Abstract
Background
Childhood maltreatment decreases age of first use and speeds the transition from first use to dependence (i.e., telescoping) for alcohol use, however, it is currently unknown whether this influence is the same for men and women.
Method
Analyses were conducted with the National Epidemiologic Survey on Alcohol and Related Conditions (n=34,653). Outcome variables included: age of alcohol initiation and time to onset of DSM-IV alcohol dependence. Predictor variables included: gender and childhood maltreatment. Linear and Poisson regression analyses were conducted.
Results
Results demonstrated that in regards to age of drinking initiation, individuals who experienced childhood maltreatment initiated 1 year earlier than those without maltreatment, however, there was no interaction of this relationship with gender. Regarding the time to dependence, it was found that women who experienced childhood maltreatment demonstrated telescoping (shorter time between onset and dependence) compared to women without maltreatment and men (both with and without maltreatment).
Conclusion
Women with a history of childhood maltreatment are particularly vulnerable to an accelerated time from initiation of alcohol use until dependence, a pattern indicative of increased negative alcohol related outcomes. Findings highlight the need for development of gender-specific prevention efforts and behavioral treatments to aid in early intervention of problematic alcohol use in women.
Keywords: Childhood maltreatment, alcohol use, trauma, gender
The early onset of use and abbreviated course from onset of use to problematic use of alcohol has been associated with a variety of deleterious physical and mental health outcomes (Brook, Brook, Zhang, Cohen, & Whiteman, 2002), including greater harmful substance related outcomes (Dewit, Adlaf, Offord, & Ogborne, 2000; Windle & Windle, 2012), and less successful alcohol use treatment outcomes (McGorry, Purcell, Goldstone & Amminger, 2011). The telescoping of alcohol use, defined as shorter trajectories from the onset of alcohol use to meeting criteria for dependence, is particularly concerning as this alcohol use pattern suggests a decreased time period to provide secondary prevention efforts, as well as an acceleration of serious alcohol use related complications (see the following for telescoping definition: Becker & Hu, 2008; Brady & Randall, 1999; Greenfield, Back, Lawson, & Brady, 2010; Kosten, Rounsaville, & Kleber, 1985). There is a clear need to understand factors which contribute to early onset and accelerated trajectories of alcohol use so that early interventions, which are sensitive to identifiable risk factors, can be implemented.
The telescoping effect for alcohol has been stronger in studies which employed clinical samples, rather than large, epidemiological datasets (Piazza et al., 1989; Randall et al., 1999). Although men have been found to have a younger age of onset of alcohol use, the period of time from onset of use to dependence has been found to be “telescoped” in women (Hernandez-Avila, Rounsaville, & Kranzler 2004; Piazza, Vrbka, & Yeager, 1989; Randall et al., 1999). Population based research has been less supportive of gender differences in the onset and course of alcohol use disorders, generally showing that men and women show small, but significant differences in age of onset but report little difference in the course and progression of use (Khan et al., 2013; Schuckit, Daeppen, Tipp, Hesselbrock, & Bucholz, 1998). The telescoping effect has also been less evident in recent studies using national data sets, challenging the existence of gender differences in onset and the time course of alcohol use disorders (Keyes, Martins, Blanco, & Hasin, 2010; Khan et al., 2013). Keyes and colleagues analyzed two national U.S. studies (National Longitudinal Alcohol Epidemiological Study (NLAES) and National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)) and found no evidence of gender differences in telescoping of alcohol use in the population overall.
Conflicting evidence for telescoping in these studies warrants further investigation into gender and substance use patterns in the population as a whole. Moreover, these findings invite a focus on factors which may moderate the relationship of gender and telescoping. The difference in findings between epidemiological and clinical samples may be due to moderators in the relationship of gender and telescoping that have not yet been identified and occur at higher frequency in clinical samples. Experience of childhood maltreatment is a potential moderator of the relationship of gender and alcohol outcomes that deserves targeted exploration. Identifying the potential risk factor of childhood maltreatment in epidemiological datasets such as the NESARC may help to further explain the relationship of gender and telescoping.
