Abstract
Background
Despite the fact that social participation is considered a pivotal outcome of a successful recovery after stroke, there has been little attention on the impact of activities and services on this important domain.
Objective
The aim was to present a systematic review and meta-analysis on the effects of rehabilitation interventions on social participation after stroke from randomized controlled trials (RCTs).
Methods
Eight electronic databases were searched for relevant RCTs that evaluated the effects of an intervention on the outcome of social participation after stroke. Reference lists of selected articles were hand-searched to identify further relevant studies. Methodological quality of the studies was assessed using the Physiotherapy Evidence Database Scale. Standardized mean differences (SMD) and confidence intervals (CI) were estimated using fixed and random effect models.
Results
Twenty four RCTs involving 2042 stroke survivors were identified and reviewed and 21 were included in the meta-analysis. There was a small beneficial effect of interventions that utilized exercise on social participation (ten studies, SMD = 0.43, 95% CI = 0.09, 0.78, p =0.01) immediately after the program ended. Exercise in combination with other interventions (thirteen studies, SMD = 0.34, 95% CI = 0.10, 0.58, p =0.006) also resulted in beneficial effects. No significant effect was observed for interventions that involved support services over nine studies (SMD =0.09 [95%CI = −0.04, 0.21], I2 = 0%, p =0.16).
Conclusions
The included studies provide evidence that rehabilitation interventions may be effective in improving social participation after stroke, especially if exercise is one of the components.
Keywords: Social participation, stroke, rehabilitation, quality of life, exercise
Introduction
A World Health Organization1 report revealed that stroke results in the greatest burden of disease amongst all neurological disorders (including Alzheimer and dementias). There is an increasing number of strokes because the North American population is aging and a greater proportion of people are surviving stroke than before. Unfortunately, not all patients are getting access to the care and rehabilitation they need to have the best possible outcome.2
Recovery of function in stroke patients is a complex process which may be spontaneous and involve the effects of therapeutic interventions.3,4 Knowledge about interventions that promote the best outcomes on recovery may help optimize health care services. Successful recovery from a stroke should result in a quality of life and degree of participation in the community similar to that prior to the stroke event. There has been increasing criticism of the lack of services and research on the long-term consequences after stroke. A BMJ commentary summarized this sentiment: “Comprehensive national audits of stroke care show alarming levels of neglect in terms of chronic disease management and seem to indicate a collective nihilism about the potential for altering function and well-being after the early treatment of stroke”.5 However, there is little consensus about the effects of rehabilitation services for stroke survivors once they have left the hospital and are living in the community. Social participation is considered one of the most relevant and pivotal outcomes of a successful recovery.6 Individuals have been shown to be dissatisfied with their ability to engage in numerous aspects of participation, including socializing, outings, and travel, at three months after sustaining a stroke.7 The provision of rehabilitation services after hospital discharge may be particularly relevant as it aims to promote patients’ independence and reintegration into the community.
The International Classification of Functioning, Disability and Health (ICF) defines participation as ‘involvement in a life situation’8 or as “the lived experience” of people in the actual context in which they live’. Participation is a treatment goal in the context of recovering from stroke and is known to correlate with domains related to quality of life.9 Using a content analysis involving 43 studies, Levasseur et al.10 defined social participation ‘as a person’s involvement in activities that provide interaction with others in society or the community’. Similarly, the Disability Creation Process conceptual model defines social participation as a means of carrying out one’s life habits in one’s environment (e.g., school, work place, neighborhood).11
Despite the fact that social participation is critical to the success of community reintegration, the literature in this area has not been systematically collated and synthesized previously to our knowledge. Therefore, we performed a systematic review and meta-analysis to determine if rehabilitation interventions improve social participation among stroke survivors based on the evidence from randomized controlled trials (RCTs).
Methods
Search Strategy, Eligibility Criteria, and Data Retrieval
An electronic database search was done up to April 2015 using eight databases. MEDLINE (OvidSP), Embase (OvidSP), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), Physiotherapy Evidence Database (PEDro), PsycINFO, ProQuest ERIC and NIH Clinical Trials Databases were searched using the MeSH and keywords stroke, cerebrovascular disease, cerebrovascular disorder, cerebral infarction and brain infarction in conjunction with rehabilitation, social participation, quality of life, and activities of daily living. We did not limit the search to any language or date. Considering the different terms that can be used for social participation, we did not restrict the review to any specific outcome measure.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines12 was followed. Peer-reviewed publications were included if they were RCTs of any non-pharmacological and non-surgical community-based intervention for community-dwelling stroke survivors, where social participation was an outcome. Further inclusion criteria were: (1) participants above 18 years of age; (2) a baseline data point and post intervention data point or at follow-up (i.e., retention of effects) assessing social participation using a validated scale; (3) intervention and control group treatments clearly defined; and (4) intervention carried out for at least 4 weeks to have sufficient duration for benefits to accrue. Studies that included other populations were included if data for the stroke group was available. A social participation outcome required measurement of one or more of the following three characteristics: social contact, contributing to society (e.g., volunteer work) or receiving from society (e.g., receiving a visit from a friend).13 Studies were excluded if the full research document was not located, if the type of intervention could not be identified or detail of intervention was not provided, and if the data was derived from a conference proceeding or abstract. Interventions which involved electrotherapeutics or electro-mechanics (e.g., electrical stimulation, vibration) were excluded as they are not typically considered community-based programs.
