Abstract
[Purpose] This study was performed to investigate the difference in body pressure–related sensory changes between the floor and mattress in a static supine position for physiotherapy research. [Subjects and Methods] To analyze body pressure, the Body Pressure Measurement System was used. Body pressure sensors were attached to mattresses and the floor beneath the subjects. The level of pain was evaluated using pain score tools before the static supine position was adopted, at 1, 5, 10, and 15 min, and in total for specific body points. [Results] In analysis of digitized images, there was no significant difference observed between floor and mattress body pressure values at the start position. However, the head pressure intensity was significantly higher than that of the other body parts. In analysis of pain scores, all body part pain scores except those for both legs were significantly higher for the floor than for the mattress. Furthermore, the pain scores of the floor group were significantly increased at minute 1 compared with those of the mattress group. [Conclusion] These results suggest that properties that change in a time-dependent manner and postural changes need to be carefully considered when applying physical therapy.
Key words: Body pressure, Sensory, Static supine position
INTRODUCTION
The concept of comfort is related to body distribution, firmness, and pain1). Therefore, it is necessary to pay attention to these three elements. In terms of body distribution, the major factor influencing the forces on the body is gravity2). Hence, body pressure is inevitable, and body pressure distribution is a significant concern. In terms of improving patients’ quality of life, in previous research, body pressure distribution has been studied for the prevention of pressure sores3). In addition, the National Pressure Ulcer Advisory Panel (NPUAP) has published guidelines related to the optimal body pressure distribution range, intensity, and time4). In terms of firmness, when lying on the side on a hard mattress, only the hip and shoulder are supported, and the spine is laterally flexed; meanwhile, a soft mattress will cause the hip and shoulder to sink, creating a lateral bend of the spine away from the mattress5). In previous research, objective variables related to firmness and pressure distribution have also been considered relevant to study of the mechanical interaction between the body and support surfaces in car seats6). Pain is subjective, subjectively experienced, and represents a necessary and informative sensory experience that encourages avoidance of danger and recuperative behaviors that promote the healing and protection of an injured or diseased area of the body7, 8). Furthermore, the sensation of pain is an emotional phenomenon that exerts multiple biologic effects, including hyperalgesia, allodynia and others9, 10). Thus, pain is also very important for postural analysis. Therefore, in the definition of comfort, all of these components are important. Physical therapy interventions potentially have targets across all three functioning domains of the International Classification of Functioning (ICF), namely body functions, structures, activities, and participation; in physical therapy, these three components are all important. In addition, they relate to body posture11). However, previous studies have shown that all three of these components are still rare, and this has attracted our attention. Most physical therapy is performed in a static supine position, and thus we have selected this position for our study. The supine position has many advantages, including ease of positioning and greater comfort12). However, few studies have focused on differences in body pressure distribution in relation to environmental variables such as firmness in this position. Moreover, the relationship between body pressure and temporal changes in a physical therapy context in the supine position has not been studied. The purpose of this study was to investigate the three components in terms of the difference in body pressure-related sensory changes between the floor and the mattress in the static supine position for physiotherapy research. We examined subjects’ body pressure using the Body Pressure Measurement System and determined pain scores using the Visual Analogue Scale (VAS), Faces Pain Rating Scale (FPRS), and Iowa Pain Thermometer (IPT).
