Dear Editor
King and colleagues recently reported in this Journal their use of electronic syndromic surveillance for the management of surgical infection, highlighting the potential of routine data collection to improve clinical services and inform research within infectious disease practice. [1] The care of patients with infectious diseases is complex and frequently dependent on multi-disciplinary input from infectious diseases physicians, microbiologists and virologists. [2,3] These teams add significant value4 and result in improved patient outcomes and reduced expenditure. [5,6] Data collected on these different aspects of the clinical service are fragmented across patient lists, paper records of phone or clinical consultations, and isolated electronic databases of patients attending specialist outpatient services, such as Outpatient Parenteral Antimicrobial Therapy (OPAT). As a result, routine clinical data are often not collected systematically or in a format that can be interrogated easily to derive meaningful in- sights into teams’ clinical activity.[7] This fragmented data collection creates a barrier to gathering large, prospective datasets that can be used to shape clinical practice, drive audit and facilitate research.[7] This is further compounded by shortcomings in traditional performance metrics, such as length of stay or the number of patients seen in outpatient clinics, which fail to reflect the significant volume of clinical workload provided by infection teams through key services such as ward consultations and antibiotic stewardship.
We developed an integrated clinical data entry system, the electronic Clinical Infection Database (elCID),[8] that allows real-time prospective data collection of clinical activity in our Division of Infection. The database is accessed via a web browser, which allows both multiple user and remote access to elCID whilst storing all information behind the Trust’s secure firewall. The system is used to maintain inpatient lists, record consultations, and track patients seen in specialist clinics such as the OPAT service. Integral to the system is the ability to capture coded entries within all fields, in particular diagnoses, antimicrobials and investiga- tions, thereby facilitating robust prospective data collection.
The main purpose of introducing elCID was to capture the full spectrum of clinical workload across an infection service at a large tertiary referral centre. To that effect, elCID brings together disparate silos of clinical data collection into a single, rapidly searchable database resource permitting unprecedented interrogation of our clinical practice. However, the benefits of the system go further, having vastly improved the quality and transparency of communication between the Division’s teams, audits of day-to-day clinical practice are now rapidly and routinely performed using high quality prospectively collected data, and research study data collection can be conducted within the main database, facilitating improved integration of the clinical and academic arms of the Division. We have provided three case studies to illustrate the impact of elCID.
Case study 1: impact of elCID on division workflow and quality of service delivery
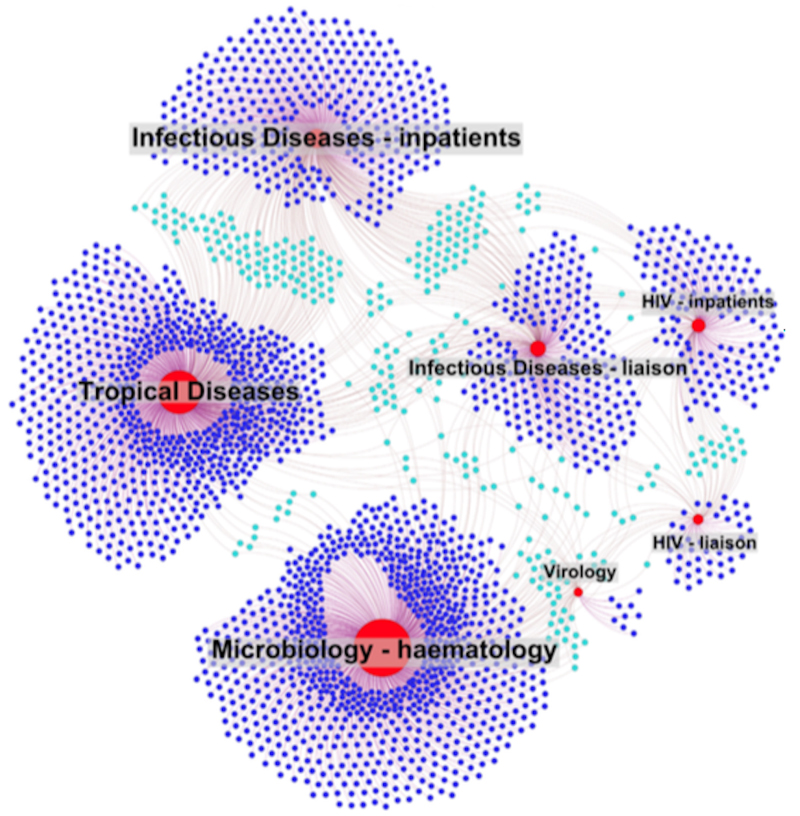