Prior work has documented that the experience of childhood maltreatment leads to negative alcohol use outcomes such as earlier age of substance use onset and increased rates of alcohol use disorder diagnoses (Benjet, Borges, Medina-Mora, & M’Endez, 2012; Elliot et al., 2014; Hussey, Chang, & Kotch, 2006; Kessler, Davis, & Kendler, 1997; Keyes et al., 2012). Prior studies have utilized the NESARC data to examine the role of childhood maltreatment with findings that childhood maltreatment has been associated with: negative physical health outcomes (Afifi, Mota, MacMillan, & Sareen, 2013), increased rates of psychiatric disorders (Afifi, Mota, Dasiewics, MacMillan, & Sareen, 2012; Keyes et al., 2012; McLaughlin, Conron, Koenen, & Gilman, 2010), increased rates of personality disorders (Afifi et al., 2011), increased rates of substance use disorders (Afifi, Henriksen, Asmundson, & Sareen, 2012; Fenton, Geier, Keyes, Skodol, Grant, & Hasin, 2013; Goldstein et al., 2013; Hughes, McCabe, Wilsnack, West, & Boyd, 2010; Pilowsky, Keyes, & Hasin, 2009), and younger age of alcohol onset (Rothman, Edwards, Heeren, & Hingson, 2008). These findings clearly show the deleterious outcomes of childhood maltreatment on many aspects of physical and psychological functioning in adulthood. A subset of these manuscripts have examined the role of gender in the development of alcohol use disorders (Afifi et al., 2012; Fenton et al., 2013; Hughes et al., 2010), and findings suggest that sexual abuse (Afifi et al., 2012; Fenton et al., 2013) and emotional neglect (Afifi et al., 2012; Fenton et al., 2013) are associated with increased rates of alcohol use disorders in women as compared to men. Despite these findings that childhood maltreatment leads to increased rates of alcohol use disorders with some findings demonstrating greater rates in women, the effects of childhood maltreatment on the course of alcohol use disorders in men and women are not well studied. Recent findings suggest that childhood maltreatment exhibits a significant role in the persistence of alcohol use disorders in adulthood (Elliott et al., 2014), further highlighting the importance of examining childhood maltreatment in relation to the time-course of alcohol dependence. However, this study did not examine associations between childhood maltreatment, gender, and the development of alcohol dependence. As telescoping, the attenuated course between onset and development of dependence on alcohol, is a unique and important factor in understanding trajectories and suggests different needs for intervention, it is essential that we understand the role of childhood maltreatment in that process.
In addition to the strong rationale for exploring the relationship of alcohol use and childhood maltreatment, prior research has found that gender affects this relationship. Specifically, both experience of childhood maltreatment and ongoing stress have been shown to play a differential role in the development and maintenance of alcohol use in women as compared to men (Enoch, 2011; Hyman, Garcia, & Sinha, 2006). The relatively stronger relationship of stress and negative alcohol use outcomes for women as compared to men further supports the necessity of examining the role of various forms of stress in moderating the relationship of gender, age of substance use onset, and telescoping.
Using a nationally representative sample of the U.S. population, the current study examined whether the experience of childhood maltreatment; as defined by physical abuse and serious neglect; moderates age of onset and time from onset of alcohol use to dependence across women and men. We hypothesized that: 1) presence of childhood maltreatment would be associated with earlier age of onset and increased telescoping (decreased time from onset to dependence) for alcohol; and 2) the impact of childhood maltreatment on age of onset and dependence telescoping would be greater for women compared to men.
Methods
Analyses were conducted with Wave 1 (2001–2002; n = 43,093, age 18+) and Wave 2 (2004–2005; n = 34,653) of NIAAA’s National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant, Moore, Shepard, & Kaplan, 2003; Grant & Kaplan, 2005). Participants were included in the current analyses if they completed both Wave 1 and Wave 2 surveys. Demographics, age of onset of substance use, and age of onset of substance dependence was obtained from Wave 1 data. Data regarding childhood maltreatment was obtained from Wave 2.
Measures
Age of onset of drinking, and time to alcohol dependence
To assess age of onset of drinking, respondents were asked, “About how old were you when you first started drinking, not counting small tastes or sips of alcohol?” Lifetime occurrence of DSM-IV alcohol dependence diagnosis, as well as age of onset for dependence, were generated using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) (Grant & Dawson, 2000; Grant et al., 2003). The AUDADIS-IV is a structured psychiatric interview which was conducted face-to-face by trained interviewers for the NESARC. In an analysis of the reliability of the AUDADIS-IV using NESARC data, the test-retest reliability for lifetime alcohol dependence was 0.70 (Grant et al., 2003). We calculated time to dependence as the age of onset of dependence minus the age of onset of drinking. The variables for both age of onset of drinking and time to dependence were Winsor-transformed to reduce the influence of outliers. This procedure iteratively replaces the most extreme value of a variable with the next most extreme value, up to a proportion of values set by the user (e.g., Allwood, Bell, & Horan, 2011; Lobbestael & Arntz, 2010). We conducted this procedure for the most extreme 5% of values.