SUBJECTS AND METHODS
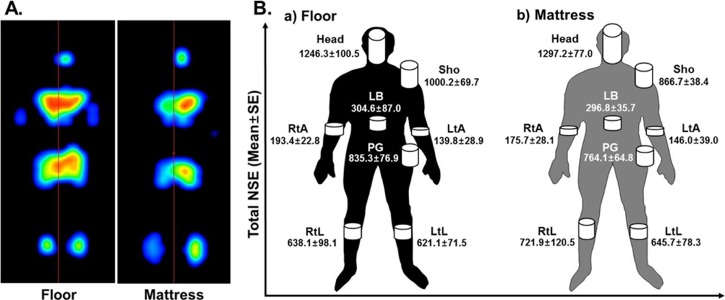
The subjects were ten healthy volunteers (five males, five females) whose mean age, height, and body mass were 29.1±3.2 years, 169.3±10.5 cm, and 63.5±16.2 kg, respectively. The subjects had no skin or musculoskeletal disorders that affected the supine position. Body pressure was measured using the Body Pressure Measurement System (Tech Storm, Republic of Korea)13). This system includes 3,000 sensing elements, and the sensor size of each cell is 20 × 20 mm. The sensor system attaches to mattresses and to the floor beneath the subjects. The system has a monitor that shows high pressures as shades of orange and red and low pressures as shades of blue and green (Fig. 1A). The measured values for particular body parts (head, shoulder, right and left arm, low back, pelvic girdle, right and left leg) were recored13). The subjects had no pain in the measured body parts that could affect this study. The pain scores were evaluated using the VAS, FPRS, and IPT before entering the static supine position, at 1, 5, 10, and 15 min, and in total for the head, shoulder, right and left arm, low back, pelvic girdle, and right and left leg13, 14). All data were expressed as the mean ± standard error (SE) of the measurement. A p value of <0.05 was considered statistically significant. PASW Statistics Version 18.0 (SPSS Inc., Chicago, IL, USA) for Microsoft Windows was used for data analysis in this study. The study’s protocol was approved by the Committee of Ethics in Research at the University of Yongin, in accordance with the terms of Resolution 5-1-20. Furthermore, all volunteers provided informed consent prior to participating in the study.
Fig. 1.
Differences in body pressure after being in the static supine position on the floor and mattress in healthy subjects
Body pressure was measured as described in the Subjects and Methods section. NSE: number of sensing elements; Sho: shoulder; RtA: right arm; LtA: left arm; LB: low back; PG: pelvic girdle; RtL: right leg; LtL: left leg
RESULTS
In analysis of digitized images, the head pressure intensity was found to be significantly higher than the pressure intensities for the other body parts (Fig. 1B). However, we divided the data according to floor and mattress and observed no significant differences (Fig. 1B-a, b). In the VAS, FPRS, and IPT, all body part pain scores except those for both legs were significantly higher for the floor than for the mattress (Table 1). Furthermore, we measured the temporal change in total pain score after maintaining the static supine position for each body part (Table 2). Overall, the pain scores increased at 1 and 5 minute in the static supine position (Table 2). The pain scores (VAS, FPRS, and IPT, respectively) of the floor group were significantly increased at minute 1 compared with the mattress group (Table 2).
Table 1. Differences in pain scale scores after being in the static supine position on the floor and mattress in healthy subjects.
| VAS (score) | FPRS (score) | IPT (score) | ||||||
|---|---|---|---|---|---|---|---|---|
| Floor | Mattress | Floor | Mattress | Floor | Mattress | |||
| Head | 3.0±0.2 | 1.9±0.2* | 3.2±0.2 | 2.1±0.2* | 4.2±0.2 | 2.5±0.3* | ||
| U-Lim | 1.3±0.1 | 0.7±0.1* | 1.7±0.1 | 1.0±0.1* | 2.7±0.1 | 1.5±0.1* | ||
| Sho | 1.5±0.1 | 1.0±0.2* | 2.0±0.1 | 1.3±0.2* | 3.0±0.2 | 1.8±0.2* | ||
| RtA | 1.2±0.1 | 0.5±0.1* | 1.6±0.1 | 0.9±0.2* | 2.5±0.2 | 1.3±0.1* | ||
| LtA | 1.2±0.1 | 0.5±0.1* | 1.6±0.1 | 0.9±0.2* | 2.5±0.2 | 1.3±0.2* | ||
| LB | 2.7±0.2 | 1.7±0.3* | 3.1±0.2 | 1.8±0.2* | 3.9±0.2 | 2.5±0.3* | ||
| L-Lim | 1.8±0.1 | 1.2±0.1* | 2.2±0.1 | 1.6±0.1* | 3.1±0.1 | 1.9±0.1* | ||
| PG | 1.7±0.1 | 1.0±0.2* | 2.2±0.2 | 1.2±0.2* | 3.2±0.2 | 1.7±0.2* | ||
| RtL | 1.8±0.1 | 1.3±0.2 | 2.3±0.1 | 1.8±0.2 | 3.1±0.2 | 2.1±0.2* | ||
| LtL | 1.8±0.1 | 1.3±0.2 | 2.3±0.1 | 1.8±0.2 | 3.1±0.2 | 2.1±0.2* | ||
All data are presented as the mean±SE. VAS: Visual Analogue Scale; FPRS: Faces Pain Rating Scale; IPT: Iowa Pain Thermometer; Sho: shoulder; RtA: right arm; LtA: left arm; LB: low back; PG: pelvic girdle; RtL: right leg; LtL: left leg. *p < 0.05. Statistically significant differences exist for the floor vs. mattress
Table 2. Differences in the time-dependent pain scale scores in the static supine position between the groups.
