Abstract
Aim
The aim of our study was to compare the angiographic changes in 53 nondiabetic patients, 54 type 2 diabetic patients of less than 5 years of duration, 41 patients with 5–10 years of diabetes, and 27 with more than 10 years of diabetic duration.
Methods
In this cross-sectional study, 175 patients, who underwent coronary angiogram for the evaluation of the coronary artery disease (CAD), were recruited. Based on the angiographic findings, syntax score, vessel score, and coronary collaterals grading were analyzed. The biochemical analysis was done by using the auto analyzer.
Results
A significant increase in the mean syntax score (p = 0.019), vessel score (p = 0.007), and coronary collateral grade (p = 0.008) was observed in the patients with 5–10 years of diabetes when compared to those with less than 5 years of diabetic duration. There was no significant difference in the mean syntax score (p = 0.979), vessel score (p = 0.299), and collateral grade (p = 0.842) between the patients with 5–10 years and more than 10 years of diabetes. The difference in the mean syntax score (p = 0.791), vessel score (p = 0.098), and collateral grade (p = 0.661) between the nondiabetic and the patients with less than 5 years of diabetes was not significant.
Conclusion
A significant structural change in the coronary arteries was found among the patients with 5–10 years of diabetes.
Keywords: Type 2 diabetes mellitus, Syntax score, Coronary artery disease
1. Introduction
The prevalence of coronary artery disease (CAD) in diabetes is not only high, but also characterized by severe disease. The prevalence of CAD in the diabetic population ranges from 9.5% to 55%,1, 2 whereas in the general population, it is reported to be 1.6–4.1%.3, 4
There are various conventional risk factors that are known to be accounted for CAD in both diabetics and nondiabetics. But in spite of controlling the conventional risk factors, the burden of CAD is high in the diabetics when compared to the nondiabetic counterparts. When the diabetic patients have the CAD, typically they have more severe disease, with more number of arteries involved, and the higher prevalence of left main stem disease.5, 6, 7, 8
The diabetes being a heterogeneous disease,9 the extent of CAD is not uniform across the diabetic population. A meta-analysis of four studies, namely Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE), United Kingdom Prospective Diabetes Study (UKPDS), and Veterans Affairs Diabetes Trial (VADT), have shown that the macrovascular complications differ with respect to the diabetes duration.10
A large number of analytical scores such as gensini, syntax, extent, and vessel scores have been developed to quantify the severity of the coronary atherosclerosis.11 The severity is said to be a prognostic factor for patients with CAD, which has been proven in several long-term clinical studies.11 The studies using these analytical scores have shown that the severity of CAD is high in diabetes when compared to the nondiabetic population.11 The utility of these scores is not only restricted to know the progression of atherosclerosis but also plays an important role in deciding the mode of coronary interventions.
Since there can be a variation in the CAD outcomes among the diabetic population of different time intervals, we wanted to look for the structural changes in coronary arteries with respect to the different time intervals of type 2 diabetes mellitus. If we are able to identify the CAD changes in a specific time frame of diabetes, it would help us in better management and prevention of the CAD among the diabetic population.
Ideally, longitudinal study has to be carried out in order to find out the structural changes in the coronary arteries with respect to the different time intervals of type 2 diabetes mellitus, but due to the practical inconvenience, a cross-sectional study was designed to compare the severity of the CAD, number of vessels involved in the lesion, coronary collateral grade, and urine microalbumin levels in nondiabetic population, in diabetic population with less than 5 years, in 5–10 years, and more than 10 years of diabetes duration.
2. Methods
This was a cross-sectional study of 175 patients who underwent coronary angiogram for the evaluation of CAD at a tertiary care hospital from February 2013 to December 2013. The patients were recruited in the study after obtaining an informed consent. In order to maintain the homogeneity among the groups and to minimize the effect of confounders, the age of the study population was restricted to 45–65 years. The patients were further grouped into diabetics and nondiabetics based on the diagnostic criteria recommended by the American diabetes association.12 The patients with congenital heart disease, valvular heart disease, and those with significant thyroid, renal dysfunction were excluded from the study. The study was conducted after obtaining the approval from institutional human ethics committee.
