Abstract
HIV remains a significant public health problem among men who have sex with men (MSM). MSM comprise 2% of the U.S. population, but constitute 56% of persons living with HIV. Mobile health technology is a promising tool for HIV prevention. The purpose of this study was to identify the desired content, features and functions of a mobile application (app) for HIV prevention in high-risk MSM. We conducted five focus group sessions with 33 MSM. Focus group recordings were transcribed and coded using themes informed by the information-motivation-behavioral (IMB) skills model. Participants identified information needs related to HIV prevention: HIV testing and prophylaxis distribution centers, support groups/peers, and HIV/STI disease/treatment information. Areas of motivation to target for the app included: attitudes and intentions. Participants identified behavioral skills to address with an app: using condoms correctly, negotiating safer sex, recognizing signs of HIV/STI. Findings from this work provide insight into the desired content of a mobile app for HIV prevention in high-risk MSM.
HIV infection remains a significant public health problem especially among men who have sex with men (MSM). Current estimates suggest that MSM account for about 2% of the U.S. population, but constitute 56% of persons living with a HIV (Centers for Disease Control and Prevention [CDC], 2014). Although the overall estimated number of new HIV infections in the U.S. remained stable from 2008 to 2010, HIV incidence increased by 12% among all MSM and by 22% among young MSM aged 13 to 24 years. The greatest number of new HIV infections from 2008 to 2012 was among young Black/African American MSM aged 13–24 years. Young Black MSM accounted for 45% of new HIV infections among all black MSM and 55% of new HIV infections among young MSM overall (CDC, 2012).
Successful HIV prevention interventions that target individuals, dyads, and communities using traditional delivery formats have been identified (Grossman et al., 2011; Sullivan et al., 2012). One novel delivery format that is becoming increasingly popular is mobile health (mHealth). The World Health Organization (WHO) defines mHealth as a component of electronic health (eHealth) that includes “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices” (mHealth Alliance, 2014; World Health Organization, 2011). The ubiquitous nature of mobile phones in daily life has created opportunities for health interventions in a portable format with enhanced privacy. mHealth is a powerful and relevant tool which can be adapted to meet the needs of its end-users. Using this technology to modify health-related behaviors has great potential to transform health care. Short message service (SMS) or text-messaging interventions targeting diabetes, obesity, smoking cessation, physical activity, and drug adherence have been effective at improving outcomes in targeted groups in the United States and abroad and there is room for expansion of this field in the realm of sexual and behavioral health (Cole-Lewis & Kershaw, 2010; Guse et al., 2012).
mHealth takes advantage of a ubiquitous platform and has broad applications with the potential to make an impact on communication, health care access, and information and resource delivery to vulnerable populations such as young and minority MSM. Ownership of a mobile phone is similar across racial and ethnic minority groups (Duggan, 2013; Smith, 2014). Likewise text messaging is used similarly across racial and ethnic minority groups (Duggan, 2013). In terms of income, although over 90% of cellphone users are in the highest income group (household income $75,000+/year), nearly 80% of those in the lowest income group (< $30,000/year) are also using cellphones for texting (Duggan, 2013). Data indicate that cellphones are a widely used tool, especially among young adult and adolescent populations across racial, ethnic, and economic lines (Lenhart, 2009).
In the case of HIV, health disparities are inextricably linked to age, race, and ethnicity. Mobile technology can be used as a means for achieving health equity in vulnerable groups because of its appeal to young minority persons. To date, quality mHealth interventions for HIV prevention have focused largely on text messaging (Schnall, Travers, Rojas, & Carballo-Dieguez, 2014). Interventions among both Black adolescents and MSM have shown promise with this technology. Adolescents have been shown to be particularly interested in receiving SMS-based information regarding sexual behavior in a format that maintains privacy yet is easily accessible (Perry et al., 2012; Selkie, Benson, & Moreno, 2011). One study of an HIV prevention intervention found daily messages to Black adolescents were acceptable, and contributed to decreased unprotected sex acts, increased HIV knowledge, and an improved attitude towards condom use (Cornelius et al., 2013). Similarly, a small pilot randomized controlled study of an SMS intervention for Black adolescents found that those who received the HIV prevention messages by SMS were more likely to report increased monogamy as compared to controls, though no difference in protected sex acts was noted (Juzang, Fortune, Black, Wright, & Bull, 2011) Among MSM, an Australian study found that routine reminders for HIV testing among self-reported high-risk MSM improved re-testing rates (Bourne et al., 2011). Another study of health education messages to MSM methamphetamine users showed decreased high-risk sexual behaviors, as well as less methamphetamine use at the end of the intervention (Reback et al., 2012)
Methods
Recruitment
Prior to study initiation, approval was obtained from the Columbia University Institutional Review Board and the CDC approved the study protocol (IRB). Eligibility criteria included: Men who reported having unprotected (condomless) anal sex with HIV-positive or unknown-status male partners, age 13–64, had the ability to provide written consent/assent and the ability to read and write in English or Spanish, and self-reported being HIV-negative or of unknown HIV status. Exclusion criteria included: consistent condom use over the past year for both receptive anal intercourse (RAI) and insertive anal intercourse (IAI), or monogamous unprotected anal intercourse (UAI) with partner of certified seronegative status.
