Abstract
Objective
To compare the gain in elbow flexion in patients with traumatic injury of the brachial plexus following muscle transfer from latissimus dorsi with the gain following free muscle transfer from the medial belly of the gastrocnemius.
Methods
This was a retrospective study in which the medical files of a convenience sample of 13 patients operated between 2000 and 2010 were reviewed. Group 1 comprised seven patients who underwent transfers from the gastrocnemius and group 2 (controls) comprised six patients who underwent transfers from the latissimus dorsi. The following functions were evaluated: (1) range of motion (ROM) of elbow flexion, in degrees, using manual goniometry and (2) grade of elbow flexion strength, using a muscle strength scale. Satisfactory results were defined as: (1) elbow flexion ROM ≥ 80° and (2) elbow flexion strength ≥ M3. The Fisher exact and Kruskal–Wallis tests were used (p < 0.05).
Results
The patients’ mean age was 32 years (range: 17–56) and 72% had been involved in motorcycle accidents. Elbow flexion strength ≥ M3 was observed in seven patients (100%) in group 1 and in five patients (83.3%) in group 2 (p = 0.462). None of the patients presented M5, and one patient (16.7%) in group 2 had a poor result (M2). Elbow flexion ROM with a gain ≥ 80° (daily functions) was found in six patients (86%) in group 1 and in three patients (50%) in group 2 (p = 0.1).
Conclusion
The patients in group 1 had greater gains in strength and ROM than did those in group 2, but without statistical significance. Thus, transfers from the gastrocnemius become a new surgical option, if other techniques cannot be used.
Keywords: Brachial plexus/surgery, Muscle/transplant, Reconstructive surgical procedures
Resumo
Objetivo
Comparar o ganho de flexão do cotovelo em pacientes com lesão traumática do plexo braquial após transferência muscular do latíssimo dorsal (TMLD) com a transferência muscular livre do ventre medial do gastrocnêmio (TMLGM).
Metódos
Estudo retrospectivo, revisão de prontuários, amostra de conveniência, com 13 pacientes operados, entre 2000 e 2010. Grupo 1 (TMLGM) com sete pacientes e grupo 2 ou controle (TMLD) com seis. Função avaliada: 1) amplitude de movimento (ADM) em graus da flexão do cotovelo, goniometria manual; 2) grau de força de flexão do cotovelo, por escala de força muscular. Satisfatórios: 1) ADM: flexão do cotovelo ≥ 80°; 2) Força: flexão do cotovelo ≥ M3. Testes exato de Fisher e Kruskal–Wallis (p < 0,05).
Resultados
Média de idade foi de 32 anos (17 a 56). Acidente de moto em 72%. Força de flexão do cotovelo ≥ M3 no grupo 1 em sete pacientes (100%) e o grupo 2 em cinco (83,3%) (p = 0,462). Não tivemos M5 e o grupo 2 apresentou um paciente (16,7%) com resultado ruim M2. ADM na flexão do cotovelo com ganho ≥ 80° (funções diárias) foram encontrados no grupo 1 em seis pacientes (86%) e no grupo 2 em três (50%) (p = 0,1).
Conclusão
Pacientes do grupo 1 tiveram um ganho maior de força e ADM, quando comparados com os do grupo 2, sem significado estatístico. Assim, TMLGM se torna uma nova opção cirúrgica, caso não possam ser aplicadas outras técnicas.
Palavras-chave: Plexo braquial/cirurgia, Músculo/transplante, Procedimentos cirúrgicos reconstrutivos
Introduction
Traumatic brachial plexus injuries (BPIs) can hinder the elbow flexion function and thus dramatically alter the quality of life of individuals. Very often, the initial microneurosurgery cannot appropriately restore movement in this joint. In older injuries, nerve repair surgeries are not recommended, as there is definite atrophy and classic muscle transfers (MT) are possible only in partial lesions. Thus, some patients require complementary interventions for functional gain of elbow flexion. These procedures are related to MT or free muscle transfer (FMT).1
The MTs were the first techniques described. Steindler flexorplasty and use of the latissimus dorsi, pectoralis major and triceps were the main types.2 The FMTs are newer and exhibit higher technical difficulty, due to the need to perform the neurovascular microanastomosis between the transplanted muscle pedicle and the vessels and nerves of the injury site. In the upper limb, and more specifically to gain elbow flexion, the techniques used are the FMT of the contralateral latissimus dorsi (LD), rectus femoris and gracilis muscles.1, 3
The literature has only three studies concerning the medial gastrocnemius (MG) used in the upper limb for FMT, in order to recover the function of an injured muscle group. Liu et al.4 used it for Volkmann's ischemic contracture in the forearm, with good functional results. Serafin5 proposed that the MG would have significant potential to restore elbow flexion or extension. Kwae et al.6 described the FMT of the MG to gain elbow flexion in patients with traumatic BPI.