The fasting blood sugar, fasting lipid profile and glycated hemoglobin levels and urine microalbumin were measured at the time of admission. The biochemical analysis was done by using the auto analyzer Hitachi P800. The coefficient of variation was <2% and <5% for intra- and inter-batch assay, respectively, in all the cases. The presence of coronary collaterals was visualized and identified after the coronary angiography and it was defined as Rentrop score ≥1.13 The number of vessels involved in the lesion were assessed by vessel score.14 Only those vessels with 70% stenosis or greater reduction in luminal diameter were considered to be significant. The left main artery stenosis was scored as single vessel disease. The number of vessels involved in the lesion ranged from 0 to 3. The severity and the extent of the CAD were assessed by the syntax score,15 which is a web-based algorithm consisting sequential and interactive self-guided questions. The syntax score, vessel score, presence of coronary collaterals and the grading were carried out by a cardiologist, who was blind to other parameters.
2.1. Statistical analysis
The data were represented as mean ± standard deviation. The Analysis of Variance (ANOVA) was performed in order to identify the differences in the mean syntax score, vessel score, coronary collaterals and urine microalbumin between the groups. The post-hoc analysis was done assuming the equality of variances. The least square difference (LSD) post-hoc test was performed to find out the significant differences in the mean syntax score, vessel score, coronary collateral grading, and microalbumin levels between the nondiabetic, diabetes with less than 5 years duration, 5–10 years of diabetes, and more than 10 years of diabetic duration. p value <0.05 was considered to be significant. The data were analyzed using the statistical package for social sciences (SPSS) version 16 (SPSS, Chicago, IL, USA).
3. Results
In a total of 175 subjects who were recruited in this study, 53 were nondiabetics, and 122 were found to be having a history of type 2 diabetes mellitus. Further, based on the duration of diabetes the type 2 diabetic population was further subdivided. Among them, 54 were with less than 5 years, 41 were with 5–10 years, and 27 were with more than 10 years of diabetes duration.
The clinical and angiographic characteristics of the study population are shown in Table 1. The mean age of the study population was 56.47 ± 5.89. The mean syntax score, vessel score, collateral grade, and microalbumin were high in patients with more than 5 years of diabetes compared to less than 5 years of diabetes and nondiabetes as shown in Table 1.
Table 1.
Clinical and angiographic characteristics of study population.
| Nondiabetes (Group 1) N = 53 |
Diabetes with <5 years (Group 2) N = 54 |
5–10 years of Diabetes (Group 3) N = 41 |
Diabetes with >10 years (Group 4) N = 27 |
F | p value | p value trend | |
|---|---|---|---|---|---|---|---|
| Syntax score | 12.28 ± 6.63 | 12.77 ± 8.82 | 17.48 ± 11.09 | 17.42 ± 13.23 | 3.65 | 0.014 | 0.003 |
| Collateral score | 0.35 ± 0.81 | 0.277 ± 0.81 | 0.80 ± 1.10 | 0.85 ± 1.19 | 3.99 | 0.009 | 0.004 |
| Vessel score | 1.32 ± 0.75 | 1.61 ± 0.81 | 2.12 ± 1.00 | 1.89 ± 1.15 | 6.65 | <0.001 | <0.001 |
| Microalbumin | 19.08 ± 30.49 | 36.72 ± 61.91 | 39.55 ± 70.94 | 81.21 ± 136.73 | 4.16 | 0.007 | 0.001 |
The mean diabetic duration was 2.62 ± 1.48 in less than 5 years of diabetes, 8.02 ± 1.73 in 5–10 years of diabetes, and 17.14 ± 3.99 in more than 10 years of diabetes. Among overall 175 subjects, 80 (46%) of them were found to be having the history of hypertension. Among the 53 nondiabetics, 17 (32.1%) of them had hypertension. The presence of hypertension was seen in 29 (52.8%) out of 54 with less than 5 years of diabetes, 22 (53.7%) out of 41 with 5–10 years, and 13 (48.1%) out of 27 with more than 10 years of diabetic duration. The biochemical characteristics of the study population are shown in Table 2.
Table 2.
Biochemical characteristics of study population.
| Nondiabetes (Group 1) N = 53 |
Diabetes with <5 years (Group 2) N = 54 |
5–10 years of diabetes (Group 3) N = 41 |
Diabetes with >10 years (Group 4) N = 27 |
|
|---|---|---|---|---|
| Fasting blood sugar | 98.71 ± 7.85 | 168.77 ± 52.73 | 194.80 ± 60.51 | 203.07 ± 64.96 |
| TC-HDL ratio | 4.39 ± 1.24 | 4.48 ± 1.67 | 4.25 ± 1.57 | 4.05 ± 1.43 |
| LDL | 119.82 ± 44.87 | 103.24 ± 49.82 | 89.43 ± 36.59 | 94.87 ± 42.28 |
| Triglycerides | 111.52 ± 52.65 | 148.47 ± 77.16 | 151.21 ± 91.44 | 137.07 ± 55.91 |
| HbA1C | 5.67 ± 0.37 | 8.29 ± 1.95 | 9.47 ± 1.83 | 9.39 ± 1.36 |
TC-HDL ratio, total cholesterol-high density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol; HbA1c, glycated hemoglobin.