Participants were recruited in New York City between June 2013 and November 2013. Flyers detailing the study were distributed at the Callen-Lorde Community Health Center, which provides medical care to lesbian, gay, bisexual, and transgender communities, as well as at other community-based organizations. These included GMHC (formerly known as Gay Men's Health Crisis), the Ali Forney Center, the Harlem United Black Men's Initiative, the Latino Commission on AIDS, Brooklyn Community Pride Center-Rainbow Heights Club, and the Lower East Side Harm Reduction Center. Recruitment also took place at the Harlem Pride Day, an event celebrating the lesbian, gay, bisexual, and transgender community in New York's Harlem neighborhood. Flyers detailing the study were distributed at this event, and interested persons were screened over the phone. There were no participation refusals among eligible participants.
Sample
One hundred and five MSM were screened through the recruitment procedures detailed above. Between June and November 2013, five focus group sessions took place with a final sample size of 33. There were between 5 and 9 participants in each group. Four focus groups were conducted in English and one in Spanish. Two focus group sessions had non-smartphone users as participants.
Procedures
Each MSM focus group session took place at the Columbia University School of Nursing campus. The sessions lasted between 48–72 minutes, and were conducted in English or Spanish. All sessions consisted of one facilitator, one assistant, and the participants. The research team members obtained written informed consent prior to the start of any research activities.
Participants received $40 for their time. Food appropriate for the time of day was served.
A member of the research team distributed surveys to participants prior to the start of each focus group session with questions regarding demographics, average smartphone usage, and general health status. Race and ethnicity were asked as separate questions. Study participants completed two additional surveys. The first detailed sexual history, as well as attitudes and knowledge regarding HIV, STDs, condoms, and sexual behavioral intentions. The second used a 28-item health information/patient privacy tool that has been evaluated in other settings to describe privacy concerns of adult patients regarding their medical history (Whiddett, Hunter, Engelbrecht, & Handy, 2006).
Following completion of the surveys, focus group sessions commenced. Each focus group session was led by a moderator who was accompanied by at least one additional study team member (facilitator). The moderator led the session using a focus group guide developed by the study team. The focus group guide was comprised of open-ended questions listed in Table 1. Following each focus group question, the moderator of the focus group session would summarize the discussion for the study participants. During the session the participants had an opportunity to comment on this summary and correct any misunderstanding by the moderator. This process served as member checks (i.e., sharing of initial data with participants to ensure accurate interpretations), which supported the credibility of the data. In addition, after each focus group, peer debriefing was conducted to confirm findings across members of the research team. All focus group sessions were audio-recorded and then transcribed.
Table 1. Focus Group Guide.
| Education and Information | |
| 1. | What HIV prevention, testing, and other content would you like to see in a mobile app? |
| 2. | What HIV prevention messages should be integrated into a testing app? |
| 3. | What is the best format for delivering information using an app? |
| Identifying Resources | |
| 4. | How would you like local HIV testing resources to be integrated into a mobile app? |
| 5. | How would you like local resources to be integrated into your app? (Probes: listing of resources, map of resources, GPS location, contact information, driving and walking directions, operating hours?) |
| 6. | How can we best integrate the new mobile app into existing HIV prevention campaigns for MSM? |
| Health Data Management | |
| 7. | What are your privacy and confidentiality concerns if you use a mobile app for HIV prevention and testing? |
| 8. | How would you like your mobile app to be able to integrate with social networking Internet sites? |
| Technology Adoption | |
| 9. | What are some of the barriers that you anticipate encountering when using mobile health applications on your phone? (Probes: difficulty with medical terminology, unmet information needs, system hard to use, privacy and confidentiality concerns?) |
| 10. | What are some of the strategies you can use to overcome these barriers? (Probes: medical dictionary, online resources, member of healthcare team, family member or friend?) |
| 11. | What are some of the ways that your overall health may benefit from using mobile health applications? (Probes: better health outcomes, fewer doctor visits?) |
| 12. | Anything else that you would like to say that you didn't get a chance to say? |
Data Analysis
Quantitative data were obtained from the surveys outlined above and entered into SPSS. Descriptive statistics including frequencies for categorical data and means and standard deviations for continuous data were calculated. Qualitative data were obtained from the focus group discussions. These groups were conducted using open-ended questions related to the desires for functions and design of the proposed mobile phone app. Although many topics emerged in the course of the discussions, the data reported in this analysis represent the most frequent themes/subthemes reported by participants. Study team members coded the transcripts using NVivo (QSR International, Victoria, Australia) software. To analyze the focus group transcripts, a codebook was developed using the IMB framework: (1) information, (2) motivation, and (3) behavioral skills. Subthemes within each of these three major themes were created as detailed below and participant quotes were sorted into these categories. The study team met, reviewed, and agreed to the coding schema that was developed. We adhered to qualitative research processes to ensure the credibility, confirmability, dependability, and transferability of the qualitative data from these analyses. The focus group-derived codebook was compared with the survey data to help confirm the interpretations. The investigators kept extensive field notes to facilitate transfer-ability of study findings into other contexts, such as the use of apps for other study populations, or the use of other technology for HIV prevention.
