Abstract
Objective
This study investigated the association of cervical Human Papillomavirus (HPV) infection with cumulative psychosocial risk reflecting family disadvantage, psychological distress, and unhealthy life style.
Methods
The sample (N=745) was comprised of sexually-active female adolescent patients (12-19 years), primarily ethnic minorities, enrolled in a free HPV vaccination program. Subjects completed questionnaires and provided cervical swabs for HPV DNA testing. Unweighted and weighted Principal Component Analyses (PCA) for categorical data were used to derive multi-systemic psychosocial risk indices using nine indicators: low socioeconomic status, lack of adult involvement, not attending high-school/college, history of treatment for depression/anxiety, antisocial/delinquent behavior, number of recent sexual partners, use of alcohol, use of drugs, and dependency risk for alcohol/drugs. The association between cervical HPV (any-type, high risk-types, vaccine-types) assayed by polymerase chain reaction and self-reported number of psychosocial risk indicators was estimated using multivariable logistic regression.
Results
Subjects had a median of three psychosocial risk indicators. Multiple logistic regression analyses showed associations with unweighted and weighted number of psychosocial indicators for HPV any-type (adjusted odds ratio [aOR]=1.1; 95% confidence interval [CI]: 1.0-1.2 ); with the strongest associations between weighted drug/alcohol use, drug/alcohol dependency risk, and antisocial/delinquent behavior and detection of HPV vaccine-types (aOR=1.5; 95%CI: 1.1-2.0) independent of number of recent sexual partners and vaccine dose (0-3).
Conclusion
Increased HPV infections including HPV vaccine-types were associated with greater number of psychosocial risk indicators even after controlling for demographics, sexual behavior, history of chlamydia, and vaccine dose.
Keywords: human papillomavirus, HPV, psychosocial risk, alcohol, drugs, sexual activity, adolescent health
Human Papillomavirus (HPV) infection is the most common sexually transmitted infection (STI) in female adolescents, and is the central cause of cervical cancers and anogenital warts. Rates of both HPV infection and associated disease in the United States are especially high in young women from disadvantaged backgrounds.1,2 While sexual practices (e.g., multiple recent sexual partners) place youth at proximal risk for HPV, effective risk reduction for infection requires a broader understanding of the interrelated, and aggregated, psychosocial influences impinging on adolescent health.3-4
Known family and individual psychosocial factors cluster to produce accumulation of risk that negatively impact adolescent health and development.5-6 Research show that broadly defined psychosocial risk often precedes sexual debut in female adolescents; it occurs together with family disadvantage and other problem behaviors (such as alcohol and substance use and antisocial behavior), and acts in an additive fashion to increase risk for sexually transmitted infection.7,8 For example, in a National Longitudinal Study of Adolescent Health (ADD Health) study of 14,322 young adults between ages 18-27, STI prevalence increased linearly from 4.9% for 0 psychosocial factors to 14.6% for 4 or more (p<.001).9
Focusing on HPV infection and vaccine response in a cohort of disadvantaged female adolescents, we selected a multi-systemic set of individual and family factors previously associated with STI risky practices (multiple sexual partners), compromised emotional/affective responses (depression and anxiety), and unhealthy behavioral lifestyles (alcohol use, drug use, risk for alcohol/drug dependency and antisocial/delinquent conduct).10,11 We included family disadvantage (including socioeconomic burden, lack of adult involvement in the home, and low educational attainment) because it may compromise adolescent health by negatively impacting on youth's emotional and behavioral pathways over the course of development.12 The selection of indicators was informed by work in family disadvantage,12 multiple problem behavior theory,5 and developmental psychopathology.6 This study examined the association of number of psychosocial risk indicators and the detection of cervical HPV in disadvantaged female youth enrolled in a free vaccination program. We hypothesized that it is the aggregate of psychosocial risk indicators rather than the presence of any single indicator that assigns increased risk for HPV infection, independent of vaccine exposure. We also explored the relationship between number of psychosocial risk indicators and prevalence of the vaccine-types targeted by the quadrivalent HPV vaccine (HPV4: 6/11/16/18) adjusting for vaccination exposure (0-3 doses) at study enrollment. While we hypothesized that psychosocial drivers of infection might be independent of HPV type, and that the prophylactic HPV4 vaccine should offer protection regardless of psychosocial risk level, we sought to examine whether youth with higher psychosocial risk might have higher prevalence of HPV infection for vaccine types and other HPV types.