One-way ANOVA showed a significant difference between the groups with respect to syntax score (p = 0.014), coronary collateral grade (p = 0.009), urine microalbumin (p = 0.007), and vessel score (p < 0.001). Further post-hoc analysis with LSD showed a significance difference in the mean syntax score, collateral grade, vessel score, and urine microalbumin within the groups.
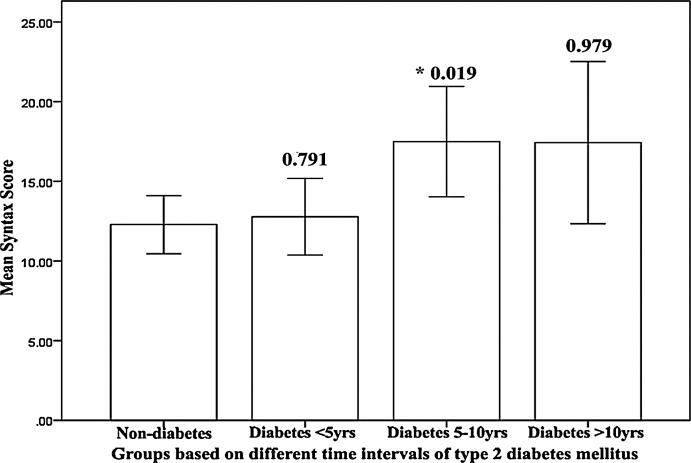
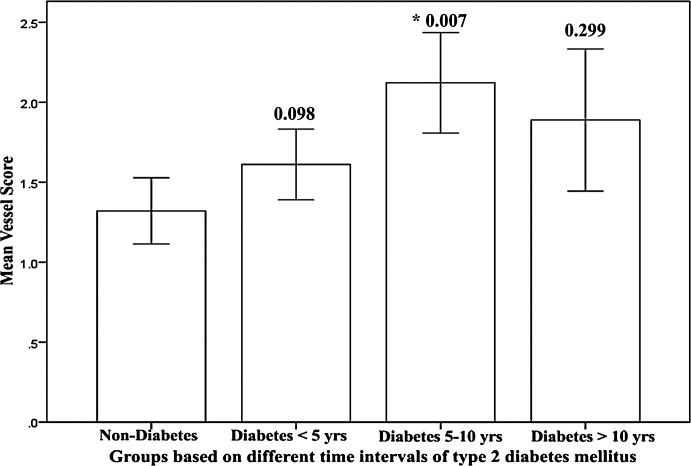
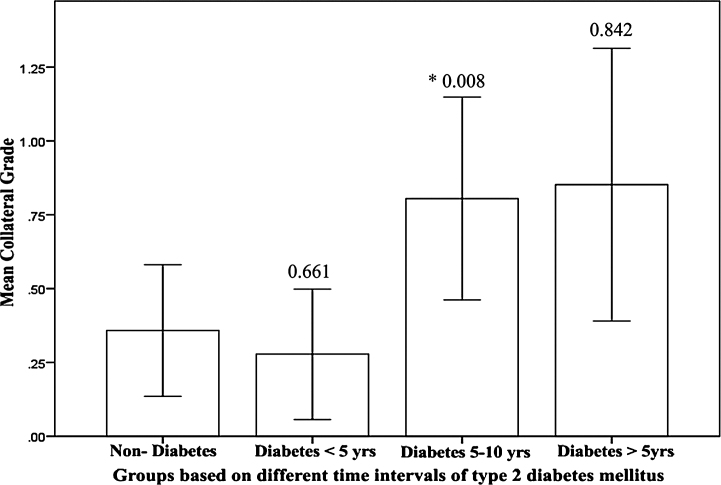
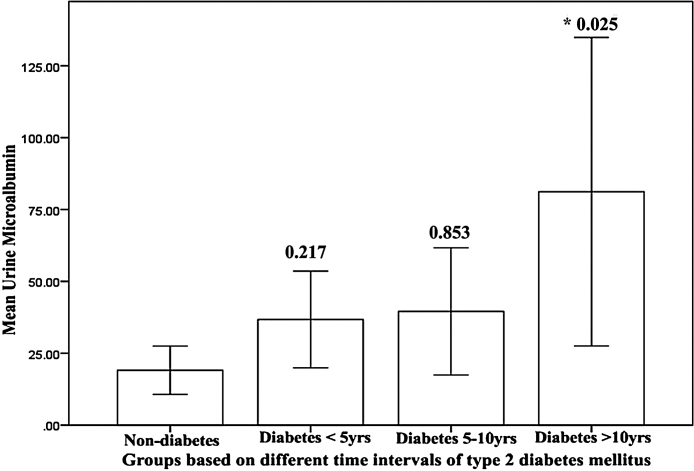
A significant difference with respect to syntax score (p = 0.019) (Fig. 1), vessel score (p = 0.007) (Fig. 2), and collateral grade (p = 0.008) (Fig. 3) was observed between less than 5 years of type 2 diabetes mellitus and 5–10 years of type 2 diabetes mellitus. A significant difference in urine microalbumin was observed only in more than 10 years of diabetes mellitus (p = 0.025) (Fig. 4) when compared with 5–10 years of diabetes mellitus. There was no significant difference in mean syntax score (p = 0.979) (Fig. 1), vessel score (p = 0.299) (Fig. 2), and collateral grade (p = 0.842) (Fig. 3) between 5 and 10 years of type 2 diabetes mellitus and more than 10 years of type 2 diabetes mellitus. There was no significant difference observed in the mean syntax score (p = 0.791) (Fig. 1), vessel score (p = 0.098) (Fig. 2), collateral grade (p = 0.661) (Fig. 3), and urine microalbumin (p = 0.217) (Fig. 4) between nondiabetics and less than 5 years of type 2 diabetes mellitus.
Fig. 1.
Graph showing the difference in mean syntax score between nondiabetes and different time intervals of type 2 diabetes mellitus. *Represents the mean difference is significant at the level of 0.05 with in the groups.
Fig. 2.
Graph showing the difference in mean vessel score between nondiabetes and different time intervals of type 2 diabetes mellitus. *Represents the mean difference is significant at the level of 0.05 with in the groups.
Fig. 3.
Graph showing the difference in mean collateral grade between nondiabetes and different time intervals of type 2 diabetes mellitus. *Represents the mean difference is significant at the level of 0.05 with in the groups.
Fig. 4.
