Summary
Purpose
Spasmodic dysphonia (SD) is a rare but often debilitating disease. Due to lack of awareness among practitioners and lack of well-defined diagnostic criteria, it can be difficult for patients with SD to receive a diagnosis and subsequent treatment. There is currently no literature documenting the efficacy of the medical community in recognizing and diagnosing this disorder. We aimed to quantify the patients’ experiences with obtaining a diagnosis of SD.
Methods
One hundred seven consecutive patients with SD completed questionnaires about their experiences with SD. Patients were recruited either during outpatient laryngology visits or during participation in a National Institutes of Health funded study investigating SD.
Results
It took patients an average of 4.43 years (53.21 months) to be diagnosed with SD after first going to a physician with vocal symptoms. Patients had to see an average of 3.95 physicians to receive a diagnosis of SD. Patients (31.4%) had been prescribed medications other than botulinum toxin to treat their symptoms. Patients (30%) attempted alternative therapies for treatment of SD, such as chiropractor or dietary modification.
Conclusions
Despite advances in diagnostic modalities in medicine, the diagnosis of SD still remains elusive. Objective criteria for the diagnosis of SD and increased clinician education are warranted to address this diagnostic delay.
Keywords: Larynx, Voice, Spasmodic dysphonia, Diagnostic delay
INTRODUCTION
Spasmodic dysphonia (SD) is a form of focal dystonia that affects the laryngeal muscles. Patients experience involuntary and sustained contractions of the laryngeal muscles resulting in voice breaks and a strained or strangulated voice. Actions such as swallowing and singing are typically unaffected.1 SD is a chronic, incurable, and disabling voice disorder. Current literature shows that SD typically presents in the 4th or 5th decade of life with a female predominance.1,2
The etiology and pathogenesis of SD is unclear and current treatments provide only temporary relief of symptoms. SD is likely multifactorial in etiology, involving both genetic and environmental factors. A current limitation in our understanding of SD is that there is no systematic method for diagnosing or screening for the disease. Due to this limitation, many patients report complicated and drawn out processes to obtain a diagnosis, and worse still, many patients report being misdiagnosed with psychiatric and psychosomatic disorders to explain their symptoms.1
This study aimed to shed better light on the process of being diagnosed with SD and assess the medical communities effectiveness in diagnosing this disorder.
METHODS
One hundred seven patients were enrolled in the study. Patients were recruited in one of the two ways. First, consecutive patients who were participating in the National Institutes of Health Dystonia Coalition Project 3: Spasmodic Dysphonia Diagnostic and Assessment Procedure at the Emory University Voice Center completed the study questionnaire about their experience with SD. Of the 107 patients, 26 patients were enrolled using this method. All other patients were enrolled during their regularly scheduled outpatient appointments at the Emory University Voice Center. Through this method, 81 consecutive patients answered the study questionnaire.
The initial patient questionnaire used in this study focused on determining several factors regarding patients’ experiences. Patients were asked the length of time it took them to receive a diagnosis after initially seeing a doctor for their symptoms. Patients were also asked how many physicians they had to see before getting a diagnosis of SD and if any of those doctors were neurologists. Finally, patients were asked whether or not they had dystonia in other parts of their body, and if they did, what specific types. During the study, this questionnaire was revised to gather a wider range of information. In the revised questionnaire, patients were also asked at what age did they begin having symptoms and at what age were they ultimately diagnosed. Patients were also asked if they had been prescribed any medications other than botulinum toxin, as well as if they had tried any alternative therapies (ie, chiropractor, diet, and so forth) to treat their symptoms.
Statistical analysis was performed using SPSS (IBM, Cambridge, MA, USA) software. Mean values for length of time to diagnosis, the number of physicians seen, and the average age of onset were calculated. The percentage of patients prescribed medications other than Botox, who tried alternative therapies, and who saw a neurologist was determined. Finally, gender analysis was performed.
All patients signed consent forms before participating in the study. All questionnaires and consents were approved by the Institutional Review Board of Emory University.