The aim of this study was to compare the gain in elbow flexion in patients with traumatic BPI after standard surgical procedure of MT of the LD (control group) with FMT of the MG (study group).
Method
Retrospective study carried out by the review of medical records from a convenience sample consisting of 13 patients with traumatic BPI that were consecutively submitted to surgical procedure from December 2000 to December 2010 at the Hand and Microsurgery Service. These patients were divided into two groups. Group 1 or study consisted of seven patients submitted to FMT of the MG and group 2 or control consisted of six patients submitted to MT of the LD.
Patients that were included in the two groups had muscle strength equal to M0 (without strength) and degree of elbow flexion between 0 and 10° (no movement), who had already been submitted to surgery with other techniques, but without success, or those that had the plexus injury for about a year and had not been treated surgically, without the possibility of a previous neural surgery. Also, as inclusion criteria, patients with preoperative LD muscle activity ≥ M4 were chosen for the LD control group, while for the MG study group, patients with LD strength ≤ M3 were selected, as LD transfer would be contraindicated in this situation.
We excluded patients that had incomplete data in their medical records, or preoperative strength ≥ M1 and elbow flexion > 10°.
The data collected from medical records consisted of age, time of injury in months, neural injury level, type of neural damage, type of muscle transfer, type of previous surgery, elbow flexion strength and range of motion for both pre- and postoperative periods.
The level and type of neurologic injury were diagnosed by preoperative electromyography. As for elbow flexion, the degree of muscle strength was measured by the British Medical Council scale (M0 = no movement; M1 = only a trace or flicker of movement is seen or felt, or fasciculations are observed; M2 = muscle can only move if resistance of gravity is removed; M3 = joint can be moved only against gravity with examiner's resistance completely removed; M4 = strength reduced, but contraction can still move joint against resistance; M5 = normal strength) and a manual goniometer was used to measure range of motion (ROM), starting from zero degrees in total elbow extension to the maximum angle achieved and maintained by the patient, one year after muscular transfer surgery.
In group 1, the MG FMT was performed with the following steps: (1) median curvilinear longitudinal incision, which starts 8 cm proximal to the popliteal crease, extends distally up to 10 cm proximal to the medial malleolus; (2) dissection of the intermuscular septum between the two gastrocnemius bellies, laterally displacing the small saphenous vein and the sural nerve, individualizing the muscle and neurovascular structures of the popliteal fossa; (3) the origin of the MG is then severed from the femoral medial condyle and the medial sural neurovascular bundle is dissected and clamped for resection, in its longest extension, 1 cm proximal to the joint; (4) identification of the sciatic, medial popliteal and tibial nerve (from the roots of L4–L5/S1–S3 of the lumbosacral plexus), from which the branch to the MG originates, called medial sural nerve (MSN), according to the anatomical model described by Moraes et al.7 (5) identification of the number of arterial and venous branches that arrive at the MG pedicle, as well as the crossing of the small saphenous vein over the MSN, which may hinder its dissection; (6) deltopectoral incision and subcutaneous dissection in the upper limb to where one intends to transfer the MG for biceps function with dissection of the artery, the thoracodorsal vein and the cephalic vein; (7) MG FMT for elbow flexion, with fixation of the proximal ventral region at the proximal end of the humerus through the bone window and fixation with cortical screws in the distal region of the distal stump of the biceps tendon; (8) microanastomosis of the arterial branch of the MG in the thoracodorsal artery; the veins were attached, one in the thoracodorsal vein and another in the cephalic vein; (9) the microanastomosis of the MG MSN was carried out in different peripheral branches, with neurotizations to the musculocutaneous from the ulnar, intercostal or accessory nerves.1, 8, 9
One of the principles of surgical reconstruction of traumatic BPIs is the recovery of elbow flexion. Thus, the following parameters are considered satisfactory: (1) ROM: elbow flexion ≥ 80° and (2) strength: elbow flexion ≥ M3. Group 2 consisted of patients submitted to ipsilateral latissimus dorsi transfer, which was performed as previously described in literature.1, 2
Data were collected and stored in Excel for Windows and analyzed using the statistical software program SPSS for Windows, version 13.0. All samples were evaluated by Fisher's exact test for parametric data and Kruskal–Wallis test for nonparametric data. Statistical significance was set at p ≤ 0.05.