Graph showing the difference in mean urine microalbumin between nondiabetes and different time intervals of type 2 diabetes mellitus. *Represents the mean difference is significant at the level of 0.05 with in the groups.
4. Discussion
In the present study, we compared the angiographic patterns of the coronary artery disease in the nondiabetics, the diabetics with less than 5 years, 5–10 years, and more than 10 years of duration. We noticed the significant structural changes in the coronary arteries in the patients with more than 5 years of type 2 diabetes mellitus.
The profile and complications of the CAD are not uniform among the diabetic population. The studies have shown that the spectra of the CAD differ with respect to the different time intervals of type 2 diabetes mellitus.10 Even in the United Kingdom Prospective Diabetes study risk engine, events less than 4 years were not considered while forming the risk score.16
Earlier studies suggested that the diabetic patients had poor collaterals formation17; however, later studies have shown that collateral formation is independent of diabetes mellitus and depends on the degree of the coronary artery stenosis.18 In our study, we observed that the presence of coronary collaterals is directly proportional to the severity of the CAD. Thus, the presence of collaterals was seen only in more than 5 years of diabetes as syntax score was high in this group compared to nondiabetes and less than 5 years of diabetes.
In the current study, a significant increase in the mean syntax score, vessel score, and coronary collateral grade was observed between 5 and 10 years of diabetic duration when compared to less than 5 years of diabetes, whereas the difference in the mean syntax score, vessel score, and coronary collateral grade both in the nondiabetics and less than 5 years of diabetes, 5–10 years, and more than 10 years of diabetes was not significant. The observation from the present study indicates that the coronary profile between the nondiabetic group and the less than 5 years of diabetes could be similar and a chronic severe structural narrowing of coronary artery takes place in 5–10 years of type 2 diabetes mellitus. Beyond 10 years, we visually noticed a plateau trend with no further morphological changes in the coronary arteries.
