Abstract
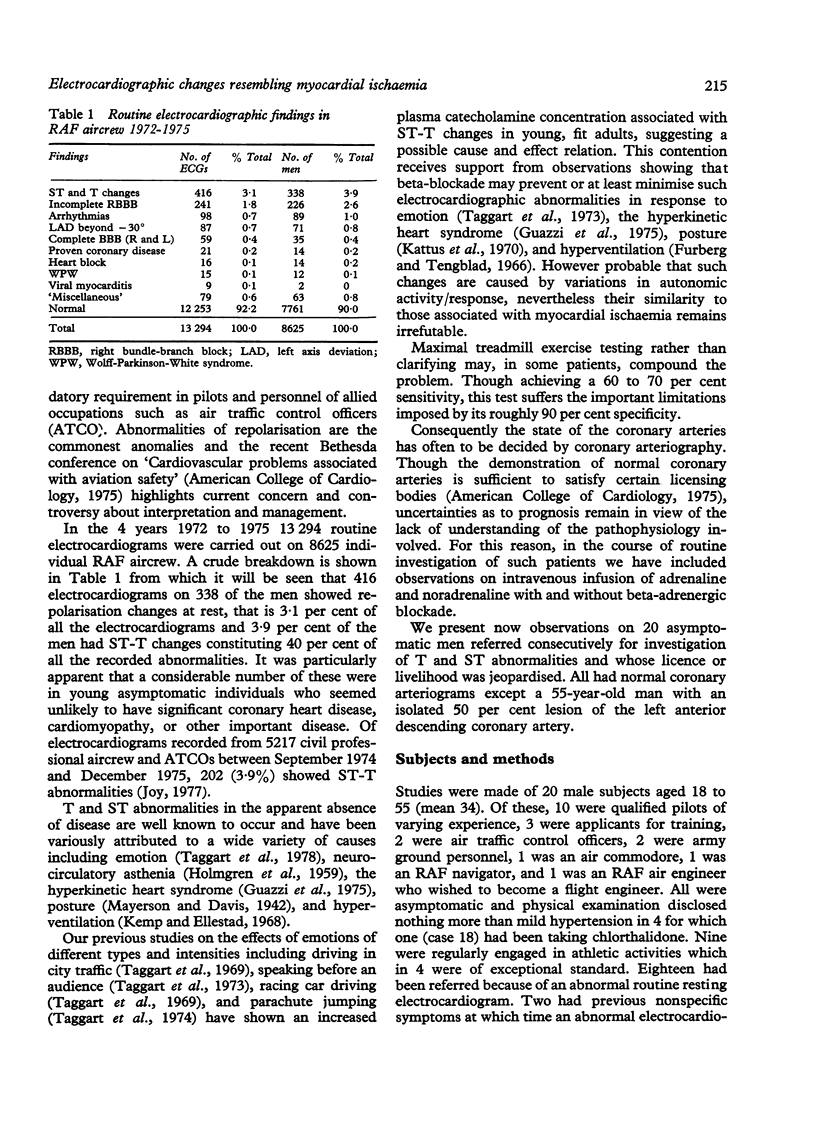
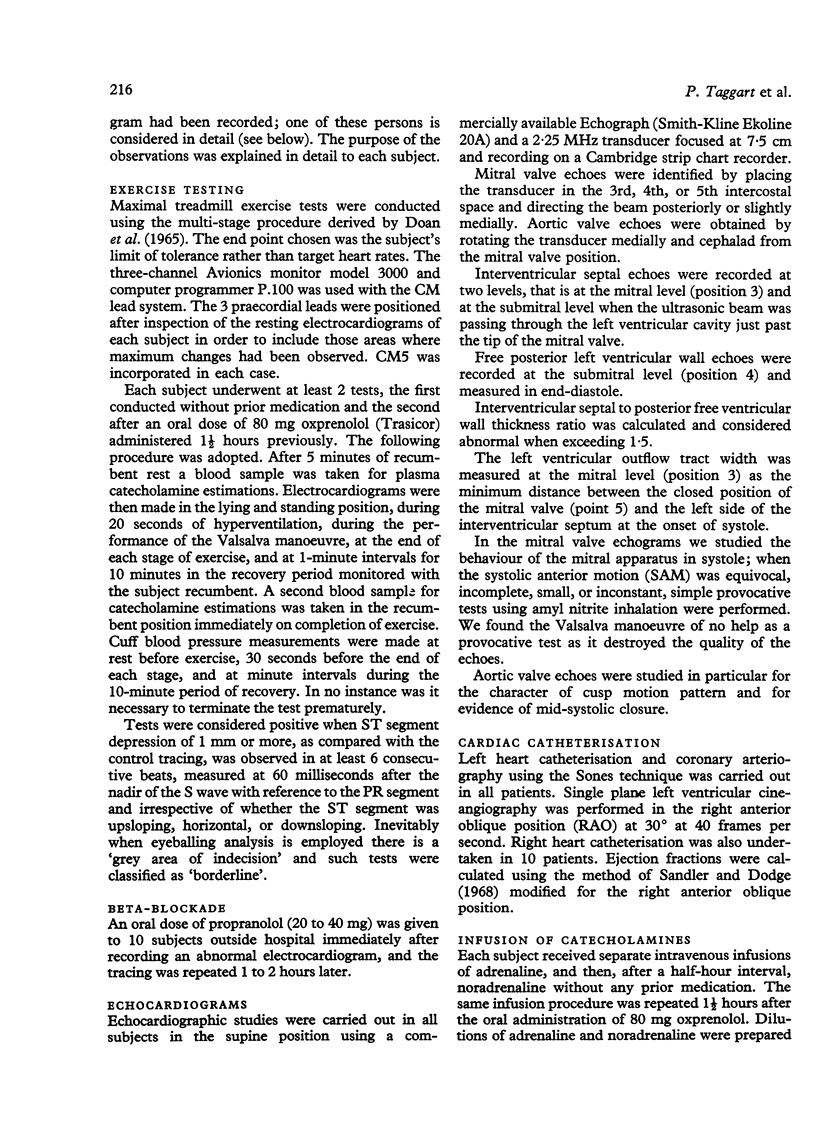
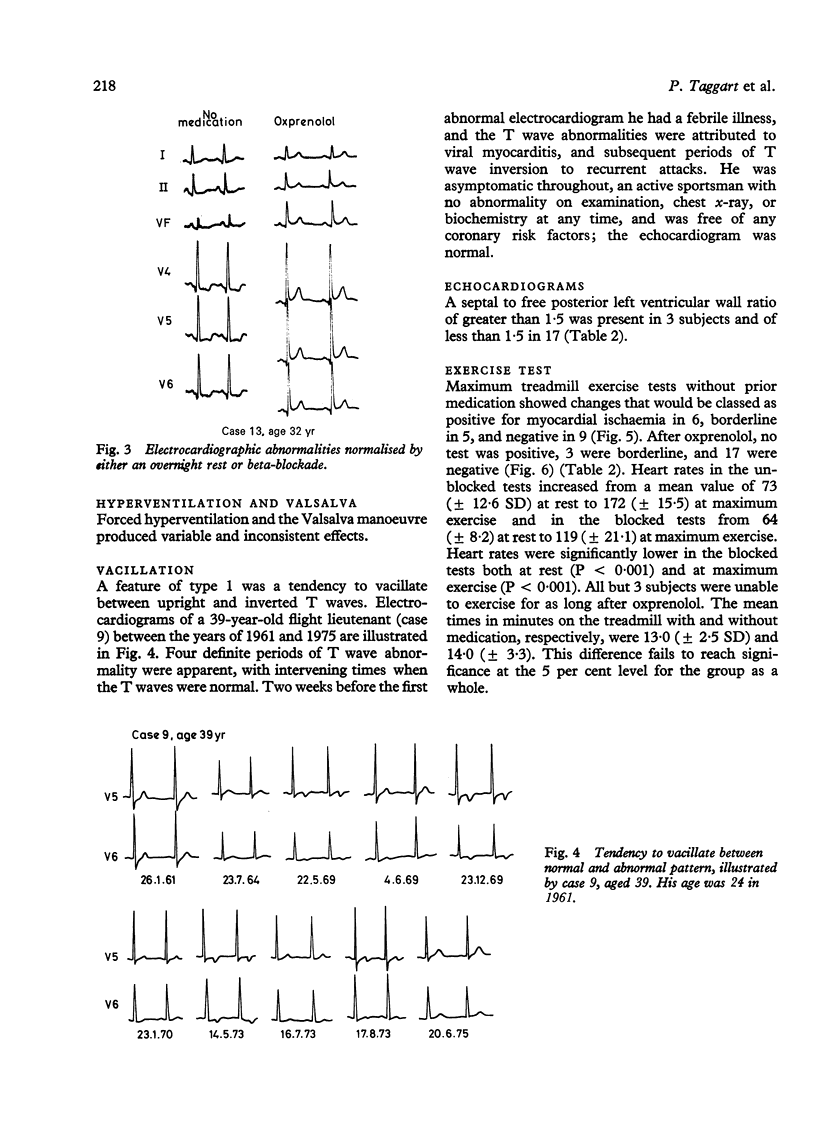
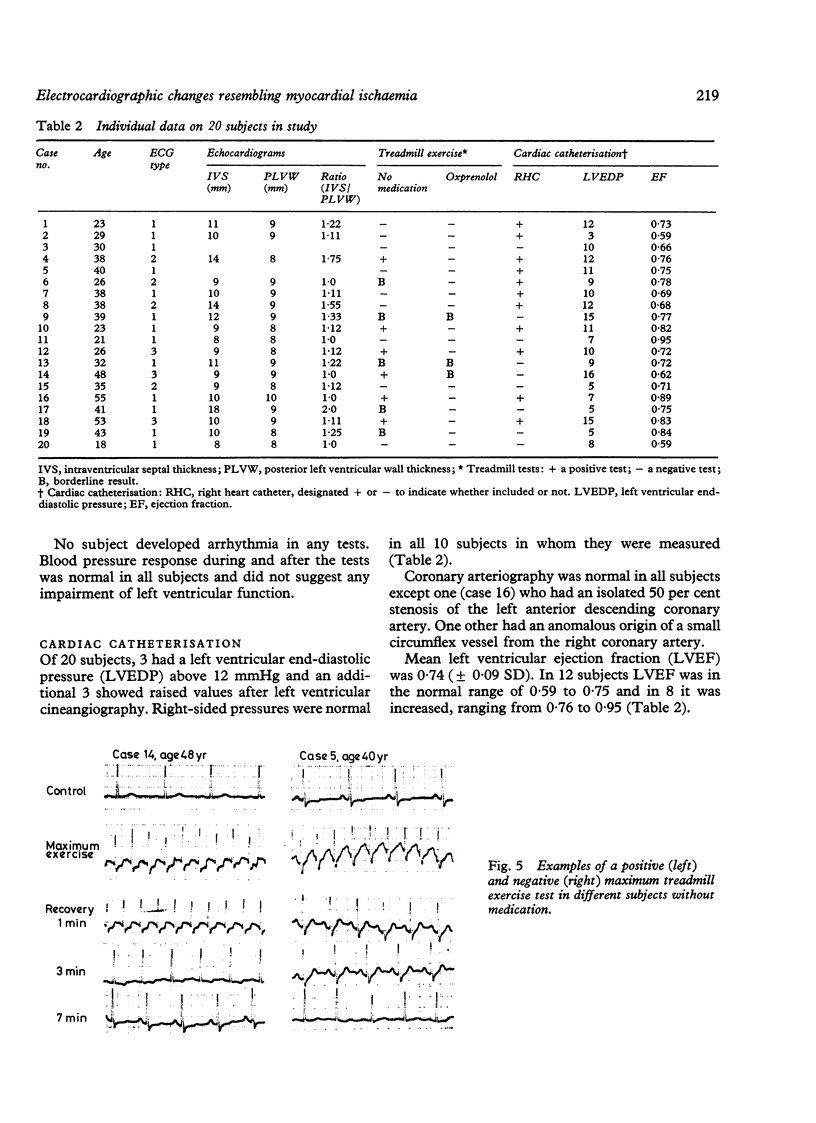
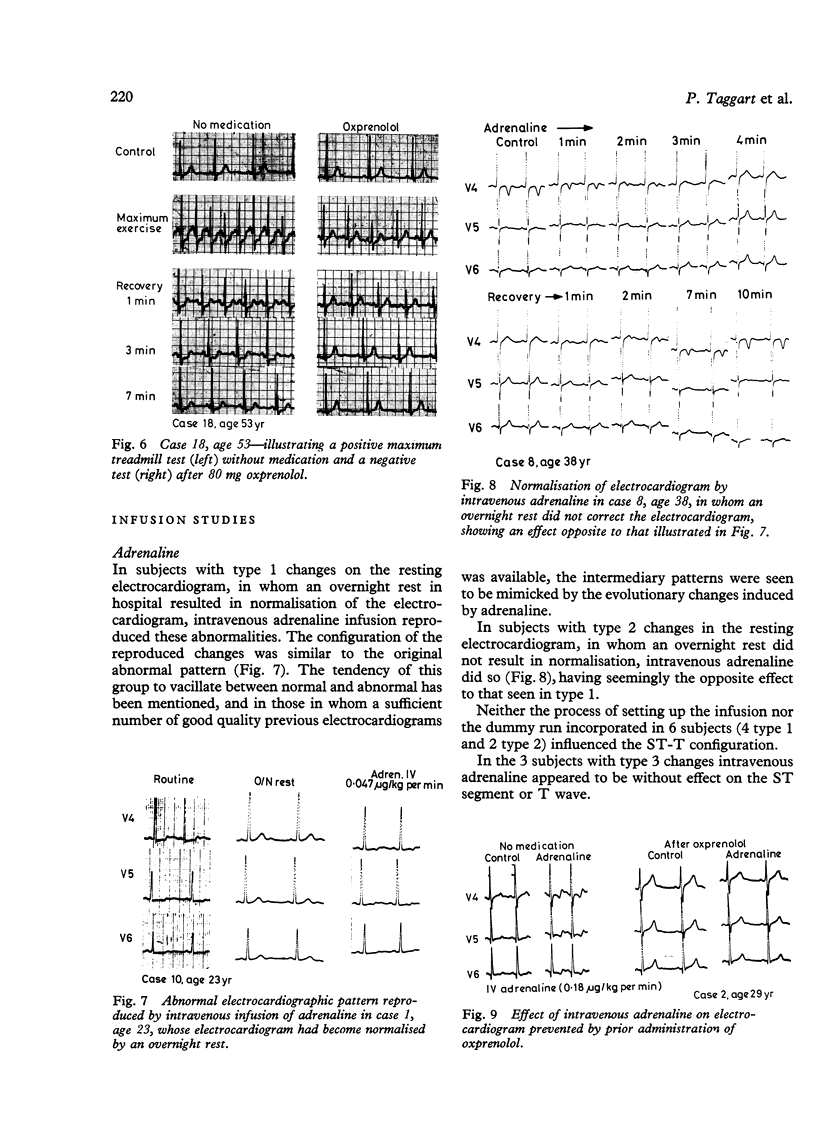
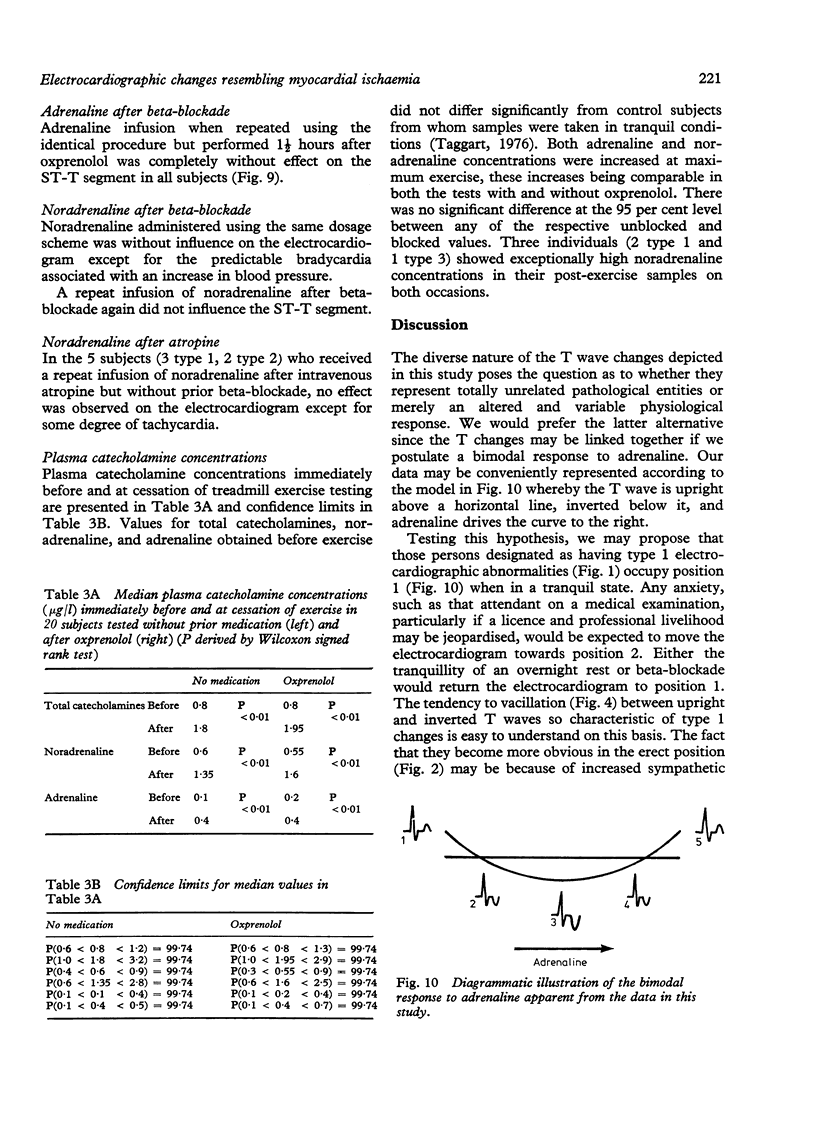
T wave and ST segment abnormalities in 20 asymptomatic men aged 18 to 55 were investigated because they were identical with myocardial ischaemic changes, and the professional livelihood of the subjects was jeopardised. Coronary arteriograms showed unobstructed arteries in all except one in whom a 50 per cent lesion of the left anterior descending artery was present. Left ventricular angiograms showed a normal contraction pattern, Ejection fractions were normal in 12 and increased in 8. Three characteristic electrocardiographic patterns were observed: flat or inverted T waves in leads II, III, aVF, and V4 to 6 designated type 1; deep T inversion particularly evident in leads V2 to 5 designated type 2, and minor ST segment depression in the inferior and lateral leads without T changes designated type 3. Characteristically, type 1 changes were temporarily suppressed by either beta-blockade or an overnight rest and were more abnormal in the standing