Results
Of the 13 patients assessed to improve elbow flexion function after traumatic BPI, seven (54%) were in group 1 (free muscle transfer of the medial gastrocnemius), with a mean lesion time of 18.4 months (10–30), and six (46%) in group 2 or control (latissimus dorsi transfer), with a mean time of lesion of 22.3 months (12–36). All patients were males.
Mean age was 32 years (17–56). The right side was affected in seven (54%) cases and the left in six (46%). Seven cases (54%) were from Goiânia and six (46%) from the state of Goiás countryside. Regarding work, two patients (15%) were unemployed, five (39%) did manual work and six (46%) worked in the administrative area.
Motorcycle accident was the cause of the injury in nine patients (70%) (p < 0.05); one (7.5%) case was due to automobile accident, one (7.5%) case was hit by a car, one (7.5%) had a work-related accident and one (7.5%) was due to firearm injury.
The clinical characteristics of patients in group 1 (MG) related to the type of brachial plexus injury and its evolution after treatment are shown in Table 1 and those of group 2 (GD) are shown in Table 2.
Table 1.
Clinical characteristics of patients submitted to free transfer from the medial gastrocnemius muscle for gain in elbow flexion (group 1).
| P | Age | Time of lesion (months) | Neural lesion level | Type of neural lesion | Previous surgery | Pre-op flexion strength | Pre-op ROM | Post-op flexion strength | Post-op ROM |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 42 | 30 | C5C6C7C8 | Axonotmesis | Neurolysis neurotization AC > SE | MO | 0–10° | M3 | 0–90° |
| 2 | 26 | 29 | C5C6C7C8 | Axonotmesis | Neurolysis neurotization AC < SE + sural graft | MO | 0–10° | M3 | 0–80° |
| 3 | 36 | 20 | C5C6C7C8 | Neurotmesis | Neurorrhaphy C5C6 + sural graft | MO | 0–10° | M3 | 0–80° |
| 4 | 31 | 11 | C5C6C7 | Axonotmesis | No surgery | MO | 0–10° | M4 | 0–60° |
| 5 | 21 | 10 | C5C6C7C8 | Axonotmesis | No surgery | MO | 0–10° | M4 | 0–90° |
| 6 | 17 | 18 | C5C6C7C8 | Axonotmesis | Neurolysis neurotization AC < SE + sural graft | MO | 0–10° | M4 | 0–90° |
| 7 | 23 | 12 | C5C6C7C8 | Neuropraxis | No surgery | MO | 0–0° | M4 | 0–90° |
Table 2.
Clinical characteristics of patients submitted to muscle transfer from latissimus dorsi for elbow flexion gain (group 2).
