Abstract
Background
Limited English proficiency is associated with disparities across diverse health outcomes. However, evidence regarding adverse birth outcomes across languages is limited, particularly among US Asian and Pacific Islander populations. The study goal was to consider the relationship of maternal language to birth outcomes using statewide hospitalization data.
Methods
Detailed discharge data from Hawai‘i childbirth hospitalizations from 2012 (n=11,419) were compared by maternal language (English language or not) for adverse outcomes using descriptive and multivariable log-binomial regression models, controlling for race/ethnicity, age group, and payer.
Results
Ten percent of mothers spoke a language other than English; 93% of these spoke an Asian or Pacific Islander language. In multivariable models, compared to English speakers non-English speakers had significantly higher risk (adjusted relative risk [ARR]: 2.02; 95% Confidence Interval [CI]: 1.34–3.04) of obstetric trauma in vaginal deliveries without instrumentation. Some significant variation was seen by language for other birth outcomes, including an increased rate of primary Caesarean sections and vaginal births after Caesarean among non-English speakers.
Conclusions
Non-English speakers had approximately two times higher risk of having an obstetric trauma during a vaginal birth when other factors, including race/ethnicity, were controlled. Non-English speakers also had higher rates of potentially high-risk deliveries.
Keywords: English proficiency, birth outcomes, obstetric trauma, Asian, Pacific Islander
Significant health disparities have been associated with lack of English proficiency across a variety of health outcomes, including health status and access to preventive care (DuBard et al. 2008; Ponce et al. 2006). Yet empirical evidence regarding adverse birth outcomes across maternal language is extremely limited, particularly among Asian and Pacific Islander populations in the United States (US). Previous research on linguistic challenges in the delivery setting has primarily focused on Hispanic populations (Pope 2005).
Understanding linguistic-related factors among US Asian and Pacific Islander populations is important due to the high rates of limited English proficiency (LEP) in many of these populations (US Census Bureau 2003). Overall, 39% percent of all US Asian and Pacific Islanders report LEP compared to 8% of the total US population (Association of Asian Pacific Community Health Organizations 2005). Rates of LEP have been considerably higher within some US Asian and Pacific Islander subgroups. For instance, 58% of Chinese, 66% of Vietnamese, and 60% of Korean speakers report LEP (US Census Bureau 2003; Tu et al. 2008).
Considering the relationship between linguistic outcomes and birth outcomes is a critical topic for research, policy, and clinical practice. Childbirth is the most frequent reason women are hospitalized in the US, responsible for 1 out of every 5 female hospitalizations (4.7 million stays in 2008) (Healthcare Cost and Utilization Project, 2010). Hospitalizations for childbirth in the US are expensive—totaling $14.8 billion in 2006 (U.S. Department of Health and Human Services, 2010) and, despite the generally good health of women hospitalized for childbirth, US maternity care has suffered from poorer than expected outcomes generally (Elixhauser & Wier 2011; Sakala & Corry 2008). Childbirth has thus been identified as a national priority area for health care quality improvement (Adams & Corrigan 2003).
One line of evidence would suggest that linguistic disparities are likely to be seen in birth outcomes among US Asian and Pacific Islanders. While birth outcomes are understudied across Asian American and Pacific Islander subgroups, the limited research on this topic has revealed poor maternal health outcomes for some Asian American and Pacific Islander populations (Centers for Disease Control and Prevention 2011; Russo et al. 2008; Rao et al. 2006; Wong et al. 2008; Qin & Gould 2006; Fuentes-Afflick & Hessol 1997). Many of these differences are not explained by the typically used risk or sociodemographic factors (Baker et al. 2007; Le et al. 1996).
Linguistic factors may explain some of these differences. As US Asian and Pacific Islanders speak over 100 languages and dialects, barriers to linguistically appropriate care present a major health care issue for some of these populations (Ro 2002). It can be challenging for a health care system to provide the needed full linguistic access across multiple domains, including face-to-face clinical care, laboratory testing, and hospitalizations (Karliner et al. 2007). Research in other countries has found that the clinical use of interpreters decreased Caesarean section rates (Small et al. 1999) and obstetrical interventions (Parson & Day 1992) for LEP patients, suggesting that linguistic barriers play a role in poorer birth outcomes.
However, another line of research has suggested that linguistic disparities may not be seen in birth outcomes among US Asian and Pacific Islanders. A literature primarily focused on Spanish speakers in the US has demonstrated low rates of adverse birth outcomes among some disadvantaged (primarily Hispanic) immigrant groups (Hoggatt et al. 2012; Pope, 2005; Gould et al. 2003). While considerable debate exists about the reasons for these paradoxical findings, a core finding of this literature was that some non-English speaking women showed surprisingly good birth outcomes (Hoggatt et al. 2012; Pope 2005; Gould et al. 2003).
The goal of the present study was to begin to address this gap in the literature regarding the role birth outcomes by language for US Asian and Pacific Islanders. Specifically, we sought to quantify adverse birth outcomes by maternal language in a location with substantial Asian and Pacific Islander populations. Our primary study hypothesis was that we would see significantly more adverse birth outcomes for those who spoke languages other than English.
However, we were also cognizant of the evidence suggesting that this might not be the case (Hoggatt et al. 2012; Pope, 2005; Gould et al. 2003). Thus, we considered an additional issue. Major linguistic barriers exist in the diagnosis and management of chronic conditions (Karliner et al. 2007). Diabetes and gestational diabetes are present in a significant number of pregnancies among US Asian and Pacific Islanders, and poor management of glucose intolerance can lead to worse birth outcomes (Rosenberg et al. 2005). Thus, study outcomes were run among the full sample and specifically among women with pre-gestational and gestational diabetes to consider whether English language was related to birth outcomes among those specifically managing a chronic condition during their pregnancy. Our secondary study hypothesis was that, even if we did not see significantly more adverse birth outcomes for those who spoke languages other than English among mothers generally, we would see poorer birth outcomes among those with a chronic condition who spoke a language other than English compared to those with the same condition who spoke English.
Methods
Location
The study was conducted in Hawai‘i, which is home to 29% of the total US Native Hawaiian or other Pacific Islander population (US Census Bureau 2012) and where over 50% of the population identifies as Asian (US Census Bureau 2011). Over one fourth of the state’s adult population (28%) speaks a language other than English, with only half of those reporting speaking English “very well” (Hawaii Economic Issues 2011). This provided a substantial sample of Asian and Pacific Islander linguistic groups for analysis.
Data
Hawai‘i Health Information Corporation’s (HHIC) inpatient database from 2012 was used (HHIC 2013). The HHIC inpatient database is Hawai‘i’s all-payer, all-visit, all-hospital inpatient data. Hospital data are submitted to HHIC monthly by all hospitals in the state. Data elements included patient race/ethnicity, age, sex, insurer, length of stay, and diagnosis (based on International Classification of Diseases – 9th revision – Clinical Modification (ICD-9) codes) (Centers for Disease Control and Prevention 2012). The HHIC inpatient database had identifiers that linked mothers to newborns and included a unique patient identifier for individuals across all hospitals. HHIC data are used as the Hawai‘i data source for the major national inpatient administrative database (Health Care Cost and Utilization Project 2014).
Samples
The study sample included all maternity delivery-related hospitalizations across the hospitals in Hawaii that included language proficiency data in 2012. We began with the 15,908 total vaginal or Caesarean delivery-related hospitalizations in Hawai‘i in 2012. The cases for which race/ethnicity data were missing (556) were excluded. From the 15,352 remaining cases, we selected unique maternal records, excluding multiply identical maternal records due to delivering twins or more babies (n=244). We also excluded two records with “miscellaneous” payer type as these could not be readily categorized. Finally, we also excluded any records for which language was “not collected” or “unknown/undermined/refused” (n=3,687). Thus, the total study sample was 11,419 (71.8% of total vaginal or Caesarean delivery-related hospitalizations). This comprised the sample used for maternal-focused outcomes. The sample for neonatal outcomes was identical to the sample for maternal outcomes, with the exception that multiple births due to delivering twins or more babies were not excluded. After using the same exclusions otherwise as listed above, the newborn sample was 11,546. For analyses of outcomes among those with diabetes, from the total study sample, we included only those diagnosed with pre-gestational and gestational diabetes using ICD-9 codes as discussed below, n=1,149 or 10.1% of the total study sample.
Variables
Language Use
Preferred language has not been traditionally part of administrative data collection in hospitals in Hawai‘i or in the US generally. However, due to the linguistic diversity of Hawai‘i, a number of hospitals have been collecting these data in advance of meaningful use requirements on this topic (Centers for Medicare and Medicaid Services 2013). These include the four hospitals on Oahu that make up more than 70% of civilian deliveries. Collection of these data has been phrased as “language of preference” or “preferred language spoken” and has been collected at intake. The language use variable used in analyses was a dichotomous measure of those who indicated that English was their language of preference versus those who selected another language. “Other” languages included Ilocano, Tagalog, Visayan, Mandarin, Cantonese, Chuukese, Marshallese, Tongan, Samoan, Hawaiian and Japanese. Because collection of language preference data was voluntary by hospital, some hospitals had language data “not collected.” The hospitals that did not collect these data were known to vary from those that did (e.g., more rural). Thus, we specifically considered differences between the hospitals that included language and the hospitals whose data were excluded from our study to consider our study results in light of these differences.