All citations obtained were exported to RefWorks bibliography management software. After duplicates were deleted, the titles and abstracts of studies identified were screened and full articles of abstracts which appeared relevant were retrieved. The reference lists of the full-text articles were searched by hand to identify additional relevant research papers. At this point, any article that did not meet the inclusion/exclusion criteria was discarded. The remaining articles were assessed for quality of evidence and risk of bias using the Physiotherapy Evidence Database (PEDro) scale (maximum score of 10).14 When available, we utilized the official scores posted on the PEDro website as these have been verified by two trained experts. If the median and range were reported, we converted them to the mean and standard deviation.15 If an interquartile range was reported, we converted to a standard deviation.16 The reviewers assessed eligibility based on the full-text papers and conducted data extraction independently using a standard form. The study selection process along with excluded articles at the full text level was presented via PRISMA study flow diagram.
Statistical Analysis
An analysis was undertaken for 1) immediate post-intervention (differences between the baseline and post-intervention) and 2) follow-up (differences between the baseline and last follow-up point, i.e., months after the intervention ended) for interventions that were reasonably homogenous. Given the outcome of social participation, we expected that programs providing support services would be a typical intervention found within this search. Thus, we planned to undertake an analysis of support service interventions as defined as those programs or services offered to assist individuals and their families in handling the myriad of physical, emotional, social, and practical problems that follow a stroke diagnosis and its subsequent treatment.17 We also expected that exercise programs would be another intervention found within the search because better mobility and endurance may be associated with the ability to participate in everyday activities.18,19 Thus, we planned to undertake an analysis of exercise as an intervention as defined as a physical activity that is planned, structured, repetitive, and purposive with the objective of improvement or maintenance of physical fitness and function.20 A standardized mean difference (SMD) was calculated for all outcomes. Heterogeneity was assessed by the I-squared (I2) value. Random effect models were used if statistical heterogeneity observed in the groups was high (I2 > 25%)21, else fixed effect models were used. All statistical analyses were performed with Review Manager 5.3 (the Nordic Cochrane Centre, Copenhagen). Statistical significance was considered as a p value less than 0.05.
Results
Included Studies
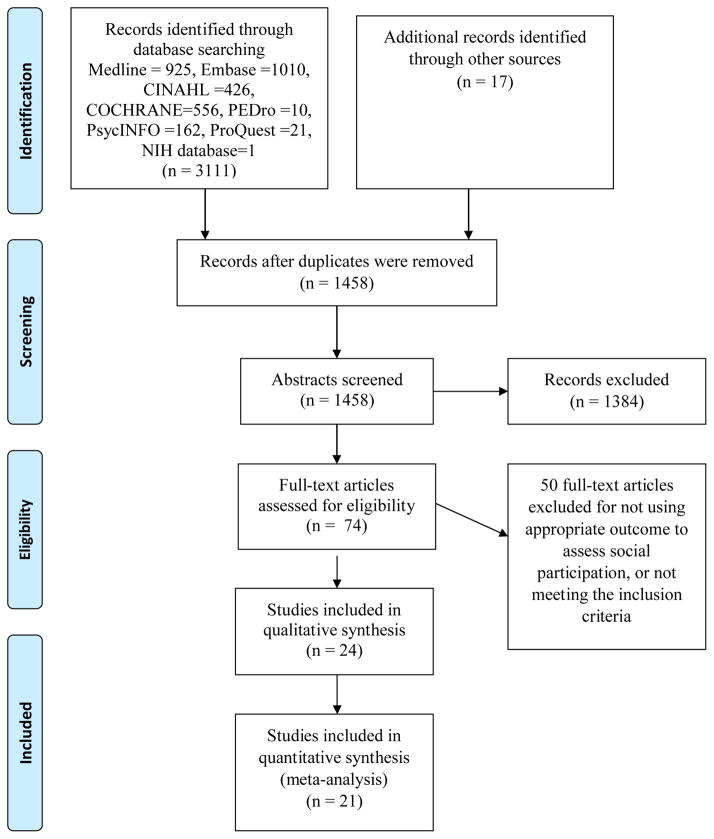
A total of 24 studies22–45 met the inclusion criteria (Figure 1), with a total of 2042 individuals with stroke. Two studies30,34 did not have immediate post-intervention data, but reported outcomes six30 and nine34 months after the intervention ended. Four studies required conversion of the data to mean and standard deviation; one each reported median and interquartile ranges27 and median and range values,33 and two reported mean and CI values28,42 The ages of the stroke survivors ranged from 30 to 91 years. The length of the intervention ranged from 4 weeks44 to 12 months35,37, with duration of 4 weeks44 to 6 months39,41,43 in most of the studies (22/24). Individual study details are included in Table 1 and present seven support service studies, eleven exercise studies, three mixed studies (support service and exercise) and three other studies which did not involve exercise or support service.