position. Type 2 and 3 changes were relatively uninfluenced by these manoeuvres. Maximal treadmill exercise tests were positive in 6 and borderline or negative in 14. When repeated after oxprenolol all tests were negative. Echocardiograms showed asymmetric septal hypertrophy in 3 subjects (ratio of greater than 1.5 between ventricular septum and posterior left ventricular wall). After normalisation by an overnight rest, type 1 T wave abnormalities were reproduced by intravenous adrenaline infusion (0.024 to 0.18 microgram/kg/min) but not by noradrenaline or by adrenaline after prior administration of oxprenolol. When the T waves had remained deeply inverted before infusion despite rest (type 2) adrenaline infusion normalised them and again noradrenaline was without effect. This effect was also prevented by oxprenolol. Type 3 changes were uninfluenced by catecholamine infusion. Plasma catecholamine estimations suggest that catecholamine hypersecretion and hypersensitivity may both be relevant, particularly the latter. The apparent bimodal response of the ventricular myocardium to adrenaline infusion is not surprising since in vitro experiments suggest that reversal of T wave polarity in either direction may result from summation of changes in action potential duration in different parts of the heart. Such changes may be unimodal, that is both areas involved show lengthening or shortening of action potential duration, but by occurring at different rates may lead to a bimodal change in the differences in duration which generate the T wave.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adrian R. H., Channell R. C., Cohen I., Noble D. The Einthoven string galvanometer and the interpretation of the T wave of the electrocardiogram [proceedings]. J Physiol. 1976 Dec;263(1):67P–70P. [PubMed] [Google Scholar]
- Carruthers M., Conway N., Somerville W., Taggart P., Bates D. Validity of plasma-catecholamine estimations. Lancet. 1970 Jul 11;1(7663):62–67. doi: 10.1016/s0140-6736(70)92638-3. [DOI] [PubMed] [Google Scholar]
- Cohen I., Giles W., Noble D. Cellular basis for the T wave of the electrocardiogram. Nature. 1976 Aug 19;262(5570):657–661. doi: 10.1038/262657a0. [DOI] [PubMed] [Google Scholar]
- DOAN A. E., PETERSON D. R., BLACKMON J. R., BRUCE R. A. MYOCARDIAL ISCHEMIA AFTER MAXIMAL EXERCISE IN HEALTHY MEN. A METHOD FOR DETECTING POTENTIAL CORONARY HEART DISEASE? Am Heart J. 1965 Jan;69:11–21. doi: 10.1016/0002-8703(65)90211-5. [DOI] [PubMed] [Google Scholar]