Gestational and Pre-gestational Diabetes
This was a dichotomous measure indicating women who had a diabetes diagnosis, measured by ICD-9 (250, 648.00, 648.01, 648.02, 648.03, 648.04, 648.80, 648.81, 648.82, 648.83, 648.84) and was used to stratify the analysis to consider outcomes among women with this chronic condition.
Outcome Variables
We considered a variety of outcome measures based on outcomes shown to vary by race/ethnicity or language use in previous research on this topic (Russo et al. 2008; Rao et al. 2006; Wong et al. 2008; Qin & Gould, 2006; Fuentes-Afflick & Hessol 1997; Coffey et al. 2005).
Maternal Outcomes
Maternal outcomes included Agency for Healthcare Research and Quality (AHRQ) maternal-specific inpatient quality indicators (1. Caesarean delivery rate; 2. Primary Caesarean delivery rate; 3. Vaginal Birth After Caesarean (VBAC) rate, uncomplicated; and 4. VBAC, all) and three AHRQ maternal-specific inpatient safety measures indicators (Obstetric trauma rate from: 1. Caesarean delivery, 2. Vaginal delivery without instrument, and 3. Vaginal delivery with instrument). These are widely used indices for birth outcomes (Sedman et al. 2005) and were measured using published guidelines (AHRQ 2013).
We also considered severity of illness (SOI) by type of birth within the All Payer Refined Diagnostic Related Groups (APR-DRG) developed by 3M (Wallingford, CT; 3M 2003), which examine “the extent of physiological decomposition or organ system loss of function” within APR-DRG (AHRQ 2011). The 3M severity-of-illness classification method considers primary and secondary diagnoses and procedures from (ICD-9-CM) discharge codes, as well as age, sex, and discharge disposition (AHRQ, 2011). Possible illness severity scores ranged from 1 to 4, with higher scores indicating greater severity (AHRQ, 2011). SOI was measured within four APR-DRG groups 540 (Caesarean delivery), 541 Vaginal Delivery w/ Sterilization &/or D&C, 542 (Vaginal Delivery w/ Complicating Procedures Excluding Sterilization &/or D&C), and 560 (Vaginal Delivery).
Gregory et al. (2009) proposed that a useful metric, easily calculated and readily understood by health care consumers, would be lack of complications in delivery. We used their published guidelines to calculate this “ideal delivery” (ID) rate, which indicated lack of complications (Gregory et al. 2009), by language use.
Neonatal Outcomes
Neonatal outcomes were preterm delivery (defined from Medicare Severity Diagnosis- Related Groups) (MS-DRGs: 790, 791 and 792), low birth weight (less than 2500g) (Centers for Disease Control and Prevention 2014), and macrosomia (greater than 4000g) (Chatfied 2001) as well as the AHRQ neonatal-focused patient safety indicator: birth trauma, injury to neonate (AHRQ 2013).
Control Variables
In multivariable models, we controlled for age group (<18, 18–34, 35+ years), payer (Public, Private, DOD, and Self-Pay), hospital location (urban vs. rural), and race/ethnicity (Filipino, Micronesian, Native Hawaiian, Japanese, Chinese, White, Other Pacific Islander, Other Asian, and race/ethnicity (including Black and Hispanic). Race/ethnicity was identified from the HHIC race/ethnicity variable created from race/ethnicity categories available consistently across all hospitals in Hawai‘i (HHIC 2013). Race/ethnicity data were typically provided by patient self-report at intake and included only one primary race. Mixed-race individuals were represented by self-report of their primary race of identification.
Hospital location was from a standard variable available in the HHIC data established in concordance with the payer community to be consistent with insurers’ classifications of hospitals in the state. Using this variable, two small community-based hospitals on the island of Oahu that are located outside urban Honolulu were designated “rural” as were all hospitals on other Hawaiian islands (i.e., Maui, Kauai, Hawai‘i island). All other hospitals were designed “urban.” Multiple gestation was included as a control variable in the neonatal outcomes and was measured by ICD-9 (651). We also controlled for mother being high risk, which was calculated based on existing metrics (Gregory et al. 2009).
Statistical Analyses
Our primary study hypothesis was that we would see poorer birth outcomes for those who spoke languages other than English vs. those who spoke English. Our secondary study hypothesis was that we would see poorer birth outcomes by language specifically among women with diabetes. To test these, we first summarized outcomes and control variables in descriptive statistics for language and compared by language using Chi-squared tests or Fisher’s exact tests (for categorical variables) and analysis of variance (ANOVA) or Kruskal-Wallis tests, if the normality assumption was not satisfied (for continuous variables).
Multivariable log-binomial regression models estimated rate ratios (RR) for all study outcomes, except SOI, comparing non-English speakers to English speakers with 95% confidence intervals (CI), adjusting for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation. For models for SOI, which had four outcome levels (SOI: 1–4), we used proportional odds models (ordered logistic regression) comparing non-English speakers to English speakers with 95% confidence intervals (CI), also adjusting for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation. These logistic regression models provided odds ratios (OR) indicating the odds of a one-level increase of SOI. For the multivariable models among those with diabetes, high risk was not included because diabetes was one of the determinants of high risk so that all respondents fell into this category. Multivariable models were only run in which we had more than 10 cases with the outcome. The overall goodness of fit of the models was assessed by Pearson chi-square statistic, and individual parameters were tested by Wald chi-square statistic. Significance was set at p≤ 0.05. All analyses were performed in SAS 9.3 (2011; Cary, NC: SAS Institute, Inc.). The study protocol was deemed exempt by the University of Hawai‘i Institutional Review Committee.
Results
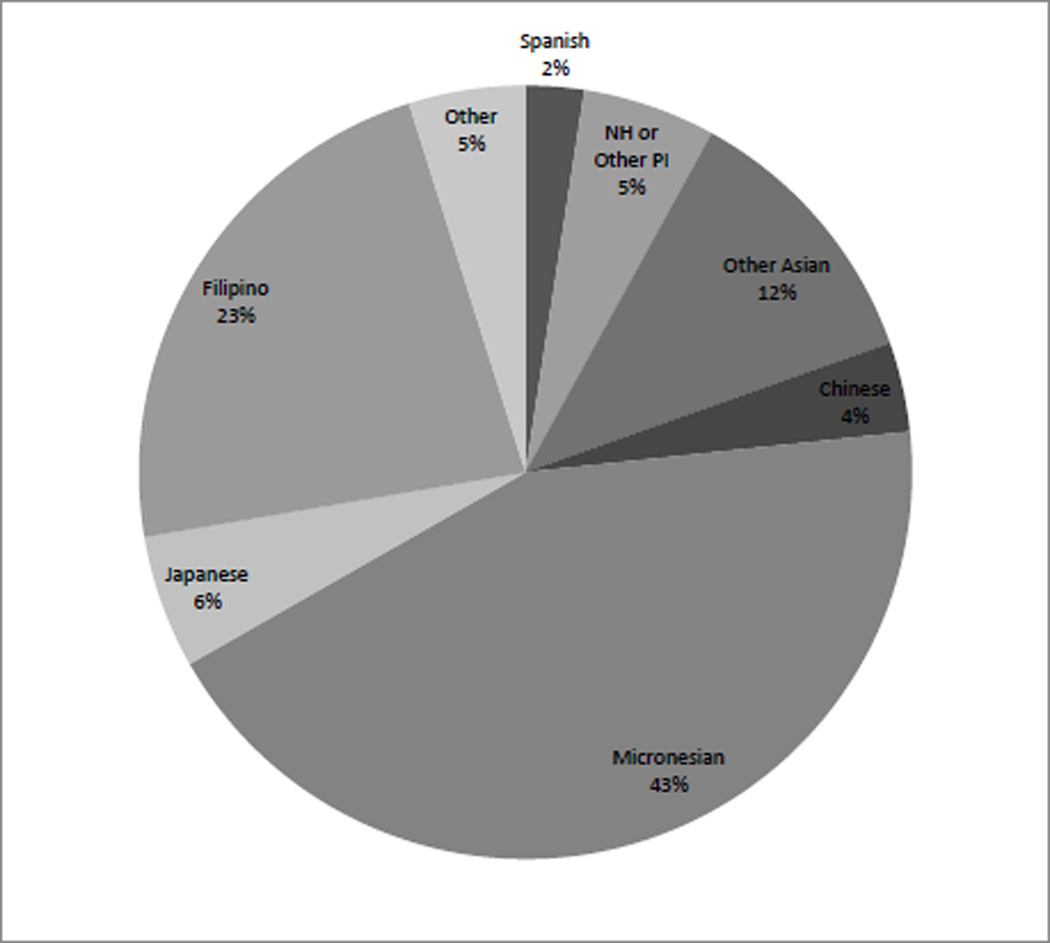
Non-English speakers were significantly (p<0.001) more likely to be Micronesian or other race/ethnicity and significantly less likely to be Japanese, White, and Native Hawaiian; Chinese and Filipino and Other Pacific Islander groups were represented similarly in both groups (Table 1). Payer varied significantly across English language use, but age group and hospital location (urban vs. rural) did not. Frequency of multiple gestation did not differ significantly across language groups. Non-English speakers were significantly (p=0.002) less likely to have a high-risk pregnancy (37% vs 42%; p=0.003). The most frequently spoken non-English languages were Micronesian (e.g., Marshallese, Chuukese), making up 43% of the non-English speaking population (Figure 1). Filipino languages (e.g., Tagalog, Ilocano, Visayan) were the next most frequent, making up 23% of the non-English speaking population. Overall, 93% of the non-English languages spoken were from Asian or Pacific regions.