Childhood maltreatment
Childhood maltreatment was assessed at Wave 2 as part of the posttraumatic stress disorder measure of the AUDADIS-IV. The occurrence of physical abuse was measured with the following item: “Before you were 18 years old, were you physically attacked or badly beaten up or injured by either of your parents or any other people who raised you?” The occurrence of serious neglect was measured with the following item: “Before you were 18 years old, were you seriously neglected by either of your parents or any other people who raised you?” These items were combined into a single binary item, with those who reported either physical abuse or neglect coded as 1, and those who reported neither physical abuse nor neglect coded as 0. For both physical abuse and neglect, a subsequent item assessed the age of first occurrence. Those who started to drink before the first occurrence of physical abuse or neglect (i.e., the outcome occurred before the predictor) were removed from analyses (n=49). The variables selected for childhood maltreatment were restricted to those described above because of limitations within the dataset (for example, despite the assessment of childhood sexual abuse in the NESARC, age of onset was not provided and thus that category of maltreatment was excluded from the analyses). We wanted to ensure that childhood maltreatment occurred prior to the onset of alcohol use, and therefore only included childhood items that provided age of occurrence.
Covariates
When calculating adjusted estimates, our analyses accounted for basic socio-demographic covariates. These included race/ethnicity, household income, and education. Race/ethnicity categories included White/Caucasian, non-Hispanic; Black/African American, non-Hispanic; American Indian/Alaska Native, non-Hispanic; Asian/Native Hawaiian/Other Pacific Islander, non-Hispanic; Hispanic, any race. The household income variable consisted of 21 categories, ranging from “Less than $5,000” to “$200,000 or more.” The education variable included 14 categories, ranging from “No formal schooling” to “Completed Master’s degree or higher graduate degree.” Both household income and education were entered into models as continuous variables.
Analyses
As previously noted, we analyzed data using two sub-samples of the NESARC data: 1) those who reported ever having consumed alcohol, and 2) those that were diagnosed with alcohol dependence at some point in their life. Using data from those who had ever consumed alcohol, we first stratified the sample by gender and computed descriptive statistics for childhood maltreatment and age of first drinking. We then computed three linear regression models: 1) age of onset of drinking on childhood maltreatment and gender, 2) age of onset of drinking on childhood maltreatment, gender, and sociodemographic covariates, and 3) age of onset of drinking on childhood maltreatment X gender, adjusted for sociodemographic covariates. The interaction between childhood maltreatment tested the following null hypothesis:
(Note: AOD = age of onset of drinking and MT = maltreatment).
We repeated these procedures for the sub-sample that was diagnosed with lifetime alcohol dependence, with time from onset of use to dependence as the outcome in all modeling. We used Poisson regression to account for the highly right-skewed distribution of the time from onset of use to dependence variable. This variable appeared to fit a Poisson distribution reasonably well, (mean = 7.50, SD = 8.57, % zeroes = 13.44, max = 55). However, due to minor concerns of over-dispersion, we re-computed all models using negative binomial regression. Results did not vary substantively between the two analyses. Results from Poisson regression are reported below. The sampling design of the NESARC survey was accounted for in analyses, and estimates were weighted to be representative of the U.S. population. Analyses were conducted using Stata version 13.0 (StataCorp, 2013).
Results
Among those who had ever consumed alcohol, 12.9% of women and 24.3% of men met criteria for a lifetime diagnosis of alcohol dependence. Descriptive statistics for those who had ever consumed alcohol and those who had a lifetime diagnosis of alcohol dependence are displayed by gender in Table 1. Among those who had ever consumed alcohol, 5.7% of women and 4.0% of men reported childhood maltreatment that occurred prior to the onset of drinking. Among those with a lifetime alcohol dependence diagnosis, 10.8% of women and 6.6% of men reported childhood maltreatment that occurred prior to the onset of drinking.
Table 1.
