Abstract
Purpose
The purpose of the present investigation is to differentiate children using cochlear implants (CIs) who did or did not achieve age-appropriate language scores by midelementary grades and to identify risk factors for persistent language delay following early cochlear implantation.
Materials and Method
Children receiving unilateral CIs at young ages (12–38 months) were tested longitudinally and classified with normal language emergence (n = 19), late language emergence (n = 22), or persistent language delay (n = 19) on the basis of their test scores at 4.5 and 10.5 years of age. Relative effects of demographic, audiological, linguistic, and academic characteristics on language emergence were determined.
Results
Age at CI was associated with normal language emergence but did not differentiate late emergence from persistent delay. Children with persistent delay were more likely to use left-ear implants and older speech processor technology. They experienced higher aided thresholds and lower speech perception scores. Persistent delay was foreshadowed by low morphosyntactic and phonological diversity in preschool. Logistic regression analysis predicted normal language emergence with 84% accuracy and persistent language delay with 74% accuracy.
Conclusion
CI characteristics had a strong effect on persistent versus resolving language delay, suggesting that right-ear (or bilateral) devices, technology upgrades, and improved audibility may positively influence long-term language outcomes.
It is well known by now that cochlear implants (CIs) often provide great benefit to young deaf children who are learning to talk. Research has demonstrated many children using CIs acquired early in life eventually achieve age-appropriate scores on spoken language tests (Duchesne, Sutton, & Bergeron, 2009; Fulcher, Purcell, Baker, & Munro, 2012; Leigh, Dettman, Dowell, & Briggs, 2013). Despite these successes, puzzling aspects remain regarding the efficacy of this technology. Primary among these is the wide variability in learning rates and outcomes across children, even among those using CIs for many years (Niparko et al., 2010) and without obvious additional risk factors. Even among children who seem to share very similar auditory history, input, and speech perception benefit, early language delays may resolve or persist with little predictability. In this article, we approach the problem by looking at longitudinal outcomes data in ways similar to the literature on chronic language delay in otherwise typically developing (TD) children without hearing loss.
In attempting to capture the nature of language development trajectories and simultaneously include clinically relevant information, many studies of hearing children at risk for language delays or impairment construct descriptive categories on the basis of both past and current language performance (Reilly et al., 2014; Rice, Taylor, & Zubrick, 2008). A deviation score cut-off on language tests is used to operationally define language delay relative to the normative mean. Then a child's language scores at two or more points in time lead to a category label (e.g., delay that resolves, delay that persists, etc.) that represents that child's growth trajectory in a clinically and educationally meaningful way.
Although it has been demonstrated that early and later language abilities are positively correlated (e.g., Pankratz, Plante, Vance, & Insalaco, 2007), the predictive accuracy for individual children is limited because a substantial proportion of language-delayed children recover throughout the preschool years (Ellis & Thal, 2008). Accuracy of prediction also decreases with age at first test and is weakest for children under 6 years of age (Birney & Sternberg, 2006), and therefore the clinical classification of children can change over time, particularly during the preschool years. Dollaghan and Campbell (2009) studied language scores of a large group of children at 3, 4, and 6 years of age and found children who obtained low scores at an earlier age were no more likely than other children to obtain low scores at later ages. Nonetheless, large-scale studies are useful in understanding the incidence of this clinical condition. An epidemiological study of 10,587 Norwegian children between 3 and 5 years of age (Zambrana, Pons, Eadie, & Ystrom, 2014) reported that 3%, 5%, and 6.5% of children displayed persistent, transient, and late-onset language delay, respectively. Delay was defined as 1.5 SD below the normative mean. Risk factors associated with persistent language delay included male gender, early comprehension delays (especially in girls), and a family history of language-related difficulties. Although children with resolving delays (i.e., transient delay or late-emerging language) are likely to perform within the range of TD peers by school age, continued weaknesses in specific areas of language have been reported (Rescorla, 2002; Rice et al., 2008). Language delay that persists beyond the preschool years is highly predictive of poor reading and academic outcomes (Scarborough, 2001; Zambrana et al., 2014). Rice (2003) proposed growth-timing factors function to help some children “reset” their growth trajectories and hence overcome their initial delays. The identification and facilitation of such factors would be of value to all clinical populations.
Predicting Language Delay in Children With CIs
The uncertainty of predicting long-term language delay is even greater in the case of children with congenital severe–profound hearing loss. Children with similar language scores before implantation exhibit very different trajectories of development (Tobey et al., 2013; Yoshinaga-Itano, Baca, & Sedey, 2010). Some children catch up rather quickly after auditory input is provided, some more slowly, and some never catch up (Geers & Sedey, 2011). Yoshinaga-Itano et al. (2010) reported 24% of CI users with longitudinal data from birth through 84 months were “gap closers” who caught up with hearing age-mates on expressive language measures, whereas only 9% of hearing aid users with similar levels of hearing loss did so.
As in children with normal hearing (NH), some children receiving CIs appear to reset their growth trajectory after some duration of use, whereas others experience chronic, persisting delays. Few empirical studies have specifically contrasted the characteristics and experiences of those with both differing initial responses to receipt of a CI as well as subsequent outcomes. Hawker et al. (2008) reported the “disproportionate language impairment (DLI)” of a group of children using CIs, characterized as performing more poorly at 7 years post-CI than a closely matched group with similar CI experience. Hawker et al. argued for the plausibility of a genetic explanation for the differences, suggesting the DLI group was predisposed to deficits seen in hearing children with specific language impairment (SLI).
In a follow-up, Ramirez-Inscoe and Moore (2011) tested a larger group of children with DLI (N = 25) and matched controls (using CIs, but no DLI). They report that 35% of the siblings in the DLI group had abnormal profiles (SLI-like language scores) versus 8% of the siblings of the matched CI users without DLI. This observation was interpreted as indicating DLI may result from “the same heritable and environmental factors that influence language development in all children” (p. 690). Whether continuing DLI in children with long-term CI use is best explained as a language impairment or as representing the furthest end of a continuum of performance negatively affected by hearing loss remains unresolved (see Gilbertson & Kamhi, 1995). With the demonstration that a notable proportion of children with early CIs do not experience delays, we may consider whether some proportion of persistent delays represent concomitant language impairment. Evidence may appear in the same linguistic indicators observed in the language and speech of children without hearing loss. Nonetheless, identifying risk factors for spoken language delay in children with CIs necessarily begins with assessing individual differences in the audibility and perception of speech.
There can be little doubt that audibility and discriminability of speech with a CI has an impact on the facility with which children acquire spoken language. Aided sound-field thresholds are used to verify that the CI provides access to soft-level speech inputs across the frequency range from 250 to 4000 Hz, and lower or better aided thresholds have been associated with better speech perception at soft and conversational levels without detrimental effects on speech perception in noise (Davidson, Geers, Blamey, Tobey, & Brenner, 2011; Davidson, Skinner, Holstad, et al. 2009; Firszt et al., 2004). Aided thresholds that approximate 20 dB HL (250–4000 Hz) have been associated with better speech perception scores for adults (Holden et al., 2013) and better speech perception, novel word learning, and ultimately vocabulary level for children (Davidson, Geers, & Nicholas, 2014).
Audibility and speech perception may be influenced by upgrades to newer speech processor technologies. Over the years, updates in CI technology have included redesigned internal equipment (i.e., electrode arrays and internal receiver stimulators), new speech processing strategies, and external device hardware (speech processors and microphones; Carlson, Driscoll, Gifford, & McMenomey, 2012; Wilson & Dorman, 2008). For example, early improvements in speech processing strategies resulted in significant improvements in speech perception for adults and children (Geers, Brenner, & Davidson, 1999; Skinner, Arndt, & Staller, 2002; Skinner et al., 1994; Tomblin, Peng, Spencer, & Lu, 2008; Wilson & Dorman, 2008). Improved front-end processing strategies and microphone and processor technology have combined to improve speech perception, especially for access to low-level speech inputs (Davidson, 2006; Dawson, Decker, & Psarros, 2004; Dawson, Vandali, Knight, & Heasman, 2007). In addition, more children are receiving a second CI, and recent evidence suggests that bilateral implantation promotes vocabulary and overall language development in children (Sarant, Harris, Bennet, & Bant, 2014). However, length of second CI use (i.e., duration of bilateral experience) did not predict language levels in a group of 39 children with two CIs (Hess et al., 2014).
A number of other risk factors for delay in spoken language have been identified, including later age at implantation (Castellanos et al., 2014; Leigh et al., 2013; Nicholas & Geers, 2007), poorer speech production and language skills in preschool, environmental factors (Castellanos et al., 2014), and inner ear malformations or meningitis (Black, Hickson, Black, & Perry, 2011; O'Brien et al., 2012). Nittrouer, Caldwell, Lowenstein, Tarr, and Holloman (2012) found that comprehension of spoken language was the best predictor, in children below 24 months of age, of their language/literacy skills in kindergarten. Tomblin et al. (2008) found that accuracy of speech sound production at 4 years postimplant was a good predictor of speech skills after 5 to 10 years of use. Moeller et al. (2007) studied speech sound development between 10 and 24 months of age in 33 children with and without hearing loss and found that early measures of syllable production predicted unique variance in later speech production and vocabulary outcomes. Their results suggested that earlier, accurate, and flexible consonant use may facilitate word learning. Six of the children reported by Moeller et al. (2007) with atypical speech and language development exhibited smaller consonant inventories, less complex syllable shapes, less accurate word forms, and frequent consonant deletions. These early speech characteristics were similar to those reported for typically hearing children with SLI (Pharr, Ratner, & Rescorla, 2000). These findings support the use of speech production characteristics as predictors of persistent language delay regardless of hearing status.