Table 1.
Demographics by English Language Use in Hawai‘i Maternity-Related Hospitalizations, 2012 (n=11,419)1
| Total | ||||
|---|---|---|---|---|
| n | 11,419 | |||
| English Speaker | ||||
| Yes | No | |||
| n (% of sample) | 10,270 (89.9%) | 1,149 (10.1%) | ||
| n (%) | n (%) | p | ||
| Age group, years | ||||
| <18 | 179 (1.7%) | 14 (1.2%) | 0.191 | |
| 18–34 | 8,058 (78.5%) | 895 (77.9%) | 0.657 | |
| 35+ | 2,033 (19.8%) | 240 (20.9%) | 0.379 | |
| Race/Ethnicity | ||||
| Chinese | 370 (3.6%) | 46 (4.0%) | 0.492 | |
| Filipino | 2,211 (21.5%) | 263 (22.9%) | 0.288 | |
| Hawaiian | 2,500 (24.3%) | 6 (0.5%) | <0.001 | |
| Japanese | 1,246 (12.1%) | 66 (5.7%) | <0.001 | |
| Micronesian | 199 (1.9%) | 500 (43.5%) | <0.001 | |
| Other | 1,130 (11.0%) | 173 (15.1%) | <0.001 | |
| Other PI | 612 (6.0%) | 76 (6.6%) | 0.376 | |
| White | 2,002 (19.5%) | 19 (1.7%) | <0.001 | |
| Payer | ||||
| Dept. of Defense | 481 (4.7%) | 2 | <0.001 | |
| Private | 6,138 (59.8%) | 368 (32.0%) | <0.001 | |
| Public | 3,592 (35.0%) | 694 (60.4%) | <0.001 | |
| Self-Pay | 59 (0.6%) | 80 (7.0%) | <0.001 | |
| High Risk3 | ||||
| Yes | 4,260 (41.5%) | 424 (36.9%) | 0.003 | |
| Hospital | ||||
| Urban | 9,252 (90.1%) | 1,022 (88.9%) | 0.222 | |
| Multiple Gestation | ||||
| Yes | 196 (1.9%) | 14 (1.2%) | 0.099 | |
P-values were based on chi-square test or Fisher’s exact test for categorical variables.
Number of observations <10 (too small to report due to data privacy rules).
High risk was defined based on previous research (Gregory et al, 2009).
Figure 1.
Non-English Language Speakers by Language for Maternity Visits in 2012 in Hawaii (n=1,149).
Maternal Outcomes
In unadjusted maternal outcome analyses (Table 2), significant differences were seen by language. Specifically, non-English speakers had significantly higher Caesarean delivery rates compared to English speakers (15% vs. 12% respectively, p=0.011) and also had significantly higher obstetric trauma rates, vaginal delivery without instrument (4.8% vs. 2.8% respectively, p=0.002). Non-English speakers also had significantly lower rates on the “ideal delivery (ID) rate” (lack of complications measure) (75% vs. 79%; p=0.003), indicating they had deliveries with significantly more complications. Non-English speakers also had significantly higher rates of Vaginal Birth After Caesarean (VBAC), all (34% vs. 23% respectively, p <0.001) and VBAC, uncomplicated (36% vs. 24%, respectively, p<0.001), compared to English speakers. Other tested maternal outcomes did not vary significantly by maternal language.
Table 2.
Unadjusted and Adjusted Maternal Outcome Comparisons by English Language Use in in Hawai‘i Maternity-Related Hospitalizations, 2012 (n=11,419)1
| Total | Multivariable Model2 |
||||
|---|---|---|---|---|---|
| n | 11,419 | ||||
| English Speaker | P value |
Non English speakers (vs. English speakers) |
|||
| Yes | No | ||||
| n (% of sample) | 10,270 (89.9%) | 1,149 (10.1%) | |||
| n (%) | n (%) | P | RR [95% CI] | ||
| Maternal Quality Indicators | |||||
| Caesarean delivery rate | 1,911 (20.7%) | 234 (22.7%) | 0.137 | 1.02 [0.88, 1.17] | |
| Primary Caesarean delivery rate | 934 (11.7%) | 127 (14.7%) | 0.011 | 1.18 [0.96, 1.45] | |
| Vaginal Birth After Caesarean, all | 324 (22.7%) | 65 (34.2%) | <.001 | 1.02 [0.75, 1.40] | |
| Vaginal Birth After
Caesarean, Uncomplicated |
318 (23.7%) | 64 (36.0%) | <.001 | 1.03 [0.75, 1.41] | |
| Obstetric Trauma Rate - C-section | 3 | 3 | 4 | ||
| Obstetric Trauma Rate -
Vaginal Delivery Without Instrument |
204 (2.8%) | 36 (4.8%) | 0.002 | 2.02 [1.34, 3.04] | |
| Obstetric Trauma Rate -
Vaginal Delivery With Instrument |
91 (18.6%) | 28 (25.9%) | 0.087 | 1.48 [0.96, 2.28] | |
| No Delivery Complications | |||||
| ID Rate | 8,108 (78.9%) | 864 (75.2%) | 0.003 | 0.97 [0.93, 1.01] | |
| Mean (SD) | Mean (SD) | P | OR [95% CI] | ||
| SOI within APR-DRGs | |||||
| 540 (Caesarean delivery) | 1.54 (0.71) | 1.58 (0.73) | 0.395 | 0.99 [0.72, 1.35] | |
| 541 (Vaginal Delivery w/ Sterilization &/or D&C) |
1.50 (0.65) | 1.52 (0.68) | 0.879 | 0.95 [0.43, 2.12] | |
| 542 (Vaginal Delivery w/ Complicating Procedures Exc Sterilization &/or D&C) |
1.73 (0.73) | 1.64 (0.50) | 0.614 | 1.61 [0.23, 11.3] | |
| 560 (Vaginal Delivery) | 1.56 (0.64) | 1.59 (0.62) | 0.179 | 1.11 [0.93, 1.34] | |
P-values were based on two –sample t-tests for continuous variables; Chi-square tests or Fisher’s exact tests for categorical variables.
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation.
Number of observations <10 (too small to report due to data privacy rules).
Not enough observations (<10) to run multivariable models.
In multivariable models for maternal outcomes (Table 2), significant differences by maternal language remained only for obstetric trauma, vaginal delivery without instrument with a twofold increased risk for non-English speakers (RR: 2.02; 95% CI: 1.34–3.04). Detailed results from the full maternal outcome models are available in Appendix 1. Race/ethnicity was significantly associated with all maternal outcomes except for Caesarean delivery rate and severity of illness for APR-DRG 541 and 542. Compared to Whites, Micronesians had higher VBAC and Caesarean delivery rates in adjusted models and greater odds of severity of illness for Caesarean deliveries and vaginal deliveries. Native Hawaiians had significantly lower rates of primary Caesarean deliveries and greater odds of severity of illness for vaginal deliveries. Filipinos had greater odds of severity of illness for both Caesarean deliveries and for vaginal deliveries. Other Pacific Islanders had greater odds of severity of illness for vaginal deliveries.
Other factors that were significantly associated across multiple (though not necessarily all) multivariable models were age group, payer, high risk, and location. These relationships varied in direction depending on the outcome. Mothers in the younger age groups were significantly more likely than older women to have obstetric trauma and significantly less likely to have a Caesarean delivery. Compared to those with private insurance, those with a public payer had significantly greater odds of severity of illness during a Caesarean delivery, but were significantly less likely to have a primary Caesarean delivery or an obstetric trauma for vaginal, delivery without instruments. Women with high risk were significantly more likely to have a Caesarean delivery and greater odds of severity of illness in all tested APR-DRG groups. They were also significantly less likely to have a VBAC or a delivery without complications. Those who delivered at rural hospitals (compared to urban hospitals) had lower odds of severity of illness for Caesarean and vaginal deliveries, were significantly more likely to have a Caesarean delivery and a delivery without complications, and were significantly less likely to have a VBAC.
Neonatal Outcomes
In infant-focused outcomes (Table 3), non-English speakers were significantly less likely to have babies with macrosomia (4.9% vs. 6.8%). However, this difference did not remain statistically significant in multivariate models (p=0.055). No significant differences were seen in descriptive results by language for preterm delivery, low birth weight, or birth trauma, injury to neonate. Detailed results from the full neonatal outcome models are available in Appendix 2. Other factors significantly related in multiple multivariable models (though not necessarily all models) to neonatal outcomes were age group, race/ethnicity, high risk, and multiple gestation. Mothers under 18 years of age were significantly more likely to have a baby with low birth weight than those 35 years or older. Women with high risk and those with multiple gestation were significantly more likely to have all four of the poor neonatal outcomes. Those who delivered at rural hospitals (compared to urban hospitals) were significantly less likely to have a premature baby.
Table 3.
Unadjusted and Adjusted Infant-Focused Outcome Comparisons by English Language Use in Hawai‘i Delivery Hospitalizations, 2012 (n=11,546)1
| Total | Multivariable Model2 | ||||
|---|---|---|---|---|---|
| N | 11,564 | ||||
| English Speaker | P value |
Non English speakers
vs. English speakers |
|||
| Yes | No | ||||
| N (% of sample) | 10,404 (90.0%) |
1,160 (10.0%) |
|||
| n (%) | n (%) | P | RR [95% CI] | ||
| Baby Outcome | |||||
| Birth Trauma - Injury to Neonate | 29 (0.3%) | 3 | 1 | 0.72 [0.16, 3.25] | |
| Premature | 928 (8.9%) | 109 (9.4%) | 0.590 | 1.08 [0.90, 1.30] | |
| Low Birth Weight | 909 (8.7%) | 112 (9.7%) | 0.296 | 1.11 [0.85, 1.45] | |
| High Birth Weight | 704 (6.8%) | 57 (4.9%) | 0.016 | 0.72 [0.52, 1.00] | |
P-values were based on Chi-square tests or Fisher’s exact tests for categorical variables
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation.