Descriptive statistics, by study sub-sample, gender, and childhood maltreatment (yes vs. no)
| Among those who ever drank alcohol (n = 27,524) | Among those with a lifetime alcohol dependence diagnosis (n = 4,054) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Women (n = 14,919) | Men (n = 12,605) | Women (n = 1,608) | Men (n = 2,446) | |||||
| CM = No (n = 14,053) Mean (SD) or % |
CM = Yes (n = 866) Mean (SD) or % |
CM = No (n = 12,042) Mean (SD) or % |
CM = Yes (n = 563) Mean (SD) or % |
CM = No (n = 1,434) Mean (SD) or % |
CM = Yes (n = 174) Mean (SD) or % |
CM = No (n = 2,265) Mean (SD) or % |
CM = Yes (n = 181) Mean (SD) or % |
|
| Age of onset for drinking a | 19.92 (4.07) | 18.95 (4.21) | 18.46 (3.25) | 17.53 (3.319) | 17.60 (3.16) | 17.54 (4.08) | 17.06 (2.45) | 16.32 (2.55) |
| Time from onset of drinking to onset of dependence a | --- | --- | --- | --- | 6.89 (8.00) | 5.96 (7.49) | 6.98 (8.09) | 7.31 (8.45) |
| Race/ethnicity | ||||||||
| W/C, NH | 76.92 | 72.36 | 75.57 | 72.39 | 82.29 | 78.59 | 79.70 | 73.45 |
| B/AA, NH | 10.36 | 11.13 | 9.11 | 6.52 | 7.38 | 7.84 | 6.93 | 6.28 |
| AI/AN, NH | 2.01 | 4.59 | 1.92 | 5.74 | 2.94 | 6.07 | 2.23 | 7.84 |
| A/NaH/PI, NH | 2.47 | 2.02 | 3.37 | 2.01 | 0.76 | 0.56 | 2.43 | 1.28 |
| Hispanic, any race | 8.24 | 9.90 | 10.03 | 13.34 | 6.64 | 6.94 | 8.70 | 11.14 |
| Household income | 10.78 (4.84) | 9.84 (4.65) | 11.50 (4.62) | 10.48 (4.35) | 10.83 (4.89) | 9.42 (4.21) | 11.09 (4.63) | 9.97 (4.16) |
| Education | 9.98 (2.25) | 9.52 (2.01) | 9.88 (2.40) | 9.46 (2.24) | 10.22 (2.05) | 9.63 (1.95) | 9.80 (2.17) | 9.25 (1.82) |
Note: Percentage and mean(SD) estimates accounted for the complex survey design, and were weighted to be representative of the U.S. population. The standard error estimates for all percentages were <0.01. W/C = White/Caucasian, B/AA = Black/African American, AI/AN = American Indian/Alaska Native, A/NaH/PI = Asian/Native Hawaiian, Pacific Islander, NH = non-Hispanic.
Age of onset for drinking and time to alcohol dependence variables were Winsor-transformed for the outermost 5% of outliers.
Annual household income ranged from 0 to 21, “less than $5,000” to “$200,000 or more.” A value of 10 represented “$35,000 to $39,999”, and a value of 11 represented “$40,000 to $49,000.”
Education level ranged from 1 to 14, “no formal schooling” to “completed Master’s degree or higher graduate degree.” A value of 9 represented “completed high school/GED,” and a value of 10 represented “some college (no degree).”
Age of onset of drinking
Prior to adjusting for covariates, the average age of onset of drinking was 19.87 for women and 18.42 for men. This difference was significant (p < 0.001), and remained significant after adjustment for covariates (p < 0.001; Table 2). Prior to adjusting for covariates, those with maltreatment started to drink approximately 1 year earlier than those without maltreatment (b = −0.95, 95% CI = −1.05, −0.86), and this difference remained significant after adjusting for covariates (p < 0.001). The interaction between gender and childhood maltreatment was not significant (p > 0.05).
Table 2.
Linear regression childhood maltreatment and gender in the prediction of age of drinking onset
| Unadjusted estimates b (95% CI) |
Adjusted estimates a b (95% CI) |
Adjusted estimates with interaction a b (95% CI) |
|
|---|---|---|---|
| Childhood maltreatment | |||
| No | Ref. | Ref. | Ref. |
| Yes | −0.95 (−1.05, −0.86)*** | −0.98 (−1.07, −0.87)*** | −1.00 (−1.14, −0.85)*** |
| Gender | |||
| Female | Ref. | Ref. | Ref. |
| Male | −1.46 (−1.51, −1.41)*** | −1.46 (−1.51, −1.41)*** | −1.46 (−1.52, −1.41)*** |
| Childhood maltreatment X Gender | --- | --- | 0.07 (−0.15, 0.29) |
Note: Estimates were calculated using linear regression, accounted for the complex survey design, and were weighted to be representative of the U.S. population.
p < 0.001.
Estimates adjusted for race/ethnicity, household income, and education level.