| P | Age | Time of lesion (months) | Neural lesion level | Type of neural lesion | Previous surgery | Pre-op flexion strength | Pre-op ROM | Post-op flexion strength | Post-op ROM |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 32 | 36 | C5C6 | Axonotmesis | Neurolysis neurotization AC < SE + sural graft | MO | 0–10° | M3 | 0–90° |
| 2 | 56 | 23 | C5C6 | Neurotmesis | Neurolysis neurotization AC < SE + sural graft + oberain | MO | 0–10° | M2 | 0–30° |
| 3 | 23 | 18 | C5C6C7 | Neurotmesis | No surgery | MO | 0–10° | M3 | 0–80° |
| 4 | 50 | 19 | C5C6C7C8 | Axonotmesis | Neurolysis neurotization AC < SE + sural graft oberain | MO | 0–10° | M3 | 0–60° |
| 5 | 39 | 12 | C5C6 | Axonotmesis | Neurolysis C5C6 | MO | 0–10° | M4 | 0–120° |
| 6 | 31 | 26 | C5C6 | Axonotmesis | Neurolysis neurotization AC < SE + sural graft + oberain | MO | 0–10° | M3 | 0–60° |
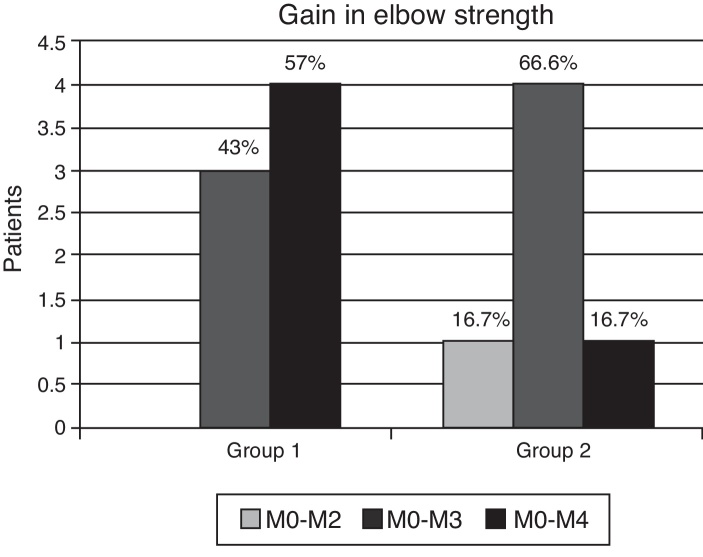
Regarding gain of strength in elbow flexion, we observed that both groups had satisfactory results with a gain equal to or above M3, group 1 with seven patients (100%) and group 2 with five (83.3%), but no significant difference (p = 0.462). There were no results with gain M5 and group 2 had one patient (16.7%) with poor results in terms of strength gain, which only achieved M2 (Fig. 1).
Fig. 1.
Assessment of gain in elbow flexion strength between the assessed groups.
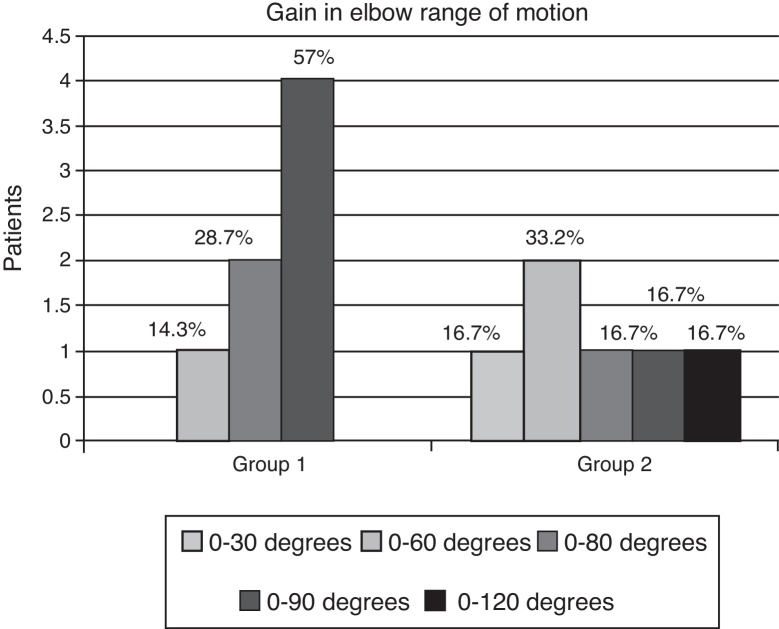
Regarding the range of motion gain in degrees of elbow flexion, we observed that satisfactory results with gains > 80° in daily functions were found in group 1 in six patients (86%) and in group 2 in three (50%), but with no significant difference (p = 0.1). There were no results with gain > 150°. Regarding the results in which flexion was only achieved up to 60°, there was only one patient (14.3%) in group 1 and three patients in group 2 (50%) (Fig. 2).
Fig. 2.
Assessment of gain in elbow flexion range of motion between the groups.