Rationale for Current Investigation
We sought to identify early risk factors and current characteristics differentiating early-implanted children who experience (a) no language delays, (b) a delay in preschool that resolves, or (c) a delay in preschool that persists to the midelementary grades. A previous report (Geers & Nicholas, 2013) on the same longitudinal sample of children confirmed long-lasting advantages of younger age at cochlear implantation, better pre-CI aided hearing, and higher nonverbal intelligence for spoken language outcomes into midelementary grades. However, regression analysis including all of these factors predicted less than half the total variance in language outcome scores. In that study, the proportion of children scoring within 1 SD of hearing age-mates in overall language skills more than doubled between preschool and primary grades, from 32% to 68%. It is presumed that those who were initially delayed but then caught up were not language-impaired, but could instead be characterized as experiencing late-emerging language. Furthermore, fully one-third of the group exhibited persistent language delay throughout the preschool and primary years. This is more than double the figure of 15% of children in the normative population who are expected to score more than 1 SD below the mean. The categorical approach used in this study compares group characteristics of children with late-emerging language and persistent language delay (as in Zambrana et al., 2014) and contrasts them with children who achieved age-appropriate language scores in preschool and maintained them into primary grades. These categories will be referred to as language-emergence groups.
The purpose of this article is to present a reanalysis and expansion of previously published longitudinal data (Geers & Nicholas, 2013; Nicholas & Geers, 2007) on the same sample of children using CIs. The previous report approached questions regarding language abilities by identifying factors associated with optimal performance. In the present article, we focus directly on those who are experiencing difficulties and try to understand who will overcome those initial difficulties and who will not. On the basis of previous investigations, we hypothesize three categories of factors that may distinguish the group with persistent language delay. First are child and family characteristics associated with language delay in hearing children: male gender, lower nonverbal intelligence, and less maternal education. Second are factors related to hearing loss: poorer preimplant hearing, older age at receipt of first hearing aid and CI, higher CI-aided thresholds, monaural device use, and less current CI technology. A third set of predictors includes aspects of early speech and language (grammar, vocabulary, speech production) informed by studies of delay and impairment in children with NH. Here the literature on persistent language delay in children with NH predicts immature lexical and morphosyntactic ability, along with more limited phonetic repertoire. Last, we include intensity of educational intervention during the elementary grades (age at mainstream placement, class size, and individual therapy) as a possible differentiating factor.
We hypothesized that very early auditory stimulation and strong cognitive ability would facilitate early speech and language with minimal delays, but that children without these advantages may still reach age-appropriate levels if they receive further improved auditory input for a sufficient length of time. The factors affecting whether a child experiences no delay, an initial delay that resolves, or an initial delay that persists differ depending on the observed course of development. Children who experience no delay (and remain so) are likely to have higher cognitive ability and the earliest ages of implantation. Children with preschool language delay who subsequently receive updated technology and/or a second CI that results in improved audibility and speech perception are more likely to have their delays resolve within several years. Children at greatest risk for language delays that persist into the middle childhood years will exhibit early signs of language impairment in their conversational speech and language.
Materials and Methods
Participants
The longitudinal sample was recruited from participants in a previous study of 76 preschoolers who received a CI between 12 and 38 months of age (Nicholas & Geers, 2006), identified by auditory-oral preschools and speech therapy practices across North America. Candidate children were excluded if there was evidence of (a) previous NH or a progressive loss, (b) below-average nonverbal learning abilities as tested in preschool, or (c) use of a language other than English as the primary language at home. The children received one CI between 1998 and 2003. Seventy-five percent of the sample received their first CI in the right ear. Length of CI use varied between 7 and 32 months at the time of first assessment at 3.5 years of age (±2 months). All children were reevaluated 1 year later (age 4.5 years), after they had used a CI between 19 and 45 months.
Sixty of the children participated in follow-up assessment at summer research camps in St. Louis, MO at an average age of 10.5 years (range = 9.1–12.7 years), and these children made up the sample included in the current investigation (see Geers & Nicholas, 2013, for more detailed description of recruiting and data collection camps). The sample was broadly distributed geographically, and expenses associated with camp attendance were covered for the family. School grades completed at the most recent assessment were: third grade (25%), fourth grade (55%), fifth grade (17%), and sixth grade (3%).
The educational setting for the majority of these students changed markedly from age 4.5 years to age 10.5 years. In preschool, 47 of the students (78%) were in a special education setting. By age 10, the majority of the students, 51 of 60 (85%), attended school in a mainstream setting. At the final assessment, all but four students attended school in regular classrooms with hearing age-mates for at least 85% of the full school day. All children continued using speech as their primary communication mode, although one child was rated as using “occasional signs” and moved from an oral to a total communication classroom in second grade.
About half of the sample (n = 29) received a second CI between the ages of 4 and 11 years and used bilateral CIs for an average of 3 years at the final test session. Two of the unilateral CI users continued using a hearing aid in the other ear. In order to examine the effects of speech processor upgrades on language development, processors were rank ordered by generation of technology for analysis, with higher rankings indicating newer technologies (i.e., from the oldest to most recent). Fifty-five of the 60 children received an upgrade to newer available speech processor technology in at least one ear between the test sessions, and 42 of them used the most recent processor available at the final test session. Aided sound-field thresholds were obtained from audiological records just prior to implantation when the children used hearing aids and postimplant at 4 years of age. Aided sound-field detection thresholds were obtained directly from each child at the age 10-years test session using frequency modulated (FM) tones at octave frequencies from 250 to 4000 Hz and an aided pure-tone average (PTA; 0.5, 1, 2 KHz) was calculated.
Preschool Assessment
Language Samples
Each child was video-recorded in a 30-min free play session with a parent at both 3.5 and 4.5 years of age. All intelligible spoken words were transcribed from the entire recording by an experienced teacher of deaf children, with transcription procedures following the format of the Child Language Data Exchange System (MacWhinney, 2000). In situations of questionable intelligibility, the following criteria were applied: same number of syllables, match on at least one vowel, and match on at least one consonant. A second transcriber reviewed each recording with its transcript and made corrections due to omissions or errors. For transcriber reliability checks, fifteen 30-min language samples were independently transcribed in their entirety by the two transcribers, and the degree of correspondence was calculated for each dependent variable (mean correspondence across variables = .97, range = .93–.99). Counting programs of the Child Language Data Exchange System provided estimates of productivity, vocabulary, and morphosyntax. The measures chosen were as follows:
Number of utterances. This measure of productivity was counted across the entire 30-min language sample and can serve to roughly equalize the corpus from which other dependent variables are computed. Utterance segmentation was determined by syntactic cues, prosodic cues, and changes in conversational turn. Mean total utterances ranged from 77 to 462 at age 3.5 years and from 99 to 378 at age 4.5 years.
Number of different root words. This measure of lexical breadth counts the number of unique words produced by the child that contain a single free (root) morpheme, such as look (root of look-s, look-ed, look-ing) as single lexical items, thereby decreasing the chance of over- or underestimating the breadth of a child's base lexicon due to high or low usage of bound morphemes. In order to control for productivity, this measure was computed only from the child's first 100 utterances, however at age 3.5 years, one child produced only 77 and another 96 utterances, and at age 4.5 years, one child produced only 99 utterances. Number of different words has been shown to effectively differentiate between children with language impairment and their TD peers (Watkins, Kelly, Harbers, & Hollis, 1995).
Mean length of utterance in words (MLU-w). This measure is included as a broad estimate of syntactic development. It is based on the entire transcript with exclusion of repetitions, false starts, and abandoned utterances. Although the utility of MLU for aid in diagnosing language impairment is debated, a low MLU may be considered a useful indicator in referred clinical populations (Aram, Morris, & Hall, 1993; Eisenberg, Fersko, & Lundgren, 2001). MLU-w and MLU-morphemes are often nearly perfectly correlated (Parker & Brorson, 2005), and MLU-w was chosen for the sake of efficiency and greater reliability of transcription in this study.
Number of different bound morphemes. A bound morpheme is a grammatical tag or marker that cannot function independently and that is attached to a free morpheme or another bound morpheme. We included word-final inflectional suffixes, such as –s, –es, –'s, –ing, –ed, –er (e.g., bigger); and derivational suffixes, such as –ly, –ist, –er (e.g., painter), –ness, and –ment; as well as contractions, such as –'s (is), –'nt (not), –ll (will), –'re (are), –'m (am), and –'us (us). This measure was calculated on the first 100 utterances.
Speech production. Phoneme production at both 3.5 and 4.5 years of age was assessed from phonetic transcription of language samples. Transcription of naturally occurring rather than elicited production has been used in other longitudinal studies of speech in children with CIs that extend to young ages (Tomblin et al., 2008). The first 100 different words produced by a child were transcribed by speech-language pathology graduate students using the International Phonetic Alphabet, following transcription protocols described by Shriberg and Kwiatkowski (1982). The transcriptions were entered into the Computer Aided Speech and Language Analysis software (Serry & Blamey, 1999) for further analyses. The phonetic transcriptions produced by the participant were entered next. Phonetic inventory and accuracy reports were obtained for each child. Interjudge reliability was determined for 20% of the participants and was found to be 81%. Vowel diversity is the number of different vowel sounds produced at least twice with 50% accuracy. Consonant diversity is the number of different consonant sounds produced at least twice with 50% accuracy.
Standardized Testing
Formal language testing was conducted at age 4.5 years to assess receptive vocabulary and global language development relative to hearing age-mates (see Geers & Nicholas, 2013; Nicholas & Geers, 2007). Children were administered the Peabody Picture Vocabulary Test–III (PPVT-III; Dunn & Dunn, 1997) as a measure of receptive vocabulary and the Preschool Language Scale–Third Edition (PLS-3; Zimmerman, Steiner, & Pond, 2002) for overall language. The PLS-3 provides scores for Auditory Comprehension (receptive language) and Expressive Communication (expressive language). Both tests provide standard scores with a mean of 100 and a standard deviation of 15.