Number of observations <10 (too small to report due to data privacy rules).
The direction of significant racial/ethnic findings varied on the outcome. Compared to Whites, Chinese women were less likely to have a baby with macrosomia. Japanese women were significantly more likely to have a baby with low birth weight and significantly less likely to have one with macrosomia. Filipinos were significantly more likely to have a premature baby or one with low birth weight, but were significantly less likely to have a baby with macrosomia. Micronesians were significantly more likely to have a premature baby or one with low birth weight. Other Pacific Islanders were significantly more likely to have a premature baby or one with macrosomia.
Diabetes Outcomes
Among women with diabetes, demographic patterns by language followed patterns seen in the overall sample (results not shown). In descriptive analyses, significant differences were seen among those with diabetes for the primary Caesarean delivery rate, with rates being significantly higher for those who did not speak English (28%) compared to those who did (17%) (p=0.017) (Table 4). VBACs were also considerably more frequent in the non-English speakers than in the English speakers (39% vs 15% respectively; p=0.003). These differences did not retain statistical significance in multivariate models (Appendix 3).
Table 4.
Unadjusted and Adjusted Outcome Comparisons by English Language Use in Hawai‘i Maternity-Related Hospitalizations among those with Diabetes, 2012 (n=1,355)1
| Diabetes Sample | Multivariable Model2 | ||||
|---|---|---|---|---|---|
| n | 1,355 | ||||
| English Speaker | P value |
Non English speakers (vs. English speakers) |
|||
| Yes | No | ||||
| n (% of sample) | 1,226 (90.5%) | 129 (9.5%) | |||
| n (%) | n (%) | p | RR [95% CI] | ||
| Maternal Quality Indicators | |||||
| Caesarean delivery rate | 337 (31.2%) | 37 (32.7%) | 0.742 | 0.91 [0.65, 1.28] | |
| Primary Caesarean delivery rate | 149 (17.3%) | 25 (27.5%) | 0.017 | 1.30 [0.83, 2.03] | |
| Vaginal Birth After Caesarean, all | 39 (15.1%) | 10 (38.5%) | 0.003 | 1.83 [0.83, 4.01] | |
| Vaginal Birth After
Caesarean, Uncomplicated |
37 (15.7%) | 10 (41.7%) | 0.002 | 1.96 [0.89, 4.30] | |
| Obstetric Trauma Rate - C-section | 3 | 3 | 3 | 4 | |
| Obstetric Trauma Rate -
Vaginal Delivery Without Instrument |
16 (2.1%) | 3 | 0.089 | 4 | |
| Obstetric Trauma Rate -
Vaginal Delivery With Instrument |
12 (26.1%) | 3 | 0.692 | 4 | |
| No Delivery Complications | |||||
| ID Rate | 989 (80.7%) | 100 (77.5%) | 0.392 | 0.96 [0.86, 1.07] | |
| Mean (SD) | Mean (SD) | p | OR [95% CI] | ||
| SOI within APR_DRGs | |||||
| 540 (Caesarean delivery) | 1.54 (0.71) | 1.58 (0.73) | 0.395 | 0.95 [0.48, 1.88] | |
| 541 (Vaginal Delivery w/
Sterilization &/or D&C) |
1.50 (0.65) | 1.52 (0.68) | 0.879 | 4 | |
| 542 (Vaginal Delivery w/ Complicating Procedures Exc Sterilization &/or D&C) |
1.73 (0.73) | 1.64 (0.50) | 0.614 | 4 | |
| 560 (Vaginal Delivery) | 1.56 (0.64) | 1.59 (0.62) | 0.179 | 1.18 [0.70, 2.00] | |
| n (%) | n (%) | p | RR [95% CI] | ||
| Baby Outcomes | |||||
| Birth Trauma | 3 | 3 | 0.540 | 4 | |
| Premature | 182 (14.7%) | 18 (13.7%) | 0.778 | 0.72 [0.43, 1.21] | |
| Low Birth Weight | 127 (10.2%) | 19 (14.5%) | 0.131 | 1.30 [0.80, 2.12] | |
| High Birth Weight | 119 (9.6%) | 12 (9.2%) | 0.876 | 0.96 [0.47, 1.95] | |
P-values were based on two –sample t-tests for continuous variables; Chi-square tests or Fisher’s exact tests for categorical variables.
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, and multiple gestation.
Number of observations <10 (too small to report due to data privacy rules).
Not enough observations (<10) to run multivariable models.
Comparison of Missing Data
Because so many hospitalizations were missing language information, we compared the sample missing language data to those reporting language data (Table 5). Most starkly, a far greater majority of data with language included were from urban hospitals. This revealed primarily that rural hospitals did not report language data. Additionally, hospitalizations included in the analysis sample (compared to those excluded) were by those who were older, had lower percentages of public insurance and of Whites and Native Hawaiians, and had higher percentages of private insurance and high risk pregnancies.
Table 5.
Demographic Information by Language Not Missing vs. Language Missing in Total Hawai‘i Maternity-Related Hospitalizations, 2012 (n=15,106)
| Language Included | Language Missing | |||
|---|---|---|---|---|
| n (% of sample) | 11,419 (75.6%) | 3,687 (24.4%) | ||
| n (%) | n (%) | p | ||
| Age Group, years | <.001 | |||
| <18 | 193 (1.7%) | 80 (2.2%) | 0.057 | |
| 18–34 | 8,953 (78.4%) | 3,008 (81.6%) | <0.001 | |
| 35+ | 2,273 (19.9%) | 599 (16.2%) | <0.001 | |
| Race/Ethnicity | <0.001 | |||
| Chinese | 416 (3.6%) | 115 (3.1%) | 0.133 | |
| Filipino | 2,474 (21.7%) | 588 (15.9%) | <0.001 | |
| Hawaiian | 2,506 (21.9%) | 1,070 (29.0%) | <0.001 | |
| Japanese | 1,312 (11.5%) | 320 (8.7%) | <0.001 | |
| Micronesian | 699 (6.1%) | 208 (5.6%) | 0.286 | |
| Other | 1,303 (11.4%) | 326 (8.8%) | <0.001 | |
| Other PI | 688 (6.0%) | 91 (2.5%) | <0.001 | |
| White | 2,021 (17.7%) | 969 (26.3%) | <0.001 | |
| Payer | <0.001 | |||
| Dept. of Defense | 488 (4.3%) | 45 (1.2%) | <0.001 | |
| Private | 6,506 (57.0%) | 1,898 (51.5%) | <0.001 | |
| Public | 4,286 (37.5%) | 1,665 (45.2%) | <0.001 | |
| Self-Pay | 139 (1.2%) | 79 (2.1%) | <0.001 | |
| High Risk | ||||
| Yes | 4,684 (41.0%) | 1,020 (27.7%) | <0.001 | |
| Hospital | ||||
| Urban | 10,274 (90.0%) | 283 (7.7%) | <0.001 | |
| Multiple Gestation | ||||
| Yes | 210 (1.8%) | 38 (1.0%) | <0.001 | |
Discussion
Our study goal was to quantify adverse birth outcomes across maternal language in a location with substantial Asian and Pacific Islander populations. Our study hypothesis was that we would see more adverse birth outcomes for those who spoke languages other than English in the general sample and particularly among mothers with diabetes. We found some evidence to support this. Speaking a non-English language was associated with approximately two times the risk of having an obstetric trauma during a vaginal birth when other factors, including race/ethnicity, were controlled. If English language proficiency leads to greater exposure to obstetric trauma, understanding and mitigating this problem is important.
Obstetric trauma indicates a tear in the area between a woman’s vagina and rectum (Russo et al. 2008). This can have significant clinical implications, including anal incontinence, and potential lifelong discomfort (Bek & Laurberg 1993; Haadem et al 1987; Haadem et al. 1988). Further compounding the issue, complications from obstetric trauma are likely to be particularly challenging for a non-English speaker to address. Problems such as anal incontinence are sensitive issues often left underreported among English-speaking individuals (Hayden & Weiss 2011). For women who do not speak English well to report any complications likely demands either a language concordant provider or a skilled and trusted interpreter.
Speaking a non-English language was also associated with significantly higher rates of primary Caesarean sections and VBACs in our descriptive analyses. The higher rates of Caesarean sections among women who do not speak English were seen both overall and specifically among those with diabetes. These findings have clinical implications. If women who were less able to communicate with their providers in English were having higher rates of Caesarean sections and VBACs, these may increase the risk of these birth options and complicate an informed choice in the delivery decision. VBACs, for instance, are often a desirable birth outcome from a quality and safety perspective, but carry increased risk for uterine rupture, infections, blood clots and hysterectomy (American College of Obstetricians and Gynecologists, 2010). Effective communication and informed choice before and during labor about these issues is thus critically important (American College of Obstetricians and Gynecologists, 2010).