METHODS
Study Subjects
The study sample included 745 female adolescents enrolled between years 2007-2012 in an observational study of the real-world effect of the HPV4 vaccine.2 The cohort was comprised of sexually active, mostly minority (Hispanic 61%, Black or African-American 35%, Other 4%) patients who attended the Mount Sinai Adolescent Health Center in New York City, which offers free integrated medical, sexual and reproductive, mental health, dental, optical, services, and HPV vaccination. Female adolescents were eligible to participate if they: i) were between 12-19 years of age at time of consent, ii) had previously engaged in vaginal or anal intercourse, and iii) intended to get or had already received the HPV4 vaccine. Potential participants who were pregnant at time of enrollment or who had either given birth or terminated a pregnancy within the prior 4-6 weeks were excluded.
Written informed consent, approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai, was collected from all subjects prior to the baseline visit. Enrolled subjects completed self-reported questionnaires that contained questions about demographics, risk behaviors for HPV acquisition, HPV vaccination dosing status/schedule at the time of the baseline visit, and indicators of psychosocial functioning.
Measures
Participant characteristics and sexual practices
Participant characteristics were categorized based on previously published cut-points associated with risk of cervical HPV infection1 and HPV4 vaccine effectiveness.2,13 Self-reported measures included: age, ethnicity (Hispanic, Black or African-American, and Other), history of cigarette smoking, number of lifetime and sexual partners within the last 6 months, use of condoms and oral contraceptives (never used, rarely/sometimes, and most/all of the time), history of other STIs (Chlamydia, Trichomoniasis, Gonorrhea and Syphilis), genital warts and bacterial vaginosis, and HPV4 vaccine dose exposure at enrollment (unvaccinated, 1-2 doses, 3 doses).
Cervical HPV DNA detection
We tested for HPV DNA in cervical specimens collected on all subjects at time of enrollment as previously reported.2 Cervical cells were obtained using a Cytobrush placed in ThinPrep® medium (Hologic Inc, Marlborough, MA) following the same procedure as for Pap smears. DNA extracted from samples was tested using a well-established PCR-based protocol.14-15 Briefly, samples were tested for over 40 HPV types known to infect the mucosal epithelia, including the HPV4 vaccine types (6, 11, 16 and 18) and other cancer-related types, using MY09/MY11 L1 consensus PCR primers, followed by dot-blot hybridization with biotinylated type-specific oligonucleotide probes.16 HPV DNA results were categorized into three overlapping outcome groups: positive for HPV: i) any-type, ii) high risk-types associated with cervical cancer, and iii) HPV4 vaccine-types.
Psychosocial indicators
The nine self-reported single indicators considered were: socioeconomic status (SES), whether an adult is living in the household (representing family support), whether participant attends school or college (reflecting educational attainment), ever treated for depression or anxiety, frequency of alcohol consumption in the past six months (none, <1/week, 1-2 days/week, 3-4 days/week, almost every day), use of drugs in the past six months (never, < once/month, 1-3 times/month, once a wk, 2-3 times/wk, 4-6 times/wk, daily), risk for alcohol or drug dependency (based on the 6-item CRAFFT scale),17 antisocial/delinquent behavior (derived from the 13-item ADD Health Antisocial/Delinquent scale),18 and number of sexual partners in the past six months.
Handling missing data
The percentage of missing data for individual measures and covariates are presented in Tables 1 and 2. Approximately 19% of subjects were incomplete information across the nine index variables, and about 2.2% had samples with insufficient material to detect HPV. It has been shown that analyses using complete case data produce biased and inefficient estimates.19,20 We therefore performed multiple imputation procedures to address missing information. We assumed that data was missing at random (MAR), meaning that the probability of missing values may depend on observed information but is unrelated to the specific missing value itself. We implemented a sequential regression multiple imputation procedure to build an appropriate and flexible imputation model. A total of 10 datasets were imputed for each HPV outcome, and results from the 10 runs were pooled for each analysis using the SAS callable “impute” module of the IVEware software.21
Table 1.