Theoretical Framework
We used the Fisher and Fisher Information, Motivation, and Behavioral Skills (IMB) model as the theoretical framework to organize our analysis. This is a comprehensive model that integrates many elements from prior theoretical models (e.g., AIDS Risk Reduction Model, Theory of Reasoned Action). The IMB posits that HIV risk reduction is a function of possessing (1) information regarding HIV, (2) motivation to practice preventive measures, and (3) behavioral skills that will decrease the risk of acquiring HIV. Each of these constructs can work independently of each other to affect behavior change, but use of all three together significantly increases the likelihood of success (Fisher, Fisher, Misovich, Kimble, & Malloy, 1996). The model asserts that specific informational, motivational, and skill factors will vary as a function of culture, class, economics, environment, and life circumstances. Therefore, Fisher and Fisher (2000) recommend:
The first step … involves elicitation research conducted with a subsample of a population of interest, to empirically identify population-specific deficits and assets in HIV prevention information, motivation, behavioral skills, and HIV risk and preventive behavior. The use of open-ended data collection techniques such as focus groups and open-ended questionnaires to avoid providing occasion for prompted responses is advocated, in addition to the use of close-ended techniques that lend themselves to quantitative analyses. (p. 41)
The IMB model has been validated and used for a variety of HIV risk-reduction interventions (Fisher et al., 1996; Kalichman et al., 2002). More recently, the IMB model was used to inform the creation of eHealth interventions for MSM and was shown to reduce sexual risk-taking behaviors (Fisher, 2011). Using the IMB Model to guide our analysis allows us to identify the content of a HIV-prevention intervention that can be used to reduce behavioral risk factors for HIV in high-risk MSM.
The IMB model guided our analysis of the focus group data so that we could identify the desired content for a mobile app for HIV prevention for MSM. The focus group results reported here are part of a larger research project to inform the development of two mobile apps for (1) HIV prevention for high-risk men who have sex with men (MSM), and (2) HIV treatment and care for people living with HIV/AIDS (PLWH). The purpose of this study is to identify and utilize the desired content and features of a mobile app for meeting the HIV prevention needs of high-risk MSM. The work conducted has the potential to address two of the primary goals of the National HIV/AIDS Strategy: (1) reducing the number of people who become infected with HIV and (2) reducing HIV-related health disparities (The White House Office of National AIDS Policy, 2010).
Results
Participant Characteristics
Table 2 shows descriptive characteristics of the 33 study participants. Mean age was 33.4 years (range 18–57 years). Our study participants were largely young adults who identified as being from ethnic or racial minority groups, who are the segment of the MSM population who are most at-risk for becoming infected with HIV (CDC, 2014) and most likely to be smartphone users (Lenhart, 2009). In terms of ethnicity, 18 (58.1%) participants identified as Hispanic/Latino. In terms of race, 17 (56.7%) identified as black, and 6 (20.0%) as white. Eighteen (56.3%) reported using a smartphone several times a day, 5 (15.6%) used once a day, 3 (9.4%) several times per week, 4 (12.5%) several times per month and 2 (6.3%) never used one. All of the participants had previously had an HIV test, and the mean number of lifetime tests was 9.1 per participant. The majority (93.9%) reported either being in excellent, very good or good health. Overall, participants reported a willingness to share clinical information with their clinicians, pharmacists, insurers, the local health department and researchers (data not shown).
Table 2. Characteristics of High Risk MSM Study Population, N = 33.
| Variable | N (%) |
|---|---|
| Age (mean years) | 33.4 |
| Race | |
| Black | 17 (56.7) |
| White | 6 (20) |
| American Indian | 2 (6.7) |
| Asian | 1 (3.3) |
| Hawaiian | 1 (3.3) |
| Other | 3 (10.0) |
| Ethnicity (Hispanic/Latino) | 18 (58.1) |
| Smartphone use | |
| Several times per day | 18 (56.3) |
| Once per day | 5 (15.6) |
| Several times per week | 3 (9.4) |
| Several times per month | 4 (12.5) |
| Never | 2 (6.3) |
| HIV testing | |
| Ever tested for HIV | 32 (100) |
| Number HIV tests ever (mean, SD) | 9 (6.2) |
Note. Not all categories equal 100% due missing data.
IMB Themes
The information themes consisted of subthemes identified through focus groups, and represented the most frequently reported knowledge deficits pertaining to HIV prevention information that participants believed the proposed app could address. These included information such as HIV testing locations, support groups, prevention methods, HIV risk information, HIV disease/treatment information, and STI information. Similarly, within the motivation theme, we identified prevalent subthemes which were: attitudes and intentions regarding HIV prevention, which have been detailed in prior work on the IMB model (Fisher, 2011). Additionally we identified a new subtheme addressing a desire for peer interaction, education, and communication. Within the behavioral skills theme, we identified condom use, identifying HIV testing locations, negotiation of safer sex, and HIV/STI symptom recognition as prevalent subthemes. Figure 1 illustrates the IMB themes that guided the content for the HIV prevention mobile app. Squares represent the IMB themes in our codebook, while circles represent areas where the mobile app can address these themes. Table 3 provides sample quotations from participants for each of the IMB themes and subthemes, as well as the specific function provided by the mobile app to address these categories.
Figure 1.
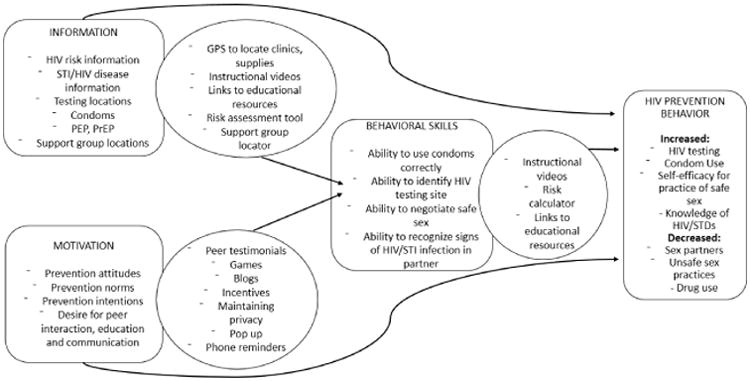
IMB model for HIV prevention, detailing the HIV prevention information/motivation and behavioral skills (squares) desired to achieve the outcome of improved HIV preventive behavior, and where the mobile app (ovals) can improve these areas.