School-Age Assessment
Follow-up testing took place at a mean age of 10.5 years (range = 9.1–12.7 years). The mean test interval was 5.9 years (range = 4.6–8.1 years). The battery included language, cognition, audition, and reading tests (see Geers & Nicholas, 2013). Language tests included the PPVT-III (to maintain a consistent measure from the preschool assessment) and the Clinical Evaluation of Language Fundamentals (CELF-4; Semel, Wiig, & Secord, 2003; provides separate receptive and expressive scales). The Wechsler Intelligence Scale for Children–Fourth Edition (WISC-IV; Wechsler, 2003) assesses cognitive level in relation to hearing age-mates and includes a Perceptual Reasoning Scale (nonverbal) to estimate learning ability independent of language skills and a Verbal Comprehension Scale to assess verbal skills. The gap between the Perceptual Reasoning Quotient (PRQ) and the Verbal Comprehension Quotient (VCQ) estimates the degree to which the child is achieving verbal reasoning skills that are commensurate with his or her nonverbal potential. All standardized tests had a mean of 100 and a standard deviation of 15. The Lexical Neighborhood Test (LNT; Kirk, Pisoni & Osberger, 1995) was administered to assess speech recognition, using prerecorded presentation of two lists of 50 monosyllabic words. Participants were seated approximately 1 m from the loudspeaker at 0° azimuth using their typical hearing device configuration. Stimuli were routed through a Grason Stadler GSI 61 audiometer and sound-field loudspeaker at both soft and loud presentation levels: 50 and 70 dB sound pressure level (SPL). The child was instructed to repeat what he or she heard, and responses were transcribed phonetically. The score represents the percentage of phonemes produced that matched the corresponding phoneme in the target word. Phoneme rather than whole-word scoring minimizes the impact of vocabulary on speech perception scores. Reading level was determined with the Woodcock Reading Mastery Test–Revised (Woodcock, 1998). Two subtest scores were averaged to represent Basic Skills: Word Attack and Word Identification. Two additional subtest scores were averaged to represent Reading Comprehension Skills: Word Comprehension and Passage Comprehension.
Intensity of Educational Intervention
Parents completed a questionnaire describing their child's educational intervention during each grade since preschool. Because the number of grades completed varied, some measures were expressed as proportion of grades completed: (a) age first entered a regular educational program (i.e., mainstreamed), (b) percentage of grades completed in classes with more than 20 students, and (c) percentage of grades completed with individual speech/language therapy.
Ethics Approval
Parental consent and student assent were obtained. The Human Research Protection Offices of Washington University in St. Louis and the University of Texas at Dallas approved the protocols for this study.
Results
Categories of Language Emergence
Children were categorized on the basis of their performance on standardized language tests at 4.5 and 10.5 years of age in relation to age-mates with NH from the normative samples. Normal language was defined as a score at or above −1 SD of the normative mean (i.e., standard score of 85), and language-delayed was defined as a standard score below 85. The distribution of children into normal and language-delayed categories on the PLS-3 at age 4.5 years and the CELF-4 at age 10.5 is summarized in Table 1. Categorization was operationally defined as follows: normal language emergence (NLE) = normal language scores at both ages 4.5 and 10.5 years; late language emergence (LLE) = delayed language scores at age 4.5 but within normal limits at 10.5 years; persistent language delay (PLD) = delayed language scores at both 4.5 and 10.5 years; late-emerging delay (LED) = normal language scores at 4.5 years but delayed language scores at 10.5 years.
Table 1.
Language emergence group classification on the basis of testing at two ages.
| Language delay at 4 years | Language delay at 10 years |
||
|---|---|---|---|
| Yes | No | Total | |
| Yes | 19 (32%) | 22 (36%) | 41 (68%) |
| PLD | LLE | ||
| No | 0 (0%) | 19 (32%) | 19 (32%) |
| LED | NLE | ||
| Total | 19 (32%) | 41 (68%) | 60 (100%) |
Note. PLD = persistent language delay; LLE = late language emergence; LED = late-emerging delay; NLE = normal language emergence.
Participants were fairly equally distributed among the NLE (n = 19), LLE (n = 22), and PLD (n = 19) groups. None of the children exhibited LED. Predicting a child will score within a standard deviation of hearing age-mates in primary grades is fairly certain for those children who score within the normal language range in preschool. We classify this as NLE. However, there is an uncertain prognosis for children exhibiting language delay in preschool; they are about equally likely to catch up with hearing age-mates (LLE) or continue to be delayed (PLD).
Demographic characteristics were compared across the three groups using analysis of variance. The groups did not differ in age at either the preschool (M = 4.5 years for all groups) or school-age (NLE = 10.3, LLE = 10.6, PLD = 10.4) assessments. Mother's education level was similar across groups (NLE = 15.9 years, LLE = 15.3 years, PLD 14.8 years) as was the distribution of female participants (NLE = 42%, LLE = 45%, PLD = 63%). Groups did not differ in area of residence (midwest [19%], northeast [25%], south [28%], or western [28%] states). They did not differ in age at first educational intervention/HA fitting (NLE = 7.8 months, LLE = 12.1 months, PLD = 13.7 months) or aided (HA) thresholds in dB, HL prior to implantation (NLE = 64.4, LLE = 63.5, PLD = 67.3). The groups did not differ in the year at which they first received a CI (M = 2000 in all groups).
Analysis Plan
The extent to which each of the variables of interest differentiates NLE and PLD groups from the LLE group is examined, and the size of the effect is determined using a standardized mean difference (Cohen's d). Standardization uses the difference between group means in the numerator of the equation and the pooled standard deviation in the denominator, thus permitting direct comparison across measures that are scaled differently. Values of d below 0.5 constituted a weak effect, between 0.5 and 0.79 a moderate effect, and 0.8 and above a strong effect (Durlak, 2009). Dichotomous variables are analyzed using odds ratio (OR), a value interpreted relative to 1.00 (equal odds). In addition, 95% confidence intervals are plotted for critical predictor variables to demonstrate the degree of uncertainty associated with the mean difference between groups. Last, related measures of the same domain are combined using principal components analysis, thereby increasing their reliability, and logistic regression analyses are used to determine the extent to which variables contribute independently to group differentiation and the probability of correctly identifying group membership for each contrast.
Predictors of Group Membership
CI Characteristics and Speech Perception
Means, standard deviations, and effect sizes for LLE/PLD and NLE/LLE group comparisons are presented in Table 2. Effect size is expressed as Cohen's d for continuous variables and OR for dichotomous variables. The age at first CI variable strongly influenced placement in the NLE group (M = 18.5 months) compared with the LLE group mean (M = 24.5 months; d= −0.81). However, implant age had almost no effect (d = −0.06) on whether the language delay persisted (PLD) or resolved (LLE). The ear first implanted variable strongly influenced placement in the PLD group. Only 53% of children in the PLD group received their first CI in the right ear compared with 86% of children in the LLE group. The odds of getting a first CI in the right ear were more than 5 times higher in the LLE group as in the PLD group (OR = 5.7). Audibility for speech was measured by CI-aided PTA at mean ages of 4.5 and 10.5 years. Threshold averages decreased (improved) in all three groups as the children got older, but the NLE and LLE groups averaged a 9-dB decrease, more than twice that of the PLD group (4 dB). The size of the effect of CI-aided thresholds on placement in LLE versus PLD groups was small (d = −0.28) at age 4.5 but was quite strong (d = −0.94) by the age 10.5 years test session. Better audibility for speech increased chances of catching up with hearing age-mates in elementary grades. The effect size was small for differentiating LLE and NLE groups. Use of most recent CI technology increased over time as children received processor upgrades and was more common in the NLE and LLE than in the PLD groups. Only 32% of those in the PLD group used most recent technology at age 4.5 years, and 42% did so at age 10 years, much smaller proportions than in the LLE group (59% at 4.5 years and 77% at 10.5 years). The odds of children in the LLE group using more recent technology than the PLD group increased from 3.1 at age 4.5 years to 4.7 at age 10.5 years. Children in the NLE group were 2.5 times more likely to use most recent technology than children in the LLE group. Bilateral CI use occurred for 29 children between the age 4.5 and 10.5 years test sessions, with fewest bilateral users in the PLD group. The odds of receiving a second device were 1.4 times higher in the LLE group compared to the PLD group. The odds of receiving a second device were 2 times more likely in the NLE group than in the LLE group.
Table 2.
Cochlear implant (CI) characteristics of the three language emergence groups.
| Demographic | Score | NLE | SD | LLE | SD | PLD | SD | d / OR LLE vs. PLD a | d / OR NLE vs. LLE a |
|---|---|---|---|---|---|---|---|---|---|
| Age at first implant | Months | 18.5 | 7.4 | 24.5 | 7.5 | 24.9 | 6.8 | −0.06 d | −0.81 d |
| Percentage of right-ear CI | % of group | 78.9 | 86.4 | 52.6 | 5.7 OR | 0.6 OR | |||
| Aided PTA at age 4.5 | dB HL | 26.9 | 3.5 | 29 | 4.4 | 30.6 | 6.9 | −0.28 d | −0.53 d |
| Aided PTA at age 10.5 | dB HL | 18 | 5.6 | 20.1 | 5 | 26.6 | 8.5 | −0.94 d | −0.40 d |
| % Most recent technology age: 4.5 | % of group | 78.9 | 59.1 | 31.6 | 3.1 OR | 2.6 OR | |||
| % Most recent technology age: 10.5 | % of group | 89.5 | 77.3 | 42.1 | 4.7 OR | 2.5 OR | |||
| % Bilateral CI use at age 10.5 | % of group | 63.2 | 45.5 | 36.8 | 1.4 OR | 2.1 OR | |||
| Duration bilateral CI use at 10.5 | Years | 2.8 | 2.2 | 3.1 | 1.8 | 2.0 | 1.2 | 0.72 d | −0.15 d |
| LNT phoneme scores at 50 dB SPL | Percent | 79.8 | 14.6 | 75.7 | 12.8 | 44.8 | 31.5 | 1.29 d | 0.30 d |
| LNT phoneme scores at 70 dB SPL | Percent | 94.0 | 4.9 | 90.4 | 6.3 | 78.4 | 21.6 | 0.75 d | 0.64 d |
Note. NLE = normal language emergence; LLE = late language emergence; PLD = persistent language delay; PTA = pure-tone average; LNT = Lexical Neighborhood Test.