Distribution of socio-demographic characteristics, sexual practices, and vaccination dose
| Complete cases N (%) | % Missing | Multiple imputation† N (%) | |
|---|---|---|---|
| Age category (N=742) | |||
| 12-15 | 57 (7.7) | 57 (7.7) | |
| 16-17 | 232 (31.1) | 0.4 | 234 (31.4) |
| 18-19 | 453 (60.8) | 454 (61.0) | |
| Ethnicity (N=736) | |||
| Hispanic | 448 (60.8) | 453 (60.8) | |
| Black or African-American | 255 (34.7) | 1.2 | 258 (34.6) |
| Other (Asian, White, Other) | 33 (4.5) | 34 (4.6) | |
| Age at sexual debut (N=732) | |||
| <14 | 119 (16.0) | 1.7 | 122(16.3) |
| 14-15 | 348 (47.5) | 355 (47.6) | |
| 16-17 | 231 (31.6) | 235 (31.5) | |
| 18-19 | 34 (4.6) | 34 (4.6) | |
| Recent use of condoms (N=727) | |||
| Never | 88(12.1) | 2.4 | 90(12.1) |
| Rarely/sometimes | 269(37.0) | 275(36.9) | |
| Most of the time | 227(31.2) | 233 (31.2) | |
| Always | 143(19.7) | 148(19.8) | |
| Use of oral contraceptive pill (N=717) | |||
| Never used | 465(64.9) | 3.7 | 483(64.8) |
| Rarely/sometimes | 111(15.5) | 117(15.7) | |
| Most/all of the time | 141(19.7) | 145 (19.5) | |
| History of sexually transmitted infections* | |||
| None | 385/680 (56.6) | 7.3 | 325(43.6) |
| Chlamydia | 233/713 (32.7) | 4.3 | 245(32.8) |
| Trichomoniasis | 42/705 (6.0) | 5.4 | 45(6.0) |
| Gonorrhea | 34/701(4.9) | 5.9 | 36(4.9) |
| Genital warts | 27/699 (3.9) | 6.2 | 28(3.8) |
| Bacterial vaginosis | 120/696 (17.2) | 6.6 | 130(17.5) |
| History of cigarette smoking (N=727) | |||
| Never | 428(58.9) | 439 (58.9) | |
| Yes; no longer | 191(26.3) | 2.4 | 194(26.0) |
| Yes; current | 108(14.9) | 113(15.1) | |
| Vaccination dose at enrollment (N=745) | |||
| Unvaccinated (0 doses) | 144 (19.3) | 0 | 144(19.3) |
| Partial (1-2 doses) | 211(28.3) | 211(28.3) | |
| Full (3-doses) | 390 (52.4) | 390(52.3) | |
| Cervical HPV DNA types | |||
| Any type | 377/729 (51.7) | 2.2 | 385(51.7) |
| High risk-types | 210/729 (28.8) | 2.2 | 214(28.7) |
| HPV4 vaccine-types | 44/729 (6.04) | 2.2 | 45(6.0) |
Table 2.
Definitions and prevalence of psychosocial risk indicators by data source
| Single indicator | Data source | Definition of high risk | ||
|---|---|---|---|---|
| Complete cases N (%) | % Missing | Multiple imputation† N (%) | ||
| Low socioeconomic status | 444/740 (60.0) | 0.7 | 552(74.0) | Positive answer for family or self to any of six items (lifetime): on public welfare, food stamps, Medicaid, WIC, free school lunch, or reported food scarcity “sometimes or often not enough to eat” (Y/N). |
| Lack of adult involvement | 162/745(21.7) | 0 | 162(21.7) | Currently does not live with an adult in the home (Y/N). |
| Not attending school | 104/739(14.1) | 0.8 | 105(14.1) | Currently does not attend school or college (Y/N). |
| Multiple sexual partners | 309/741(41.7) | 0.5 | 311(41.7) | Recent (past 6 months) ≥ 2 vaginal sexual partners. |
| Depression or anxiety | 88/707(12.5) | 5.1 | 92(12.3) | Lifetime (ever) treated for depression or anxiety (Y/N) |
| Use of alcohol | 40/735(5.4) | 1.3 | 41(5.4) | Recent (past 6 months) > 1 drink/week |
| Use of drugs | 162/732(22.1) | 1.7 | 167(22.4) | Recent (past 6 months) > never use of drugs other than alcohol, cigarettes or caffeine. |
| Risk for alcohol or drug dependency | 244/713(34.2) | 4.3 | 260(34.8) | Lifetime (ever) ≥ 2 score in the 6-item CRAFFT1. Alpha coeffcient= .740. |
| Antisocial/Delinquent behavior | 295/664 (44.4) | 10.9 | 358(48.1) | Recent (past twelve months) ≥ 3 score in the 13-item Antisocial/Delinquent scale2. Alpha coefficient= .756 |
| Psychosocial Risk Index (Index9) | 3 (1, 4) | 18.7 | 3 (1, 4) | Median number of unweighted risk indicators out of 9 (interquartile range). |
Developing the psychosocial risk indices
On the basis of above nine single indicators, four composite psychosocial risk indices were derived on the imputed datasets: i) an unweighted binary index, ii) a weighted binary index, iii) a weighted original scale index, and iv) a reduced weighted original scale index (based on eight indicators). The unweighted binary index consisted of responses to the above mentioned single indicators that were dichotomized as 1=high risk; 0=low risk and assigned equal weight (0-9) following an approach by Rutter.6 Binary categories were based on either a conceptual consideration (e.g., receiving a need-based public entitlement) or an established threshold cut-off (e.g., for the CRAFFT and ADD Health scales).17,18 Higher scores indicate higher cumulative risk. Table 2 depicts the definitional criteria used to assign binary risk (high or low). Since some indicators might contribute more than others to risk of HPV, we performed Principal Component Analysis (PCA) for categorical data to create the three weighted indices (ii-iv). This procedure allows for simultaneous quantification of binary, multinomial and continuous scale variables while reducing the dimensionality of the data.22 Standardized scores based on the first component were computed for each participant. The PCA for categorical variables were performed on each of the 10 imputed datasets individually for the three weighted outcome variables. The weights based on first PCA component for the weighted binary index (ii) on HPV any type were: alcohol risk dependency (0.78), drug use (0.67), antisocial behavior (0.61), number of sexual partners (0.42), alcohol use (0.39), history of treatment for depression or anxiety (0.36), low SES (0.18), family structure (0.15), and education (0.07).