- Friesinger G. C., Biern R. O., Likar I., Mason R. E. Exercise electrocardiography and vasoregulatory abnormalities. Am J Cardiol. 1972 Nov;30(7):733–740. doi: 10.1016/0002-9149(72)90147-6. [DOI] [PubMed] [Google Scholar]
- Furberg C. Adrenergic beta-blockade and electrocardiographical ST-T changes. Acta Med Scand. 1967 Jan;181(1):21–32. doi: 10.1111/j.0954-6820.1967.tb07221.x. [DOI] [PubMed] [Google Scholar]
- Furberg C., Tengblad C. F. Adrenergic beta-receptor blockade and the effect of hyperventilation on the electrocardiogram. Scand J Clin Lab Invest. 1966;18(5):467–472. doi: 10.3109/00365516609103907. [DOI] [PubMed] [Google Scholar]
- GARDBERG M., ROSEN I. L. The effects of nonpathologic factors on the electrocardiogram. II. Analysis. Am Heart J. 1957 May;53(5):711–734. doi: 10.1016/0002-8703(57)90340-x. [DOI] [PubMed] [Google Scholar]
- Giotti A., Ledda F., Mannaioni P. F. Effects of noradrenaline and isoprenaline, in combination with - and -receptor blocking substances, on the action potential of cardiac Purkinje fibres. J Physiol. 