Table 3. HIV Prevention Information, Motivation, and Behavioral Skills of Participants and Tools for Enhancing These With a Mobile Phone App.
| Theme | Focus Group Quote | Mobile App Tool |
|---|---|---|
| 1. HIV Prevention Information | ||
| HIV testing locations | I believe it would be useful for example to have an app … it should have like a button saying ‘AIDS testing,’ and a map appears such as Google maps.” | GPS testing site locator |
| Support group/peers | “If I got HIV, it would be nice to have an app … who I could talk to, some information that would make me not want to kill myself.” | GPS function to locate support groups, clinics; directory of support groups, clinics; link to hotlines |
| I would want … counseling services if I … needed someone to talk to. And that could either connect me by phone or … lead me to a place where someone's … sitting there in person.” | ||
| Prevention methods | “… where I can get free condoms.” | GPS function to locate condoms, PrEP/PEP; links to information on PEP, PreP |
| “I feel like we [focus group participants] already know what PrEP and PEP are …. But Joe Schmo on Grindr does not know what that is.” | ||
| HIV risk information | “[Include] messages about the risk of HIV and what the disease really entails because it sounds like it is easy to forget, specially in New York City, what that is.” | Informational pages with keyword search tool about behaviors and practices that increase risk for infection; Links to resources for more information |
| [The app] should specify really well [risky behaviors] … the use of drugs, the use of syringes, the contact with blood and all that, it should be specified well.” | ||
| HIV disease/treatment information | “More than talk, the prevention part of what to do before, or what happens when you are, what happens when you already have the virus. Or also the different HIV treatments, so you can have a notion of the side effects, what follows, or like a manual of what you have to do based on what you need to do for your specific situation.” | Informational pages and links to other resources |
| STD symptoms, treatment, prevention | “Apps that test how much you know and maybe could be on sexual awareness, STDs, just things that I don't think a lot of you know, kids even know, that condoms are not only for HIV, you can get STDs, you might not get HIV, you get an STD.” | Informational pages and links to other resources |
| “If I'm curious about an STD or something then I'll look it up and read about it.” | ||
| 2. HIV Prevention Motivation | ||
| Prevention attitudes | “And the real issue is … just to outlive, you know, protection, and being responsible.” | Links to video peer testimonials; blogs; pop-ups with information bytes |
| Prevention norms | “One young boy is not going to ask his homeboy…. I'm going to get tested because that's not like the cool thing to do probably, so looking on the computer, you know what I'm saying, if that app or something was there, just there, you know what I'm saying and he can personally just look it up and find information on his own time, without his friends around, it might help.” | Links to video peer testimonials; role play videos |
| Prevention intentions | “So sometimes when you are in the spur of the moment and … when you drink or smoke, you don't really think about protection.” | Pop-up text reminders |
| Desire for peer interaction, communication, education | “It would be very important for me to feel like it [the smartphone app] was peer-made. So that like other people who are having a lot of sex are making [the app], rather than like a nurse being like ‘ribbing is dangerous.’” | GPS support group locator; directory of support groups targeted to specific populations; links to video peer testimonials; blogs |
| “I have a lot of friends who recently arrived in New York, and they really don't know where to go, where to look for support groups or where gay men meet to discuss topics such as AIDS, protection.” | ||
| “There should be a chat where people can speak, or speak to a person live, and say ‘look, I am going through this…I want to have sex or sexual relationships’…there are people who talk this way and they don't care, and they need to speak to someone | ||
| 3. HIV prevention behavioral skills | ||
| Ability to use condoms correctly | “Here is a 15-second clip of how you put a condom on with your mouth.” | Instructional videos |
| Ability to negotiate safer sex | [speaking of proof of HIV testing by sex partner prior to engaging in sex] “You know it's like…let me see your paperwork. Bam, pull it right there up on the phone… I take pictures of mine.” | Record keeping function for HIV test results |
| Ability to recognize signs of HIV/STI | “The same symptoms you may get from HIV, it can be from something else. Even though you go on the Internet and you look up these symptoms and so forth it's always best to go to a physician.” | Links to informational pages; GPS for STI clinic locations |
HIV Prevention Information
Focus group findings indicated that respondents desired information about STI/HIV risk and disease, HIV testing locations, PrEP/PEP, and support groups in a mobile phone app.
STI/HIV Risk and Disease
Participants stressed the importance of having access to accurate information regarding HIV risk factors, particularly since many misconceptions about HIV transmission exist: “There are people who think HIV is spread by talking, by touching, and that's not the case. You can live with an HIV [positive] person, as long as there is not blood contact…you can eat with them, because eating with a person with HIV is nothing…” Most were aware that “not only gays get STDs; there are other people who can get them … the use of drugs, the use of syringes, and the contact with blood.” Though many felt they knew the basics, there was awareness of some knowledge gaps, specifically related to risk assessment. As one participant stated, he desired a tool for “risk assessment … sometimes … I will engage in some behavior. And … I wonder how risky that is? And I'll Google it later. But it would be nice to have … [this information on the app].”