The PCA for the weighted original scale index (iii) gave following weights to the indicators: alcohol risk dependency (0.81), drug use (0.73), alcohol use (0.70), antisocial behavior (0.59) and lower weights for number of sexual partners (0.42), history of treatment for depression or anxiety (0.25), family structure (0.18), low SES (0.11), and education (0.06). Lastly, the reduced weighted original scale index (iv) based on eight indicators excluding number of sexual partners was fitted. The PCA first component estimates provided following weights: alcohol risk dependency (0.83), drug use (0.73), alcohol use (0.72), antisocial behavior (0.59), history of treatment for depression or anxiety (0.25), family structure (0.17), low SES (0.11), and education (0.08). The binary and original scale PCAs gave similar weights on the imputed datasets for high-risk HPV and vaccine types. PCA was performed using SPSS v 21 (IBM Corp., Armonk, NY).
Statistical Analyses
Descriptive analyses of both complete case and imputation data are presented. Mean, median, standard deviation, minimum and maximum statistics were used to describe continuous variables. Frequencies and percentages were used to describe categorical variables. Multiple logistic regression was used to estimate the effects of socio-demographic, behavioral, and psychosocial covariates in the detection of HPV any type, high-risk types, and HPV4 vaccine types. Potential confounding variables were screened for in unadjusted models (including sexual activity measures: lifetime and number of sexual partners in the past 6 months, and age at first sexual intercourse), and if associated with the outcomes at the ≤20% level of significance, were included in the multivariate models along with the hypothesized indices. The weighted index on eight psychosocial variables had number of sexual partners in the past 6 months as a covariate in the final model. We present the summaries of the results based primarily on data obtained from the imputation analysis. The process of combining results from different datasets were performed using the SAS callable “regress” module of the IVEware software.21 All other analyses were performed using SAS v9.3 (SAS Institute Inc, Cary, NC).
RESULTS
Study Participants
Distribution of socio-demographic, sexual practices, and vaccination dose patient characteristics by both complete case and multiple imputation summaries are presented in Table 1. The majority of participants (61%) were 18-19 years of age and most were Hispanic (61%) or non-Hispanic Black or African-American (35%). Reflecting the enrollment criteria in this study, all participants were sexually active at the time of enrollment; two-thirds (63%) reported having had vaginal sex before the age of 16, and most (66.6%) reported having three or more lifetime male sexual partners. A third (33%) reported ever having Chlamydia, and almost half (41%) had ever smoked cigarettes. About half of participants (52%) had received all three doses of the HPV4 vaccine at the time of enrollment, while 28% were completing the vaccine series (1-2 doses), and 19% had not yet been vaccinated (0 doses).
Psychosocial Risk Indicators
Five percent (n=40 subjects) had zero risk indicators, 21% had one, 21% had two, 23% had three, 15% had four, 10% had five, and 5% had six or more. Median number of risk indicators was three, with an interquartile range (IQR) from 1 to 4. Seventy-four percent experienced lifetime or current low SES, and nearly half (42%) reported having multiple (>1) sexual partners in the past six months. Risk of drug or alcohol dependency, as measured by the CRAFFT scale, was high (35%), with almost a quarter (22%) reporting having used illicit drugs, and 5% reported consuming alcohol in the past 6 months (refer to Table 2).
To illustrate the interrelatedness of the single psychosocial indicators, we plotted the PCA analysis loading weights for the nine original scale variables for the first three components (Figure 1). Two distinct clusters are discernible, one including alcohol/drug use/risk dependency measures, antisocial/delinquent behaviors and sexual activity, which were heavily loaded on the first principal component (‘dimension 1’), while the second and third dimensions differentiated these indicators from education, family structure, mental health, and low socioeconomic status. The medians and IQR of the standardized weighted binary and original scale scores were −0.22 (−0.85, 0.68) and −0.17 (−0.82, 0.66), respectively.