Time to alcohol dependence
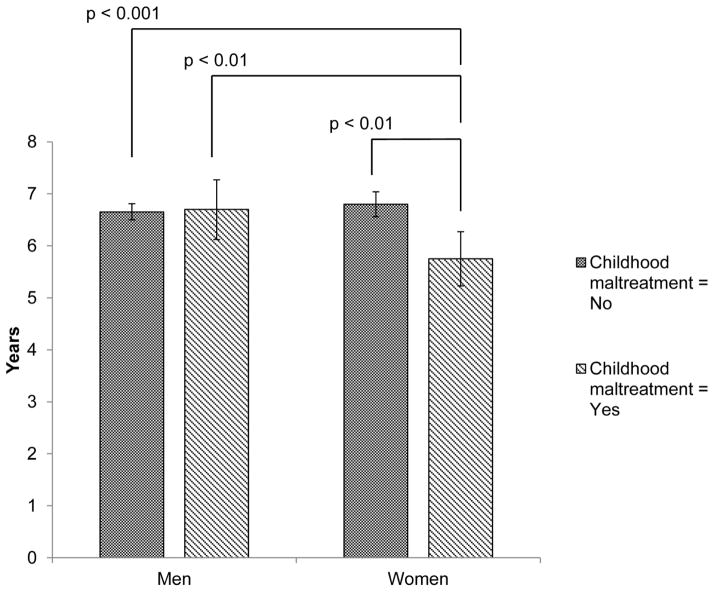
Prior to adjusting for covariates, women had an average of 6.8 years between onset of alcohol use and onset of alcohol dependence. The corresponding figure for men was 7.0 years. This gender difference was not significant (Table 3), and remained so after adjustment for covariates (p > 0.05). Both unadjusted and adjusted associations between childhood maltreatment and time from alcohol use onset to alcohol dependence in the full sample were non-significant. There was a significant interaction between gender and childhood maltreatment, which is displayed in Figure 1. Women with childhood maltreatment developed alcohol dependence approximately 1 year earlier than all other categories (5.8 years vs. 6.8 for women without maltreatment, 6.7 for men without maltreatment, and 6.7 for men with maltreatment). The comparisons between women with maltreatment and the other three categories were all statistically significant after accounting for multiple comparisons. Among women, those with a history of maltreatment developed dependence approximately 15% earlier than those without maltreatment [incidence rate ratio (IRR) = 0.85, 95% CI = 0.76, 0.94]. Among men, there was no difference between those with or without childhood maltreatment (IRR = 1.01, 95% CI = 0.92, 1.10). Among those with childhood maltreatment, women had developed alcohol dependence approximately 14% earlier than men (IRR = 0.86, 95% CI = 0.77, 0.96). This gender difference was not significant among those without childhood maltreatment (IRR = 1.02, 95% CI = 0.98, 1.07).
Table 3.
Modeling results for the prediction of time from onset of drinking to alcohol dependence by childhood maltreatment and gender
| Unadjusted estimates IRR (95% CI) |
Adjusted estimates a IRR (95% CI) |
Adjusted estimates with interaction a IRR (95% CI) |
|
|---|---|---|---|
| Childhood maltreatment | |||
| No | Ref. | Ref. | Ref. |
| Yes | 0.96 (0.89, 1.04) | 0.93 (0.87, 1.01) | 0.85 (0.76, 0.94)** |
| Gender | |||
| Female | Ref. | Ref. | Ref. |
| Male | 1.02 (0.98, 1.06) | 0.99 (0.95, 1.03) | 0.98 (0.94, 1.02) |
| Childhood maltreatment X Gender | --- | --- | 1.19 (1.05, 1.35)** |
Note: Estimates were calculated using poisson regression, accounted for the complex survey design, and were weighted to be representative of the U.S. population. IRR = Incidence rate ratio.
p < 0.01.
Estimates adjusted for race/ethnicity, household income, education level, and age of onset of drinking.
Figure 1.
Time from onset of drinking to alcohol dependence, by gender and childhood maltreatment categories. Estimates were adjusted for race/ethnicity, household income, education level, and age of onset of drinking. Estimates were calculated using Poisson regression, accounted for the NESARC sampling design, and were weighted to be representative of the U.S. population. Error bars represent 95% confidence intervals.
Discussion
Using a large nationally representative dataset, this is the first study to document that childhood maltreatment differentially affect men and women with regard to the time from onset of alcohol use to dependence. Specifically, women demonstrated an accelerated transition from the time of first alcohol use to dependence (telescoping) when they had experienced childhood maltreatment compared to men (with or without childhood maltreatment) or compared to women who did not report childhood maltreatment. Further, our results supported our hypotheses that childhood maltreatment plays an important role in age of drinking onset across the full sample of adults, but this relationship between maltreatment and onset of use was not different between men and women. The previously established findings (Khan et al., 2013; Schuckit, Daeppen, Tipp, Hesselbrock, & Bucholz, 1998) that men have a younger age of onset of use was replicated. Early age of onset is an important factor in predicting long-term risk for deleterious effects of substance use (Brook et al., 2002; DeWit et al., 2000; McGorry et al., 2011; Windle & Windle 2012).