Effect size measures: d = Cohen's d; OR = odds ratio.
Duration of bilateral CI use at the age 10.5 years test session was compared for the 29 bilateral users. Greater duration of bilateral experience in the LLE group (3 years, vs. 2 years in the PLD group) had a moderate effect on language emergence (d = 0.7). Analysis of phoneme identification scores on the Lexical Neighborhood Test revealed that perception of soft speech (50 dB) had a strong effect on LLE versus PLD group placement (d = 1.3) and perception of loud speech (70 dB) a moderate effect (d = 0.75).
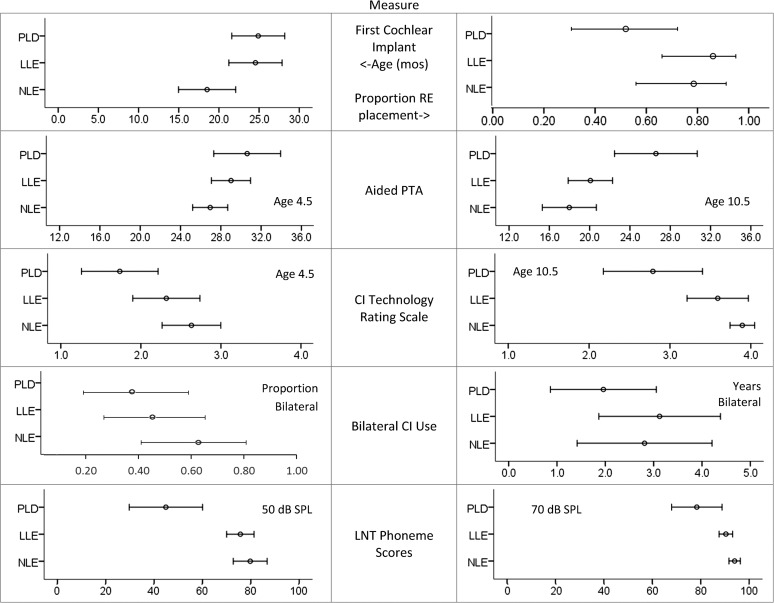
Figure 1 shows means and 95% confidence intervals for CI characteristics for inspection of the degree of overlap across the three language groups. Clearly separate distributions are apparent for age at CI, CI-aided PTA, and LNT phoneme scores at 50 dB. Children receiving a first implant before 24 months of age were most likely to reach normal language levels by age 4 years. Children who reached elementary grades with CI-aided PTA thresholds of 24 dB or higher, used outdated technology, and scored below 60% phoneme recognition on LNT word lists presented at soft levels were likely to experience PLD.
Figure 1.
Mean and 95% confidence intervals for three language emergence groups on cochlear implant (CI) characteristics: Age of first cochlear implantation, proportion of children with first CI in the right ear, aided CI PTA thresholds at ages 4.5 and 10.5 years, CI technology rating scale (1 = least recent to 4 = most recent) at ages 4.5 and 10.5 years, proportion of children using bilateral CIs at age 10.5 years, and the duration of bilateral use, and Lexical Neighborhood Test (LNT) phoneme scores at soft (50 dB) and loud (70 dB) presentation levels.
Conversational Speech and Language in Preschool Ages
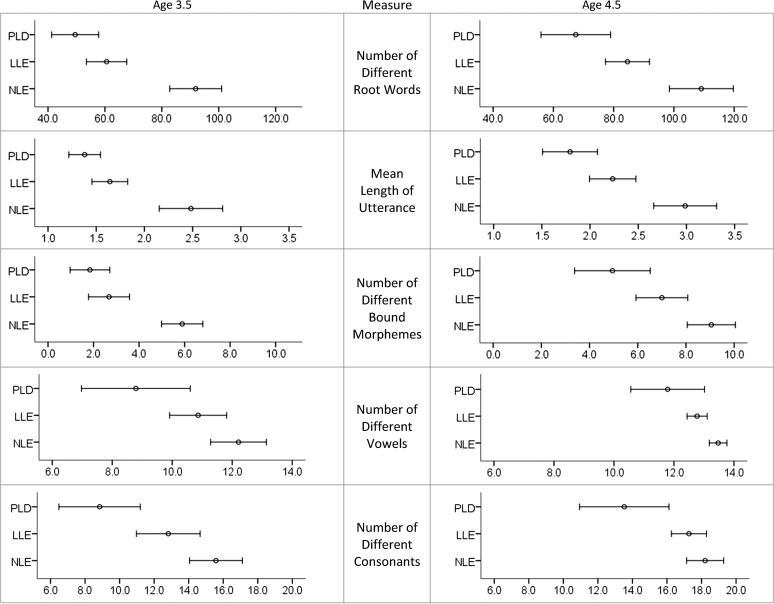
Comparison of lexical, morphosyntactic, and phoneme production measures derived from the language samples collected at 3.5 and 4.5 years of age was undertaken to identify specific markers in early spoken communication that might facilitate early detection of PLD. Table 3 summarizes means and effect sizes for discriminating language-emergence groups by speech and language measures. Although performance improved over time for all three groups, similar effects were obtained from independently collected and transcribed conversational samples collected 1 year apart. Comparison of language sample scores for the PLD and LLE groups suggests that the later acceleration in language that occurs for the LLE group is apparent in a linguistic advantage over the PLD group at 3 and 4 years of age, with moderate-to-strong effect sizes (d = 0.47–0.92). Children with PLD produced fewer different words, shorter utterances, fewer different bound morphemes, and a smaller phonemic repertoire. Comparison of the LLE and NLE groups resulted in strong effect sizes (d = 0.65–1.79), even at age 3.5 years, indicating that the language advantage of the NLE group was evident at least 1 year prior to formal testing at age 4.5 years. Group means and 95% confidence intervals are plotted in Figure 2. The small degree of overlap between confidence intervals for the PLD and LLE groups at the 4.5 years test age indicates that children who had MLUs below 2.0, used fewer than six different bound morphemes, and used fewer than 16 different consonant sounds were very likely to exhibit PLD into the elementary grades.
Table 3.
Preschool speech and language measures for each language-emergence group, by age at test.
| Characteristic | Score | NLE |
LLE |
PLD |
Cohen's d
|
||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | LLE vs. PLD | NLE vs. LLE | ||
| Age 3.5 | |||||||||
| Root words | # Diff | 91.9 | 18.9 | 60.6 | 15.9 | 49.5 | 17.4 | 0.67 | 1.79 |
| Utterance length | MLU | 2.5 | 0.7 | 1.6 | 0.4 | 1.4 | 0.3 | 0.57 | 1.58 |
| Bound morphemes | # Diff | 5.9 | 1.9 | 2.7 | 2.0 | 1.8 | 1.8 | 0.47 | 1.64 |
| Vowels | # Diff | 12.2 | 1.9 | 10.9 | 2.1 | 8.8 | 3.8 | 0.68 | 0.65 |
| Consonants | # Diff | 15.6 | 3.2 | 12.8 | 4.2 | 8.8 | 4.9 | 0.88 | 0.75 |
| Age 4.5 | |||||||||
| Root words | # Diff | 109.1 | 22.0 | 84.6 | 16.4 | 67.4 | 24.0 | 0.84 | 1.26 |
| Utterance length | MLU | 3.0 | 0.7 | 2.2 | 0.5 | 1.8 | 0.6 | 0.72 | 1.32 |
| Bound morphemes | # Diff | 9.1 | 2.1 | 7.0 | 2.4 | 5.0 | 3.3 | 0.69 | 0.93 |
| Vowels | # Diff | 13.5 | 0.6 | 12.8 | 0.8 | 11.8 | 2.6 | 0.52 | 0.99 |
| Consonants | # Diff | 18.2 | 2.2 | 17.3 | 2.3 | 13.5 | 5.4 | 0.92 | 0.40 |
Note. NLE = normal language emergence; LLE = late language emergence; PLD = persistent language delay; Diff = difference; MLU = mean length of utterance.
Figure 2.
Mean and 95% confidence intervals for three language emergence groups on speech and language counts made from conversational language samples at 3.5 (left column) and 4.5 (right column) years of age: Number of different root words, MLU-w, number of different bound morphemes, number of different vowels, and number of different consonants.
Standardized Language Testing
Results of testing at ages 4.5 and 10.5 years are summarized in Table 4. Although LLE and PLD groups were initially formed because overall PLS language scores at age 4.5 were more than 1 SD below the normative mean for both groups, the LLE group exhibited a strong advantage in receptive language (PPVT d = 1.29, PLS-R d = 0.95) and a moderate advantage in expressive language (PLS-E, d = 0.66) over the PLD group during preschool. All three groups improved their language performance relative to age-mates with NH between 4.5 and 10.5 years of age, but the PLD group gained an average of only 6.8 standard score points across the three language measures over the intertest interval compared with a gain of 19.5 points in the LLE group. Figure 3 shows means and 95% confidence intervals for the NLE, LLE, and PLD groups. The separation of PLD/LLE distributions at age 4.5 years suggests that PLD may be identified early for children with receptive language standard scores more than 2 SD below the normative mean when they are 4.5 years old.
Table 4.