Figure 1.
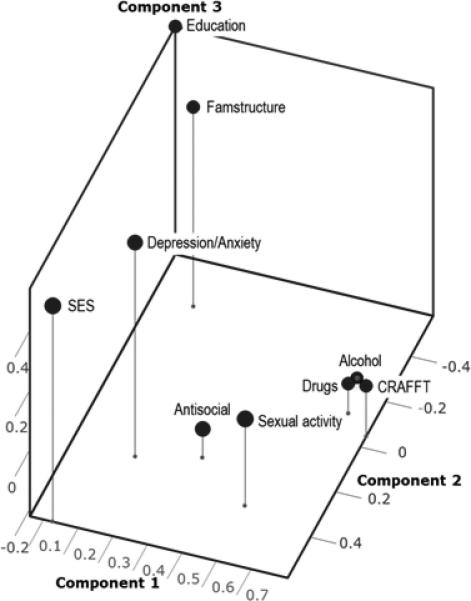
Principal Component Analysis plot (3 components) of the nine psychosocial indicators associated with cervical HPV detection
Association with HPV
We compared the relative increases in odds of detecting any HPV (and by risk type) for the four derived indices: i) unweighted score, ii) weighted score based on binary scale variables, iii) weighted score based on the original scale variables, and iv) weighted score based on eight psychosocial variables with independent adjustment for sexual activity (Table 3). Assuming equal weights (i.e., equal to 1) for each of the nine binary variables in the index, the estimated odds of detecting HPV any type increased 10% with each unit increase in the unweighted index score (p=0.037). In contrast, we observed stronger associations weighted score on original scale variables (p=0.024). The estimated odds of HPV any type infection increased by 19% for a unit increase in unweighted (p=0.037) and weighted psychosocial risk score (p=0.024). The odds of detecting a HPV4 vaccine type specifically increased almost 50% with each unit increase in weighted psychosocial risk score (p=0.007), which remained significant even after separating the proximal risk variable for HPV, number of sexual partners in the past 6 months, from the weighted index, and adjusting for it separately (p=.024).
Table 3.
Adjusted associations between psychosocial risk indices and detection of cervical HPV*
| HPV DNA Group Types‡ |
||||||
|---|---|---|---|---|---|---|
| Psychosocial risk indices | Any-typea | P | High risk-typesb | p | Vaccine-types | p |
| Unweighted index | 1.10 (1.01,1.21) | 0.037 | 1.09 (.98,1.21) | 0.097 | 1.11 (.92,−1.34) | 0.282 |
| Weighted index (binary scale) | 1.16 (1.00,1.35) | 0.056 | 1.13 (0.96,1.33) | 0.150 | 1.25 (0.92,1.70) | 0.148 |
| Weighted index (original scale) | 1.19 (1.02,1.39) | 0.024 | 1.14 (0.97,1.34) | 0.115 | 1.49 (1.12,2.00) | 0.007 |
| Weighted index (original scale eight variables)† | 1.08 (0.92, 1.27) | 0.345 | 1.11 (0.93, 1.31) | 0.234 | 1.42 (1.05, 1.94) | 0.024 |
| Number of recent partners | 1.21 (1.06, 1.37) | 0.002 | 1.04(0.93, 1.17) | 0.446 | 1.09 (0.91, 1.32) | 0.350 |
Pooled adjusted odd ratios (OR) and 95% confidence intervals (CI) across multiple imputation datasets are shown for a unit increase in psychosocial risk index score, adjusted for age, ethnicity, history of chlamydia, and vaccination dose.
Adjusted OR for weighted index based on 8 index variables and number of recent partners modeled as separate variable (also shown).
HPV outcomes:
Any-type.
High risk-types: 16,18,31,33,35,39,45,51,52,56,58,59.
c HPV4 vaccine-types: 6,11,16,18.
All associations were also independent of age, ethnicity, history of chlamydia, and vaccination dose, which were previously shown to be associated with HPV detection in this population.2 Further adjusting for history of age at first sexual intercourse did not modify the observed associations for detection of high-risk and HPV4 vaccine types (not shown). The model based on the weighted eight-psychosocial-variable index revealed that the odds of detecting a HPV4 vaccine type increased 42% with each unit increase in the weighted score beyond the contribution of number of recent partners, which itself was not significant (p=0.350). When compared to the weighted nine-indicator original index, excluding sexual activity resulted in only a 9% reduction in odds of detecting a HPV4 vaccine type with each unit increase in risk score.