In the present study, a significant difference in the urine microalbumin is observed in more than 10 years of diabetes. Even though the microvascular changes are set in at initial stages of diabetes, their progression is significant only after10 years as pointed by our result. But the macrovascular changes are time-dependent, getting established between 5 and 10 years of diabetes. Our study also shows that there is no significant correlation between the urine microalbumin and the syntax score (r = 0.11, p = 0.125), vessel score (r = 0.10, p = 0.143), and collateral grading (r = 0.15, p = 0.095).
The prevalence of microvascular complications increases with the duration of the diabetes.19 A recent study has showed that the incidence of microvascular outcomes is higher after 10 years of type 2 diabetes mellitus and keeps on progressing, whereas the cardiovascular complications seem to be appearing before 10 years of diabetes.20 Type 2 diabetes mellitus with more than 5 years of duration have quantitative and qualitative, severe vascular disease compared to less than 5 years of diabetes. This raises the interesting possibility of insulin resistance in generation of macrovascular complications in type 2 diabetes mellitus. Hyper insulinemia brings about both functional and structural changes in the blood vessels. Functional changes are mediated through nitric oxide by receptor-mediated resistance and maintain the vasodilatation. But the structural changes occur by proatherogenic response mediated by MAP kinase pathway, which is not affected by IR. The continuous action of hyper insulin through the MAP kinase pathway results in a significant structural change over a period of time.21 The peak effect of hyper insulinemia and insulin resistance probably appears from 4 to 5 years of diabetes mellitus and thus resulting in increased severity of the CAD between five and 10 years of diabetes.
Our study confirms that the extent and the degree of the CAD are similar both in nondiabetics and diabetes with less than 5 years. They are often present with discrete lesions, less severe disease, and involvement of single vessel. However, the structural changes in the coronary arteries were observed in more than 5 years of diabetes with diffused, long segment and multi vessel stenosis, a characteristic feature of a typical diabetic coronary artery disease. It is likely that most of the patients with type 2 diabetes mellitus with less than 5 years of duration might be suitable candidates for angioplasty, whereas candidates with more than 5 years of diabetes may be suitable for coronary artery bypass graft (CABG).
The microvascular benefits can be seen even in the longer duration of diabetes but macrovascular benefits are restricted to the initial 5 years of type 2 diabetes mellitus. Thus, the potential window of opportunity for modifying the macrovascular complications is restricted to 0–5 years because beyond 5 years the severe irreversible structural modifications are observed.
Even the previous UKPDS studies have shown that intense therapeutic interventions have reduced the macrovascular complications in less than 5 years of diabetes.5 Thus, in general, the diabetic population intense therapeutic interventions are to be considered within 5 years to reduce the cardiovascular complications.
Individual variations are seen in diabetes complications but our study showed that the variations with respect to the specific time intervals need to be considered. There appears to be a threshold period of 5–10 years, beyond which the CAD appears.
The limitation of the study is the cross-sectional design. The coronary collaterals have been assessed by angiographic images. Further classification of patients based on major adverse cardiac events might give us a better insight to compare the coronary patterns between the different groups.
5. Conclusion
Based on the limitations, the study highlights that the structural changes in the coronary arteries have been observed in more than 5 years of diabetes. The coronary patterns are similar among the nondiabetics and in those with less than 5 years of diabetes. Similarly, the coronary profile between 5 and 10 years and more than 10 years of diabetes is same. This emphasizes that the irreversible cardiovascular damage has already occurred between 5 and 10 years of diabetes and there is no scope for interventions beyond 10 years. Thus, there is a need to target the intense therapeutic intervention within 5 years of type 2 diabetes mellitus.
Conflicts of interest
The authors have none to declare.
Acknowledgements
The authors thank all the patients and the hospital staff members for their co-operation during the study. We also acknowledge Mr Mohammed Ameen and Mr Ganesh P, Cath lab technologists for their assistance in angiographic findings.