HIV Testing Locations
Nearly all respondents expressed that they knew where to obtain HIV testing and correctly listed hospitals, clinics, pharmacies, and mobile health vans as potential sites, but there was still a desire for an app to make the process easier. “There are a lot of places where you can get free HIV testing citywide … they do testing for free.” Survey findings echoed this, as 91% reported they knew where to get HIV tested. Still, many desired a GPS function as noted earlier for making the search for testing sites easier. In addition, participants also suggested pop-up messages to help locate testing sites, “(the app should have) a health tip or … a bit of information (that) a facility is giving out free testing … just pop up (as you're) navigating the app.” Participants expressed the need to have an easy way to find HIV testing locations, because as one participant stated, “I sense the community lacks knowledge … on all aspects, and lacks promotion on where to go or how to get a test.” One respondent suggested the app should “have a button saying ‘AIDS testing’ and a map appears such as Google Maps, and you find places in your area.”
Supplies
Participants felt that many in their community knew where to get free condoms, but information regarding other supplies such as PrEP/PEP was lacking. “It's easy to find the New York City condoms…” said one participant. Although a few knew where to access PrEP/PEP, “if you think you are at high risk, you go to the emergency room and ask for the PrEP,” many did not, and felt that the larger community did not. As one participant stated, “So I feel like there are all the good work of prevention and…condoms and those barrier methods. But then there is also … the [need] to be integrated more into messages … the fact that PrEP and PEP exist.”
Support Groups
Participants thought it would be useful to incorporate support group functionality into their mobile app. As one participant stated, “Outreach and peers are where I get more of my information.” One member provided outreach to young males with a peer, “We'd go to certain neighborhoods around Staten Island … we'd go out looking for some guys between the ages of 13 and 24. And we give out free condoms.” Others obtained support through social media, “sometimes when I go on Facebook, I see these groups and social sites where they talk about HIV, where they have open discussions about HIV and awareness.”
Findings from the survey data supported the focus group data. Although respondents were aware of HIV-related information, such as the utility of condoms, there were gaps in their knowledge about STD/HIV acquisition. Eighty-five percent of respondents believed sex without a condom is risky, and 76% correctly believed the presence of an STD increases risk of HIV acquisition. However, about 15% incorrectly believed that the withdrawal method prevents HIV/STIs. Nearly half of respondents correctly knew they could not get HIV from sharing utensils with an HIV-positive person but some had misinformation regarding new HIV acquisition: 15% felt that an HIV test is accurate one week after potential exposure, and 6% believed all HIV-positive people show signs of infection soon after becoming infected. In terms of HIV disease information, almost all (94%) knew that there is no cure for HIV. For STD-related information, 85% believed condoms protect against STDs when used correctly. In summary, the HIV prevention information needs that were identified in the focus group sessions indicated that our participants were interested in an app that would identify free HIV testing, condom and PrEP/PEP distribution locations, as well as information about support groups, and STI/HIV risk, and disease information.
Motivation for HIV Prevention
The motivation for HIV prevention among our focus group participants was evident in the attitudes and intentions for HIV prevention. The role of the proposed mobile app to improve these areas was envisioned through peer interaction through education and communication.
Attitudes
Respondents indicated that they desired to practice safer sex even though they were aware that this is not always possible. One participant stated “sometimes people don't use protection through no fault of their own…people are human beings, people sometimes forget, sometimes holes are in condoms, that happens. Sometimes the passion becomes so great that you don't think about it.” Another participant, when discussing the need for practicing safer sex, went on to acknowledge, “I'm not going to say go out and be stupid and risk your life every day and be a dummy … what I'm saying [is] you can't not live either.” Survey findings complemented the focus group findings. While 91% of participants believed that anyone who has unprotected sex should be tested for HIV, 18% reported they were too scared to be tested. Furthermore, 42% of participants felt that sex does not feel as good with condoms, 15% felt that condoms ruin the mood and 18% felt too embarrassed to ask his partner to use a condom.
Intentions
Respondents discussed their intentions to practice safer sex, but some acknowledged they did not always follow through with the plan. Similarly, respondents reported in the surveys that they all believed they would have sex in the next three months, but only 30% reported they would always use condoms. A participant stated, in reference to the usefulness of text reminders by the app, “Yeah! Absolutely because … I had everything planned out to be safe and to have a good time, but I only ended up … protecting myself halfway.”
Desire for Peer Education/Communication
Results from the focus group data revealed participants rely on peers to provide them with HIV prevention information. As one person noted “outreach and peer (interaction) is where I get … [most] of my information.” One participant poignantly discussed outreach he did with sex workers, “sometimes … they have low self-esteem. And some of them are still in the sex trade. But who … could get them out of the sex trade to tell them that they are important, they are still loved.” This highlighted a prevalent theme that peer support needs to be a major component of HIV prevention interventions. The participants wanted this peer interaction to be delivered in a variety of formats. There was a desire for video testimonials and short stories from peers as supportive tools, because as one person noted, “it would be very important for me to feel like it [the app] was peer-made” and not provided through medical staff. There was a particular need to have the tools cater to targeted groups of high risk MSM, such as sex workers, men on the down low (that is, men who do not identify as gay or disclose their same-sex activities,) young MSM and older MSM. One person suggested for the app to “try to have stories, true stories from all types of ages, from the younger to the oldest, for the one that is negative and to the one that is positive. The one that is actually making 20-something years being HIV positive … to the one that … haven't experienced sex yet.” They also expressed an interest in an educational gaming function with health tips, such as “a multiplayer game … you can play with other people who have the app, because … I always feel more motivated to play the games where … my friends are waiting for me to do my turn, so that they can go do their turn.” Participants suggested that a mobile app could also provide peer-led education and communication by interactive blogs and forums, making it a versatile support tool for HIV prevention.