DISCUSSION
The majority of women in the U.S. become sexually active between the ages of 15-24,23 and inner-city and minority women are especially at risk for STIs,24 with high prevalence rates seen especially for HPV despite vaccination.2 While it is known that minority adolescents from disadvantaged background and who engage in risky sexual practices are at increased risk of STIs, less is known about the association of these interrelated psychosocial factors taken together and HPV infection risk or vaccine response. We examined the association between cervical HPV-DNA detection and multi-systemic psychosocial risk based on a broadly defined set of psychosocial indicators including family disadvantage (low SES, no adult involvement in the home, not attending school or college), history of depression or anxiety, and risky lifestyle (use of alcohol, use of drugs, risk for alcohol or drug dependency, multiple sexual partners, and antisocial/delinquent behavior).
We found evidence for the association of aggregated psychosocial risk and biologic detection of HPV, with number and intensity of psychosocial risk indicators associated with increased odds of detecting cervical HPV in general, and HPV4 vaccine types in particular, which was independent of vaccine dose exposure and other traditional risk factors for cervical HPV infection. While the pattern of associations for our psychosocial indices (using unweighted and weighted variants) was similar for HPV any type, aggregating and assigning weights to the different indicators revealed which psychosocial risk indicators were relatively more important for predicting cervical HPV detection despite vaccination. Previous studies have shown a correlation between alcohol use and increases in risky sexual activity 8,10,11 and history of other STIs like chlamydia.8,24 Our study expands the current literature by showing an aggregated effect of drug and alcohol use, history of treatment for depression and anxiety, and family background, on the likelihood of cervical HPV infection in female adolescents.
Importantly, when evaluated by PCA, the strongest component weightings were observed with self-reported habitual alcohol use (>1 drink/week) and drug use in the past six months, risk of drug and alcohol dependency, and antisocial/ delinquent behaviors, which were distinct from education, family structure, treatment for depression/anxiety, and low SES. Not surprisingly, sexual activity also clustered with the alcohol and drug related risk behaviors.24 When regressed separately onto detection of HPV4 vaccine types, the eight-variable weighted psychosocial index showed a significant association, independent of number sexual partners in the past 6 months (which was not significant) and number of vaccine doses (which was significant).
The finding that detection of HPV4 vaccine types was associated with increased number of psychosocial indicators independent of number of vaccine doses and recent sexual activity is intriguing and deserves further examination. In this clinic-based study, enrolled youth were already sexually active and at different stages of vaccination course; thus it is not possible to conclude whether female adolescents with high psychosocial risk would benefit more or less from HPV vaccination. More likely, the finding of increased vaccine-type infection may be related to delayed uptake and higher likelihood of previously acquired (pre-existing) HPV4 vaccine type infection before vaccination. Early HPV vaccination (i.e., prior to exposure) is important for the vaccine to be most effective, and necessary given the challenges of predicting onset of sexual activity. Individuals still benefit from vaccination provided that they have not already been infected with all HPV4 vaccine types.25,26 While vaccination is recommended for girls aged 11-12, and catch-up vaccination for females 13-26 years of age, an earlier age (e.g., 9 and 10 years) may be considered for those with high psychosocial risk given that upstream family disadvantage and other individual problem behaviors are often already present prior to sexual debut.27
The study has several limitations. It was not possible to assess individual HPV types associated with cancer (e.g., HPV16/18) or anogenital warts (HPV 6/11) due to the low prevalence of these vaccine types (N=45) to further evaluate the public health implications of the study. While we refer to ‘psychosocial indicators’, we recognize that these are not derived solely from the youth's social environment. Youth's psychological stress response to adversity and risky lifestyles are the result of the complex interplay between genetic susceptibilities and specific social context.28 Furthermore, history of child maltreatment is prevalent in our population,29 which has been associated with widespread consequences including drug and alcohol use, depression and increased risk of STIs.30 Although our results show that cumulative psychosocial risk is associated with HPV infection, independent of vaccination, it was not possible to separate biological effects from environmental influences in our psychosocial risk measures.
There were 19% of incomplete data. Assessment of psychosocial indicators involving sensitive subjects was based on self-reports. Psychological stress, which also directly or indirectly underlies our psychosocial risk indicators was not objectively measured in this study. Thus we could not assess whether stress related to psychosocial risk factors might have affected immune response; a hypothesis that should be further evaluated (e.g., in studies with vaccine type antibody titers). Future studies should consider the contribution of traumatic stress on proximal measures of neuro-endocrinological (i.e., cortisol) stress response,31 and the role of psychological distress in modulating neuro-immunological (e.g., antibody response) function following vaccination.32
Furthermore, while our analyses demonstrated that female adolescents with fewer psychosocial risk factors were less likely to be HPV positive than those with higher number of risk factors, it is premature to propose the utility of our indices as a risk assessment tool;7 further studies are needed to establish a specific threshold number of risk factors above which HPV infection may be predicted with adequate specificity and sensitivity, and should consider additional contextual risk common in disadvantaged youth such as exposure to childhood sexual abuse and intimate partner violence.