1973 Feb;229(1):99–113. doi: 10.1113/jphysiol.1973.sp010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guazzi M., Fiorentini C., Polese A., Magrini F., Olivari M. T. Stress-induced and sympathetically-mediated electrocardiographic and circulatory variations in the primary hyperkinetic heart syndrome. Cardiovasc Res. 1975 May;9(3):342–354. doi: 10.1093/cvr/9.3.342. [DOI] [PubMed] [Google Scholar]
- HOLMGREN A., JONSSON B., LEVANDER M., LINDERHOLM H., SJOSTRAND T., STROM G. ECG changes in vasoregulatory asthenia and the effect of physical training. Acta Med Scand. 1959 Nov 18;165:259–271. doi: 10.1111/j.0954-6820.1959.tb14499.x. [DOI] [PubMed] [Google Scholar]
- JOHANSSON B., VENDSALU A. The influence of adrenaline, nor-adrenaline, and acetylcholine on the electrocardiogram of the isolated perfused guinea-pig heart. Acta Physiol Scand. 1957 Jul 1;39(4):356–369. doi: 10.1111/j.1748-1716.1957.tb01434.x. [DOI] [PubMed] [Google Scholar]
- Jackson W. B. The use of propranalol in ECG diagnosis. N Z Med J. 1971 Feb;73(465):65–68. [PubMed] [Google Scholar]
- Jacobs W. F., Battle W. E., Ronan J. A., Jr False-positive ST-T-wave changes secondary to hyperventilation and exercise. A cineangiographic correlation. Ann Intern Med. 1974 Oct;81(4):479–482. doi: 10.7326/0003-4819-81-4-479. [DOI] [PubMed] [Google Scholar]