Figure 1.
PRISMA study selection flow diagram
Table 1.
Characteristics of included studies
| First author and year | Number of patients | Time since stroke | Outcome | Use of outcome | Type of Intervention | Length of Intervention | Control group | Pedro Score |
|---|---|---|---|---|---|---|---|---|
| Ada 2013 | 68 | > 6 months | AAP | Secondary | Exercise | 4 months | No intervention | 8 |
| Beinotti 2013 | 20 | ≥ 1 year | SF 36 | Primary | Horseback riding | 16 weeks | Usual care | 5 |
| Chan 2006 | 52 | > 3 months | CIQ | Primary | Exercise | 6 weeks | OT | 6 |
| Chumbler 2012 | 48 | > 1 month | LLFDI | Secondary | Support services | 3 months | Usual care | 7 |
| Flansbjer 2012 | 18 | > 6 months | SIS | Primary | Exercise | 10 weeks | Usual care | 4 |
| Harrington 2010 | 243 | >6 months | FAI | Primary | Mixed | 8 weeks | Usual care | 8 |
| Holmgren 2010 | 34 | > 3 weeks | FAI | Tertiary | Exercise | 5 weeks | Group discussion | 8 |
| Immink 2014 | 22 | >9 months | SIS | Primary | Yoga | 10 weeks | Wait list | 6 |
| Katz-Leurer 2003 | 79 | >4 weeks | FAI | Primary | Exercise | 6 weeks | Usual care | 5 |
| Kendall 2007 | 100 | > 3 months | SSQoL | Primary | Support services | 7 weeks | Usual care | 4 |
| Lai 2006 | 95 | < 1 month | SIS | Primary | Exercise | 3 months | Usual care | 6 |
| Lennon 2008 | 46 | > 12 months | FAI | Primary | Mixed | 10 weeks | Usual care | 7 |
| Lund 2011 | 86 | > 3 months | SF 36 | Primary | Support services | 36 weeks | Usual care | 7 |
| Markle-Reid 2011 | 82 | > 6 months | SF 36 | Primary | Support services | 12 months | Usual care | 6 |
| Marsden 2010 | 26 | > 6 months | SIS | Primary | Support services | 7 weeks | Wait list | 7 |
| Mayo 2015 | 186 | > 6 months | RNL | Secondary | Mixed | 12 months | Wait list | 7 |
| Nadeau 2013 | 282 | < 2 months | SIS | Tertiary | Exercise | 4 months | Usual care | 7 |
| Ostwald 2014 | 134 | < 12 months | SIS | Primary | Support services | 6 months | Mailed information | 7 |
| Ouellette 2004 | 41 | > 6 months | LLFDI | Primary | Exercise | 12 weeks | Stretching | 7 |
| Rochette 2013 | 186 | < 1 month | LIFE-H | Secondary | Support services | 6 months | passive intervention | 6 |
| Rydwik 2006 | 18 | ≥ 1 year | SF 36 | Primary | Ankle ROM | 6 weeks | Wait list | 5 |
| Shaughnessy 2012 | 63 | >3 months | SIS | Primary | Exercise | 6 months | Stretching | 4 |
| Smith 2008 | 20 | > 3 months | SIS | Primary | Exercise | 4 weeks | Phone calls | 3 |
| Studenski 2005 | 93 | > 1 month | SIS | Primary | Exercise | 12 weeks | Usual care | 6 |
AAP – Adelaide activities profile, CIQ - Community Integration Questionnaire, LLFDI - Late Life Function and Disability Instrument, FAI –Frenchay Activities Index, LIFE-H- Assessment of Life Habits, RNL- Reintegration to Normal Living Index, SIS-Stroke Impact Scale, SSQoL-Stroke Specific Quality of Life Scale, OT- Occupational Therapy, ROM- Range of Motion, Mixed indicates both exercise and support services were involved.
Studies utilizing support services included telephone calls25,41, home visits35,39, educational courses31,34, mailed educational information39 and group discussions.36 Studies utilizing support services as an intervention or in combination with other interventions25,27,31,33–37,39,41 had a frequency of at least one session per month for eight weeks. Studies utilizing exercise included treadmill training22,38,43,44, cycling30,33, group exercise37, and progressive resistance exercise.28,32 Studies utilizing exercise had a frequency of at least two sessions per week.
Outcome Measures of Social Participation
Most of the studies (18/24) assessed social participation as a primary outcome,23,24,26,27,29–36,39,40,42–45 and nine studies26,29,32,36,38,39,43–45 used the social participation subscale of the Stroke Impact Scale. Two studies27,37 used both a subscale and full scale to assess social participation. In these instances, complete scales used to assess social participation were chosen over subscales.
Quality of Evidence
The PEdro scores ranged from three44 to eight.22,27,28 One study41 did not have a confirmed PEdro score and it was calculated independently by two authors and disagreements were resolved by discussion. Eleven studies23,24,26,29–31,34,42–45 did not perform an intention to treat analysis. More than 15% of loss to follow-up occurred in four studies.31,35,40,41 Two exercise studies recorded adverse events38,40, while one28 only reported falls. One study each reported that no adverse events25 and no serious adverse events occurred.37 Seventeen studies22–24,26,27,29–36,39,43–45, including ten with exercise components, did not state whether any adverse events occurred or not.