RESULTS
Of the 107 patients enrolled, 80.4% were female and 19.6% were male. It took patients an average of 53.21 months or 4.43 years (σ = 79.4 months) after first seeing a physician for their symptoms to be ultimately diagnosed with SD. These patients saw an average of 3.95 (σ = 3.9 physicians) physicians before being diagnosed. Average age of symptom onset was 44.65 years (σ = 13.6 years). Only 33.6% of patients had seen a neurologist.
Patients (31.4%) were prescribed a medication other than Botox to treat their symptoms. As seen in Figure 1, a total of 15.6% of patients were prescribed antianxiety medication and 9.4% were prescribed acid reflux medication. Thirty percent of patients tried alternative therapies to alleviate their symptoms. Figure 2 shows that 6.8% saw a chiropractor, whereas 3.4% tried to alter their diet. Patients (24.4%) reported having a dystonia in another part of their body with cervical dystonia, 14.1%, being the most common.
FIGURE 1.
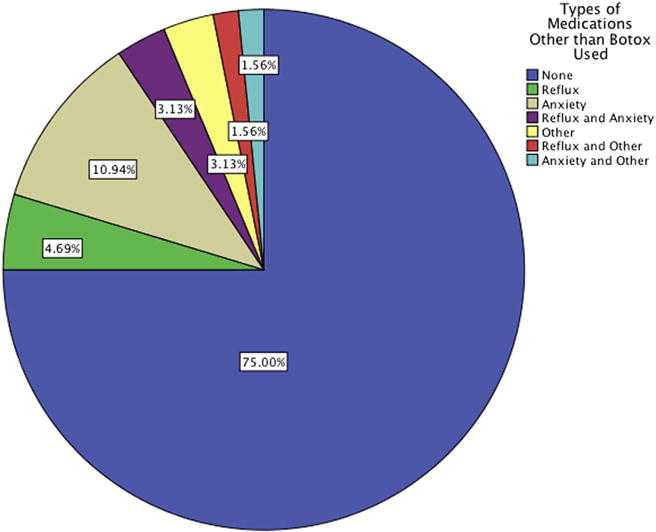
Medications other than Botox prescribed to treat patient’s SD symptoms.
FIGURE 2.
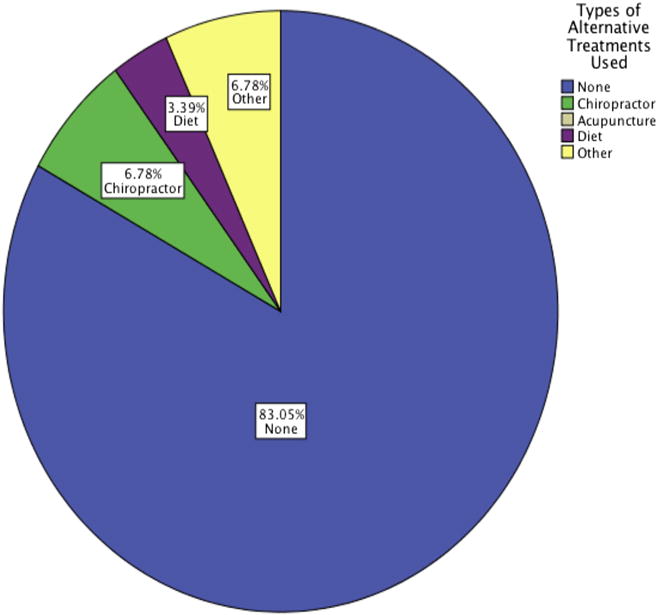
Alternative treatments tried by SD patients to alleviate symptoms.
DISCUSSION
Our study shows that there is a substantial delay in the diagnosis of SD. Patients reported an average of almost 4.5 years from the time they first sought treatment until ultimate diagnosis. This period is obviously too long. This delay is not only too long for patients, who struggle with the social and professional difficulties of SD symptoms, but from a larger public health perspective, this delay wastes health care resources. Patients reported seeing an average of almost four physicians while seeking a diagnosis, which wastes both health care resources as well as patients’ time. Although seeing multiple physicians is a waste of resources and money, more importantly, patients are often, over 30% of the time, exposed to medications unnecessarily. Although prescriptions such as acid reflux medications are likely benign, over 15% of patients were prescribed antianxiety medications, which carry serious medical side effects and addiction potential.