Despite above considerations, this study suggests a detrimental role of higher multi-systemic psychosocial risk on cervical HPV, including for HPV4 vaccine types, and points to the need for broad-based approaches in disadvantaged adolescents and young adults at risk of HPV beyond those currently afforded in primary care settings with HPV vaccination programs. In the course of delivering sexual and reproductive health care to high-risk female adolescents, practitioners may assess externalizing behaviors such as alcohol and drug use and antisocial/delinquency, in addition to history of treatment for depression or anxiety, and family disadvantage. Broad-based assessment of these clustered psychosocial risk indicators may expand counseling about healthy choices involving not only sexual decision making, but also psychological well-being, and healthy lifestyles. Furthermore, the early identification of girls at most risk for HPV infection may inform joint decisions by the practitioner, the youth, and her family about the appropriateness of initiating prophylactic HPV vaccination at an earlier age (within the range of approved ages 9-26 years) than currently recommended.
ACKNOWLEDGEMENTS
We thank the participants of this study; Mary Rojas, Yakhira Encarnacion, Tiffany Holder, Whitney Arons, Sophie Soares, Mahelet Kebede and Remy Sanders for their time and effort spent enrolling participants and with data entry; Janae Ostoloza, Sharod McKinney, Anne Dunne, Jennifer Rosenbaum, Thomas Moody and Katerine Kaiser for the HPV genotyping analyses; and Paul Francaviglia, Christine Soghomonian, Mindy Ginsberg, Carlo Garcia and Victor Kamensky for their assistance with data management.
SOURCES OF FUNDING
Funding for this study was provided by the National Institute of Allergy and Infectious Diseases (R01 grant AI072204). Additional funding was provided in part by the Einstein-Montefiore Center for AIDS funded by the National Institutes of Health (AI51519), and the Einstein Cancer Research Center (P30 CA013330) from the National Cancer Institute. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Kahn JA, Lan D, Kahn RS. Sociodemographic factors associated with high-risk human papillomavirus infection. Obstetrics and gynecology. 2007 Jul;110(1):87–95. doi: 10.1097/01.AOG.0000266984.23445.9c. [DOI] [PubMed] [Google Scholar]
- 2.Schlecht NF, Burk RD, Nucci-Sack A, et al. Cervical, anal and oral HPV in an adolescent inner-city health clinic providing free vaccinations. PloS one. 2012;7(5):e37419. doi: 10.1371/journal.pone.0037419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. Journal of public health. 2012 Mar;34(Suppl 1):i3–10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE, Jr, Ross DA, Shek DL. Worldwide application of prevention science in adolescent health. Lancet. 2012;379:1653–64. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. Academic Press; New York: 1977. [Google Scholar]
- 6.Rutter M. Statistical and personal interactions: Facets and perspectives. In: Magnusson D, Allen V, editors. Human development: An interactional perspective. Academic Press; New York, NY: 1983. pp. 295–319. [Google Scholar]
- 7.Dempsey AF, Gebremariam A, Koutsky LA, Manhart L. Using risk factors to predict human papillomavirus infection: implications for targeted vaccination strategies in young adult women. Vaccine. 2008 Feb 20;26(8):1111–1117. 6. doi: 10.1016/j.vaccine.2007.11.088. [DOI] [PubMed] [Google Scholar]
- 8.Sales JM, Brown JL, Vissman AT, DiClemente RJ. The association between alcohol use and sexual risk behaviors among African American women across three developmental periods: a review. Current drug abuse reviews. 2012 Jun;5(2):117–128. doi: 10.2174/1874473711205020117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buffardi AL, Thomas KK, Holmes KK, Manhart LE. Moving upstream: ecosocial and psychosocial correlates of sexually transmitted infections among young adults in the United States. American journal of public health. 2008 Jun;98(6):1128–1136. doi: 10.2105/AJPH.2007.120451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infection in the United States: assessment of differences by race. American journal of public health. 2012 May;102(5):867–876. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanna EZ, Yi HY, Dufour MC, Whitmore CC. The relationship of early-onset regular smoking to alcohol use, depression, illicit drug use, and other risky behaviors during early adolescence: results from the youth supplement to the third national health and nutrition examination survey. Journal of substance abuse. 2001;13(3):265–282. doi: 10.1016/s0899-3289(01)00077-3. [DOI] [PubMed] [Google Scholar]