Our findings provide clarity to the conflicting information regarding gender differences in the progression of alcohol use disorders (Hernandez-Avila et al., 2004; Piazza et al., 1989; Randall et al. 1999; Schuckit et al., 1998), and emphasize the importance of examining childhood maltreatment as a moderating variable. Specifically, it was found that childhood maltreatment affects gender-specific telescoping. With no experience of physical abuse or severe neglect, there is little evidence to support a telescoping effect for alcohol use in women. However, with the experience of either physical abuse or severe neglect, telescoping is evident for women only. This latter finding may explain why studies of treatment-seeking and clinical samples have been more likely to find stronger evidence of telescoping effects than population studies (Piazza et al., 1989; Randall et al.,1999), as the prevalence of childhood maltreatment is much greater among these treatment-seeking populations (Langeland & Van Den Brink, 2004).
There is a large body of research describing the profound effects of childhood maltreatment on adulthood health outcomes, health behavior, and psychological functioning (Arnow, 2004). Further, research has suggested a connection between childhood maltreatment and increased risk for the development of alcohol and drug dependence in adulthood (Enoch, 2011). While less is known about the gender effects in the relationship between childhood maltreatment and the time progression to substance dependence, the current findings provide a broad overview of the role of childhood maltreatment in the progression of men’s and women’s alcohol use and demonstrates strong support for a substantial role of childhood maltreatment in the progression of women’s alcohol use. Further, the current findings provide evidence that childhood maltreatment has a significant impact on negative alcohol use outcomes for women, regardless of the severity of the maltreatment, or the type of stressor (physical abuse or severe neglect). The telescoping pattern is concerning because it suggests an acceleration of serious alcohol use related outcomes and less time to intervene. The findings add to the growing literature showing that the experience of childhood maltreatment can have a profound impact on functioning into adulthood.
Implications
The current findings provide strong evidence for the clear need to develop age-appropriate and gender-sensitive prevention strategies for women who have experienced childhood maltreatment. Understanding the role of childhood maltreatment provides a rationale for increased community efforts to provide early primary prevention strategies, and secondary interventions for individuals exposed to childhood maltreatment with an added focus on women, and continued assessment of childhood maltreatment in women seeking substance use treatment. Our study suggests that women with a history of childhood maltreatment are particularly vulnerable to the deleterious effects of alcohol use once exposed, and therefore increased efforts for early intervention is warranted. Early secondary intervention efforts for those with known exposure to childhood maltreatment should provide substance use education and prevention efforts targeted for adolescent women who have been exposed to child maltreatment ideally before the onset of alcohol use. In the effort to identify at risk women before the onset of regular alcohol use, interventions would most appropriately be provided through agencies such as primary care centers, schools, and through state Departments of Children and Families, at which a large breadth of women with exposure to childhood maltreatment could be identified. Tertiary efforts, for women who have initiated drinking and have experienced childhood maltreatment, could be conducted at both the population level and clinical treatment levels. At the population level, interventions might include increased monitoring of drinking through workplaces and interventions provided through healthcare facilities (e.g., Room, Babor, & Rehm, 2005). At the clinical level, increased efforts to understand and improve our treatment of women who have co-occurring alcohol use disorders and exposure to childhood maltreatment (with or without subsequent Post-Traumatic Stress Disorder) may be warranted.”
Limitations
There are limitations that should be noted. First, there is an inherent limitation in the self-report nature of the data and the possibility of recall bias, however, the use of in-depth interviews, and the large sample size all reduce the impact of this limitation Second, childhood maltreatment is likely only one of many variables that may influence the relationship of gender and substance use patterns, additional studies should be conducted integrating research on adulthood stressors, environmental exposure to substances, biological and/or genetic factors, or other potentially mediating variables to continue exploring the phenomenon of telescoping in women. Third, there were limitations of the existing data in that: a) the categories of childhood maltreatment examined in this study were limited by the childhood experiences included in the NESARC which identify age of onset (for example, we were unable to analyze child sexual abuse because age of onset was not provided); b) we were unable to analyze anyone whose use of alcohol or diagnosis of dependence had an onset in between Wave 1 and Wave 2, as age of alcohol use onset was not collected at Wave 2. Age of onset for the childhood maltreatment variable was needed for our analyses to ensure that the maltreatment occurred prior to the onset of alcohol use. Future research should examine broader experiences of childhood maltreatment, severity of maltreatment, chronicity of maltreatment, and also explore the independent role of each of the childhood stressor subtype on the relationship of gender and alcohol use telescoping. Finally, it is still unknown whether the effects of childhood maltreatment on the progression from use to dependence is more pronounced for women in regards to other drug categories (e.g., cannabis, cocaine, nicotine, etc.).