| VAS (score) | FPRS (score) | IPT (score) | ||||||
|---|---|---|---|---|---|---|---|---|
| Floor | Mattress | Floor | Mattress | Floor | Mattress | |||
| Head 1′ | 1.6±0.2 | 0.0±0.0* | 2.0±0.0 | 0.0±0.0* | 2.5±0.2 | 0.0±0.0* | ||
| 5′ | 2.6±0.3 | 1.8±0.3 | 2.6±0.3 | 1.8±0.2* | 3.8±0.2 | 2.4±0.3* | ||
| 10′ | 3.7±0.2 | 2.6±0.3* | 3.8±0.2 | 2.8±0.3* | 4.8±0.2 | 3.3±0.3* | ||
| 15′ | 4.0±0.2 | 3.3±0.3* | 4.4±0.3 | 3.6±0.3* | 5.5±0.3 | 4.3±0.3* | ||
| U-Lim 1′ | 0.5±0.1 | 0.0±0.0* | 0.9±0.2 | 0.0±0.0* | 1.3±0.1 | 0.0±0.0* | ||
| 5′ | 0.9±0.1 | 0.2±0.1* | 1.7±0.1 | 0.3±0.1* | 2.3±0.1 | 1.1±0.1* | ||
| 10′ | 1.6±0.1 | 1.0±0.1* | 2.0±0.0 | 1.7±0.1* | 3.1±0.2 | 2.1±0.1* | ||
| 15′ | 2.1±0.1 | 1.6±0.1* | 2.3±0.1 | 2.1±0.1 | 4.0±0.1 | 2.6±0.1* | ||
| Sho 1′ | 0.6±0.2 | 0.0±0.0* | 1.2±0.3 | 0.0±0.0* | 1.5±0.2 | 0.0±0.0* | ||
| 5′ | 1.1±0.1 | 0.5±0.2* | 2.0±0.0 | 0.8±0.3* | 2.5±0.2 | 1.4±0.2* | ||
| 10′ | 1.9±0.2 | 1.5±0.2 | 2.0±0.0 | 2.0±0.0 | 3.4±0.4 | 2.6±0.2 | ||
| 15′ | 2.5±0.2 | 2.1±0.3 | 2.8±0.3 | 2.4±0.3 | 4.5±0.3 | 3.2±0.3* | ||
| RtA 1′ | 0.4±0.2 | 0.0±0.0* | 0.8±0.3 | 0.0±0.0* | 1.2±0.2 | 0.0±0.0* | ||
| 5′ | 0.8±0.1 | 0.0±0.0* | 1.6±0.3 | 0.0±0.0* | 2.2±0.2 | 1.0±0.0* | ||
| 10′ | 1.5±0.2 | 0.8±0.1* | 2.0±0.0 | 1.6±0.3 | 2.9±0.2 | 1.8±0.1* | ||
| 15′ | 1.9±0.1 | 1.3±0.2* | 2.0±0.0 | 2.0±0.0 | 3.8±0.2 | 2.3±0.2* | ||
| LtA 1′ | 0.4±0.2 | 0.0±0.0* | 0.8±0.3 | 0.0±0.0* | 1.2±0.2 | 0.0±0.0* | ||
| 5′ | 0.8±0.1 | 0.0±0.0* | 1.6±0.3 | 0.0±0.0* | 2.2±0.2 | 1.0±0.0* | ||
| 10′ | 1.5±0.2 | 0.8±0.1* | 2.0±0.0 | 1.6±0.3 | 2.9±0.2 | 1.8±0.1* | ||
| 15′ | 1.9±0.1 | 1.3±0.2* | 2.0±0.0 | 2.0±0.0 | 3.8±0.2 | 2.4±0.2* | ||
| LB 1′ | 1.3±0.3 | 0.0±0.0* | 1.8±0.2 | 0.0±0.0* | 2.4±0.3 | 0.0±0.0* | ||
| 5′ | 2.4±0.4 | 1.2±0.4* | 2.8±0.3 | 1.0±0.3* | 3.6±0.3 | 2.2±0.4* | ||
| 10′ | 3.2±0.3 | 2.5±0.3 | 3.2±0.3 | 2.9±0.3 | 4.3±0.3 | 3.6±0.4 | ||
| 15′ | 3.8±0.3 | 3.2±0.4 | 4.4±0.3 | 3.1±0.3* | 5.1±0.4 | 4.2±0.4 | ||
| L-Lim 1′ | 0.9±0.1 | 0.0±0.0* | 1.7±0.1 | 0.0±0.0* | 1.9±0.1 | 0.0±0.0* | ||
| 5′ | 1.5±0.1 | 0.9±0.1* | 1.9±0.1 | 1.3±0.2* | 2.8±0.1 | 1.8±0.1* | ||
| 10′ | 2.1±0.1 | 1.5±0.1* | 2.3±0.1 | 2.1±0.2 | 3.5±0.1 | 2.6±0.1* | ||
| 15′ | 2.6±0.1 | 2.3±0.1 | 3.0±0.2 | 2.8±0.2 | 4.2±0.2 | 3.4±0.1* | ||
| PG 1′ | 0.8±0.1 | 0.0±0.0* | 1.6±0.3 | 0.0±0.0* | 1.7±0.2 | 0.0±0.0* | ||
| 5′ | 1.4±0.2 | 0.6±0.3* | 1.8±0.2 | 0.8±0.3* | 2.9±0.3 | 1.6±0.3* | ||
| 10′ | 2.0±0.1 | 1.2±0.3* | 2.4±0.3 | 1.6±0.3* | 3.6±0.3 | 2.4±0.3* | ||
| 15′ | 2.7±0.2 | 2.0±0.3 | 3.0±0.3 | 2.4±0.3 | 4.5±0.3 | 2.9±0.2* | ||
| RtL 1′ | 0.9±0.1 | 0.0±0.0* | 1.8±0.2 | 0.0±0.0* | 2.0±0.1 | 0.0±0.0* | ||
| 5′ | 1.6±0.2 | 1.0±0.2* | 2.0±0.0 | 1.6±0.3 | 2.8±0.2 | 1.9±0.2* | ||
| 10′ | 2.1±0.2 | 1.7±0.2 | 2.2±0.2 | 2.4±0.3 | 3.5±0.3 | 2.7±0.2* | ||
| 15′ | 2.5±0.2 | 2.5±0.2 | 3.0±0.3 | 3.0±0.3 | 4.0±0.3 | 3.6±0.2 | ||
| LtL 1′ | 0.9±0.1 | 0.0±0.0* | 1.8±0.2 | 0.0±0.0* | 2.0±0.1 | 0.0±0.0* | ||
| 5′ | 1.6±0.2 | 1.0±0.2* | 2.0±0.0 | 1.6±0.3 | 2.8±0.2 | 1.9±0.2* | ||
| 10′ | 2.1±0.2 | 1.7±0.2 | 2.2±0.2 | 2.4±0.3 | 3.5±0.3 | 2.7±0.2* | ||
| 15′ | 2.5±0.2 | 2.5±0.2 | 3.0±0.3 | 3.0±0.3 | 4.0±0.3 | 3.6±0.2 | ||