Standardized test results for language, cognition, and reading, at two test ages.
| Characteristic | Score | NLE | SD | LLE | SD | PLD | SD | Cohen's d
|
|
|---|---|---|---|---|---|---|---|---|---|
| LLE vs. PLD | NLE vs. LLE | ||||||||
| Age 4.5: Language | |||||||||
| PLS, Receptive | Standard | 103.7 | 9.9 | 77.8 | 9.4 | 69.5 | 15.1 | 0.95 | 2.68 |
| PLS, Expressive | Standard | 100.8 | 13.1 | 64.6 | 9.0 | 58.7 | 8.8 | 0.66 | 3.22 |
| PPVT | Standard | 101.5 | 7.8 | 84.0 | 9.7 | 65.7 | 17.5 | 1.29 | 1.99 |
| Age 10.5: Language | |||||||||
| CELF, Receptive | Standard | 104.0 | 13.8 | 89.2 | 9.4 | 71.8 | 10.5 | 1.75 | 1.25 |
| CELF, Expressive | Standard | 110.4 | 11.4 | 97.0 | 8.2 | 69.3 | 14.8 | 2.32 | 1.35 |
| PPVT | Standard | 114.6 | 14.1 | 98.6 | 15.0 | 73.1 | 14.1 | 1.75 | 1.10 |
| Age 10.5: Cognition/Reading | |||||||||
| WISC, PRQ | Quotient | 110.0 | 10.0 | 104.0 | 12.0 | 102.0 | 15.0 | 0.15 | 0.54 |
| WISC, VCQ | Quotient | 109.0 | 11.0 | 99.0 | 14.0 | 78.0 | 15.0 | 1.45 | 0.79 |
| WISC Gap | PRQ – VCQ | 1.0 | 9.8 | 5.0 | 17.4 | 24.0 | 13.0 | −1.24 | −0.28 |
| Basic Reading Skills | Quotient | 122.9 | 22.7 | 100.4 | 14.3 | 90.5 | 17.7 | 0.62 | 1.19 |
| Reading Comprehension | Quotient | 121.4 | 20.1 | 101.6 | 13.1 | 84.1 | 13.0 | 1.34 | 1.17 |
Note. NLE = normal language emergence; LLE = late language emergence; PLD = persistent language delay; PLS = Preschool Language Scale–Third Edition; PPVT = Peabody Picture Vocabulary Test–III; CELF = Clinical Evaluation of Language Fundamentals–Fourth Edition; WISC = Wechsler Intelligence Scale for Children–Fourth Edition; PRQ = Perceptual Reasoning Quotient; VCQ = Verbal Comprehension Quotient.
Figure 3.
Means and 95% confidence intervals for standardized language tests administered at 4.5 (left column) and 10.5 (right column) years of age. Peabody Picture Vocabulary Test (both test ages), Preschool Language Scale: Receptive and Expressive scales (at age 4.5 years), Clinical Evaluation of Language Function: Receptive and Expressive scales (at age 10.5 years).
Cognition and Reading
At the age 10.5 years test session, cognitive level was measured on the WISC-IV and reading skills on the Woodcock Reading Mastery Test–Revised. The effect size of PRQ (nonverbal intelligence) is very small for differentiating PLD from LLE groups (d = 0.1). There is a moderate tendency (d = 0.5) for children in the NLE group to achieve PRQs that are higher than either of the other groups. Their mean score (110) is also more than 0.5 SD above the average quotient of the normative sample (100). The VCQ on the WISC-IV reflects verbal achievement in relation to hearing age-mates, and a strong effect for language group is apparent (LLE vs. PLD d = 1.45 and NLE vs. LLE d = 0.79). The size of the gap between PRQ and VCQ can be used to compare verbal achievement with nonverbal aptitude, as an index of the degree to which a child's verbal skills approximate his or her potential. Very small average gaps are observed in both the LLE (M = 5) and NLE (M = 1) groups, compared with a 24-point gap for the PLD group. This result indicates that by reaching normal language levels in primary grades, the LLE and NLE groups achieved verbal comprehension at or very close to their potential, whereas children in the PLD group scored far below their nonverbal potential in verbal comprehension skill.
Reading results are considered separately for basic skills (phonological skills including word attack and word identification) and comprehension (word recognition and paragraph comprehension). Children in all three groups scored within or above 1 SD of the normative range (i.e., 85–115) on basic reading skills (M = 123 for NLE group, 100 for LLE group, and 90 for PLD group), and the effect size for differences between the LLE and PLD group means was moderate (d = 0.62). However, the PLD group comprehension mean of 84 was more than 1 SD below the normative mean, which resulted in a large effect size (d = 1.3) when compared with the LLE group mean score of 102.
Educational Intensity
It was predicted that children with preschool language delay would require longer placement in special education and increased use of special services once they entered mainstream classrooms. Children in the LLE group entered regular classes at a median of first grade compared with kindergarten in the NLE group, resulting in a strong effect (d = –0. 89). Although the PLD group entered the mainstream, on average, in second grade, later mainstreaming did not strongly differentiate them from the LLE group (d = –0.5). Next, we examined the extent to which mainstreaming took place in small classes and with added individual therapy. On average, the NLE group spent 59% of grades completed in large classes, which was similar to the 51% observed in the LLE group (d = 0.17). The PLD group, on the other hand, attended large classes for only 29% of grades completed, a moderate effect when compared with the LLE group (d = 0.54). There was little difference among the groups in the amount of individual therapy, itinerant teacher support, or resource room help provided. Overall, there was a tendency for children with more severe and persistent language delays to enter the mainstream later and with smaller class sizes, but not to receive substantially more special services in the regular classroom than children with no delays or resolving delays.
Multivariate Analysis
Multinomial logistic regression analysis was used to calculate expected language group membership from a set of seven participant characteristics. Variables were entered in a hierarchical fashion, roughly in the order of presumed chronological impact, to determine their independent successive contribution to language progress.
Intelligence: The WISC PRQ score was entered in the analysis first, to control for effects of learning ability on language emergence. Cognitive ability is assumed to be relatively stable over the lifespan. To the extent that higher nonverbal intelligence gave children in the NLE group an advantage over LLE and PLD groups, this advantage was controlled before examining other effects.
Age at First CI: This variable indicates the point at which auditory input using electrical stimulation was introduced.
Ear first implanted: This dichotomous variable indicates which children received their first CI in the right ear.
Preschool speech and language factor: This variable was created through principal components analysis of five measures derived from the language sample collected at two points in time: 3.5 and 4.5 years of age. The 10 measures listed in Table 3 loaded on a single factor, with loadings ranging from .77 to .88 and accounting for 69% of common variance.
Bilateral CI use: This variable represents whether or not the child received a second CI between the age 4.5 and 10.5 years test sessions.
CI benefit factor: This factor score was created through principal components analysis of CI-aided thresholds, generation of speech processor technology used, and LNT scores at 50 and 70 dB SPL. Together they loaded on a single factor, with loadings ranging from .71 to .90 and accounting for 63% of common variance.
Education factor: This factor score was created through principal components analysis of age at mainstream placement, percentage of grades in class size > 20, and percentage of grades with individual therapy. Together these loaded on a single factor, with loadings ranging from .68 to .83 and accounting for 56% of common variance.
Results of the hierarchical analyses, consisting of regression coefficients and their standard errors as each variable was entered, are summarized in Table 5. For these analyses, assignment to LLE represents the reference group to which both NLE and PLD group assignment is compared. Exponentiating the regression coefficient (B) produces an odds ratio (OR).
Table 5.
Regression Model 1.
| Language Emergence Group | B | SEB | B | SEB | B | SEB | B | SEB | B | SEB | B | SEB |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NLE | ||||||||||||
| Intercept | −5.17 | 3.06 | −1.43 | 3.37 | −0.38 | 3.44 | −1.58 | 3.53 | −1.93 | 3.78 | −1.90 | 3.81 |
| Perceptual Reasoning Quotient | 0.05 | 0.03 | 0.04 | 0.03 | 0.04 | 0.03 | 0.04 | 0.03 | 0.05 | 0.03 | 0.04 | 0.03 |
| Age at Implant | −0.12 | 0.05 | −0.13 | 0.05 | −0.13 | 0.05 | −0.13 | 0.06 | −0.12 | 0.06 | ||
| Ear First CI (0 = Left, 1 = Right) | −1.24 | 0.93 | −1.29 | 0.96 | −1.56 | 1.02 | −1.53 | 1.03 | ||||
| Bilateral Status (0 = No, 1 = Yes) | 0.91 | 0.72 | 0.65 | 0.75 | 0.64 | 0.75 | ||||||
| CI Benefit Factor | 0.89 | 0.66 | 0.87 | 0.67 | ||||||||
| Education Factor | −0.27 | 0.41 | ||||||||||
| PLD | ||||||||||||
| Intercept | 0.75 | 2.53 | 0.64 | 2.92 | 2.28 | 3.14 | 2.59 | 3.27 | 2.49 | 3.51 | 2.26 | 3.61 |
| Perceptual Reasoning Quotient | −0.01 | 0.02 | −0.01 | 0.03 | −0.01 | 0.03 | −0.01 | 0.03 | −0.01 | 0.03 | −0.01 | 0.03 |
| Age at Implant | 0.00 | 0.04 | −0.02 | 0.05 | −0.02 | 0.05 | −0.04 | 0.05 | −0.05 | 0.06 | ||
| Ear First CI (0 = Left, 1 = Right) | −1.79 | 0.79 | −1.78 | 0.80 | −1.88 | 0.91 | −1.82 | 0.93 | ||||
| Bilateral Status (0 = No, 1 = Yes) | −0.31 | 0.68 | 0.62 | 0.82 | 0.57 | 0.83 | ||||||
| CI Benefit Factor | −1.36 | 0.47 | −1.25 | 0.48 | ||||||||
| Education Factor | 0.33 | 0.45 |
Note. Bold text indicates significant predictors at p < .05.