Conclusions
The current study is the first to use a large, epidemiological database to explore the interaction of childhood maltreatment and gender in alcohol use patterns and replication is warranted. The current findings suggest that it is essential to consider both childhood maltreatment and gender in predicting alcohol use progression and developing tailored prevention and treatment interventions.
References
- Afifi TO, Henriksen CA, Asmundson GJG, Sareen J. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Canadian Journal of Psychiatry. 2012;57(11):677–686. doi: 10.1177/070674371205701105. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Mather A, Boman J, Fleisher W, Enns MW, MacMillan H, Sareen J. Childhood adversity and personality disorders: results from a nationally representative population-based study. Journal of psychiatric research. 2011;45(6):814–822. doi: 10.1016/j.jpsychires.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Mota NP, Dasiewicz P, MacMillan HL, Sareen J. Physical punishment and mental disorders: Results from a nationally representative US sample. Pediatrics. 2012;130(2):184–192. doi: 10.1542/peds.2011-2947. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Mota N, MacMillan HL, Sareen J. Harsh physical punishment in childhood and adult physical health. Pediatrics. 2013;132(2):333–340. doi: 10.1542/peds.2012-4021. [DOI] [PubMed] [Google Scholar]
- Allwood Maureen A, Bell Debora J, Horan Jacqueline. Posttrauma Numbing of Fear, Detachment, and Arousal Predict Delinquent Behaviors in Early Adolescence. Journal of Clinical Child & Adolescent Psychology. 2011;40(5):659–667. doi: 10.1080/15374416.2011.597081. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: 2000. text rev. [Google Scholar]
- Arnow BA. Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. Journal of Clinical Psychology. 2004;65(12):10–15. [PubMed] [Google Scholar]
- Benjet C, Borges G, Medina-Mora ME, M’Endez E. Chronic childhood adversity and stages of substance use involvement in adolescents. Drug and Alcohol Dependence. 2012;131(1–2):85–91. doi: 10.1016/j.drugalcdep.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Elsman L, Foote J, Lovejoy M, Wenzel K, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59(11):1039. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Chu DA, Williams LM, Harris AW, Bryant RA, Gatt JM. Early life trauma predicts self-reported levels of depressive and anxiety symptoms in nonclinical community adults: Relative contributions of early life stressor types and adult trauma exposure. Journal of Psychiatric Research. 2012;47(1):23–32. doi: 10.1016/j.jpsychires.2012.08.006. [DOI] [PubMed] [Google Scholar]
- Cui JS, Yip PS, Chau P. Estimation of reporting delay and suicide incidence in Hong Kong. Statistics in Medicine. 2004;23(3):467–476. doi: 10.1002/sim.1604. [DOI] [PubMed] [Google Scholar]
- Dewit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. American Journal of Psychiatry. 2000;157(5):745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Elliott J, Stohl M, Wall M, Keyes K, Goodwin R, Skodol A, Krueger R, Grant B, Hasin D. The risk for persistent adult alcohol and nicotine dependence: the role of childhood maltreatment. Addiction. 2014 May;109(5):842–50. doi: 10.1111/add.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology. 2011;214:17–31. doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Geier T, Keyes K, Skodol AE, Grant BF, Hasin DS. Combined role of childhood maltreatment, family history, and gender in the risk for alcohol dependence. Psychological Medicine. 2013;43:1045–1057. doi: 10.1017/S0033291712001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Henriksen CA, Davidov DM, Kimber M, Pitre NY, Afifi TO. Childhood maltreatment, alcohol use disorders, and treatment utilization in a national sample of emerging adults. Journal of Studies on Alcohol and Drugs. 2013;74:185–194. doi: 10.15288/jsad.2013.74.185. [DOI] [PubMed] [Google Scholar]
- Gordon HW. Early environmental stress and biological vulnerability to drug abuse. Psychoneuroendocrinology. 2002;27(1):115–126. doi: 10.1016/s0306-4530(01)00039-7. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KD. Source and Accuracy Statement: The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61(11):1107. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Gross ST, Huber-Carol C. Regression models for truncated survival data. Scandinavian Journal of Statistics. 1992;19(3):193–213. [Google Scholar]