All data are presented as the mean±SE. VAS: Visual Analogue Scale; FPRS: Faces Pain Rating Scale; IPT: Iowa Pain Thermometer; Sho: shoulder; U-Lim: upper limb; RtA: right arm; LtA: left arm; LB: low back; L-Lim: lower limb; PG: pelvic girdle; RtL: right leg; LtL: left leg. *p < 0.05. Statistically significant differences exist for the floor vs. mattress
DISCUSSION
Pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”15, 16). In particular, clinical pain is not simply the consequence of a “switching on” of the “pain system” in the periphery by a particular pathology, but it instead reflects to a substantial extent the state of excitability of the central nociceptive circuits17). In previous research, mattress comfort was investigated by analyzing sensations related to body pressure distribution, but the results showed high variability3, 18,19,20,21). In this study, we analyzed body pressure distribution and subjective sensation according to the environment in a static supine position. In relation to body distribution, we hypothesized that mattress body pressure values would be significantly lower than for the floor. However, there was no significant difference, possibly due to the firmness of the therapeutic mattresses. In addition, we considered the subjective sensation of pain. From another perspective, pain represents individual, physical, and psychosocial factors that should be addressed simultaneously22). To confirm these subjective sensations, we commonly measure the temporal changes in the VAS, FPRS, and IPT pain scales in the static supine position, applying the scales in this order. In our results, pain appeared after 10 min for all measured body parts on a mattress23). On the floor, pain appeared immediately for all measured parts. In addition, there was a significant difference in pain scores between the floor and mattress for most measured body parts. However, as time progressed, the pain scores increased for both the mattress and floor. Subjects could not remain on either surface for more than 15 min. Many suggestions for various situations in physical therapy can be made from our results. First, physical therapy is performed in various environments to relieve pain and restore function. In hospitals and centers, it is carried out on a mattress. Meanwhile, in sports physical therapy situations, it is almost always carried out on the floor. Our results indicate that pain appears almost immediately in the supine position pain and is more intense in firm environments. Therefore, in such a situation, it would be difficult for subjects to focus on the therapy. When applying treatment in firm environments, our results should be considered. Second, most physical therapy is performed with patients maintaining the static supine position for quite a long time, and most of them try to focus on the treatment. Without protective pain sensations, patients may not be conscious of potential tissue damage24). Our results indicate that subjects could not hold a static supine position for over 15 min, either on the mattress or on the floor. However, various physical therapy practices, such as treatment for knee pain and low back pain, take over 15 min in the static supine position to perform. This seems to relate to the therapeutic effect. Therefore, posture control is very important13). In other