These issues may be particularly challenging to address among the Asian and Pacific Islander groups that were the focus of this study. The non-English speaking Asian and Pacific Islander population in Hawai‘i is extremely linguistically diverse (Figure 1). If the need for better in-language communication is the key to resolving disparities in maternal and infant outcomes, it can be challenging to design clinical care with the capacity to readily communication with all these language groups using in-person methods. Thus, many locations rely on telephone translator services. Addressing this issue is not only an issue in Hawai‘i. Asians and Pacific Islanders are swiftly growing demographic groups. The large majority of the growth in the Asian US population, in particular, is due to immigration (Perez & Hirshman 2009). Chinese (Mandarin and Cantonese) and Tagalog are the second and third most frequently spoken non-English languages in the US, with over three million speakers, making this a potentially urgent issue not only in Hawai‘i, but in many other US locations (US Census Bureau 2003).
While our study hypotheses were supported for some outcomes, we also found English proficiency was not associated with most of the adverse neonatal outcomes among Asian and Pacific Islanders in Hawai‘i, nor was it clearly associated with all our adverse outcomes generally and specifically among women with diabetes. Our finding in US Asian and Pacific Islanders may be related to the paradoxical findings regarding low rates of low birth weight among some disadvantaged Hispanic immigrant groups (Gould et al. 2003; Hoggatt et al. 2012). Previous research has suggested that risk profiles by language, and associated factors, such as acculturation and nativity are complex (Gould et al. 2003; Hoggatt et al. 2012). For instance, language of preferences has served as a proxy for acculturation in many studies (Lee at al. 2011). It may also be that our study had location-specific effects. If our results are location-specific, this suggests that at least some hospitals, community health centers, and providers in Hawai‘i who see large numbers of those with limited English proficiency have successful clinical practices to address linguistic differences. It may also be that during the delivery language is less important than in the care up to delivery. However, for this reason we also included those with diabetes and did not find significant disparities in these groups either. However, the numbers for these analyses were very small and may have had limited statistical power to detect meaningful differences as statistically significant. Our study design did not allow us to adjudicate among the reasons for these findings, which may be a fruitful are for further study.
Further examination of health/healthcare policies and practices affecting neonatal outcomes in Asian and Pacific Islanders across diverse linguistic groups is an important area of inquiry due to the growing numbers of these populations in the US. Our findings revealed quality disparities that could be resolved. Quality issues in maternal care lead to higher costs (Russo et al. 2009). Complicated deliveries are considerably more expensive than uncomplicated deliveries (Elixhauser & Wier 2011). These costs fall heavily on the taxpayer and public health system as Medicaid is the primary payer for 42% of these hospitalizations, but also impact employers and private insurers, who are the primary payers for 51% of the births (Russo et al. 2009; Sakala & Corry. 2008). This is particularly important as the U.S. is struggling to meet quality improvement in this area. A mid-course review of national Healthy People 2010 objectives found the U.S. to be missing targets for many maternity objectives, including Caesarean measures (Sakala & Corry. 2008; US DHHS 2006; US DHHS 2000). Also, language barriers cannot only affect health care outcomes, but also lead to poorer satisfaction with health care (Ponce et al. 2006). Further exploration to consider other sources of variation by language may be interesting, particularly as patient experience measures become incorporated in quality metrics.
Limitations
This study had several important strengths. We drew from all hospitalizations in a diverse state for a full year with detailed language use data, adjusting for race/ethnicity. Hawai‘i hospital data are extremely unique, including racial/ethnic groups not easily captured in most population-based samples that have increasing relevance to the U.S. population generally (US Census 2003). We can identify quality differences by language use at a level of detail that, to our knowledge, has not previously been reported.
This study also had some limitations. One limitation was that the analyses did not include some important clinical factors that particularly affect laceration rates (e.g., body mass index, birth weight). Until this information is elicited and included in analyses, the conclusions are limited. This study can help justify and guide further research with more detailed clinical information.
Another limitation was the significant amount of missing data due to unreported language information, which might mask disparities. Our comparison of the demographic information between included and missing data helped to resolve some of these concerns. The hospitals that did not report language data were less likely to have non-English speakers as they were rural hospitals, which were more likely to have Native Hawaiians and Whites (who were more likely to be English speakers). The included hospitals were the ones that had higher percentages of Filipinos, Japanese, other Pacific Islanders—groups that were more likely to not speak English—indicating that we were likely capturing the majority of non-English speakers in the state. However, it is also possible that the lack of poor maternal outcomes was due to the higher amount of data from our major hospitals, which might have had a greater ability to deal with linguistic issues than rural hospitals. Thus, even if the numbers of non-English speakers would be small (or perhaps because they would be small) in rural hospitals, the outcomes for non-English speakers might be worse there. However, the urban hospitals included in our study take the majority of high-risk deliveries for whom outcomes are likely to be worse. To some degree, we addressed the urban vs. rural topic by including rural vs. urban hospital location in our multivariate models. This variable was significant in relation to Caesarean rate and VBAC models. (This was because, lacking in-house anesthesia, rural hospitals have to schedule Caesarean sections more routinely and lacking ready access to a neonatal intensive care unit, they are far less likely to allow VBACs.) This variable was also significant in the SOI model for vaginal birth, likely reflecting the less urgent case mix of rural hospitals. Further study with language data from all Hawai‘i hospitals will be an important area for future study.
Another study limitation was that the data collected were administrative data. While such data were comprehensive, they lacked some important demographic information, such as immigration history (Fuentes-Afflick & Hessol 1997) as well as previous birth histories and status, and other clinical factors discussed above. Our models controlled for some demographics, but may not have controlled for enough. These are important areas for further study. Also, our sample was all maternity delivery-related hospitalizations, not individuals. Women could be included multiple times if they had more than one birth during 2012, but this was not a frequent problem as the time frame was only one year.
We were also limited by having only one year of data, particularly as some of these outcomes had low numbers. However, even with only one year of data, we found that we had at least 82% power to detect a 2% difference even in outcome (obstetric trauma rate) that affected the smallest difference and the least frequent outcome. This indicated that our lack of significant findings across other birth outcomes by English proficiency overall did not appear to be due to issues of statistical power. However, power was lower in the diabetes sample.
Finally, it is important to note that the linguistic and racial/ethnic groups here were heterogeneous. Risk profiles have been shown to vary across diverse racial/ethnic groups (Hoggatt et al, 2002). Due to sample size limitations, we included all the non-English speaking group together. However, further research should evaluate these outcomes across the heterogeneous Asian and Pacific Islander languages. It may be that the most frequent languages show fewer disparities than rare ones as hospitals will be more prepared for, and familiar with, these populations.
Conclusions
Speaking a non-English language was associated with approximately two times higher risk of having an obstetric trauma during a vaginal birth when other factors, including race/ethnicity, were controlled. Understanding and mitigating this problem is important. Speaking a non-English language was also associated with significantly higher rates of Caesarean sections and VBACs in descriptive analyses, which may increase the clinical risk and decreased the informed choice in these birth options. These are important areas for further inquiry.