Discussion
Elbow flexion improvement in patients with traumatic BPIs provides an important gain in the injured limb function and an elbow considered adequate is the one with strength ≥ M3, ideally ≥ M4 and with more than 80° of active flexion.2 The MTs are mainly indicated in cases where the patient has had a partial injury or only in the upper trunk (C5C6) or shows good hand and wrist function.
The FMT have a wider range of possibilities, but with far greater technical difficulties. For the hand to work adequately, the shoulder must be stable and the elbow must have adequate flexion–extension activity, to position it in the space.9 Otherwise the limb will become nonfunctional. Both in the MT or FMT for elbow recovery, regardless of the chosen technique, the elbow joint cannot be ankylosed or contracted and the chosen muscle must have M4 or M5 strength.
The MT from the triceps to the biceps is considered by Steindler10 as unsatisfactory, as it can affect elbow extension. The triceps has an important function in the upper limb and, therefore, the MT should be used only as a last resort. According to some authors, such as Pardiniet al.11 they use it due to the technical simplicity, as well as because this MT is able to allow the patient to move the hand to the head and mouth with satisfactory flexion of around 120° and provides muscle strength to support up to three and a half kilograms.
The MT from the pectoralis major to the biceps can be used in the partial unipolar, partial bipolar or complete bipolar manner, in which the sternocostal, clavicular and humeral portions are used. Its main contraindication in relation to other MTs is damage to the axillary artery, which impairs the thoracoacromial artery. However, it is not the first option either, as the pectoralis major is part of the shoulder girdle and may be used for shoulder recovery and its results are not satisfactory for most patients, who end up attaining only 60° of elbow flexion in average and with little strength.12
Steindler flexorplasty10 was the first procedure used for rehabilitation of the paralyzed elbow. It was initially applied in patients with polio sequelae, obstetrical and arthrogrypotic paralysis and only later in traumatic BPI. That MT is performed by freeing the medial elbow epicondyle along with flexor–pronator muscles of the forearm (pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis and flexor carpi ulnaris) and then subsequently fixation to a more proximal portion of the humerus. It is currently one of the most widely used techniques, as it is simple to perform and can attain more than 100° of elbow flexion in 70% of patients. However, its disadvantages are a decrease in the flexing strength of the hand and wrist; objects can be raised only if they weight up to two kilograms and the contracture of elbow joint.13
However, it is the main MT used for elbow recovery and from the latissimus dorsi to the ipsilateral biceps, where the results can reach over 100° of active elbow flexion and M4 strength. The latissimus dorsi can be transferred in unipolar or bipolar manner and the main contraindication is the lack of an adequate postoperative rehabilitation program.14
As for the FMT, the most often used muscle is the contralateral latissimus dorsi15, 16, 17 followed by the gracilis (GD) from the lower limb, and rarely the rectus femoris.1 The indication for a FMT comes from the need to restore elbow flexion function in traumatic BPIs, even after neurosurgical procedures in the plexus, or in cases that are referred for treatment after one year. The FMT will not be necessary when science is able to maintain the morphology and ultrastructure of denervated muscle make neural grafts directly onto the spinal cord and accelerate the neuronal regeneration velocity.18
The gracilis FMT can be performed as a single procedure to gain elbow flexion function or as dual procedure to attain elbow flexion and at the same time improve hand function and shoulder stability. When it is used only to gain elbow flexion, approximately 80% of patients reach M4 strength, but when used as dual function, this number decreases to 60%.19, 20, 21
According to the literature,22, 23, 24, 25, 26 the MG has attractive features for FMT, such as: length, excursion capacity, contraction force proportional to the sectional area, long insertional tendon, adequate neurovascular bundle (blood supply class I), pure motor branch of the MSN from the medial popliteal nerve (95% single branch).
Other advantages are: resection of only one gastrocnemius belly, which does not affect the plant flexion function and does not cause major deformity. The scar left by the MG removal is cosmetically acceptable, especially in men. Moreover, in patients that may be submitted to local transfers, the MG FMT has the advantage of adding another muscle group to a weakened upper limb, aiming at better function. The disadvantages are: the scars in women; the supine position makes it difficult to dissect at the donor site (popliteal fossa) in FMT to upper limb. Optionally, the procedure can be performed with the patient in the lateral decubitus position.