Behavioral Skills for HIV Prevention
Behavioral skills necessary for HIV prevention included the ability to: use condoms correctly, negotiate and practice safer sex, and recognize signs of STI.
Condom Use and Safer Sex
Condom use was inconsistent among participants. Survey data showed high levels of sexual activity and inconsistent condom use. Twenty-six respondents reported a mean of 2.7 vaginal sex partners (range 0–40), 29 reported 4.9 mean anal sex partners (range 1–30), and 28 reported 7 mean oral sex partners (range 1–40), in the past 3 months. With their vaginal sex partners, 56% reported using a condom with their main partner and 39% with their casual partner at last sexual activity. With anal sex partners, 57% used a condom with their main partner and 61% used one with their casual partner. In terms of oral sex partners, 30% used condoms with their main partner and 29% with their casual partner. The majority of participants (82%) reported that they knew how to put on a condom correctly, and 85% felt they were easy to use, a small number of participants believed that a condom should first be unrolled, then put on, thought that the time to put on a condom was just before ejaculation, and did not know to leave space at the tip of the condom when using it. There was a desire for instructional videos on condom use, such as “a 15 second clip of how you put a condom on with your mouth.” Another participant suggested teaching safer sex acts through videos, and yet another through photos, “like a safe sex Kama Sutra.”
Negotiating Safer Sex
Many participants noted diffculty with negotiating safer sex with their partners, identifying proof of their partners' status as important factor. One person, however, frankly stated “You better get me some papers,” referring to HIV test results, and another suggested having the app store listing test results for ease of sharing between partners.
Recognizing Signs of HIV/STIs
Many participants reported awareness that recognizing STI and new HIV infection was difficult. One person commented that “the same symptoms you may get from HIV can be something else.” This was also evident in the surveys, as only 21% believed they could tell if their partner has an STI. There was a request for instructional videos, particularly for “the newcomer that's coming out, basically [to learn] how to use a condom and the risk of HIV and STIs.” Additionally, testing these skills could also be achieved through the app; one participant noted, “we could test people's knowledge, like what they already know…like the true or false [quiz].” In summary, respondents thought that a mobile app could support skills for HIV prevention by providing a tool for teaching and learning.
Content Delivery and Privacy Concerns
Focus group participants shared other concerns for delivery of an intervention through a mobile phone app. Participants desired the delivery of this information to be in language that was simple and fun. They expressed the need for “information people can understand, not what the doctors say, but what people can understand.” The delivery of this information was also important, and as one participant reported, it should be “not too sensational, like having HIV is a death sentence”. Finally, maintaining privacy was a principal concern and participants identified methods to keep their information safe, such as using password protection on the app or having a neutral app icon, to help avoid stigma.
Discussion
We conducted a descriptive study to identify the desired content for an HIV-prevention mobile app among high-risk urban MSM. We used a hybrid qualitative-ethnographic approach and asked open-ended question to allow our participants to express their preferences and information needs in a mobile app. Following this method for data collection, we used the IMB model to organize our findings. Using this approach we did not impose a theory during our data collection, which may have limited the richness of our findings. However, we did use the IMB model to organize our data. Our purpose in using this approach was so that our data can be used to easily inform the development of behavioral interventions, in this case a mobile app. Findings from this formative work are a first step in identifying the mobile app content necessary for improving HIV prevention in high-risk MSM. Data collected in this study are informative and can help us shape interventions urgently needed for MSM.
mHealth interventions that serve as interactive tools to engage end-users through SMS are starting to increase in popularity. Preliminary studies have shown that this format is desirable, feasible and acceptable. Two recent studies of MSM using Grindr showed that mobile technology can be used as a recruitment tool for HIV prevention studies as well as a tool for linking this population to HIV testing (Martinez et al., 2014; Rendina, Jimenez, Grov, Ventuneac, & Parsons, 2014), demonstrating the usefulness of mHealth and social networking for improving HIV prevention in high-risk MSM. Another recent study sent prevention tips by SMS to teens and also provided links at the end of each message to websites that provided more information that teens could directly click on and access in the moment (Perry et al., 2012). One well-received function of this intervention was the clinic locator function, which allowed teens to text their zip code to a number that would then direct them to the closest clinic in their area. In this context, our findings inform a similarly comprehensive app that moves beyond one-way reminders, and incorporates a package of services focused on a particularly vulnerable demographic. The strength of our findings largely come from use of the validated IMB model for behavior change, as well as the user-driven component, which gives a voice to urban minority MSM in the development of a comprehensive care package for HIV prevention.
