysholm scale for groups A and B. The mean for group A was 92.45 (standard deviation = 6.58). The mean for group B was 92 (standard deviation = 8.80). The difference between the means was not significant (p = 0.8967).
Table 1.
Descriptive statistics on the scores obtained via the Lysholm scale.
| Participants | Statistics |
p-Value | ||||
|---|---|---|---|---|---|---|
| n | Minimum | Maximum | Mean | Standard deviation | ||
| Group A | 22 | 77 | 100 | 92.45 | 6.58 | 0.8967 |
| Group B | 8 | 76 | 100 | 92.00 | 8.80 | |
Table 2 presents the descriptive statistics and p-values of comparison tests on the mean scores obtained via the Kujala scale for groups A and B. The mean for group A was 89.68 (standard deviation = 9.87). The mean for group B was 84.75 (standard deviation = 14.27). The difference between the means was not significant (p = 0.4109).
Table 2.
Descriptive statistics on the scores obtained via the Kujala scale.
| Participants | Statistics |
p-Value | ||||
|---|---|---|---|---|---|---|
| n | Minimum | Maximum | Mean | Standard deviation | ||
| Group A | 22 | 64 | 100 | 89.68 | 9.87 | 0.4109 |
| Group B | 8 | 57 | 98 | 84.75 | 14.27 | |
Table 3 shows the result from the scores obtained by the entire group without separation.
Table 3.
Descriptive statistics on the scores obtained using the two scales, without separation according to groups.
| Scales | Statistics |
||||
|---|---|---|---|---|---|
| n | Minimum | Maximum | Mean | Standard deviation | |
| Lysholm | 30 | 76 | 100 | 92.33 | 7.08 |
| Kujala | 30 | 57 | 100 | 88.37 | 11.16 |
Four patients underwent reconstruction bilaterally. Two of them presented the tunnel within the anatomical region in both knees. In the other two, a tunnel that was satisfactorily located was only obtained on one side, but there were no differences in the results from the functional scores.
Discussion
Several authors have advocated reconstruction of the MPFL as the treatment for patellar instability, instead of proximal realignment.17, 18, 19, 20 Independent of the technique used, reconstruction of the MPFL has produced good patellar stability. In a review article, Lind et al.21 observed that post-reconstruction recurrence was absent from five of the eight studies, while in the remaining three, the recurrent dislocation rates were lower than 7%, which can be considered to be a success, given that in other patellar stabilization procedures, the recurrent dislocation rates have been reported to be 10–35%.7 In the present study too, there was no recurrence of patellar dislocation.
Just like Servien et al.,22 we used the radiographic method of Schöttle et al.16 in the present study to pre-establish the femoral insertion point of the graft, with modification of the zone of 5 mm in diameter to ± 7 mm, because of the diameter of the femoral tunnel. The tunnel positioning was considered to be poor when this was found to be outside of any part of the point of Schöttle et al.16 Good positioning of the femoral fixation (group A) was obtained in 73.33% of our cases and poor positioning (group B) was found in 26.67%, and this result was similar to that of Servien et al.,22 who found that 70% of the femoral points were inside the anatomical region.
McCarthy et al.23 conducted a retrospective study on 50 patients who underwent reconstruction of the MPFL alone or in association with distal realignment. These authors also used the method of Schöttle et al.16 to determine the positioning of the tunnel, and they evaluated their patients using the KOOS scale. In 36 cases (64%), the tunnel was considered to be outside of the anatomical position. Their results were concordant with those obtained in the present study and by Servien et al.,22 considering that there was no statistically significant difference in the functional scores between the groups, with regard to comparisons with the anatomical positioning in the femur.
In the present study, it was observed that 86.36% of the results were good or excellent according to the Lysholm scale in group A, while the remainder presented fair results (13.64%). None of the patients presented poor results. In group B, 87.5% of the patients presented good or excellent results. The remainder presented fair results (12.5%) and none of the patients presented poor results. These results were similar to those obtained by Servien et al.,22 who did not find any correlation between the positioning of the femoral tunnel and the IKDC analysis.
Hopper et al.24 evaluated 72 knees in 68 patients who underwent MPFL reconstruction, using the Kujala, Lysholm and Tegner scales. The radiographic positioning was also evaluated using the method of Schöttle et al.16 It was found that 46 patients (71.7%) presented the femoral tunnel in the anatomical region, and this was very similar to what was obtained in the present study and in the study by Servien et al.22 However, differing from the present study, the results were significantly better in the patients with anatomical tunnels than in the group in which the tunnel was out of position (Kujala p = 0.028; and Lysholm p = 0.012). These results were obtained after excluding patients with trochlear dysplasia from the evaluation.
It can be asked whether these poorly positioned tunnels would lead to increased incidence of osteoarthrosis over the long term, given that in these studies, in which similar results were obtained between the groups, the follow-up was only over the short term. In a biomechanical study on cadavers, Stephen et al.25 demonstrated that poorly positioned femoral tunnels that were proximal or distal in relation to their anatomical position led to significantly greater medial patellar contact pressure and medial patellar tilt during flexion–extension. This demonstrated the need for correct positioning of the femoral tunnel to restore the normal patellofemoral kinematics. Similar findings were also described by the same authors in another biomechanical study26 and by Elias and Cosgarea14 and Beck et al.27
In our setting, Bitar et al.28 compared the results from reconstruction of the MPFL using the patellar tendon with the results from conservative treatment for primary patellar dislocation. They obtained better results from the group that underwent surgery. The surgical group presented a mean score of 88.9 on the Kujala scale, i.e. similar to the result from the present study, which was 88.3 on the same scale. In the surgical group of the previous study, there were no reports of recurrences or subluxation, just as in the present study.