Utilising elCID, we were able to visualise an output of the departmental workload generated in real-time. This permitted us to both quantify our caseload to hitherto unachievable levels of accuracy (Table 1), but also demonstrate the interconnectedness and multidisciplinary nature of care provided to all 2589 patients (Figure 1). This step change in performance metrics has enabled the Division to reassess workload requirements, including the redeployment of junior doctors across our various teams. Concurrently, elCID has also facilitated a number of improvements to the delivery of routine clinical care. Ward- and telephone-based clinical advice is now remotely accessible and searchable. Free-text searching has revealed that around 10% of clinical reviews recommended stopping antimicrobial prescriptions, an intervention difficult to quantify from paper records. In addition, the system can automatically transfer coded clinical information between inpatient and outpatient episodes resulting in significant time-savings across patient’s complete clinical journey.
Table 1.
Summary characteristics of patient population recorded on elCID including sources of underlying infection, cultured organisms and prescribed antimicrobials.
| Age | |
| Median | 50 |
| Min-Max | 0-95 |
| Interquartile range | 34-65 |
| Source of infection | % of patients |
| Urinary tract | 20 |
| Skin & soft tissue | 20 |
| Respiratory | 20 |
| Tropical | 10 |
| Gastrointestinal | 7 |
| Blood stream | 5 |
| Bone + joint | 4 |
| Neurological | 3 |
| Other | 3 |
| Cardiac | 1 |
| Organisms cultured from sterile site | % of cultured organisms |
| Escherichia coli | 19 |
| Pseudomonas aeruginosa | 11 |
| Klebsiella sp | 9 |
| Coagulase negative staphylococcus | 8 |
| Staphylococcus aureus | 8 |
| Enterococcus sp | 5 |
| Alpha haemolytic streptococci | 5 |
| Candida sp | 4 |
| Enterobacter sp | 4 |
| Beta haemolytic streptococci | 2 |
| Streptococcus pneumoniae | 2 |
| Stenotrophomonas sp | 2 |
| Antimicrobials prescribed | % of total antibiotics |
| Piperacillin tazobactam | 17 |
| Meropenem | 8 |
| Co-Amoxiclav | 6 |
| Teicoplanin | 6 |
| Ciprofloxacin | 5 |
| Cefuroxime | 5 |
| Flucloxacillin | 5 |
| Gentamicin | 4 |
| Clarithromycin | 4 |
| Metronidazole | 3 |
| Ceftriaxone | 3 |
| Clindamycin | 3 |
Figure 1.
Network diagram representation of clinical input (edges) into individual patient episodes (blue nodes) by different Infection teams at UCLH (red nodes). Dark blue nodes represent patient episodes involving one clinical team and light blue nodes represent patient episodes involving >one clinical team.
Case study 2: Haematology consult service
Records of the clinical liaison service offered for patients with haematological malignancies had previously been captured on hand-written T-Cards. The switch to elCID has revolutionised our ability to capture and interrogate this dataset. In the first 12 months of elCID use, the haematology service generated 3674 clinical reviews from which clinical advice was offered on 1490 occasions. The clinical reviews also resulted in 799 antimicrobial prescription changes and infection control advice being offered directly during these ward rounds on 362 occasions. These figures are in sharp contrast to attempts to derive such information pre-elCID, namely a time- consuming, manual review of a limited subset of T-cards and subsequent extrapolation from a potentially unrepresentative and biased sample. In addition to the benefits of improved data capture, the system has improved provision of care for this patient cohort. By definition, the previous T-Card based system relied on single user, physical data capture that limited real-time collaborative reviews and clinical input into the care of patients. The switch to elCID has allowed faster, more detailed recording of clinical interactions that are remotely and contemporaneously accessible to clinicians in both microbiology and haematology departments.