We used the IMB Model to guide our analysis but we are aware that this model only includes some of the factors that need to be taken in consideration when developing a HIV prevention intervention. There are a number of individual, interpersonal, and social factors that may affect HIV prevention behaviors (Ames, Atchinson, & Rose, 1995; Schwartz, 1973; van Kesteren, Hospers, van Empelen, Breukelen, & Kok, 2007). Moreover the number of desired topics for an app mentioned by the MSM during our focus group sessions is huge. To address all of these components would require an enormous and complicated app. As such, these focus groups were the first stage in an iterative and multi-staged process to inform the development of a mobile app for high-risk MSM. Findings from these focus group sessions informed the desired content and some of the functional specifications for a mobile app for HIV prevention in high-risk MSM. In order to best meet the needs of end-users, future work will include further study of the functional specifications through user-centered design sessions as well as design of the user interface through usability evaluations. Once we have identified the content, user interface, and functional specifications of an HIV prevention app for high-risk MSM, it will be important to study the use of the app as well as factors that contribute to men downloading the app. In addition to downloads and use, ultimately further study of an app's effectiveness in a trial is necessary to assess whether this technology can improve HIV prevention behaviors and health outcomes.
Although HIV prevention apps are available commercially, consumers have not downloaded them frequently or rated them highly (Muessig, Pike, Legrand, & Hightow-Weidman, 2013). Our study findings support the many barriers that have been previously cited as to why HIV prevention apps fail (Muessig et al., 2013). Participants in our study indicated that they wanted an app to provide on-the-spot information that may be beneficial ultimately improving HIV prevention behaviors and outcomes in this high-risk group. Specifically, our study population indicated that a lack of desired content such as tools for providing emotional support or improving interpersonal skills in safer sex negotiation. The poor success of these apps highlights the need to work with the targeted end-user populations as well as developers and public health offcials to design appropriate content. The work conducted in our study is the first step in building an app that is potentially useful for the target audience. Past development of e-health-related apps rarely involves the end-users in its conceptualization or development (McCurdie et al., 2012). The work conducted in this study focuses on the intended end-users' needs. This is a critical step in ensuring uptake of the proposed app, as past research has documented that inclusion of the end-users' in the development of health information technology, such as mHealth, makes it more likely to be utilized (Maguire, 2001).
Limitations
Although this study provided much-needed information on desired content for HIV prevention in a high-risk group, we were limited by a single geographic area. These study findings are applicable to high risk MSM in urban environments such as New York City, an area with the highest HIV burden in the United States. As a result, issues relevant to high-risk persons in rural areas may have been missed. Another potential limitation is that survey data were self-reported and so participants may have under-reported their high-risk behaviors. Finally our study sample was small for survey data, thus making it difficult to reach generalizations from this data source.
Conclusions
Our study offers much-needed information provided by the target population regarding the desirable content for a mobile app aimed at HIV prevention. The content of the mHealth app that is desired by our study population fits well within the validated IMB model and is therefore a promising tool to enact behavior change. Findings from this study can be used to inform the development of a convenient, easily disseminated tool to help prevent HIV infection among high-risk MSM.
Acknowledgments
This publication was supported by a cooperative agreement between the Columbia University School of Nursing and the Centers for Disease Control and Prevention (CDC; 1U01PS00371501; PI: R Schnall). The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Grant support for N. Aliabadi provided through a Columbia University Primary Care Research Fellowship in General Medicine, Health Resources and Services Administration (HRSA; T32HP1026000). William Brown III is supported by NLM research training fellowship T15 LM007079 and NIMH center grant P30 MH43520.
Contributor Information
Negar Aliabadi, Division of General Medicine, Columbia University, New York, New York.
Alex Carballo-Dieguez, Division of General Medicine, Columbia University, New York, New York; HIV Center, Division of Gender, Sexuality and Health, New York State Psychiatric Institute. New York, NewYork.
Suzanne Bakken, Division of General Medicine, Columbia University, New York, New York.
Marlene Rojas, Division of General Medicine, Columbia University, New York, New York.
William Brown, III, Division of General Medicine, Columbia University, New York, New York; HIV Center, Division of Gender, Sexuality and Health, New York State Psychiatric Institute. New York, NewYork.
Monique Carry, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia.
Jocelyn Patterson Mosley, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia.
Deborah Gelaude, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia.
Rebecca Schnall, Division of General Medicine, Columbia University, New York, New York.