Appendix 1
Results from Multivariable model for maternity outcomes by English Language Use in Hawai‘i Maternity-Related Hospitalizations, 2012 (n=11,419)1,2,3
| Caesarean delivery rate |
Primary Caesarean delivery rate |
Vaginal Birth After Caesarean rate, all |
Vaginal Birth After Caesarean rate, Uncomplicated |
Obstetric Trauma Rate - Vaginal Delivery Without Instrument |
Obstetric Trauma Rate - Vaginal Delivery With Instrument |
ID Rate4 | SOI APR-DRG5 540 |
SOI APR-DRG 541 |
SOI APR-DRG 542 |
SOI APR-DRG 560 |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR6 [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | ||
| English Use | ||||||||||||
| No vs. Yes | 1.02 [0.88, 1.17] | 1.18 [0.96, 1.45] | 1.02 [0.75, 1.40] | 1.03 [0.75, 1.41] | 2.02 [1.34, 3.04] | 1.48 [0.96, 2.28] | 0.97 [0.93, 1.01] | 0.99 [0.72, 1.35] | 0.95 [0.43, 2.12] | 1.61 [0.23, 11.3] | 1.11 [0.93, 1.34] | |
| Age, years | 2 | 2 | 2 | 2 | 2 | 2 | ||||||
| <18 vs. 35+ | 0.35 [0.22, 0.56] | 0.67 [0.41, 1.10] | N/A | N/A | 2.62 [1.03, 6.71] | 1.05 [0.26, 4.33] | 0.84 [0.76, 0.92] | 2.25 [0.92, 5.47] | N/A | N/A | 1.86 [1.37, 2.52] | |
| 18–34 vs. 35+ | 0.68 [0.63, 0.74] | 0.74 [0.65, 0.84] | 1.45 [1.14, 1.83] | 1.37 [1.08, 1.72] | 2.04 [1.36, 3.05] | 0.87 [0.61, 1.26] | 0.94 [0.92, 0.96] | 0.90 [0.75, 1.07] | 0.60 [0.34, 1.04] | 0.58 [0.09, 3.81] | 0.97 [0.85, 1.10] | |
| Payer | 2 | 2 | 2 | 2 | ||||||||
| DOD vs. private | 1.04 [0.86, 1.26] | 0.81 [0.59, 1.12] | 0.74 [0.44, 1.25] | 0.74 [0.44, 1.25] | 0.63 [0.32, 1.21] | 0.33 [0.08, 1.27] | 1.11 [1.07, 1.15] | 0.63 [0.42, 0.93] | 2.13 [0.44, 10.3] | 1.53 [0.16, 14.6] | 0.74 [0.58, 0.93] | |
| Public vs. private |
0.93 [0.86, 1.02] | 0.83 [0.73, 0.95] | 1.16 [0.95, 1.41] | 1.14 [0.94, 1.39] | 0.49 [0.36, 0.68] | 0.72 [0.48, 1.08] | 1.02 [1.00, 1.05] | 1.30 [1.08, 1.57] | 1.40 [0.77, 2.52] | 0.61 [0.17, 2.12] | 0.96 [0.86, 1.06] | |
| Self Pay vs. private |
0.69 [0.45, 1.04] | 0.55 [0.28, 1.07] | 1.43 [0.71, 2.90] | 1.48 [0.74, 2.97] | 0.88 [0.39, 1.95] | 0.55 [0.16, 1.85] | 0.94 [0.84, 1.04] | 0.71 [0.29, 1.75] | 1.88 [0.11, 31.2] | 0.00 [0.00, 0.00] | 1.31 [0.88, 1.95] | |
| High Risk | ||||||||||||
| Yes vs. No | 1.69 [1.57, 1.83] | 2.22 [1.98, 2.49] | 0.74 [0.63, 0.88] | 0.77 [0.65, 0.92] | 1.00 [0.77, 1.30] | 1.18 [0.86, 1.64] | 0.97 [0.95, 0.99] | 3.44 [2.91, 4.06] | 7.15 [4.16, 12.3] | 13.5 [4.20, 43.6] | 9.85 [8.86, 10.9] | |
| Hospital | ||||||||||||
| rural vs. urban | 1.70 [1.54, 1.88] | 1.58 [1.35, 1.86] | 0.02 [0.00, 0.12] | 0.02 [0.00, 0.12] | 0.93 [0.57, 1.50] | 0.58 [0.29, 1.18] | 1.13 [1.10, 1.16] | 0.42 [0.33, 0.54] | 0.73 [0.27, 1.98] | 2.76 [0.58, 13.3] | 0.48 [0.40, 0.58] | |
| Race/Ethnicity | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||||
| Chinese vs. White |
1.01 [0.81, 1.26] | 0.99 [0.72, 1.35] | 0.88 [0.48, 1.64] | 0.83 [0.43, 1.60] | 1.36 [0.74, 2.51] | 0.64 [0.24, 1.72] | 1.02 [0.97, 1.07] | 0.95 [0.59, 1.51] | 0.92 [0.18, 4.57] | 2.53 [0.19, 33.7] | 0.75 [0.57, 0.99] | |
| Filipino vs. White |
1.11 [0.98, 1.25] | 1.02 [0.86, 1.22] | 1.19 [0.88, 1.61] | 1.19 [0.88, 1.61] | 0.78 [0.51, 1.20] | 1.12 [0.67, 1.87] | 0.95 [0.93, 0.98] | 1.56 [1.21, 2.01] | 0.56 [0.22, 1.43] | 1.46 [0.25, 8.42] | 1.47 [1.26, 1.72] | |
| Hawaiian vs. White |
0.95 [0.84, 1.07] | 0.73 [0.60, 0.88] | 1.06 [0.77, 1.44] | 1.06 [0.78, 1.45] | 0.77 [0.50, 1.20] | 0.50 [0.23, 1.10] | 1.02 [0.99, 1.05] | 0.95 [0.73, 1.24] | 0.92 [0.37, 2.30] | 0.60 [0.11, 3.45] | 1.31 [1.13, 1.53] | |
| Japanese vs. White |
1.05 [0.92, 1.21] | 0.99 [0.81, 1.21] | 0.82 [0.53, 1.27] | 0.83 [0.54, 1.28] | 1.28 [0.81, 2.02] | 1.12 [0.63, 1.97] | 0.99 [0.96, 1.03] | 1.05 [0.78, 1.41] | 0.73 [0.21, 2.61] | 0.28 [0.03, 2.35] | 0.98 [0.81, 1.18] | |
| Micronesian vs. White |
1.28 [1.04, 1.57] | 1.27 [0.92, 1.73] | 1.52 [1.01, 2.29] | 1.53 [1.01, 2.30] | 0.84 [0.42, 1.70] | 0.87 [0.39, 1.96] | 0.98 [0.92, 1.03] | 1.57 [1.01, 2.44] | 1.08 [0.26, 4.52] | 1.13 [0.09, 14.5] | 1.71 [1.33, 2.20] | |
| Other vs. White | 1.12 [0.97, 1.28] | 1.04 [0.85, 1.27] | 0.85 [0.57, 1.25] | 0.86 [0.58, 1.27] | 1.63 [1.07, 2.48] | 1.44 [0.82, 2.54] | 0.98 [0.94, 1.01] | 1.02 [0.75, 1.39] | 0.64 [0.22, 1.87] | 1.01 [0.13, 7.59] | 1.17 [0.98, 1.41] | |
| Other PI vs. White | 1.00 [0.83, 1.21] | 0.83 [0.62, 1.12] | 1.31 [0.90, 1.89] | 1.34 [0.92, 1.93] | 1.01 [0.56, 1.85] | 0.21 [0.03, 1.53] | 1.00 [0.96, 1.05] | 1.14 [0.76, 1.70] | 1.93 [0.63, 5.93] | 0.71 [0.06, 9.09] | 1.86 [1.50, 2.30] | |
|
Multiple Gestation |
||||||||||||
| Yes vs. No | N/A | N/A | 0.55 [0.21, 1.44] | N/A | 0.52 [0.07, 3.68] | 0.57 [0.09, 3.69] | 1.00 [0.93, 1.07] | 9.58 [7.02, 13.1] | N/A | N/A | 13.4 [7.76, 23.3] | |
N/A: Number of the category with age <18 were zero or number of outcomes for multiple gestation were zero, no relative risk or odds ratios were provided.
Indicates that this set of variables is significant overall in multivariable models at p<.05.
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation.
ID Rate is the “Ideal Delivery” rate (i.e., deliveries without complications) (Gregory et al, 2009).
SOI is Severity of Illness; APR-DRG is All Patient Refined Diagnosis Related Groups.
RR is Rate Ratio; OR is Odds Ratio; CI is Confidence Interval.
Appendix 2
Results from Multivariable model for baby outcomes in Hawai‘i Delivery-Related Hospitalizations, 2012 (n=11,546)1,2
| Birth Trauma- Injury to Neonate |
Premature | Low Birth Weight | High Birth Weight | ||
|---|---|---|---|---|---|
| RR [95% CI] | RR [95% CI] | RR [95% CI] | RR [95% CI] | ||
| LEP | 1 | 1 | |||
| Yes vs. No | 0.72 [0.16, 3.25] | 1.08 [0.90, 1.30] | 1.11 [0.85, 1.45] | 0.72 [0.52, 1.00] | |
| Age, years | |||||
| <18 vs. 35+ | 2.70 [0.31, 23.7] | 1.12 [0.71, 1.75] | 1.64 [1.07, 2.52] | 0.37 [0.15, 0.90] | |
| 18–34 vs. 35+ | 1.18 [0.47, 2.97] | 0.89 [0.79, 1.01] | 0.83 [0.72, 0.96] | 1.00 [0.84, 1.20] | |
| Payer | |||||
| DOD vs. private | 1.32 [0.29, 6.11] | 0.79 [0.56, 1.12] | 0.97 [0.69, 1.37] | 0.96 [0.70, 1.32] | |
| Public vs. private | 0.90 [0.39, 2.06] | 1.09 [0.97, 1.24] | 1.10 [0.95, 1.27] | 0.87 [0.74, 1.01] | |
| Self Pay vs. private | 0.00 [0.00, 0.00] | 1.07 [0.62, 1.87] | 0.49 [0.20, 1.20] | 0.95 [0.50, 1.80] | |
| High Risk | |||||
| Yes vs. No | 2.82 [1.34, 5.92] | 2.59 [2.27, 2.96] | 3.04 [2.63, 3.51] | 1.41 [1.23, 1.62] | |
| Hospital | |||||
| rural vs. urban | 0.66 [0.16, 2.79] | 0.73 [0.57, 0.92] | 0.96 [0.76, 1.21] | 0.78 [0.61, 1.01] | |
| Race/Ethnicity | 1 | 1 | 1 | ||
| Chinese vs. White | 0.76 [0.09, 6.35] | 0.87 [0.60, 1.27] | 1.42 [0.98, 2.05] | 0.50 [0.32, 0.79] | |
| Filipino vs. White | 0.99 [0.34, 2.85] | 1.44 [1.20, 1.73] | 1.88 [1.52, 2.31] | 0.34 [0.26, 0.44] | |
| Hawaiian vs. White | 0.69 [0.22, 2.16] | 1.25 [1.04, 1.51] | 1.15 [0.92, 1.45] | 0.89 [0.73, 1.09] | |
| Japanese vs. White | 0.69 [0.17, 2.79] | 1.13 [0.91, 1.40] | 1.33 [1.04, 1.70] | 0.31 [0.22, 0.44] | |
| Micronesian vs. White | 1.88 [0.33, 10.8] | 1.39 [1.07, 1.81] | 1.56 [1.11, 2.20] | 0.97 [0.66, 1.42] | |
| Other vs. White | 0.48 [0.10, 2.31] | 0.90 [0.70, 1.15] | 1.09 [0.83, 1.43] | 0.66 [0.51, 0.86] | |
| Other PI vs. White | 0.92 [0.18, 4.63] | 1.45 [1.13, 1.86] | 1.12 [0.81, 1.57] | 1.73 [1.38, 2.18] | |
| Multiple gestation | |||||
| Yes vs. No | 2.82 [1.34, 5.92] | 2.59 [2.27, 2.96] | 3.04 [2.63, 3.51] | 1.41 [1.23, 1.62] | |
Indicates that this set of variables is significant overall in multivariable models at p<.05.