We believe that the anastomosis of the MSN with part of the ulnar showed better performance than with the intercostal nerve, due to the shorter reinnervation distance. However, the use of the intercostal nerve can be considered an option if the ulnar is not available.
The MG FMT to biceps had not been performed, until then, for this purpose. Thus Kuwae et al.6 described in two cases the MG FMT for elbow flexion function recovery in patients with traumatic BPIs. In our study, we observed good results ≥ M3 in 100% of MG FMT and 85.6% in GD MT and excellent results with M4 in 57% of the MG FMT and 29% in GD MT, but without significant difference. Regarding the elbow range of motion, flexion exceeded 80° in 85.6% of patients undergoing MG FMT and in 57% of patients submitted to GD MT. This difference was not significant between the groups.
When comparing the results of the two groups, there was no difference in elbow flexion gain. Patients submitted to free transfer of the medial gastrocnemius muscle had a higher gain in strength and ROM when compared with the control group submitted to latissimus dorsi transfer, but without statistical significance. Thus, MG FMT can be considered a technique of which results are not inferior to those of the LD MT standard technique and becomes a viable option if other techniques cannot be applied.
Conclusion
Patients submitted to the free transfer of the medial gastrocnemius muscle had a higher gain in strength and ROM when compared with the control group submitted to latissimus dorsi transfer, but without statistical significance. Thus, the free muscular transfer of the gastrocnemius becomes a new surgical option if other techniques cannot be applied.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study carried out at Hand and Microsurgery Service, Hospital das Clínicas, Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil.
References
- 1.Vekris M.D., Beris A.E., Lykissas M.G., Korompilias A.V., Vekris A.D., Soucacos P.N. Restoration of elbow function in severe brachial plexus paralysis via muscle transfers. Injury. 2008;39(Suppl 3):S15–S22. doi: 10.1016/j.injury.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Bengtson K.A., Spinner R.J., Bishop A.T., Kaufman K.R., Coleman-Wood K., Kircher M.F. Measuring outcomes in adult brachial plexus reconstruction. Hand Clin. 2008;24(4):401–415. doi: 10.1016/j.hcl.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Barrie K.A., Steinmann S.P., Shin A.Y., Spinner R.J., Bishop A.T. Gracilis free muscle transfer for restoration of function after complete brachial plexus avulsion. Neurosurg Focus. 2004;16(5):E8. doi: 10.3171/foc.2004.16.5.9. [DOI] [PubMed] [Google Scholar]
- 4.Liu X.Y., Ge B.F., Win Y.M., Jing H. Free medial gastrocnemius myocutaneous flap transfer with neurovascular anastomosis to treat Volkmann's contracture of the forearm. Br J Plast Surg. 1992;45(1):6–8. doi: 10.1016/0007-1226(92)90105-7. [DOI] [PubMed] [Google Scholar]
- 5.Serafin D. The gastrocnemius flap. In: Serafin D., editor. Atlas of microsurgical composite tissue transplantation. Saunders; Philadelphia: 1996. pp. 303–310. [Google Scholar]
- 6.Kuwae M.Y., Moraes F.B., Paranahyba R.M., Oliveira E. Transferência muscular livre funcional do gastrocnêmio medial em lesão do plexo braquial: relato de dois casos. Rev Bras Ortop. 2007;42(1):37–40. [Google Scholar]
- 7.Moraes F.B., Oliveira E., Paranahyba R.M., Kwae M.Y., Rocha V.L. Estudo anatômico do músculo gastrocnêmio medial visando transferência muscular livre. Rev Bras Ortop. 2007;42(1/2):37–40. [Google Scholar]
- 8.Hattori Y., Doi K., Baliarsing A.S. A part of the ulnar nerve as an alternative donor nerve for functioning free muscle transfer: a case report. J Hand Surg Am. 2002;27(1):150–153. doi: 10.1053/jhsu.2002.29484. [DOI] [PubMed] [Google Scholar]