References
- Ames LJ, Atchinson AB, Rose T. Love, lust, and fear. Journal of Homosexuality. 1995;30:53–73. doi: 10.1300/J082v30n01_03. [DOI] [PubMed] [Google Scholar]
- Bourne C, Knight V, Guy R, Wand H, Lu H, McNulty A. Short message service reminder intervention doubles sexually transmitted infection/HIV re-testing rates among men who have sex with men. Sexually Transmitted Infections. 2011;87:229–231. doi: 10.1136/sti.2010.048397. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Diagnoses of HIV infection and AIDS among adolescents and young adults in the United States and 5 U.S. dependent areas, 2006–2009. HIV Surveillance Supplemental Report. 2012;17 [Google Scholar]
- Centers for Disease Control and Prevention. HIV Among Gay and Bisexual Men. 2014 Retrieved November 5, 2014, from http://www.cdc.gov/hiv/risk/gender/msm/facts/
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews. 2010;32:56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius JB, Dmochowski J, Boyer C, St Lawrence J, Lightfoot M, Moore M. Text-messaging-enhanced HIV intervention for African American adolescents: a feasibility study. Journal of the Association of Nurses in AIDS Care. 2013;24:256–267. doi: 10.1016/j.jana.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M. Cell phone activities 2013. PewResearch Internet Project. 2013 May 19; Retrieved August 26, 2014, from http://www.pewinternet.org/2013/09/19/cell-phone-activities-2013/
- Fisher CM. Are information, motivation, and behavioral skills linked with HIV-related sexual risk among young men who have sex with men? Journal of HIV/AIDS and Social Services. 2011;10:5–21. doi: 10.1080/15381501.2011.549064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change. New York: Kluwer Academic/Plenum Press; 2000. [Google Scholar]
- Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: Effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychology. 1996;15:114–123. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- Grossman CI, Forsyth A, Purcell DW, Allison S, Toledo C, Gordon CM. Advancing novel HIV prevention intervention research with MSM—meeting report. Public Health Reports. 2011;126:472–479. doi: 10.1177/003335491112600404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guse K, Levine D, Martins S, Lira A, Gaarde J, Westmorland W, Gilliam M. Interventions using new digital media to improve adolescent sexual health: A systematic review. Journal of Adolescent Health. 2012;51:535–543. doi: 10.1016/j.jado-health.2012.03.014. [DOI] [PubMed] [Google Scholar]
- Juzang I, Fortune T, Black S, Wright E, Bull S. A pilot programme using mobile phones for HIV prevention. Journal of Telemedicine and Telecare. 2011;17:150–153. doi: 10.1258/jtt.2010.091107. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Stein JA, Malow R, Averhart C, Devieux J, Jennings T, et al. Feaster DJ. Predicting protected sexual behaviour using the information-motivation-behaviour skills model among adolescent substance abusers in court-ordered treatment. Psychology, Health and Medicine. 2002;7:327–338. doi: 10.1080/13548500220139368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A. Teens and mobile phones over the past five years: Pew internet looks back. 2009 Retrieved March 28, 2010, from http://www.pewinternet.org/Reports/2009/14—Teens-and-Mobile-Phones-Data-Memo/1-Data-Memo/5-How-teens-use-text-messaging.aspx?r=1.
- Maguire M. Methods to support human-centred design. International Journal of Human-Computer Studies. 2001;55:587–634. doi: 10.1006/ijhc.2001.0503. [DOI] [Google Scholar]
- Martinez O, Wu E, Shultz AZ, Capote J, Lopez Rios J, Sandfort T, et al. Rhodes SD. Still a hard-to-reach population? Using social media to recruit Latino gay couples for an HIV intervention adaptation study. Journal of Medical Internet Research. 2014;16:e113. doi: 10.2196/jmir.3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, Cafazzo J. mHealth Consumer Apps: The case for user-centered design. Biomedical Instrumentation & Technology. 2012;46:S49–S56. doi: 10.2345/0899-8205-46.s2.49. [DOI] [PubMed] [Google Scholar]
- mHealth Alliance. Frequently asked questions. 2014 Retrieved March, 2014 from mhealthalliance.org/about/faq.
- Muessig KE, Pike EC, Legrand S, Hightow-Weidman LB. Mobile phone applications for the care and prevention of HIV and other sexually transmitted diseases: A review. Journal of Medical Internet Research. 2013;15:e1. doi: 10.2196/jmir.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry RC, Kayekjian KC, Braun RA, Cantu M, Sheoran B, Chung PJ. Adolescents' perspectives on the use of a text messaging service for preventive sexual health promotion. Journal of Adolescent Health. 2012;51:220–225. doi: 10.1016/j.jadohealth.2011.11.012. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Grant DL, Fletcher JB, Branson CM, Shoptaw S, Bowers JR, et al. Mansergh G. Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. AIDS and Behavior. 2012;16:1993–2002. doi: 10.1007/s10461-012-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Jimenez R, Grov C, Ventuneac A, Parsons J. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS and Behavior. 2014;18:41–49. doi: 10.1007/s10461-013-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall R, Travers J, Rojas M, Carballo-Dieguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. Journal of Medical Internet Research. 2014;16:e134. doi: 10.2196/jmir.3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SH. Normative explanations of helping behavior: A critique, proposal, and empirical test. Journal of Experimental Social Psychology. 1973;9:349–364. doi: 10.1016/0022-1031(73)90071-1. [DOI] [Google Scholar]
- Selkie EM, Benson M, Moreno M. Adolescents' views regarding uses of social networking websites and text messaging for adolescent sexual health education. American Journal of Health Education. 2011;42:205–212. doi: 10.1080/19325037.2011.10599189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. African Americans and technology use: A demographic portrait. Pew Research Center; 2014. http://www.pewinternet.org/2014/01/06/african-americans-and-technology-use/ [Google Scholar]
- Sullivan PS, Carballo-Dieguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, et al. Sanchez J. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–399. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kesteren NC, Hospers H, van Empelen P, Breukelen G, Kok G. Sexual decision-making in HIV-positive men who have sex with men: How moral concerns and sexual motives guide intended condom use with steady and casual sex partners. Archives of Sexual Behavior. 2007;36:437–449. doi: 10.1007/s10508-006-9125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiddett R, Hunter I, Engelbrecht J, Handy J. Patients' attitudes towards sharing their health information. International Journal of Medical Informatics. 2006;75:530–541. doi: 10.1016/j.ijmedinf.2005.08.009. [DOI] [PubMed] [Google Scholar]
- White House Office of National AIDS Policy. National HIV/AIDS strategy for the United States. 2010 Jul; Retrieved November 30, 2014, from https://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- World Health Organization. New horizons for health through mobile technologies Based on the findings of the second global survey on eHealth. Vol. 3. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]