Quantitative Analysis
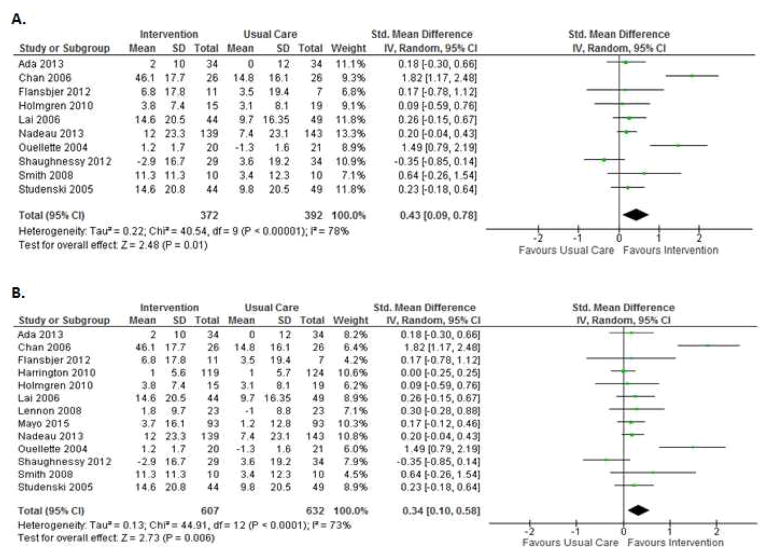
Analysis of the ten studies that used exercise alone (n = 764) produced a significant model immediately after the intervention ended (SMD = 0.43 [95% CI = 0.09, 0.78], I2 = 78%, p =0.01) (Figure 2A). As some studies have multiple components, restricting the analysis to thirteen studies that involved at least an exercise program (n=1239) also produced a significant model (SMD = 0.34 [95%CI = 0.10, 0.58], I2 = 73%, p =0.006) (Figure 2B). After removing two studies considered as outliers because their SMDs were greater than 1.4 (i.e., very strong effect of exercise)24,40, while all others were less than 0.7, the model remained significant (SMD = 0.14 [95% CI = 0.02, 0.25], I2 = 0%, p =0.02). Removing the only study44 that was considered of poor methodological quality following risk of bias assessment (PEDro score ≤ 3) still produced significant models for studies that involved exercise alone (SMD = 0.42 [95% CI = 0.06, 0.78], I2 = 80%, p =0.02) or at least an exercise program (SMD = 0.32 [95% CI = 0.07, 0.57], I2 = 75%, p =0.01). There was no statistically significant effect of exercise for the follow-up period of six studies which used exercise alone or seven studies which used exercise in conjunction with other components.
Figure 2.
Post intervention forest plot of interventions involving A) exercise alone or B) at least exercise
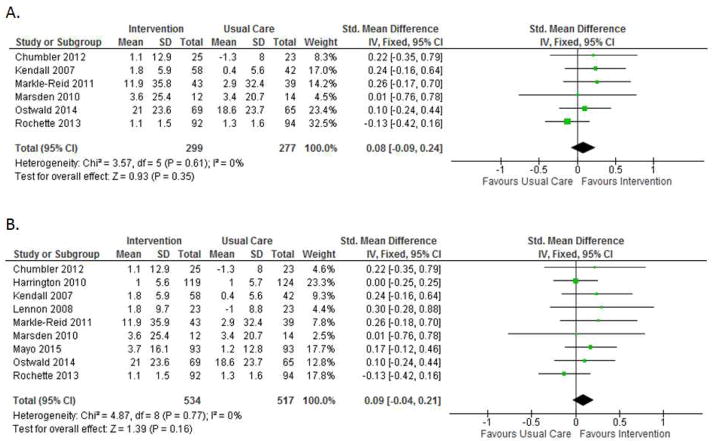
No significant difference was observed for interventions that involved support services over nine studies (SMD =0.09 [95%CI = −0.04, 0.21], I2 = 0%, p =0.16) (Figure 3). Removing the only study41 that did not involve face-to-face contact or require the participant to leave the home resulted in a near significant effect (SMD=0.13[95%CI = −0.00,0.27], I2 = 0%, p =0.05). There was no statistically significant effect of support services for the follow-up period of four studies which used support services alone or five studies which used support services in conjunction with other components. Of the three studies that did not involve support service or exercise as defined in the study, a study reported significant improvement on social participation using passive and active ankle range of motion42 (SMD = 3.13 [95%CI = 1.65, 4.61]), and two reported no significant impact using yoga29 (SMD= 0.65 [95%CI = −0.21, 1.51]) or horseback riding23 (SMD = −0.05 [95%CI = −0.93, 0.83]).
Figure 3.