References
- 1.Bryfogle J.W., Bradley R.F. The vascular complications of diabetes mellitus. Diabetes. 1957;6:159–167. doi: 10.2337/diab.6.2.159. [DOI] [PubMed] [Google Scholar]
- 2.Liebow I.M., Newill V.A., Oseasolin R. Incidence of ischemic heart disease in a group of diabetic women. Am J Med Sci. 1964;248:403–407. doi: 10.1097/00000441-196410000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Epstein F.H., Ostrander L.D., Jr., Johnson B.C. Epidemiological studies of cardiovascular disease in a total community: Tecumseh, Michigan. Ann Intern Med. 1965;62:1170–1187. doi: 10.7326/0003-4819-62-6-1170. [DOI] [PubMed] [Google Scholar]
- 4.Kannel W.B., Dawber T.R., Kagan A., Revotskie N., Stokes J. Factors of risk in the development of coronary heart disease: six-year follow-up experience: the Framingham Study. Ann Intern Med. 1961;55:3–50. doi: 10.7326/0003-4819-55-1-33. [DOI] [PubMed] [Google Scholar]
- 5.Arad Y., Newstein D., Cadet F., Roth M., Guerci A.D. Association of multiple risk factors and insulin resistance with increased prevalence of asymptomatic coronary artery disease by an electron-beam computed tomographic study. Arterioscler Thromb Vasc Biol. 2001;21:2051–2058. doi: 10.1161/hq1201.100257. [DOI] [PubMed] [Google Scholar]
- 6.Natali A., Vichi S., Landi P., Severi S., Abbate A.L., Ferrannini E. Coronary atherosclerosis in Type II diabetes: angiographic findings and clinical outcome. Diabetologia. 2000:632–641. doi: 10.1007/s001250051352. [DOI] [PubMed] [Google Scholar]
- 7.Moise A., Théroux P., Taeymans Y. Clinical and angiographic factors associated with coronary artery disease progression of coronary artery disease. J Am Coll Cardiol. 1984;3:659–667. doi: 10.1016/s0735-1097(84)80240-5. [DOI] [PubMed] [Google Scholar]
- 8.Dortimer A.C., Shenoy P.N., Shiroff R.A. Diffuse coronary artery disease in diabetic patients: fact or fiction? Circulation. 1978;57:133–136. doi: 10.1161/01.cir.57.1.133. [DOI] [PubMed] [Google Scholar]
- 9.Tuomi T., Santoro N., Caprio S., Cai M., Weng J., Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet. 2013;6736:1–11. doi: 10.1016/S0140-6736(13)62219-9. [DOI] [PubMed] [Google Scholar]
- 10.Turnbull F.M., Abraira C., Anderson R.J. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009;52:2288–2298. doi: 10.1007/s00125-009-1470-0. [DOI] [PubMed] [Google Scholar]
- 11.Sponder M., Fritzer-Szekeres M., Marculescu R., Litschauer B., Strametz-Juranek J. A new coronary artery disease grading system correlates with numerous routine parameters that were associated with atherosclerosis: a grading system for coronary artery disease severity. Vasc Health Risk Manag. 2014;10:641–647. doi: 10.2147/VHRM.S68919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peter Rentrop K., Cohen M., Blanke H., Phillips R.A. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985;5:587–592. doi: 10.1016/s0735-1097(85)80380-6. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan D.R., Marwick T.H., Freedman S.B. A new method of scoring coronary angiograms to reflect extent of coronary atherosclerosis and improve correlation with major risk factors. Am Heart J. 1990;119:1262–1267. doi: 10.1016/s0002-8703(05)80173-5. [DOI] [PubMed] [Google Scholar]
- 15.Sianos G., Morel M.-A., Kappetein A.P. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219–227. [PubMed] [Google Scholar]
- 16.Stevens R.J., Kothari V., Adler I., Stratton I.M. The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56) Clin Sci. 2001;101:671–679. [PubMed] [Google Scholar]
- 17.Abaci A., Oguzhan A., Kahraman S. Effect of diabetes mellitus on formation of coronary collateral vessels. Circulation. 1999;99:239–242. doi: 10.1161/01.cir.99.17.2239. [DOI] [PubMed] [Google Scholar]
- 18.Melidonis A., Tournis S., Kouvaras G. Comparison of coronary collateral circulation in diabetic and nondiabetic patients suffering from coronary artery disease. Clin Cardiol. 1999;22:465–471. doi: 10.1002/clc.4960220706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Kidney Foundation KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am J Kidney Dis. 2007;49:S1–S180. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Huang E.S., Laiteerapong N., Liu J.Y., John P.M., Moffet H.H., Karter A.J. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014;174:251–258. doi: 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mather K.J., Steinberg H.O., Baron A.D. Insulin resistance in the vasculature. J Clin Invest. 2013;123:2013–2014. doi: 10.1172/JCI67166. [DOI] [PMC free article] [PubMed] [Google Scholar]