Two sets of regressions were conducted; Model 1 excludes the early speech/language factor and Model 2 includes it. The first model (Table 5) examines the extent to which reaching age-appropriate language level in elementary grades was affected by the chronology of predictor events without regard to early speech and language skills. The second model (Table 6) inserts the early speech and language factor into the hierarchical analysis prior to entering CI and education characteristics occurring between preschool and elementary grades. Significant (p < .05) predictors appear in bold. Beta weights and their standard errors are presented for each predictor. OR values are reported below for predictors reaching statistical significance.
Table 6.
Regression Model 2, with Early Speech/Language Factor added.
| Language emergence group | Step 1 |
Step 2 |
Step 3 |
Step 4 |
Step 5 |
Step 6 |
Step 7 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SEB | B | SEB | B | SEB | B | SEB | B | SEB | B | SEB | B | SEB | |
| NLE | ||||||||||||||
| Intercept | −5.17 | 3.06 | −1.43 | 3.37 | −0.38 | 3.44 | −5.04 | 4.30 | −5.19 | 4.32 | −4.96 | 4.44 | −5.21 | 4.48 |
| Perceptual Reasoning Quotient | 0.05 | 0.03 | 0.04 | 0.03 | 0.04 | 0.03 | 0.02 | 0.03 | 0.02 | 0.03 | 0.02 | 0.04 | 0.02 | 0.04 |
| Age at Implant | −0.12 | 0.05 | −0.13 | 0.05 | 0.02 | 0.07 | 0.02 | 0.07 | 0.01 | 0.07 | 0.02 | 0.07 | ||
| Ear First CI (0 = Left, 1 = Right) | −1.24 | 0.93 | 0.81 | 1.26 | 0.77 | 1.28 | 0.67 | 1.35 | 0.86 | 1.40 | ||||
| Speech and Language Factor | 3.06 | 1.11 | 3.00 | 1.12 | 2.93 | 1.18 | 3.15 | 1.27 | ||||||
| Bilateral Status (0 = No, 1 = Yes) | 0.33 | 0.85 | 0.34 | 0.87 | 0.26 | 0.89 | ||||||||
| CI Benefit Factor | 0.13 | 0.80 | 0.09 | 0.79 | ||||||||||
| Education Factor | 0.24 | 0.51 | ||||||||||||
| PLD | ||||||||||||||
| Intercept | 0.75 | 2.53 | 0.64 | 2.92 | 2.28 | 3.14 | 7.54 | 4.36 | 7.32 | 4.42 | 5.84 | 4.51 | 6.64 | 4.79 |
| Perceptual Reasoning Quotient | −0.01 | 0.02 | −0.01 | 0.03 | −0.01 | 0.03 | −0.03 | 0.03 | −0.03 | 0.03 | −0.02 | 0.03 | −0.03 | 0.03 |
| Age at Implant | 0.00 | 0.04 | −0.02 | 0.05 | −0.13 | 0.07 | −0.13 | 0.07 | −0.11 | 0.08 | −0.12 | 0.08 | ||
| Ear First CI (0 = Left, 1 = Right) | −1.79 | 0.79 | −3.16 | 1.15 | −3.17 | 1.15 | −2.97 | 1.18 | −3.21 | 1.29 | ||||
| Speech and Language Factor | −2.18 | 0.76 | −2.21 | 0.77 | −1.70 | 0.79 | −1.95 | 0.93 | ||||||
| Bilateral Status (0 = No, 1 = Yes) | 0.25 | 0.84 | 0.71 | 0.93 | 0.74 | 0.93 | ||||||||
| CI Benefit Factor | −0.90 | 0.56 | −0.97 | 0.58 | ||||||||||
| Education Factor | −0.29 | 0.53 | ||||||||||||
Note. NLE = normal language emergence; PLD = persistent language delay; LLE = late language emergence. The reference category is: LLE. Exponentiating a regression coefficient (B) produces an odds ratio. Beta weights and their standard errors are presented for each predictor. Bold text indicates significant predictors at p < .05.
Distinguishing NLE from LLE
In the first model (Table 5), the only variable with a significant independent contribution for predicted placement in NLE or LLE groups is age at first CI. For each month increase in age at first CI, the odds of being in the NLE (instead of the LLE) group decreases by a factor of .88. In the second model (Table 6), the age at first CI variable is significant only through Step 4, when the early speech/language factor is added to the model. After this point, the only factor distinguishing NLE from LLE groups is early speech/language skill—which was, after all, the basis for assignment to those groups (OR = 23.2).
Distinguishing PLD from LLE
The variables contributing independently to distinguishing predicted placement in PLD or LLE groups in the first model are ear first implanted and the CI benefit factor score. Children who received their first CI in the left ear and those who received limited auditory benefit for detecting sound and discriminating speech were unlikely to achieve age-appropriate language levels by mid-to-late elementary grades. The odds of being in the PLD group are reduced when the implant is in the right rather than the left ear (OR = .162). The odds of being in the PLD group are also reduced (i.e., multiplied by the OR of .288) with a one-unit (i.e., 1 SD) increase in the CI benefit factor. In Model 2, when the early speech and language factor is added to the analysis, it supersedes the CI factor score in predictive power. The odds of being in the PLD group are reduced (i.e., multiplied by the OR of .14) with a one-unit (i.e., 1 SD) increase in the speech/language factor. Children with low speech/language scores at very young ages were also those who gained less auditory benefit from a CI throughout the duration of the study, thus the suppression of the CI benefit factor score when the speech/language factor score was removed first in the stepwise analysis (OR = .38, which did not differ significantly from 1.0).
Group Classification Probabilities for Specific Predictors
In order to examine the influence of specific predictor variables on group classification, the regression model is used to generate predicted logits (natural log of the odds) for each categorical outcome. Then, those logits are backtransformed to probabilities using standard formulas. In this manner, the probability associated with predicted placement in each of the three categories is determined. Given that the analysis is based on stepwise regression, the probabilities derived are controlled for variables entered earlier in the model.
Observed Versus Expected Group Classification
Results of the multinomial regression analysis allow us to determine for each individual the predicted probability of being in each language emergence group, with classification on the basis of the highest probability. Table 7 compares the number of cases correctly predicted on the basis of the six-step model presented in Table 5 with the observed group membership. The overall correct prediction is 67%; highest for the NLE group (74%) and lowest for the LLE group (59%). Adding early language as a predictor (Table 8) increases the overall correct classification by about 6%. The greatest increase in certainty is observed for the NLE group placement (10% increase) and relatively little increase in prediction is observed for the LLE and PLD groups (4%–5% increase) by adding early language to the model.
Table 7.
Observed versus predicted classification, with early language excluded.
| Observed | Predicted |
|||
|---|---|---|---|---|
| NLE | LLE | PLD | Percent correct | |
| NLE | 14 | 4 | 1 | 73.7 |
| LLE | 3 | 13 | 6 | 59.1 |
| PLD | 3 | 3 | 13 | 68.4 |
| Overall percentage | 33.3 | 35.0 | 31.7 | 66.7 |
Note. NLE = normal language emergence; LLE = late language emergence; PLD = persistent language delay.
Table 8.
Observed versus predicted classification, with early language included.
| Observed | Predicted |
|||
|---|---|---|---|---|
| NLE | LLE | PLD | Percent correct | |
| NLE | 16 | 3 | 0 | 84.2 |
| LLE | 3 | 14 | 5 | 63.6 |
| PLD | 1 | 4 | 14 | 73.3 |
| Overall percentage | 33.3 | 35.0 | 31.7 | 71.7 |
Note. NLE = normal language emergence; LLE = late language emergence; PLD = persistent language delay.
Discussion
Overall, this study was successful in identifying risk factors for PLD for this sample of children with early CIs. Forty-one of the sample of 60 children were language-delayed in preschool, but by mid-to-late elementary grades the same number (LLE, n = 41) scored within 1 SD of hearing peers on standardized tests. Nineteen of these children had reached age-appropriate levels by age 4.5 years, and none of those fell below that threshold as they progressed through elementary grades (NLE). However, another 19 children exhibited PLD throughout the longitudinal study. Fifty-seven of 60 attended regular education classes for some or all of their elementary grades.
The following four hypotheses were examined:
1. Children whose language reaches normal levels very early in life (NLE) most often have early advantages, including higher cognitive ability and younger age at implantation.
This hypothesis was confirmed as evidenced by a moderate effect of WISC-PRQ (Table 4) and a strong effect of age at implantation (Table 2) on normal versus late-emerging language. Although receiving a CI at a younger age was a significant independent predictor of NLE versus LLE groups, it did not differentiate LLE from PLD groups (Table 5).
2. Children with early language delays that eventually resolve will be more likely to have received updated technology and a second CI in between preschool and elementary grades, resulting in better CI-aided thresholds and speech perception scores than children whose language delay persists.
This hypothesis was confirmed (Table 2), showing that odds were 3–4 times greater that children in the LLE group used more recent CI technology compared with those in the PLD group. In addition CI-aided PTA and LNT phoneme scores at age 10.5 years both showed strong effects for discriminating PLD from LLE groups. Speech perception scores at the soft presentation level were particularly sensitive to group differences. Consistent audibility of speech at levels ranging from soft to loud is necessary for young children who are both active and passive listeners and language learners in a variety of auditory environments throughout the day (Bess, Dodd-Murphy, & Parker, 1998; Flexer, 1999). Children often learn new language by overhearing speech in their home or classroom environments. This incidental or casual language acquisition depends on the ability to overhear soft speech in addition to speech at normal conversation level (Ross, 1990). Children with PLD had less access to soft speech than those whose early language delay recovered over time. Regression analysis (Table 5) revealed a significant independent contribution of audition to differentiating PLD from LLE groups. Only a small-to-moderate advantage for receipt of a second CI was observed in the LLE group, and this variable did not contribute independently to language emergence.