Post intervention forest plot of interventions involving A) support services alone or B) at least support services
Discussion
Social participation is one of the most important end points of recovery from a stroke, and it is usually the ultimate goal of rehabilitation. In a recent meta-ethnographic review of the experiences and views of community-dwelling stroke survivors46, most studies reported that stroke disrupts the lives of participants leading to a change in their social lives, loss of autonomy and independence. The findings in our study showed that it is possible to improve social participation with certain rehabilitation interventions. In particular, interventions that involved exercises (in part or alone) were effective. The prominence of studies focusing on the impact of exercise is not surprising given the long-held clinical belief in the value of active exercise in stroke rehabilitation.47
There are a number of mechanisms which may explain the impact of exercise on social participation. Exercise can improve mobility48, balance, fatigue and endurance after stroke49, which may enable the stroke survivor to engage in activities. Physical activity is also known to improve a number of the secondary effects of stroke which may be a barrier to social participation. For example, exercise can prevent or reduce depressive symptoms after stroke50 which may lead to greater willingness to engage in activities. Hence, exercise has a very real protective function, helping to increase physical independence and improving quality of life.
All but two32,45 of the studies that involved exercise had the intervention carried out in either a community setting22,27,37 or rehabilitation centre.24,26,28,30,33,38,40,44 Since these venues are different from their homes, they provide a form of social participation. Exercise provided in groups may also provide an additive benefit that has an element of social participation in socially engaging settings with participants experiencing similar health issues.51 The support provided by the exercise instructors (e.g., external encouragement, qualified personnel) has been identified as a facilitator in participating in exercise.52 Group exercise can also increase levels of participation in physical activity as social support from other group members provide encouragement to attempt new exercises and challenge negative perception of ability.53 Stroke specific exercise groups are viewed as enabling social support, increasing confidence, improving mood, motivation, and an opportunity for knowledge acquisition.54 Exercise appeared to have been beneficial in stroke, but the effects were not retained after the intervention ended. Being physically active on a regular basis is recommended by all exercise guidelines.
It is possible that the act of getting out of the home to engage with other people is the critical element of the exercise programs which resulted in improved social participation. However, some of the exercise studies required both the experimental and control groups to participate in a community group program which would account for attention, engaging with others and getting out of the home. In fact, some of the exercise studies which utilized attention controls had the largest effect sizes24,40, suggesting that it is the exercise itself which is effective. Some of the studies requested that participants exclude their outings due to the exercise itself when estimating their social participation 37, which provides additional evidence that it is the act of exercise that is beneficial for improving social participation.
Over the long term, a stroke survivor’s focus on recovery shifts from physical concerns to social concerns, where there is a desire to participate in the social world and integrate into lives and relationships.55 While it may seem logical that providing services to support community integration would enhance social participation, the meta-analysis showed that the effect of support services on social participation is questionable. Of interest, removing the only study41 that did not involve face-to-face contact resulted in a near significant effect, suggesting that the act of leaving the house and interacting in-person with others may need to be an active ingredient of a social participation intervention. It is important to note that participants only received usual care (and not an attention control) in four25,31,33,35 out of five studies that showed that support service was more beneficial, and thus, it is not possible to disentangle the effects of attention versus support.
In this present meta-analysis, only one study37 developed the intervention with the intention of enhancing participation after stroke. In addition to exercise, these participants explored local community resources and opportunities and were encouraged to engage in community-based activities to meet leisure and life-goals. The authors noted that their strongest effects were demonstrated at the end of the intervention (at 12 months) and at follow-up (3 months later) versus mid-intervention (6 months) and they suggested that gains in participation take time. Other studies may be limited by their short duration. It is possible that the efficacy of support service interventions may have also been affected by the treatment frequency. Most of the support service interventions had less treatment frequency (typically once a week) compared to interventions that utilized a component of exercise (frequency of two to five times a week). Duration and intensity are important factors in the effectiveness of rehabilitation.56
It is difficult to draw conclusions about the interventions that did not involve social support or exercise, since there was only one study for each. In the study by Rydwik42 involving passive and active range of motion training, the authors attributed a large effect on social participation to attention potentially from the health care providers since the control group received no intervention and these effects were not accompanied by any physiological changes. We did not categorize horseback riding or yoga as exercise according to our definition and found that neither had an effect on social participation, despite the additional attention provided over the usual care control group. While some forms of horseback riding and yoga can be considered exercise, the one study with horseback riding utilized it mostly as an educational form of therapy, including touching different parts of the horse 23 while the one yoga study included some physical aspects and also mental imagery when the exercises were too challenging.29
This systematic review has some limitations. There was heterogeneity in the studies, especially with variability in interventions and outcomes. Although interventions that involved exercise may be beneficial for community-dwelling stroke survivors, the specific type of exercise with most benefit, and the effects of duration are unclear. Given the lack of effect from social support interventions, we would suggest that future studies target their interventions to improve specific aspects of social participation, including the individual’s involvement in activities that provide interaction with the community and society. In addition, outcome measures which measure multiple characteristics of social participation such as social contacts as well as contributions to society should be used. Studies are needed to determine the optimal rehabilitation strategy for improving social participation. Future research should follow individuals for a longer period post-intervention (e.g., 6 – 12 month follow-up) to elucidate the effects of duration on improvements. In addition, the use of control groups matched for attention will help to understand the impact of these interventions on social participation. This will ultimately advance knowledge about the rehabilitation strategy for promoting social participation in individuals with stroke.