words, as in our results, when physical therapy is performed in the static supine position to eliminate subjects’ pain, they may in fact feel pain due to a firm environment or long therapeutic period. Thus, it is necessary to consider the proper time, environment, and posture for physical therapy. Moreover, our results should also be considered in relation to treatment of renal failure, such as kidney dialysis, where patients need to maintain a static supine position25, 26). A major limitation of our study is the lack of measurements of other postures. If future studies are performed on another posture, their results could be combined with those of the present research to inform physical therapy practice. Furthermore, further systematic and scientific studies in the fields of pain, rehabilitation and others are needed to confirm the effects of physical therapy10, 27,28,29). In summary, we analyzed the body pressure-related sensory changes and compared them between the floor and mattress in a static supine position. Therefore, when performing physical therapy, the properties of time and posture must be carefully considered13).
REFERENCES
- 1.Scott EM, Baker EA, Kelly PJ, et al. : Measurement of interface pressures in the evaluation of operating theatre mattresses. J Wound Care, 1999, 8: 437–441. [DOI] [PubMed] [Google Scholar]
- 2.Normand MC, Descarreaux M, Poulin C, et al. : Biomechanical effects of a lumbar support in a mattress. J Can Chiropr Assoc, 2005, 49: 96–101. [PMC free article] [PubMed] [Google Scholar]
- 3.López-Torres M, Porcar R, Solaz J, et al. : Objective firmness, average pressure and subjective perception in mattresses for the elderly. Appl Ergon, 2008, 39: 123–130. [DOI] [PubMed] [Google Scholar]
- 4.European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel: Prevention and treatment of pressure ulcers: quick reference guide. Washington DC: NPUAP, 2009. [Google Scholar]
- 5.Gracovetsky SA: The resting spine. A conceptual approach to the avoidance of spinal reinjury during rest. Phys Ther, 1987, 67: 549–553. [DOI] [PubMed] [Google Scholar]
- 6.Gyi DE, Porter JM: Interface pressure and the prediction of car seat discomfort. Appl Ergon, 1999, 30: 99–107. [DOI] [PubMed] [Google Scholar]
- 7.Cole LC, LoBiondo-Wood G: Music as an adjuvant therapy in control of pain and symptoms in hospitalized adults: a systematic review. Pain Manag Nurs, 2014, 15: 406–425. [DOI] [PubMed] [Google Scholar]
- 8.Bolles RC, Fanselow MS: Endorphins and behavior. Annu Rev Psychol, 1982, 33: 87–101. [DOI] [PubMed] [Google Scholar]
- 9.Jamison RN, Edwards RR: Integrating pain management in clinical practice. J Clin Psychol Med Settings, 2012, 19: 49–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee LK, Kim JH, Kim MY, et al. : A review of signal transduction of endothelin-1 and mitogen-activated protein kinase-related pain for nanophysiotherapy. J Phys Ther Sci, 2014, 26: 789–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gómara-Toldrà N, Sliwinski M, Dijkers MP: Physical therapy after spinal cord injury: a systematic review of treatments focused on participation. J Spinal Cord Med, 2014, 37: 371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valdivia Uría JG, Valle Gerhold J, López López JA, et al. : Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol, 1998, 160: 1975–1978. [DOI] [PubMed] [Google Scholar]