To improve patient care, safety, and streamline the use of precious health care resources, we believe that greater education among clinicians on the signs and symptoms of SD is needed to improve the delays in diagnosis. Although data were not collected specifically looking into which type of physicians patients saw before obtaining a diagnosis from an otolaryngologist, it is likely that most of these patients saw their primary care physician at some point during their diagnostic journey. Therefore, education should not focus on otolaryngologists alone but also on primary care providers and internist to help facilitate triage toward appropriate providers.
The remainder of the data from this study provides further information on the epidemiology of SD. Just over 80% of our patients were female, which is similar to the previous studies.1 The average age of onset was 44.65 years, which was slightly younger than what most previous studies report.1–3 There was a wide standard deviation (σ = 13.6 years) for the average age of onset and wide range in age of onset, from 9 to 70 years, which might explain the small differences seen from previous literature.
Interestingly, the percentage of patients reporting a secondary dystonia other that SD was high, almost 25%. Most patients reported having cervical dystonia, 14.1%, whereas 2.6% reported having writer’s cramp. These numbers are different from previous reports, which indicate that writer’s cramp is the most common focal dystonia in patients with SD.3 Although these differences are small, the important implication from this data is that clearly SD is related to other forms of dystonia. Although almost 25% of our patients reported having a second dystonia, the national prevalence has been reported anywhere from 0.280% to 0.03%, clearly indicating a relationship.4,5
The information from this study can help inform clinicians in the diagnosis of SD. The epidemiologic information provides clinicians expected age ranges, average age of 44.65 years, and gender disparities, 80% female predominance, related to SD. Furthermore, the data show that multiple different medications patients have been prescribed inappropriately for SD symptoms, and, therefore, clinicians should think of SD as a possibility in patients with voice complaints who do not respond to reflux or antianxiety medications. Finally, a large percentage of patients, almost 25% of patients had a secondary dystonia. Investigating whether a patient with voice complaints has a dystonia can alert clinicians to patients with a higher likelihood of having SD.
Although it is easy to blame these delays on physicians, it is important to note that because no objective diagnostic criteria exist for SD, it is extremely difficult for physicians, even otolaryngologists and neurologists, to provide definitive diagnosis. The current diagnostic criteria are subjective and based on individual practitioners interpretation of examination findings. We believe these results underscore the fact that objective criteria and procedures for diagnosis of SD are greatly needed to improve diagnostic delays in SD.
CONCLUSIONS
There are multiple results from this study, but we believe that they all add to the small and growing fund of knowledge on the epidemiology and natural history of SD, which has been designated as a priority in SD research.1 Furthermore, we believe that our results elucidating the delays in diagnosis of SD shed light onto an ongoing dilemma for both patients and physicians alike. Objective criteria for the diagnosis of SD and increased clinician education are greatly needed to address this diagnostic delay.
Acknowledgments
This research was supported in part by NIH Grant # NS065701.
References
- 1.Ludlow CL, Adler CH, Berke GS, et al. Research priorities in spasmodic dysphonia. Otolaryngol Head Neck Surg. 2008;139:495–505. doi: 10.1016/j.otohns.2008.05.624. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schweinfurth JM, Billante M, Courey MS. Risk factors and demographics in patients with spasmodic dysphonia. Laryngoscope. 2002;112:220–223. doi: 10.1097/00005537-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Sharma N, Franco RA., Jr Consideration of genetic contributions to the risk for spasmodic dysphonia. Otolaryngol Head Neck Surg. 2011;14:369–370. doi: 10.1177/0194599811411656. [DOI] [PubMed] [Google Scholar]
- 4.Jankovic J, Tsui J, Bergeron C. Prevalence of cervical dystonia and spasmodic torticollis in the United States general population. Parkinsonism Relat Disord. 2007;13:411–416. doi: 10.1016/j.parkreldis.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Stacy M. Epidemiology, clinical presentation, and diagnosis of cervical dystonia. Neurol Clin. 2008;26(suppl 1):23–42. doi: 10.1016/s0733-8619(08)80003-5. Review. [DOI] [PubMed] [Google Scholar]