Conclusion
The included studies provide evidence that rehabilitation interventions may be effective in improving social participation in individuals with stroke, especially if exercise is one of the components.
Acknowledgments
Sources of funding
Grant support from the Canadian Institutes of Health Research (CIHR) (MOP-136965) and Social Sciences and Humanities Research Council (895-2013-1021), fellowship support (to AOO) from CIHR and the Michael Smith Foundation of Health Research, and salary support (to JJE) from the Canada Research Chair Program (143864).
Footnotes
Disclosures: None
References
- 1.World Health Organization. [Accessed January 18, 2015];Neurological disorders: public health challenges. 2014 http://www.who.int/mental_health/neurology/neurological_disorders_report_web.pdf.
- 2.Heart and Stroke Foundation of Canada. [Accessed January 30, 2015];Stroke Report 2014: Together against a rising tide: Advancing Stroke Systems of Care. http://www.heartandstroke.com/atf/cf/%7B99452D8B-E7F1-4BD6-A57D-B136CE6C95BF%7D/HSF_SMReport2014E_Final.pdf.
- 3.Belda-Lois J-M, Mena-del Horno S, Bermejo-Bosch I, et al. Rehabilitation of gait after stroke: a review towards a top-down approach. J NeuroEngineering Rehabil. 2011;8:66. doi: 10.1186/1743-0003-8-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levin MF, Kleim JA, Wolf SL. What Do Motor “Recovery” and “Compensation” Mean in Patients Following Stroke? Neurorehabil Neural Repair. 2008;23:313–319. doi: 10.1177/1545968308328727. [DOI] [PubMed] [Google Scholar]
- 5.O’Neill D, Horgan F, Hickey A, McGee H. Long term outcome of stroke: Stroke is a chronic disease with acute events. BMJ. 2008;336:461. doi: 10.1136/bmj.39500.434086.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noreau L, Desrosiers J, Robichaud L, Fougeyrollas P, Rochette A, Viscogliosi C. Measuring social participation: Reliability of the LIFE-H in older adults with disabilities. Disabil Rehabil. 2004;26:346–352. doi: 10.1080/09638280410001658649. [DOI] [PubMed] [Google Scholar]
- 7.Mayo NE, Wood Dauphinee S, Ahmed S, Gordon C, Higgins J, Mc Ewen S, Salbach N. Disablement following stroke. Disabil Rehabil. 1999;21:258–268. doi: 10.1080/096382899297684. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF. World Health Organization; 2002. [Accessed January 20, 2015]. http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. [Google Scholar]
- 9.Mayo NE, Bronstein D, Scott SC, Finch LE, Miller S. Necessary and sufficient causes of participation post-stroke: practical and philosophical perspectives. Qual Life Res. 2014;23:39–47. doi: 10.1007/s11136-013-0441-6. [DOI] [PubMed] [Google Scholar]
- 10.Levasseur M, Richard L, Gauvin L, Raymond A. Inventory and analysis of definitions of social participation found in the aging literature: Proposed taxonomy of social activities. Soc Sci Med. 2010;71:2141–2149. doi: 10.1016/j.socscimed.2010.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Network on the Disability Creation Process (INDCP) The Human Development Model - Disability Creation Process (HDM-DCP) [Accessed June 15, 2015];What is Social Participation? 2014 http://ripph.qc.ca/node/153.