- 13.Lee WD, Lee JU, Park J, et al. : Analysis of the body pressure-related sensory changes in the static supine position for healthy science research: a randomized controlled pilot trial. Toxicol Environ Health Sci, 2015, 7: 211–216. [Google Scholar]
- 14.Kim MY, Kim JH, Lee JU, et al. : Temporal change in pain and sensory threshold of geriatric patients after moist heat treatment. J Phys Ther Sci, 2011, 23: 797–801. [Google Scholar]
- 15.Kim JH, Lee JU, Kim IH, et al. : Noxiousness of hypertension-related norepinephrine and upregulation of norepinephrine induced by high intensity electrical stimulation in healthy volunteers. J Phys Ther Sci, 2012, 24: 795–800. [Google Scholar]
- 16.International Association for the Study of Pain: www.iasp-pain.org/Taxonomy, 2014.
- 17.Woolf CJ: Central sensitization: implications for the diagnosis and treatment of pain. Pain, 2011, 152: S2–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Defloor T, De Schuijmer JD: Preventing pressure ulcers: an evaluation of four operating-table mattresses. Appl Nurs Res, 2000, 13: 134–141. [DOI] [PubMed] [Google Scholar]
- 19.Black J, Berke C, Urzendowski G: Pressure ulcer incidence and progression in critically ill subjects: influence of low air loss mattress versus a powered air pressure redistribution mattress. J Wound Ostomy Continence Nurs, 2012, 39: 267–273. [DOI] [PubMed] [Google Scholar]
- 20.Wild D: Body pressures and bed surfaces. Nurs Stand, 1991, 5: 23, 25–27. [DOI] [PubMed] [Google Scholar]
- 21.Nicol K, Rusteberg D: Pressure distribution on mattresses. J Biomech, 1993, 26: 1479–1486. [DOI] [PubMed] [Google Scholar]
- 22.Rithalia SV, Gonsalkorale M: Assessment of alternating air mattresses using a time-based interface pressure threshold technique. J Rehabil Res Dev, 1998, 35: 225–230. [PubMed] [Google Scholar]
- 23.Loeser JD, Melzack R: Pain: an overview. Lancet, 1999, 353: 1607–1609. [DOI] [PubMed] [Google Scholar]
- 24.Scott RG, Thurman KM: Visual feedback of continuous bedside pressure mapping to optimize effective patient repositioning. Adv Wound Care N Rochelle, 2014, 3: 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krasnoff J, Painter P: The physiological consequences of bed rest and inactivity. Adv Ren Replace Ther, 1999, 6: 124–132. [DOI] [PubMed] [Google Scholar]
- 26.Schapira D, Militeanu D, Israel O, et al. : Insufficiency fractures of the pubic ramus. Semin Arthritis Rheum, 1996, 25: 373–382. [DOI] [PubMed] [Google Scholar]
- 27.Hong HS, Lim SV, Son Y: Evaluation of substance-P toxicity with single dose and repeated dose in rats. Mol Cell Toxicol, 2015, 11: 201–211. [Google Scholar]
- 28.Cha HJ, Ahn JI, Jeong JY, et al. : Identification of modulated mRNAs and proteins in human primary hepatocytes treated with non-steroidal anti-inflammatory drugs. Mol Cell Toxicol, 2015, 11: 335–342. [Google Scholar]
- 29.Kim J, Won KJ, Jung SH, et al. : DJ-1 protects against undernutrition-induced atrophy through inhibition of the MAPK-ubiquitin ligase pathway in myoblasts. Life Sci, 2015, 143: 50–57. [DOI] [PubMed] [Google Scholar]