- 9.Akasaka Y., Hara T., Takahashi M. Free muscle transplantation combined with intercostal nerve crossing for reconstruction of elbow flexion and wrist extension in brachial plexus injuries. Microsurgery. 1991;12(5):346–351. doi: 10.1002/micr.1920120506. [DOI] [PubMed] [Google Scholar]
- 10.Steindler A. Muscle and Tendon transplantation at the elbow. In: Arbor A., Edwards J.W., editors. Instructional course lectures on reconstructive surgery. JW Edwards; Ann Arbor: 1944. pp. 276–283. [Google Scholar]
- 11.Pardini A.G., Freitas A.L., Freitas A.D., Tavares K.E. Transferências tendinosas para flexão do cotovelo. Rev Bras Ortop. 1996;31(3):211–216. [Google Scholar]
- 12.Hierner R., Berger A. Pectoralis major muscle transfer for reconstruction of elbow flexion in posttraumatic brachial plexus lesions. Oper Orthop Traumatol. 2009;21(2):126–140. doi: 10.1007/s00064-009-1701-z. [DOI] [PubMed] [Google Scholar]
- 13.Al-Qattan M.M. Elbow flexion reconstruction by Steindler flexorplasty in obstetric brachial plexus palsy. J Hand Surg Br. 2005;30(4):424–427. doi: 10.1016/j.jhsb.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Kawamura K., Yajima H., Tomita Y., Kobata Y., Shigematsu K., Takakura Y. Restoration of elbow function with pedicled latissimus dorsi myocutaneous flap transfer. J Shoulder Elbow Surg. 2007;16(1):84–90. doi: 10.1016/j.jse.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Hovnanian A.P. Latissimusdorsi transplantation for loss of flexion or extension at the elbow; a preliminary report on technic. Ann Surg. 1956;143(4):493–499. doi: 10.1097/00000658-195604000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oberlin C. Brachial plexus palsy in adults with radicular lesions, general concepts, diagnostic approach, and results. Chir Main. 2003;22(6):273–284. doi: 10.1016/j.main.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Terzis J.K., Kostopoulos V.K. The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg. 2007;119(4):73e–92e. doi: 10.1097/01.prs.0000254859.51903.97. [DOI] [PubMed] [Google Scholar]
- 18.Bishop A.T. Functioning free-muscle transfer for brachial plexus injury. Hand Clin. 2005;21(1):91–102. doi: 10.1016/j.hcl.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Doi K., Muramatsu K., Hattori Y., Otsuka K., Tan S.H., Nanda V. Restoration of prehension with the double free muscle technique following complete avulsion of the brachial plexus. Indications and long-term results. J Bone Joint Surg Am. 2000;82(5):652–666. [PubMed] [Google Scholar]
- 20.Chung D.C., Carver N., Wei F.C. Results of functioning free muscle transplantation for elbow flexion. J Hand Surg Am. 1996;21(6):1071–1077. doi: 10.1016/s0363-5023(96)80318-2. [DOI] [PubMed] [Google Scholar]
- 21.Salibian A.H., Rogers F.R., Lamb R.C. Microvascular gastrocnemius muscle transfer to the distal leg using saphenous vein grafts. Plast Reconstr Surg. 1984;73(2):302–307. doi: 10.1097/00006534-198402000-00030. [DOI] [PubMed] [Google Scholar]
- 22.Smrcka V., Stingl J., Kubin K., Moravec Z. Anatomical notes on gastrocnemius muscle uses for muscle flap preparation. Acta Chir Plast. 1986;28(2):112–120. [PubMed] [Google Scholar]
- 23.Mairesse J.L., Mestdagh H., Procyk S., Depreux R. Contribution à l’étude de la vascularisation artérielle du muscle triceps sural. Anat Anz. 1984;155(1–5):195–202. [PubMed] [Google Scholar]
- 24.Dibbell D.G., Edstrom L.E. The gastrocnemius myocutaneous flap. Clin Plast Surg. 1980;7(1):45–50. [PubMed] [Google Scholar]
- 25.McCraw J.B., Fishman J.H., Sharzer L.A. The versatile gastrocnemius myocutaneous flap. Plast Reconstr Surg. 1978;62(1):15–23. doi: 10.1097/00006534-197807000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Arnold P.G., Mixter R.C. Making the most of the gastrocnemius muscles. Plast Reconstr Surg. 1983;72(1):38–48. doi: 10.1097/00006534-198307000-00010. [DOI] [PubMed] [Google Scholar]