- 12.Moher D, Liberati A, Tezlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mars G, Kempen G, Mesters I, Proot I, Van Eijk J. Characteristics of social participation as defined by older adults with a chronic physical illness. Disabil Rehabil. 2008;30:1298–1308. doi: 10.1080/09638280701623554. [DOI] [PubMed] [Google Scholar]
- 14.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 15.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Limpert E, Stahel WA, Abbt M. Log-normal distributions across the sciences: Keys and Clues. BioScience. 2001;51:341–352. [Google Scholar]
- 17.Matthews BA, Baker F, Spiller RL. Oncology professionals and patient requests for cancer support services. Support Care Cancer. 2004;12:731–738. doi: 10.1007/s00520-004-0647-9. [DOI] [PubMed] [Google Scholar]
- 18.Danielsson A, Willén C, Sunnerhagen KS. Is walking endurance associated with activity and participation late after stroke? Disabil Rehabil. 2011;33:2053–2057. doi: 10.3109/09638288.2011.560329. [DOI] [PubMed] [Google Scholar]
- 19.Weinrich M, Stuart M, Benvenuti F. Community-Based Exercise for Chronic Disease Management: An Italian Design for the United States? Neurorehabil Neural Repair. 2014;28:729–732. doi: 10.1177/1545968314531073. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Physical Activity. [Accessed January 30, 2015];Glossary of Terms. 2011 http://www.cdc.gov/physicalactivity/everyone/glossary/
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ada L, Dean CM, Lindley R. Randomized trial of treadmill training to improve walking in community-dwelling people after stroke: the AMBULATE trial. Int J Stroke. 2013;8:436–444. doi: 10.1111/j.1747-4949.2012.00934.x. [DOI] [PubMed] [Google Scholar]
- 23.Beinotti F, Christofoletti G, Correia N, Borges G. Effects of Horseback Riding Therapy on Quality of Life in Patients Post Stroke. Top Stroke Rehabil. 2013;20:226–232. doi: 10.1310/tsr2003-226. [DOI] [PubMed] [Google Scholar]
- 24.Chan DYL, Chan CCH, Au DKS. Motor relearning programme for stroke patients: A randomized controlled trial. Clin Rehabil. 2006;20:191–200. doi: 10.1191/0269215506cr930oa. [DOI] [PubMed] [Google Scholar]
- 25.Chumbler NR, Quigley P, Li X, et al. Effects of telerehabilitation on physical function and disability for stroke patients: a randomized, controlled trial. Stroke. 2012;43:2168–2174. doi: 10.1161/STROKEAHA.111.646943. [DOI] [PubMed] [Google Scholar]
- 26.Flansbjer UB, Lexell J, Brogardh C. Long-term benefits of progressive resistance training in chronic stroke: a 4-year follow-up. J Rehabil Med. 2012;44:218–221. doi: 10.2340/16501977-0936. [DOI] [PubMed] [Google Scholar]
- 27.Harrington R, Taylor G, Hollinghurst S, Reed M, Kay H, Wood VA. A community-based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clin Rehabil. 2010;24:3–15. doi: 10.1177/0269215509347437. [DOI] [PubMed] [Google Scholar]
- 28.Holmgren E, Lindstrom B, Gosman-Hedstrom G, Nyberg L, Wester P. What is the benefit of a high intensive exercise program? A randomized controlled trial. Adv Physiother. 2010;12:115–124. doi: 10.3109/14038196.2010.488272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Immink M, Hillier S, Petkov J. Randomized Controlled Trial of Yoga for Chronic Poststroke Hemiparesis: Motor Function, Mental Health, and Quality of Life Outcomes. Top Stroke Rehabil. 2014;21:256–71. doi: 10.1310/tsr2103-256. [DOI] [PubMed] [Google Scholar]
- 30.Katz-Leurer M, Carmeli E, Shochina M. The effect of early aerobic training on independence six months post stroke. Clin Rehabil. 2003;17:735–741. doi: 10.1191/0269215503cr671oa. [DOI] [PubMed] [Google Scholar]
- 31.Kendall E, Catalano T, Kuipers P, Posner N, Buys N, Charker J. Recovery following stroke: the role of self-management education. Soc Sci Med. 2007;64:735–746. doi: 10.1016/j.socscimed.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 32.Lai S-M, Studenski S, Richards L, et al. Therapeutic Exercise and Depressive Symptoms After Stroke. J Am Geriatr Soc. 2006;54:240–7. doi: 10.1111/j.1532-5415.2006.00573.x. [DOI] [PubMed] [Google Scholar]
- 33.Lennon O, Carey A, Gaffney N, Stephenson J, Blake C. A pilot randomized controlled trial to evaluate the benefit of the cardiac rehabilitation paradigm for the non-acute ischaemic stroke population. Clin Rehabil. 2008;22:125–133. doi: 10.1177/0269215507081580. [DOI] [PubMed] [Google Scholar]
- 34.Lund A, Michelet M, Wyller TB, Sandvik L, Sveen U. A lifestyle intervention as supplement to a physical activity programme in rehabilitation after stroke: a randomized controlled trial. Clin Rehabil. 2012;26:502–512. doi: 10.1177/0269215511429473. [DOI] [PubMed] [Google Scholar]
- 35.Markle-Reid M, Orridge C, Weir R, et al. Interprofessional stroke rehabilitation for stroke survivors using home care. Can J Neurol Sci. 2011;38:317–334. doi: 10.1017/s0317167100011537. [DOI] [PubMed] [Google Scholar]
- 36.Marsden D, Quinn R, Pond N, et al. A multidisciplinary group programme in rural settings for community-dwelling chronic stroke survivors and their carers: a pilot randomized controlled trial. Clin Rehabil. 2010;24:328–341. doi: 10.1177/0269215509344268. [DOI] [PubMed] [Google Scholar]