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, high-risk pregnancy, and multiple gestation.
Appendix 3
Results from Multivariable models in Hawai‘i Maternity-Related Hospitalizations among those with Diabetes, 2012 (n =1,355)1,2
| Caesarean delivery rate |
Primary Caesarean delivery rate |
Vaginal Birth After Caesarean rate, all |
Vaginal Birth After Caesarean rate, Uncomplicated |
ID Rate3 | SOI APR-DRG 540 |
SOI APR-DRG4 560 |
Premature | Low Birth Weight |
High Birth Weight |
||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RR [95%CI]5 | RR [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | OR [95%CI] | OR [95%CI] | RR [95%CI] | RR [95%CI] | RR [95%CI] | ||
| LEP | |||||||||||
| Yes vs No | 0.91 [0.65, 1.28] | 1.30 [0.83, 2.03] | 1.83 [0.83, 4.01] | 1.96 [0.89, 4.30] | 0.96 [0.86, 1.07] | 0.95 [0.48, 1.88] | 1.18 [0.70, 2.00] | 0.72 [0.43, 1.21] | 1.30 [0.80, 2.12] | 0.96 [0.47, 1.95] | |
| Age, years | |||||||||||
| 18–34 vs 35+ | 0.78 [0.66, 0.92] | 0.94 [0.70, 1.25] | 1.48 [0.84, 2.62] | 1.39 [0.78, 2.45] | 0.99 [0.93, 1.04] | 0.44 [0.30, 0.65] | 0.97 [0.72, 1.31] | 0.02 [0.00, 35E4] | 0.05 [0.00, 19E3] | 1.35 [0.92, 1.98] | |
| Payer | |||||||||||
| DOD vs private | 1.07 [0.62, 1.83] | 0.84 [0.33, 2.16] | N/A | N/A | 1.01 [0.86, 1.20] | 1.24 [0.44, 3.48] | 1.15 [0.54, 2.47] | 0.50 [0.14, 1.78] | 0.85 [0.26, 2.80] | 0.79 [0.30, 2.10] | |
| Public vs private | 1.14 [0.95, 1.37] | 1.08 [0.80, 1.47] | 0.93 [0.52, 1.64] | 0.91 [0.50, 1.63] | 0.99 [0.93, 1.05] | 2.01 [1.34, 3.02] | 1.01 [0.74, 1.37] | 1.43 [1.09, 1.88] | 1.05 [0.75, 1.48] | 0.92 [0.64, 1.33] | |
| Hospital | |||||||||||
| rural vs urban | 1.77 [1.42, 2.20] | 1.95 [1.35, 2.82] | N/A | N/A | 1.12 [1.03, 1.22] | 0.37 [0.19, 0.73] | 0.52 [0.25, 1.05] | 0.94 [0.52, 1.70] | 0.37 [0.12, 1.12] | 1.01 [0.54, 1.91] | |
| Race/Ethnicity | |||||||||||
| Chinese vs. White | 0.67 [0.35, 1.27] | 0.52 [0.19, 1.43] | N/A | N/A | 1.09 [0.95, 1.25] | 1.14 [0.44, 2.96] | 0.54 [0.25, 1.16] | 0.82 [0.36, 1.86] | 3.39 [1.37, 8.34] | 0.81 [0.31, 2.08] | |
| Filipino vs. White | 1.02 [0.76, 1.37] | 0.93 [0.58, 1.47] | 1.76 [0.57, 5.46] | 2.24 [0.56, 8.95] | 0.97 [0.88, 1.07] | 1.38 [0.72, 2.64] | 0.95 [0.59, 1.52] | 1.03 [0.66, 1.61] | 2.30 [1.07, 4.95] | 0.44 [0.24, 0.81] | |
| Hawaiian vs. White | 1.13 [0.84, 1.52] | 0.92 [0.56, 1.50] | 0.80 [0.23, 2.75] | 1.12 [0.26, 4.85] | 1.05 [0.95, 1.16] | 0.92 [0.48, 1.78] | 1.35 [0.79, 2.29] | 1.03 [0.66, 1.63] | 2.45 [1.12, 5.38] | 1.30 [0.77, 2.18] | |
| Japanese vs. White | 0.95 [0.66, 1.37] | 0.99 [0.58, 1.70] | 1.59 [0.42, 6.08] | 2.36 [0.50, 11.1] | 1.02 [0.92, 1.13] | 0.84 [0.38, 1.85] | 0.92 [0.52, 1.64] | 1.17 [0.70, 1.96] | 2.62 [1.17, 5.85] | 0.16 [0.05, 0.54] | |
| Micronesian vs. White |
1.54 [0.95, 2.48] | 1.59 [0.80, 3.15] | 1.73 [0.43, 6.99] | 2.32 [0.47, 11.4] | 1.11 [0.96, 1.29] | 1.25 [0.41, 3.78] | 2.46 [0.93, 6.51] | 1.70 [0.79, 3.62] | 2.97 [1.10, 8.00] | 1.09 [0.41, 2.91] | |
| Other vs. White | 0.94 [0.66, 1.33] | 0.83 [0.48, 1.45] | 1.18 [0.29, 4.74] | 1.70 [0.35, 8.38] | 0.95 [0.84, 1.06] | 0.68 [0.30, 1.51] | 1.38 [0.80, 2.40] | 1.05 [0.61, 1.81] | 2.00 [0.86, 4.67] | 0.72 [0.37, 1.41] | |
| Other PI vs. White | 0.87 [0.54, 1.39] | 0.75 [0.35, 1.60] | 1.04 [0.20, 5.47] | 1.55 [0.25, 9.65] | 1.05 [0.92, 1.20] | 2.80 [1.10, 7.15] | 2.15 [1.10, 4.22] | 1.48 [0.81, 2.71] | 2.10 [0.79, 5.56] | 1.25 [0.63, 2.48] | |
| Multiple Gestation | |||||||||||
| No vs. Yes | N/A | N/A | 0.67 [0.10, 4.34] | N/A | 1.03 [0.88, 1.21] | 22.3 [7.88, 62.9] | 11.2 [2.42, 51.8] | 4.04 [3.06, 5.34] | 4.29 [3.14, 5.85] | N/A | |
N/A: Number of the categories for outcomes was 0, no relative risk /odds ratios were provided.
Models adjusted for race/ethnicity, age group, payer, rural vs. urban hospital location, and multiple gestation.
ID Rate is the “Ideal Delivery” rate (i.e., deliveries without complications) (Gregory et al, 2009).
SOI is Severity of Illness; APR-DRG is All Patient Refined Diagnosis Related Groups.
RR is Rate Ratio; OR is Odds Ratio; CI is Confidence Interval.
Contributor Information
Tetine Sentell, Office of Public Health Studies, University of Hawai‘i at Manoa, 1960 East-West Road, Biomed T102, Honolulu, HI 96822, tsentell@hawaii.edu.
Ann Chang, Department of OB/GYN, John A. Burns School of Medicine, University of Hawai‘i, 1319 Punahou St., Suite 824, Honolulu, HI 96826, annchang@hawaii.edu.
Hyeong Jun Ahn, Biostatistics Core, John A. Burns School of Medicine, University of Hawai‘i, 651 Ilalo Street, Biosciences Building, Suite 211, Honolulu, HI 96813, hjahn@hawaii.edu.
Jill Miyamura, Hawai‘i Health Information Corporation, 733 Bishop St, Honolulu, HI 96813, jmiyamura@hhic.org.
References
- Agency for Healthcare Research and Quality. Rockville, Md: Agency for Health Care Research and Quality; 2011. [Accessed May 14, 2014]. 2011 APR-DRG Classification Software—Overview. www.ahrq.gov/qual/mortality/Hughessumm.pdf. [Google Scholar]
- Agency for Healthcare Research and Quality. [Accessed May 14, 2014];2013 http://www.qualityindicators.ahrq.gov/
- American College of Obstetricians and Gynecologists (ACOG) Vaginal birth after previous cesarean delivery. Washington (DC): American College of Obstetricians and Gynecologists (ACOG); 2010. Aug. [Accessed May 14, 2014]. p. 14. (ACOG practice bulletin; no. 115). http://www.acog.org/~/media/Practice%20Bulletins/Committee%20on%20Practice%20Bulletins%20--%20Obstetrics/pb115.pdf?dmc=1&ts=20130415T1216109630. [Google Scholar]
- Association of Asian Pacific Community Health Organizations. AAPI Limited English Proficiency (LEP) [Accessed May 14, 2013];2005 http://www.aapcho.org/wp/wp-content/uploads/2012/02/AAPCHO_FactSheet-AAPI_LEP_2005.pdf. [Google Scholar]
- Baker LC, Afendulis CC, Chandra A, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal mortality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161:69–76. doi: 10.1001/archpedi.161.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bek KM, Laurberg S. Risks of anal incontinence from subsequent vaginal delivery after a complete obstetric anal sphincter tear. Obstet Gynecol Surv. 1993;48:238–240. doi: 10.1111/j.1471-0528.1992.tb13870.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) International Classification of Diseases – 9th revision – Clinical Modification (ICD-9) codes) CDC. [Accessed May 14, 2014];2012 http://www.cdc.gov/nchs/icd/icd9cm.htm.