- Kemp G. L., Ellestad M. H. The significance of hyperventilative and orthostatic T-wave changes on the electrocardiogram. Arch Intern Med. 1968 Jun;121(6):518–523. [PubMed] [Google Scholar]
- Kuo C. S., Surawicz B. Ventricular monophasic action potential changes associated with neurogenic T wave abnormalities and isoproterenol administration in dogs. Am J Cardiol. 1976 Aug;38(2):170–177. doi: 10.1016/0002-9149(76)90145-4. [DOI] [PubMed] [Google Scholar]
- LEPESCHKIN E., MARCHET H., SCHROEDER G., WAGNER R., de PAULA E SILVA, RAAB W. Effect of epinephrine and norepinephrine on the electrocardiogram of 100 normal subjects. Am J Cardiol. 1960 May;5:594–603. doi: 10.1016/0002-9149(60)90124-7. [DOI] [PubMed] [Google Scholar]
- LITTMAN A., GROSSMAN M. I., GUNNAR R. M., ISAACS J. H., HIRSCHMANN J. H., FOLEY E. F. Electrocardiographic effects of arterenol and isopropylarterenol in man, with a note on the auricular T wave. J Appl Physiol. 1950 Nov;3(5):235–242. doi: 10.1152/jappl.1950.3.5.235. [DOI] [PubMed] [Google Scholar]