- 37.Mayo N, Anderson S, Barclay R, et al. Getting on with the Rest of Your Life after Stroke: Evaluation of a Complex Intervention Aimed at Enhanced Life Participation Post-Stroke. [Accessed March 30, 2015];Clin Rehabil. 2015 doi: 10.1177/0269215514565396. published online ahead of print January 27, 2015. Available at: http://cre.sagepub.com/cgi/doi/10.1177/0269215514565396. [DOI] [PubMed]
- 38.Nadeau SE, Wu SS, Dobkin BH, et al. Effects of task-specific and impairment-based training compared with usual care on functional walking ability after inpatient stroke rehabilitation: LEAPS Trial. Neurorehabil Neural Repair. 2013;27:370–380. doi: 10.1177/1545968313481284. [DOI] [PubMed] [Google Scholar]
- 39.Ostwald SK, Godwin KM, Cron SG, Kelley CP, Hersch G, Davis S. Home-based psychoeducational and mailed information programs for stroke-caregiving dyads post-discharge: a randomized trial. Disabil Rehabil. 2014;36:55–62. doi: 10.3109/09638288.2013.777806. [DOI] [PubMed] [Google Scholar]
- 40.Ouellette MM, LeBrasseur NK, Bean JF, et al. High-intensity resistance training improves muscle strength, self-reported function, and disability in long-term stroke survivors. Stroke. 2004;35:1404–1409. doi: 10.1161/01.STR.0000127785.73065.34. [DOI] [PubMed] [Google Scholar]
- 41.Rochette A, Korner-Bitensky N, Bishop D, et al. The YOU CALL-WE CALL randomized clinical trial impact of a multimodal support intervention after a mild stroke. Circ Cardiovasc Qual Outcomes. 2013;6:674–679. doi: 10.1161/CIRCOUTCOMES.113.000375. [DOI] [PubMed] [Google Scholar]
- 42.Rydwik E, Eliasson S, Akner G. The effect of exercise of the affected foot in stroke patients-a randomized controlled pilot trial. Clin Rehabil. 2006;20:645–55. doi: 10.1191/0269215506cre986oa. [DOI] [PubMed] [Google Scholar]
- 43.Shaughnessy M, Michael K, Resnick B. Impact of treadmill exercise on efficacy expectations, physical activity, and stroke recovery. J Neurosci Nurs. 2012;44:27–35. doi: 10.1097/JNN.0b013e31823ae4b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith PS, Thompson M. Treadmill training post stroke: are there any secondary benefits? A pilot study. Clin Rehabil. 2008;22:997–1002. doi: 10.1177/0269215508088988. [DOI] [PubMed] [Google Scholar]
- 45.Studenski S, Duncan PW, Perera S, Reker D, Lai SM, Richards L. Daily functioning and quality of life in a randomized controlled trial of therapeutic exercise for subacute stroke survivors. Stroke. 2005;36:1764–1770. doi: 10.1161/01.STR.0000174192.87887.70. [DOI] [PubMed] [Google Scholar]
- 46.Woodman P, Riazi A, Pereira C, Jones F. Social participation post stroke: a meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disabil Rehabil. 2014;36:2031–2043. doi: 10.3109/09638288.2014.887796. [DOI] [PubMed] [Google Scholar]
- 47.Lang CE, MacDonald JR, Reisman DS, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil. 2009;90:1692–8. doi: 10.1016/j.apmr.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Globas C, Becker C, Cerny J, et al. Chronic Stroke Survivors Benefit From High-Intensity Aerobic Treadmill Exercise: A Randomized Control Trial. Neurorehabil Neural Repair. 2012;26:85–95. doi: 10.1177/1545968311418675. [DOI] [PubMed] [Google Scholar]
- 49.Duncan P, Studenski S, Richards L, et al. Randomized clinical trial of therapeutic exercise in subacute stroke. Stroke. 2003;34:2173–2180. doi: 10.1161/01.STR.0000083699.95351.F2. [DOI] [PubMed] [Google Scholar]
- 50.Eng JJ, Reime B. Exercise for depressive symptoms in stroke patients: A systematic review and meta-analysis. Clin Rehabil. 2014;28:731–9. doi: 10.1177/0269215514523631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen M, Rimmer J. Effects of exercise on quality of life in stroke survivors A meta-analysis. Stroke. 2011;42:832–7. doi: 10.1161/STROKEAHA.110.607747. [DOI] [PubMed] [Google Scholar]
- 52.Simpson LA, Eng JJ, Tawashy AE. Exercise perceptions among people with stroke: Barriers and facilitators to participation. Int J Ther Rehabil. 2011;18:520–530. doi: 10.12968/ijtr.2011.18.9.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morris J, Oliver T, Kroll T, Macgillivray S. The importance of psychological and social factors in influencing the uptake and maintenance of physical activity after stroke: A structured review of the empirical literature. Stroke Res Treat. 2012:195249. doi: 10.1155/2012/195249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tuffy A. “Back in the usual normal world”. Barriers and enablers to exercise and community participation after stroke: the role of community health and support services. [Accessed January 18, 2015];FINAL REPORT: Rural Research and Capacity Building Program Health Education and Training Institute (HETI) 2010 http://www.heti.nsw.gov.au/Global/rural/completed-projects/amanda-tutty-final-report.pdf.
- 55.Reed M, Harrington R, Duggan Á, Wood VA. Meeting stroke survivors’ perceived needs: A qualitative study of a community-based exercise and education scheme. Clin Rehabil. 2010;24:16–25. doi: 10.1177/0269215509347433. [DOI] [PubMed] [Google Scholar]
- 56.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8:741–754. doi: 10.1016/S1474-4422(09)70150-4. [DOI] [PubMed] [Google Scholar]