Gonçalves et al.29 evaluated 23 patients who underwent reconstruction of the MPFL using a free graft from the semitendinosus tendon. After a minimum follow-up of 24 months, 22 patients were evaluated using the Kujala and Lysholm clinical protocols. According to the Lysholm protocol, the patients presented a mean postoperative score of 93.36 points; and according to the Kujala protocol, the mean score was 83.54 points. These results were similar to those shown in the present study, with 92.33 and 88.37, respectively. Likewise, it could be seen that reconstruction of the medial patellofemoral ligament showed excellent short-term results, when evaluated using clinical protocols.
Conclusion
No correlation was shown in this study between good femoral radiographic positioning of the graft and better functional clinical results, with regard to reconstruction of the medial patellofemoral ligament. However, caution is needed in interpreting these results because of the short duration of the follow-up.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed in the Knee Group of Belo Horizonte, Hospital Mater Dei, Belo Horizonte, Minas Gerais, Brazil.
References
- 1.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 2.Panagiotopoulos E., Strzelczyk P., Herrmann M., Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 3.Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 4.Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87(1):36–40. [PubMed] [Google Scholar]
- 5.Davis D.K., Fithian D.C. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res. 2002;(402):38–52. doi: 10.1097/00003086-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Nomura E., Inoue M. Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy. 2003;19(5):E47. doi: 10.1053/jars.2003.50167. [DOI] [PubMed] [Google Scholar]
- 7.Sandmeier R.H., Burks R.T., Bachus K.N., Billings A. The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med. 2000;28(3):345–349. doi: 10.1177/03635465000280031001. [DOI] [PubMed] [Google Scholar]
- 8.Ellera Gomes J.L., Stigler Marczyk L.R., Cesar de Cesar P., Jungblut C.F. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20(2):147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Fithian D.C., Paxton E.W., Cohen A.B. Indications in the treatment of patellar instability. J Knee Surg. 2004;17(1):47–56. doi: 10.1055/s-0030-1247149. [DOI] [PubMed] [Google Scholar]
- 10.Smirk C., Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221–227. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 11.Nomura E., Horiuchi Y., Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9(2):139–143. doi: 10.1016/s0968-0160(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 12.Nomura E., Inoue M., Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 13.Bicos J., Carofino B., Andersen M., Schepsis A.A., Fulkerson J.P., Mazzocca A. Patellofemoral forces after medial patellofemoral ligament reconstruction: a biomechanical analysis. J Knee Surg. 2006;19(4):317–326. doi: 10.1055/s-0030-1248124. [DOI] [PubMed] [Google Scholar]
- 14.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 15.Steensen R.N., Dopirak R.M., McDonald W.G., 3rd The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32(6):1509–1513. doi: 10.1177/0363546503261505. [DOI] [PubMed] [Google Scholar]
- 16.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 17.Schöttle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 18.Nomura E., Horiuchi Y., Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121–127. doi: 10.1016/s0968-0160(00)00038-7. [DOI] [PubMed] [Google Scholar]
- 19.Drez D., Jr., Edwards T.B., Williams C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 20.Muneta T., Sekiya I., Tsuchiya M., Shinomiya K. A technique for reconstruction of the medial patellofemoral ligament. Clin Orthop Relat Res. 1999;(359):151–155. doi: 10.1097/00003086-199902000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Lind M., Jakobsen B.W., Lund B., Christiansen S.E. Reconstruction of the medial patellofemoral ligament for treatment of patellar instability. Acta Orthop. 2008;79(3):354–360. doi: 10.1080/17453670710015256. [DOI] [PubMed] [Google Scholar]
- 22.Servien E., Fritsch B., Lustig S., Demey G., Debarge R., Lapra C. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy M., Ridley T.J., Bollier M., Wolf B., Albright J., Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. [PMC free article] [PubMed] [Google Scholar]
- 24.Hopper G.P., Leach W.J., Rooney B.P., Walker C.R., Blyth M.J. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42:716–722. doi: 10.1177/0363546513518413. [DOI] [PubMed] [Google Scholar]
- 25.Stephen J.M., Kaider D., Lumpaopong P., Deehan D.J., Amis A.A. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42(2):364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
- 26.Stephen J.M., Lumpaopong P., Deehan D.J., Kader D., Amis A.A. The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40(8):1871–1879. doi: 10.1177/0363546512449998. [DOI] [PubMed] [Google Scholar]
- 27.Beck P., Brown N.A.T., Greis P.E., Burks R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 28.Bitar A.C., D’Elia C.O., Demange M.K., Viegas A.C., Camanho G.L. Estudo prospectivo randomizado sobre a luxação traumática de patela: tratamento conservador versus reconstrução do ligamento femoropatelar medial com tendão patelar. Mínimo de dois anos de seguimento. Rev Bras Ortop. 2011;46(6):675–683. doi: 10.1016/S2255-4971(15)30324-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gonçalves M.B.J., Carvalho L.H., Jr., Soares L.F.M., Gonçalves T.J., Santos R.L., Pereira M.L. Reconstrução do ligamento patelofemoral medial para tratamento da luxação recidivante da patela. Rev Bras Ortop. 2011;46(2):160–164. doi: 10.1016/S2255-4971(15)30233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]