3. Children with persistent delay will show possible early signs of language impairment, including a smaller repertoire of lexical, syntactic, morphological, and phonological elements in preschool-aged conversational language when compared with children whose early delays resolve.
Preschool language sample analysis (Table 3) indicates moderate-to-strong effects of lexical, syntactic, and phonological diversity on differentiating LLE from both PLD and NLE groups. Lower language skills were evident in the PLD group as early as 3.5 years of age, with smaller language gains between 3.5 and 4.5 years than the LLE group, foreshadowing slower long-term language development. Furthermore, when the contribution of early conversational language ability to language emergence group placement was examined in logistic regression analysis (Table 8), the later contribution of auditory benefit was suppressed, suggesting that these two variables are highly related and that differentiating their separate contributions is not possible. However, we surmise that the six children with PLD who were misclassified as NLE or LLE when only auditory predictors were included (Table 7) may have a language impairment, which interfered with faster language progress than would be predicted by their auditory skills profile.
4. Long-term detrimental effects of language delay will encompass phonological decoding, reading comprehension, and verbal comprehension.
PLD was strongly associated with lower verbal comprehension and reading comprehension skills at age 10.5 years compared with the LLE group (Table 4). The gap between the nonverbal and verbal quotient scores as measured by the WISC-IV was quite small for children with NLE and LLE, indicating that both groups had achieved verbal comprehension skills that closely approximated their potential. On the other hand, the gap was substantial for those children with PLD, indicating they are far from achieving verbal comprehension skills commensurate with their nonverbal potential. In reading, only moderate differences were observed between PLD and LLE groups on Basic Reading skills (phonological processing/decoding skills), but strong effects on Reading Comprehension (deriving meaning from words, sentences and paragraphs) were observed.
Unanticipated Findings
The PLD groups surprisingly did not differ on many of the characteristics associated with language outcome in predictive studies covering the entire range of language performance in children with CIs (e.g., Geers & Nicholas, 2013). Children with PLD did not differ from children with LLE in preimplant aided hearing, age at first CI, gender, maternal education, or intensity of educational intervention (although they entered the mainstream, on average, one grade later).
A surprising (and unanticipated) factor distinguishing PLD from LLE groups was choice of ear for implantation. The finding that a much larger percentage (47%) of children with PLD had left-ear CIs as compared with LLE (14%) or NLE (21%) adds to a small set of previous reports that examine this factor. An advantage in speech perception outcomes for right-side CIs has been noted for children with unilateral (Henkin et al., 2008) and bilateral (Henkin et al., 2014) implantation. For children, as test age and duration of use increased, the right-side advantage increased (Henkin et al., 2014). Consistent with our findings, research by Niedzielski, Humeniuk, Blaziak, and Gwizda (2006) showed children with right-sided unilateral hearing loss show significantly poorer performance on verbal intelligence measures than those children with left-sided loss, despite equal nonverbal skills.
Conclusions
These results have important implications for surgeons, speech-language pathologists, educators, and audiologists serving young children with CIs. For the surgeon, right-ear placement of the first CI should be preferred over the left unless cochlear anatomy precludes placement at the right ear. This, along with implantation by 18 months, may help to maximize chances of age-appropriate spoken language development. For the speech-language pathologist, the extent of immature speech production and language use during preschool years may foreshadow later language difficulties. In particular, language test scores more than 2 SD delayed relative to the normative mean at age 4 years constitute a significant risk factor for long-term language delay. For the audiologist, encouraging upgraded speech processor technology and working to ensure thresholds of approximately 20 dB HL when programming the device may positively influence future language development. For the educator, recognition of risk factors for PLD may signal increased intensity of language intervention. Whether auditory oral intervention should be supplemented by the addition of sign language for these children remains controversial. Sign language was added for only one of the children in this sample, and this child continued to exhibit PLD. Studies comparing language results for children with and without sign language suggest that change in communication mode from oral to simultaneous communication may not result in resolving language delay (Geers & Sedey, 2011; Nittrouer, 2010).
These findings may be influenced by the nature of the sample choosing to participate, particularly in the follow-up data collection, which required both the child and a parent to travel to St. Louis for several days of testing (all expenses paid). Participating children received early listening and spoken language intervention along with a CI by their third birthday. The mean parental education and income levels were higher than the average for the general American population, and the mean nonverbal intelligence quotient (105) was slightly higher than the normative mean (100). It will be important to replicate these findings with children from more heterogeneous backgrounds, who may better represent the population of children receiving CIs in North America today.
Acknowledgments
This work was funded by National Institute on Deafness and Other Communication Disorders Grant R01DC004168 (Nicholas, PI). Special thanks to Michael Strube, Department of Psychology, Washington University, for aid in statistical analysis and interpretation; Christine Brenner for data preparation and analysis; Sarah Fessenden and Julia Biedenstein for help with data collection and research camp coordination; and to all of the families and programs that participated in this project.
Funding Statement
This work was funded by National Institute on Deafness and Other Communication Disorders Grant R01DC004168 (Nicholas, PI).
References
- Aram D., Morris R., & Hall N. E. (1993). Clinical and research congruence in identifying children with specific language impairment. Journal of Speech and Hearing Research, 36, 580–591. [DOI] [PubMed] [Google Scholar]
- Bess F. H., Dodd-Murphy J., & Parker R. A. (1998). Children with minimal sensorineural hearing loss: Prevalence, educational performance, and functional status. Ear and Hearing, 19, 339–354. [DOI] [PubMed] [Google Scholar]
- Birney D. P., & Sternberg R. J. (2006). Intelligence and cognitive abilities as competencies in development. In Bialystok E. (Ed.), Lifespan cognition: Mechanisms of change (pp. 315–330). New York, NY: Oxford University Press. [Google Scholar]
- Black J., Hickson L., Black B., & Perry C. (2011). Prognostic indicators in pediatric cochlear implant surgery: A systematic literature review. Cochlear Implants International, 12, 67–93. [DOI] [PubMed] [Google Scholar]
- Carlson M. L., Driscoll C. L., Gifford R. H., & McMenomey S. O. (2012). Cochlear implantation: Current and future device options. Otolaryngology Clinics of North America, 45, 221–248. [DOI] [PubMed] [Google Scholar]
- Castellanos I., Kronenberger W., Beer J., Henning S., Colson B., & Pisoni D. (2014). Preschool speech intelligibility and vocabulary skills predict long-term speech and language outcomes following cochlear implantation in early childhood. Cochlear Implants International, 15, 200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L. S. (2006). Effects of stimulus level on the speech perception abilities of children using cochlear implants or digital hearing aids. Ear and Hearing, 27, 493–507. [DOI] [PubMed] [Google Scholar]
- Davidson L. S., Geers A., Blamey P., Tobey E., & Brenner C. (2011). Factors contributing to speech perception scores in long-term pediatric cochlear implant users. Ear and Hearing, 32, 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L. S., Geers A., & Nicholas J. (2014). The effects of audibility and novel word learning ability on vocabulary level in children with cochlear implants. Cochlear Implants International, 15, 211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L. S., Skinner M. W., Holstad B. A., Fears B. T., Richter M. K., Matusofsky M., … Scolli S. (2009). The effect of instantaneous input dynamic range setting on the speech perception of children with the nucleus 24 implant. Ear and Hearing, 30, 340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson P. W., Decker J. A., & Psarros C. E. (2004). Optimizing dynamic range in children using the nucleus cochlear implant. Ear and Hearing, 25, 230–241. [DOI] [PubMed] [Google Scholar]
- Dawson P. W., Vandali A. E., Knight M. R., & Heasman J. M. (2007). Clinical evaluation of expanded input dynamic range in Nucleus cochlear implants. Ear and Hearing, 28, 163–176. [DOI] [PubMed] [Google Scholar]
- Dollaghan C. A., & Campbell T. F. (2009). How well do poor language scores at ages 3 and 4 predict poor language scores at age 6? International Journal of Speech-Language Pathology, 11, 358–365. [Google Scholar]
- Duchesne L., Sutton A., & Bergeron F. (2009). Language achievement in children who received cochlear implants between 1 and 2 years of age: Group trends and individual patterns. Journal of Deaf Studies and Deaf Education, 14, 465–485. [DOI] [PubMed] [Google Scholar]
- Dunn L. M., & Dunn D. M. (1997). The Peabody Picture Vocabulary Test–III. Circle Pines, MN: AGS. [Google Scholar]
- Durlak J. A. (2009). How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology, 34, 917–928. [DOI] [PubMed] [Google Scholar]
- Eisenberg S. L., Fersko T. M., & Lundgren C. (2001). The use of MLU for identifying language impairment in preschool children: A review. American Journal of Speech-Language Pathology, 10, 323–342. [Google Scholar]
- Ellis E., & Thal D. (2008). Early language delay and risk for language impairment. Perspectives on Language Learning and Education, 15, 93–100. [Google Scholar]