- Mines G. R. On functional analysis by the action of electrolytes. J Physiol. 1913 Jun 19;46(3):188–235. doi: 10.1113/jphysiol.1913.sp001588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordenfelt O. Orthostatic ECG changes and the adrenergic beta-receptor blocking agent, propranolol (Inderal). Acta Med Scand. 1965 Oct;178(4):393–401. doi: 10.1111/j.0954-6820.1965.tb04284.x. [DOI] [PubMed] [Google Scholar]
- Noskowicz T., Chrzanowski W. The influence of propranolol on functional alterations of the electrocardiogram. Cardiologia. 1968;52(6):324–329. doi: 10.1159/000166134. [DOI] [PubMed] [Google Scholar]
- Prichard B. N., Gillam P. M. Assessment of propranolol in angina pectoris. Clinical dose response curve and effect on electrocardiogram at rest and on exercise. Br Heart J. 1971 Jul;33(4):473–480. doi: 10.1136/hrt.33.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler H., Dodge H. T. The use of single plane angiocardiograms for the calculation of left ventricular volume in man. Am Heart J. 1968 Mar;75(3):325–334. doi: 10.1016/0002-8703(68)90089-6. [DOI] [PubMed] [Google Scholar]
- Taggart P., Gibbons D., Somerville W. Some effects of motor-car driving on the normal and abnormal heart. Br Med J. 1969 Oct 18;4(5676):130–134. doi: 10.1136/bmj.4.5676.130. [DOI] [PMC free article] [PubMed] [Google Scholar]