- Hasin D, Kilcoyne B. Comorbidity of psychiatric and substance use disorders in the United States: Current issues and findings from the NESARC. Addictive Disorders. 2012;25(3):165–171. doi: 10.1097/YCO.0b013e3283523dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis-and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug and Alcohol Dependence. 2004;74(3):265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, Boyd CJ. Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction. 2010;105(12):2130–2140. doi: 10.1111/j.1360-0443.2010.03088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Sinha R. Gender specific associations between types of childhood maltreatment and the onset, escalation and severity of substance use in cocaine dependent adults. The American Journal of Drug and Alcohol Abuse. 2006;32(4):655–664. doi: 10.1080/10623320600919193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EO, Schultz L. Forward telescoping bias in reported age of onset: an example from cigarette smoking. International Journal of Methods in Psychiatric Research. 2005;14(3):119–129. doi: 10.1002/mpr.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27(5):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, Hasin DS. Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry. 2012;200(2):107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, Hasin DS. Telescoping and gender differences in alcohol dependence: new evidence from two national surveys. American Journal of Psychiatry. 2010;167(8):969–976. doi: 10.1176/appi.ajp.2009.09081161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Mclaughlin KA, Koenen KC, Goldmann E, Uddin M, Galea S. Child maltreatment increases sensitivity to adverse social contexts: neighborhood physical disorder and incident binge drinking in Detroit. Drug and Alcohol Dependence. 2012;122(1):77–85. doi: 10.1016/j.drugalcdep.2011.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan SS, Okuda M, Hasin DS, Secades-Villa R, Keyes K, Lin KH, Grant B, Blanco C. Gender differences in lifetime alcohol dependence: Results from the National Epidemiologic Survey of Alcohol and Related Conditions. Alcoholism: Clinical and Experimental Research. 2013;37(10):1696–1705. doi: 10.1111/acer.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein JP, Moeschberger ML. Survival analysis: Techniques for censored and truncated data. New York: Springer; 2003. [Google Scholar]
- Langeland W, Van Den Brink W. Child sexual abuse and substance use disorders: role of psychiatric comorbidity. The British Journal of Psychiatry. 2004;185(4):353. doi: 10.1192/bjp.185.4.353. [DOI] [PubMed] [Google Scholar]
- Lobbestael Jill, Arntz Arnoud. Emotional, cognitive and physiological correlates of abuse-related stress in borderline and antisocial personality disorder. Behaviour Research and Therapy. 2010;48(2):116–124. doi: 10.1016/j.brat.2009.09.015. doi: http://dx.doi.org/10.1016/j.brat.2009.09.015. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Current Opinion in Psychiatry. 2011;24(4):301–306. doi: 10.1097/YCO.0b013e3283477a09. [DOI] [PubMed] [Google Scholar]
- McKee SA, Falba T, O’Malley SS, Sindelar J, O’Connor PG. Smoking status as a clinical indicator for alcohol misuse in US adults. Archives of Internal Medicine. 2007;167(7):716. doi: 10.1001/archinte.167.7.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza NJ, Vrbka JL, Yeager RD. Telescoping of alcoholism in women alcoholics. Substance Use & Misuse. 1989;24(1):19–28. doi: 10.3109/10826088909047272. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Keyes KM, Hasin DS. Adverse childhood events and lifetime alcohol dependence. American Journal of Public Health. 2009;99(2):258–263. doi: 10.2105/AJPH.2008.139006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall CL, Roberts JS, Del Boca FK, Carroll KM, Connors GJ, Mattson ME. Telescoping of landmark events associated with drinking: a gender comparison. Journal of Studies on Alcohol and Drugs. 1999;60(2):252. doi: 10.15288/jsa.1999.60.252. [DOI] [PubMed] [Google Scholar]
- Room R, Babor T, Rehm J. Alcohol and public health. The Lancet. 2005;365(9458):519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:298–304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Daeppen JB, Tipp JE, Hesselbrock M, Bucholz KK. The clinical course of alcohol-related problems in alcohol dependent and nonalcohol dependent drinking women and men. Journal of Studies on Alcohol and Drugs. 1998;59(5):581. doi: 10.15288/jsa.1998.59.581. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- Wei Q, Fentress HM, Hoversten MT, Zhang L, Hebda-Bauer EK, Watson SJ, Seascholtz AF, Akil H. Early-life forebrain glucocorticoid receptor overexpression increases anxiety behavior and cocaine sensitization. Biological Psychiatry. 2012;71(3):224–231. doi: 10.1016/j.biopsych.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Windle RC. Early onset problem behaviors and alcohol, tobacco, and other substance use disorders in young adulthood. Drug and Alcohol Dependence. 2012;121(1):152–158. doi: 10.1016/j.drugalcdep.2011.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]