- Firszt J. B., Holden L. K., Skinner M. W., Tobey E. A., Peterson A., Gaggi W., … Wackym P. A. (2004). Recognition of speech presented at soft to loud levels by adult cochlear implant recipients of three cochlear implant systems. Ear and Hearing, 25, 375–387. [DOI] [PubMed] [Google Scholar]
- Flexer C. (1999). The importance of hearing and the impact of hearing problems. Facilitating hearing and listening in young children (2nd ed., pp. 1–22). San Diego, CA: Singular. [Google Scholar]
- Fulcher A., Purcell A., Baker E., & Munro N. (2012). Listen up: Children with early identified hearing loss achieve age appropriate speech/language outcomes by 3 years of age. International Journal of Pediatric Otolaryngology, 76, 1785–1794. [DOI] [PubMed] [Google Scholar]
- Geers A. E., Brenner C., & Davidson L. (1999). Speech perception changes in children switching from M-Peak to SPEAK coding strategy. In Waltzman S. B. & Cohen N. L. (Eds.), Cochlear implants (pp. 211). New York, NY: Thieme. [Google Scholar]
- Geers A. E., & Nicholas J. G. (2013). Enduring advantages of early cochlear implantation for spoken language development. Journal of Speech, Language, and Hearing Research, 56, 643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geers A. E., & Sedey A. L. (2011). Language and verbal reasoning skills in adolescents with 10 or more years of cochlear implant experience. Ear and Hearing, 32, 39S–48S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbertson M., & Kamhi A. G. (1995). Novel word learning in children with hearing impairment. Journal of Speech and Hearing Research, 38, 630–642. [DOI] [PubMed] [Google Scholar]
- Hawker K., Ramirez-Inscoe J., Bishop D. V., Twomey T., O'Donoghue G. M., & Moore D. R. (2008). Disproportionate language impairment in children using cochlear implants. Ear and Hearing, 29, 467–471. [DOI] [PubMed] [Google Scholar]
- Henkin Y., Sweat R. T., Roth D. A., Kishon-Rabin L., Shapira Y., Migirov L., … Kaplan-Neeman R. (2014). Evidence for a right cochlear implant advantage in simultaneous bilateral cochlear implantation. Laryngoscope, 124, 1937–1941. [DOI] [PubMed] [Google Scholar]
- Henkin Y., Taitelbaum-Swead R., Hildesheimer M., Migirov L., Kronenberg J., & Kison-Rabin L. (2008). Is there a right cochlear implant advantage? Otology & Neurotology, 29, 489–494. [DOI] [PubMed] [Google Scholar]
- Hess C., Zettler-Greeley C., Godar S., Ellis-Weismer S., & Litovsky R. (2014). The effect of differential listening experience on the development of expressive and receptive language in children with bilateral cochlear implants. Ear and Hearing, 35, 387–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden L. K., Finley C. C., Firszt J. B., Holden T. A., Brenner C., Potts L. G., … Skinner M. W. (2013). Factors affecting open-set word recognition in adults with cochlear implants. Ear and Hearing, 34, 342–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk K. I., Pisoni D. B., & Osberger M. J. (1995). Lexical effects on spoken word recognition by pediatric cochlear implant users. Ear and Hearing, 16, 470–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh J., Dettman S., Dowell R., & Briggs R. (2013). Communication development in children who receive a cochlear implant by 12 months of age. Otology & Neurotology, 34, 443–450. [DOI] [PubMed] [Google Scholar]
- MacWhinney B. (2000). The CHILDES project: Tools for analyzing talk (3rd ed.). Mahwah, NJ: Erlbaum. [Google Scholar]
- Moeller M., Hoover B., Putman C., Arbataitis K., Bohenkamp G., Peterson B., … Stelmachowicz P. (2007). Vocalizations of infants with hearing loss compared with infants with normal hearing: Part II—Transition to words. Ear and Hearing, 28, 628–642. [DOI] [PubMed] [Google Scholar]
- Nicholas J. G., & Geers A. E. (2006). Effects of early auditory experience on the spoken language of deaf children at 3 years of age. Ear and Hearing, 27, 286–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas J. G., & Geers A. E. (2007). Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe to profound hearing loss. Journal of Speech, Language, and Hearing Research, 50, 1048–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzielski A., Humeniuk E., Blaziak P., & Gwizda G. (2006). Intellectual efficiency of children with unilateral hearing loss. International Journal of Pediatric Otolaryngology, 70, 1529–1532. [DOI] [PubMed] [Google Scholar]
- Niparko J. K., Tobey E. A., Thal D. J., Eisenberg L. S., Wang N. Y., Quittner A. L., … CDaCl Investigative Team. (2010). Spoken language development in children following cochlear implantation. Journal of the American Medical Association, 303, 1498–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nittrouer S. (2010). Early development of children with hearing loss. San Diego, CA: Plural. [Google Scholar]
- Nittrouer S., Caldwell A., Lowenstein J. H., Tarr E., & Holloman C. (2012). Emergent literacy in kindergartners with cochlear implants. Ear and Hearing, 33, 683–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien L. C., Valim C., Neault M., Krammerer B., Clark T., Johnston J., … Licameli G. R. (2012). Prognosis tool based on a modified children's implant profile for use in pediatric cochlear implant candidacy evaluation. Annals of Otology, Rhinology, and Laryngology, 12, 73–84. [DOI] [PubMed] [Google Scholar]
- Pankratz M. E., Plante E., Vance R., & Insalaco D. M. (2007). The diagnostic and predictive validity of the Renfrew Bus Story. Language, Speech, and Hearing Services in Schools, 38, 390–399. [DOI] [PubMed] [Google Scholar]
- Parker M. D., & Brorson K. (2005). A comparative study between mean length of utterance in morphemes (MLUm) and mean length of utterance in words (MLUw). First Language, 25, 365–376. [Google Scholar]
- Pharr A. B., Ratner N. B., & Rescorla L. (2000). Syllable structure development of toddlers with expressive specific language impairment. Applied Psycholinguistics, 21, 429–449. [Google Scholar]
- Ramirez-Inscoe J., & Moore D. R. (2011). Processes that influence communicative impairments in deaf children using cochlear implants. Ear and Hearing, 32, 690–698. [DOI] [PubMed] [Google Scholar]
- Reilly S., Tomblin B., Law J., McKean C., Mensah F., Morgan A., … Wake M. (2014). Specific language impairment: A convenient label for whom? International Journal of Communication Disorders, 49, 416–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rescorla L. (2002). Language and reading outcomes to age 9 in late-talking toddlers. Journal of Speech, Language, and Hearing Research, 45, 360–371. [DOI] [PubMed] [Google Scholar]
- Rice M. L. (2003). A unified model of specific and general language delay: Grammatical tense as a clinical marker of unexpected variation. In Levy Y. & Schaeffer J. (Eds.), Language competence across populations: Toward a definition of specific language impairment (pp. 63–95). Mahwah, NJ: Erlbaum. [Google Scholar]
- Rice M. L., Taylor C., & Zubrick S. R. (2008). Language outcomes of 7-year old children with or without a history of late language emergence at 24 months. Journal of Speech, Language, and Hearing Research, 51, 394–407. [DOI] [PubMed] [Google Scholar]
- Ross M. (1990). Implications of delay in detection and management of deafness. Volta Review, 92, 69–79. [Google Scholar]
- Sarant J., Harris D., Bennet L., & Bant S. (2014). Bilateral versus unilateral cochlear implants in children: A study of spoken language outcomes. Ear and Hearing, 35, 396–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarborough H. (2001). Connecting early language and literacy to later reading (dis)abilities: Evidence, theory and practice. In Neuman S. B. & Dickinson D. K. (Eds.), Handbook for research in early literacy (pp. 97–110). New York, NY: Guilford. [Google Scholar]
- Semel E., Wiig E. H., & Secord W. A. (2003). Clinical Evaluation of Language Fundamentals–Fourth Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Serry T. A., & Blamey P. J. (1999). A 4-year investigation into phonetic inventory development in young cochlear implant users. Journal of Speech, Language, and Hearing Research, 42, 141–154. [DOI] [PubMed] [Google Scholar]
- Shriberg L. D., & Kwiatkowski J. (1982). Phonological disorders I: A diagnostic classification system. Journal of Speech and Hearing Disorders, 47, 226–241. [DOI] [PubMed] [Google Scholar]
- Skinner M. W., Arndt P. L., & Staller S. J. (2002). Nucleus 24 advanced encoder conversion study: Performance versus preference. Ear and Hearing, 23, 2S–17S. [DOI] [PubMed] [Google Scholar]
- Skinner M. W., Clark G. M., Whitford L. A., Seligman P. M., Staller S. J., Shipp D. B., … Beiter A. L. (1994). Evaluation of a new spectral peak coding strategy for the Nucleus 22 Channel Cochlear Implant System. American Journal of Otology, 15, 15–27. [PubMed] [Google Scholar]
- Tobey E. A., Thal D., Niparko J., Eisenberg L. S., Quittner A. L., Wang N. Y., & CDaCL Investigative Team. (2013). Influence of implantation age on school-age language performance in pediatric cochlear implant users. International Journal of Audiology, 52, 219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J. B., Peng S.-C., Spencer L. J., & Lu N. (2008). Long-term trajectories in the development of speech sound production in pediatric cochlear implant recipients. Journal of Speech, Language, and Hearing Research, 51, 1353–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins R. V., Kelly D. J., Harbers H. M., & Hollis W. (1995). Measuring children's lexical diversity: Differentiating typical and impaired language learners. Journal of Speech and Hearing Research, 38, 1349–1355. [DOI] [PubMed] [Google Scholar]
- Wechsler D. (2003). Wechsler Intelligence Scale for Children–Fourth Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wilson B. S., & Dorman M. F. (2008). Cochlear implants: Current designs and future possibilities. Journal of Rehabilitation Research Development, 45, 695–730. [DOI] [PubMed] [Google Scholar]
- Woodcock R. W. (1998). Woodcock Reading Mastery Test–Revised. Bloomington, MN: Pearson. [Google Scholar]
- Yoshinaga-Itano C., Baca R., & Sedey A. (2010). Describing the trajectory of language development in the presence of severe-to-profound hearing loss: A closer look at children with cochlear implants versus hearing aids. Otology & Neurotology, 31, 1268–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrana I. M., Pons F., Eadie P., & Ystrom E. (2014). Trajectories of language delay from age 3 to 5: Persistence, recovery and late onset. International Journal of Communication Disorders, 49, 304–316. [DOI] [PubMed] [Google Scholar]
- Zimmerman I. L., Steiner V. G., & Pond R. E. (2002). Preschool Language Scale–Third Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]