Case study 3: integrated clinical research platform
The modular nature of elCID allows research data to be collected alongside routine clinical data, reducing the need for additional research specific databases. User-specific access rights allow additional components of the database to be restricted to clinicians and academics participating in studies whilst simultaneously linking this research data to patients’ underlying routine clinical data. As data are captured prospectively in a coded format, the system provides a platform to identify individuals meeting specified criteria and trigger referral to research nurses or additional data collection. Utilisation of such functionality helps to bridge gaps between provision of clinical care and participation in research, and has specifically been exploited by the Rapid Identification of Respiratory Tract Infection (RiD-RTI) European FP7 project that utilises elCID to both identify eligible patients for the study, as well as anonymously process and record research data collection.[9]
Conclusions
Fragmented data presents a barrier to high quality patient care, service evaluation and research. The development of elCID has resulted in an integrated platform to address these key unmet needs, and its utilisation has provided a platform to both drive clinical service delivery and undertake audit and research. Adoption of elCID, or development of similar solutions, to record clinical activity should be considered widely across other Trusts in the UK with similar visions for data-driven improvement in quality and care delivery.
Funding
This work is supported by NIHR Biomedical Research Centre funding to UCLH and UCL, and by Wellcome Trust Clinical Research Fellowships to MM (WT102807) and GP (WT101766). The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of interest:
DM and CR are employees of Open Health Care UK (OHCUK), the company that designed elCID. The other authors have no financial relationship with OHCUK.
References
- 1.King C, Aylin P, Moore LSP, Pavlu J, Holmes A. Syndromic surveillance of surgical site infectionsea case study in coronary artery bypass graft patients. J Infect. 2014;68:23e31. doi: 10.1016/j.jinf.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Petrak Russell M, Sexton Daniel J, Butera Michael L, Tenenbaum Marvin J, MacGregor Mary C, Schmidt Mary E, et al. The value of an infectious diseases specialist. Clin Infect Dis Off Publ Infect Dis Soc Am. 2003;36(8):1013e7. doi: 10.1086/374245. [DOI] [PubMed] [Google Scholar]
- 3.Bursle EC, Playford EG, Looke DFM. Infectious diseases consultations at an Australian tertiary hospital: a review of 11,511 inpatient consultations. Intern Med J. 2014;44:998e1004. doi: 10.1111/imj.12536. [DOI] [PubMed] [Google Scholar]
- 4.Vehreschild JJ, Morgen G, Cornely OA, Hartmann P, Koch S, Kalka-Moll W, et al. Evaluation of an infectious disease consultation programme in a German tertiary care hospital. Infection. 2013;41(6):1121e8. doi: 10.1007/s15010-013-0512-1. [DOI] [PubMed] [Google Scholar]
- 5.Steven Schmitt, McQuillen Daniel P, Ronald Nahass, Lawrence Martinelli, Michael Rubin, Kay Schwebke, et al. In- fectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;58(1):22e8. doi: 10.1093/cid/cit610. [DOI] [PubMed] [Google Scholar]
- 6.Sharma R, Loomis W, Brown RB. Impact of mandatory inpatient infectious disease consultation on outpatient parenteral antibiotic therapy. Am J Med Sci. 2005;330:60e4. doi: 10.1097/00000441-200508000-00002. [DOI] [PubMed] [Google Scholar]
- 7.De Lusignan S, Hague N, van Vlymen J, Kumarapeli P. Routinely-collected general practice data are complex, but with systematic processing can be used for quality improvement and research. Inf Prim Care. 2006;14:59e66. doi: 10.14236/jhi.v14i1.615. [DOI] [PubMed] [Google Scholar]
- 8.Electronic clinical infection database (elCID) at http://elcid.openhealthcare.org.uk.
- 9.RiD-RTI Rapid identification of respiratory tract infections. at http://www.rid-rti.eu/rid-rti/home_page.