- Centers for Disease Control and Prevention (CDC) Maternal, pregnancy, and birth characteristics of Asians and Native Hawaiians/Pacific Islanders--King County, Washington, 2003–2008. MMWR Morb Mortal Wkly Rep. 2011;60:211–213. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2014 Low birth weight. [Accessed May 14, 2013]; http://www.cdc.gov/pednss/how_to/interpret_data/case_studies/low_birthweight/what.htm.
- Chatfield J. ACOG Issues Guidelines on Fetal Macrosomia: Practice Guidelines. Am Fam Physician. 2001;64:169–170. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Eligible Professional Meaningful Use Core Measures Measure 7 of 14 Stage 1 Last Updated: April 2013. [Accessed May 14, 2013];2013 http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/7_Record_Demographics.pdf.
- Coffey RM, Andrews RM, Moy E. Racial, ethnic, and socioeconomic disparities in estimates of AHRQ patient safety indicators. Med Care. 2005;43:I48–I57. doi: 10.1097/00005650-200503001-00008. [DOI] [PubMed] [Google Scholar]
- DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- Fuentes-Afflick E, Hessol NA. Impact of Asian ethnicity and national origin on infant birth weight. Am J Epidemiol. 1997;145:148–155. doi: 10.1093/oxfordjournals.aje.a009085. [DOI] [PubMed] [Google Scholar]
- Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: a dual epidemiologic paradox. Pediatrics. 2003;111:e676–e682. doi: 10.1542/peds.111.6.e676. [DOI] [PubMed] [Google Scholar]
- Gregory KD, Fridman M, Shah S, Korst LM. Global measures of quality- and patient safety-related childbirth outcomes: should we monitor adverse or ideal rates? Am J Obstet Gynecol. 2009;200:681.e1–681.e7. doi: 10.1016/j.ajog.2009.02.033. [DOI] [PubMed] [Google Scholar]
- Haadem K, Ohrlander s, Lingman G. Long-term ailments due to anal sphincter rupture caused by delivery—a hidden problem. Eur J Obstet Gynecol Reprod Biol. 1988;27:27–32. doi: 10.1016/s0028-2243(88)80007-8. [DOI] [PubMed] [Google Scholar]
- Haadem K, Dahlstrom JA, Ling L, Ohrlander S. Anal sphincter function after delivery rupture. Obstet Gynecol. 1987;70:53–56. [PubMed] [Google Scholar]
- Hawaii Economic Issues. Data report 2011. [Accessed May 14, 2014];The non-English speaking Population in Hawaii. 2011 http://files.hawaii.gov/dbedt/census/acs/Report/Data-Report-Non-English-Speaking-Profile-Hawaii.pdf.
- Hawaii Health Information Corporation Inpatient Data. [Accessed April 19, 2013];2012 http://hhic.org/inpatient-data.asp. [Google Scholar]
- Hayden DM, Weiss EG. Fecal incontinence: Etiology, evaluation, and treatment. Clin Colon Rectal Surg. 2011;24:64–70. doi: 10.1055/s-0031-1272825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Accessed May 14, 2014]. HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2008. http://www.hcup-us.ahrq.gov/reports/factsandfigures/2008/pdfs/FF_report_2008.pdf. [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) Databases; Healthcare Cost and Utilization Project (HCUP) Rockville, MD: 2014. [Accessed May 14, 2014]. Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/databases.jsp. [PubMed] [Google Scholar]
- Hoggatt KJ, Flores M, Solorio R, Wilhelm M, Ritz B. The "Latina epidemiologic paradox" revisited: the role of birthplace and acculturation in predicting infant low birth weight for Latinas in Los Angeles, CA. J Immigr Minor Health. 2012;14:875–884. doi: 10.1007/s10903-011-9556-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le LT, Kiely JL, Schoendorf KC. Birthweight outcomes among Asian American and Pacific Islander subgroups in the United States. Int J Epidemiol. 1996;25:973–979. doi: 10.1093/ije/25.5.973. [DOI] [PubMed] [Google Scholar]
- Lee S, Nguyen HA, Tsui J. Interview language: A proxy measure for acculturation among Asian Americans in a population-based survey. J Immigr Minor Health. 2011;13:244–252. doi: 10.1007/s10903-009-9278-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons L, Day S. Improving obstretric outcomes in ethnic minorities: An evaluation of health advocacy in Hackney. Journal of Public Health Medicine. 1992;14:183–191. [PubMed] [Google Scholar]
- Perez AD, Hirschman C. The changing racial and ethnic composition of the US population: Emerging American identities. Popul Dev Rev. 2009;35:1–51. doi: 10.1111/j.1728-4457.2009.00260.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Intern Med. 2006;21:786–791. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C. Addressing limited English proficiency and disparities for Hispanic postpartum women. J Obstet Gynecol Neonatal Nurs. 2005;34:512–520. doi: 10.1177/0884217505278295. [DOI] [PubMed] [Google Scholar]
- Qin C, Gould JB. The Asian birth outcome gap. Paediatr Perinat Epidemiol. 2006;20:279–289. doi: 10.1111/j.1365-3016.2006.00737.x. [DOI] [PubMed] [Google Scholar]
- Rao AK, Daniels K, El-Sayed YY, Moshesh MK, Caughey AB. Perinatal outcomes among Asian American and Pacific Islander women. Am J Obstet Gynecol. 2006;195:834–838. doi: 10.1016/j.ajog.2006.06.079. [DOI] [PubMed] [Google Scholar]
- Ro M. Moving forward: Addressing the health of Asian American and Pacific Islander. Women. Am J Public Health. 2002;92:516–519. doi: 10.2105/ajph.92.4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg TJ, PhD, Garbers S, Lipkind H, Chiasson MA. Maternal obesity and diabetes as risk factors for adverse pregnancy outcomes: Differences among 4 racial/ethnic groups. Am J Public Health. 2005;95:1545–1551. doi: 10.2105/AJPH.2005.065680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo CA, Andrews RM, Barrett M. Racial and Ethnic Disparities in Hospital Patient Safety Events, 2005. [Accessed May 14, 2014];Statistical Brief #53. 2008 http://www.ncbi.nlm.nih.gov/books/NBK56034/ [PubMed]
- Russo CA, Wier L, Steiner C. Hospitalizations Related to Childbirth, 2006. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [Accessed May 14, 2014]. (HCUP Statistical Brief, 71.) http://www.hcup-us.ahrq.gov/reports/statbriefs/sb71.jsp. [PubMed] [Google Scholar]
- Sakala C, Corry M. Evidence-based maternity care: What it is and what it can achieve. [Accessed May 14, 2014];Co-published by Childbirth Connection, the Reforming States Group, and the Milbank Memorial Fund. 2008 http://www.milbank.org/uploads/documents/0809MaternityCare/0809MaternityCare.html. [Google Scholar]
- Sedman A, Harris JM, II, Schulz K, Schwalenstocker E, Remus D, Scanlon M, Bahl V. Relevance of the Agency for Healthcare Research and Quality Patient Safety Indicators for children's hospitals. Pediatrics. 2005;115:135–145. doi: 10.1542/peds.2004-1083. [DOI] [PubMed] [Google Scholar]
- Small R, Rice PL, Yelland J, Lumley J. Mothers in a new country: The role of culture and communication in Vietnamese, Turkish and Filipino Women's experiences of giving birth in Australia. Women and Health. 1999;28:77–101. doi: 10.1300/J013v28n03_06. [DOI] [PubMed] [Google Scholar]
- Tu S-P, Yip M-P, Chun A, Choe J, Bastani R, Taylor V. Development of intervention materials for individuals with limited English proficiency: Lessons learned from “Colorectal Cancer Screening in Chinese Americans”. Medical Care. 2008;46:S51–S61. doi: 10.1097/MLR.0b013e31817f0cde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong LF, Caughey AB, Nakagawa S, Kaimal AJ, Tran SH, Cheng YW. Perinatal outcomes among different Asian-American subgroups. Am J Obstet Gynecol. 2008;199:382.e1–382.e6. doi: 10.1016/j.ajog.2008.06.073. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Rockville (MD): Agency for Healthcare Research and Quality; 2010. [Accessed May 14, 2014]. National healthcare quality report. http://www.ahrq.gov/qual/nhqr10/nhqr10.pdf. [Google Scholar]
- US Census Bureau. The Native Hawaiian and Other Pacific Islander population 2010. [Accessed May 14, 2014];2012 Issued May 2012. http://www.census.gov/prod/cen2010/briefs/c2010br-12.pdf.
- US Census Bureau. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States: April 1, 2000 to July 1, 2009. [Accessed May 14, 2014];2011 http://www.census.gov/compendia/statab/2011/tables/11s0006.pdf.
- US Census Bureau. Washington, DC: U.S. Department of Commerce; 2003. Language use and English speaking ability: 2000. [Google Scholar]
- U.S. Department of Health and Human Services. Washington, DC: U.S. Government Printing Office; 2006. Healthy People 2010 Midcourse Review. [Google Scholar]
- US Department of Health and Human Services. With Understanding and improving health and objectives for improving health. 2nd. Vol. 2. Washington, DC: U.S. Government Printing Office; 2000. [November 2000]. HP 2010. [Google Scholar]