- 12.Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences. 2010 Feb;1186:37–55. doi: 10.1111/j.1749-6632.2009.05334.x. [DOI] [PubMed] [Google Scholar]
- 13.Markowitz LE, Hariri S, Unger ER, Saraiya M, Datta SD, Dunne EF. Post-licensure monitoring of HPV vaccine in the United States. Vaccine. 2010 Jul 5;28(30):4731–4737. doi: 10.1016/j.vaccine.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 14.Castle PE, Schiffman M, Gravitt PE, et al. Comparisons of HPV DNA detection by MY09/11 PCR methods. Journal of medical virology. 2002 Nov;68(3):417–423. doi: 10.1002/jmv.10220. [DOI] [PubMed] [Google Scholar]
- 15.Qu W, Jiang G, Cruz Y, et al. PCR detection of human papillomavirus: comparison between MY09/MY11 and GP5+/GP6+ primer systems. J Clin Microbiol. 1997 Jun;35(6):1304–1310. doi: 10.1128/jcm.35.6.1304-1310.1997. 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bouvard V, Baan R, Straif K, et al. A review of human carcinogens--Part B: biological agents. The lancet oncology. 2009 Apr;10(4):321–322. doi: 10.1016/s1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 17.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Archives of pediatrics & adolescent medicine. 2002 Jun;156(6):607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 18.ADDHealth Section 29: Delinquency Scale. ( http://www.cpc.unc.edu/projects/addhealth/codebooks/wave1/index.html)
- 19.Raghunathan TE, Lepkowski JM, VanHoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 20.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd ed. Wiley-Interscience; Hoboken, NJ: 2002. [Google Scholar]
- 21.IVEware: Imputation and Variance Estimation Software User Guide [computer program] 2002 [Google Scholar]
- 22.Bartholomew D, Steele F, Moustaki I, Galbraith J. The Analysis and Interpretation of Multivariate Data for Social Scientists. Chapman & Hall CRC Press; Boca Raton, FL: 2002. [Google Scholar]
- 23.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2011. Morbidity and mortality weekly report. Surveillance summaries. 2012 Jun 8;61(4):1–162. [PubMed] [Google Scholar]
- 24.STDs in Racial and Ethnic Minorities. Center for Disease Control and Prevention; 2011. [February 28, 2014]. http://www.cdc.gov/std/stats11/minorities.htm. [Google Scholar]
- 25.Olsson SE, Kjaer SK, Sigurdsson K, et al. Evaluation of quadrivalent HPV 6/11/16/18 vaccine efficacy against cervical and anogenital disease in subjects with serological evidence of prior vaccine type HPV infection. Human vaccines. 2009 Oct;5(10):696–704. doi: 10.4161/hv.5.10.9515. [DOI] [PubMed] [Google Scholar]
- 26.Haupt RM, Wheeler CM, Brown DR, et al. Impact of an HPV6/11/16/18 L1 virus-like particle vaccine on progression to cervical intraepithelial neoplasia in seropositive women with HPV16/18 infection. International journal of cancer. Journal international du cancer. 2011 Dec 1;129(11):2632–2642. doi: 10.1002/ijc.25940. [DOI] [PubMed] [Google Scholar]
- 27.Paul C, Fitzjohn J, Herbison P, Dickson N. The determinants of sexual intercourse before age 16. Journal of Adolescent Health. 2000;27:136–147. doi: 10.1016/s1054-139x(99)00095-6. [DOI] [PubMed] [Google Scholar]
- 28.McEwen BS. Brain on stress: how the social environment gets under the skin. Proceedings of the National Academy of Sciences of the United States of America. 2012 Oct 16;109(Suppl 2):17180–17185. doi: 10.1073/pnas.1121254109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diaz A, Edwards S, Neal WP, et al. The Mount Sinai journal of medicine. 3. Vol. 71. New York: May, 2004. Obtaining a history of sexual victimization from adolescent females seeking routine health care. pp. 170–173. [PubMed] [Google Scholar]
- 30.Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006 Apr;38(4):444, e441–410. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Linares LO, Shrout PE, Nucci-Sack A, Diaz A. Child maltreatment, dating perpetration of physical assault, and cortisol reactivity among disadvantaged female adolescents. Neuroendocrinology. 2013;97(3):252–259. doi: 10.1159/000342958. [DOI] [PubMed] [Google Scholar]
- 32.Miller GE, Cohen S, Pressman S, Barkin A, Rabin BS, Treanor JJ. Psychological stress and antibody response to influenza vaccination: when is the critical period for stress, and how does it get inside the body? Psychosomatic medicine. 2004 Mar-Apr;66(2):215–223. doi: 10.1097/01.psy.0000116718.54414.9e. [DOI] [PubMed] [Google Scholar]


