Abstract
Study Design A systematic review of the literature.
Objectives To review the published results to date of motion-preserving direct reconstruction of C1 ring fractures with combined coronal plane displacement of at least 7 mm (rule of Spence) and so at risk for Dickman type I or II disruption of the transverse atlantal ligament (TAL).
Methods A structured literature review prompted by successful management of a typical case.
Results To date only 65 such cases are reported and follow-up is almost uniformly short. Although reported clinical success is uniform, the case mix is heterogenous and confirmation/classification of ligamentous injury at baseline is often lacking.
Conclusions Direct C1 stabilization shows promise as a “more selective” option in managing displaced atlas fractures with probable TAL disruption but cannot yet be recommended as a practice standard. Prospective clinical studies are indicated and should be structured so as to differentiate between Dickman type I and type II injuries of the TAL.
Keywords: atlas, fracture, displacement, instability, transverse atlantal ligament
Introduction
Isolated fractures of the atlas vertebra are relatively rare and the management of these injuries are largely dependent on the integrity of the transverse atlantal ligament (TAL).1 2 3 4 5 6 7 These injuries were first classified by Dickman et al as type I (intraligamentous disruption) or type II (avulsion of the ligament's bony insertion).5 6 In cases where the TAL is completely disrupted (Dickman type I injuries) and surgical intervention is considered, the current literature recommends fusing the atlas to an adjacent level to prevent late atlantoaxial instability and degenerative arthritis.8 9 10 11 12 13 Unfortunately, this intervention results in substantial loss of cervical range of motion with significant functional and occupational implications.14
Growing evidence from several case reports and cohort studies suggests that these fractures can be successfully treated with solitary atlas fixation without the need for adjacent-level instrumentation or fusion.15 16 17 18 19 20 21 22 23 24 25
We present an illustrative case of solitary C1 fixation for unstable atlas fracture with short-term follow-up and a systematic review of the available literature on this controversial advance in “more selective surgery.”26
Case Report
A 52-year-old healthy laborer presented to the emergency department after falling headfirst off of his bicycle and sustaining an axial load injury to his head with acute onset of proximal neck pain and no neurologic deficits. Plain film and computed tomography (CT) imaging identified an isolated minimally displaced two-part bursting fracture of the atlas with an incidental developmentally bifid posterior arch, and the patient was initially treated on an ambulatory basis in a rigid cervical orthosis with planned weekly clinical reevaluation. Over the next 2 weeks, the patient exhibited increasing clinical torticollis with incremental widening and displacement of the C1 lateral masses on radiographs (Fig. 1) and CT scan (Fig. 2), suggesting complete disruption of the TAL and inherent instability of the fracture. After a thorough discussion of the treatment options with a particular focus on the patient's restoration of function and occupational expectations, a decision was made to attempt solitary surgical fixation of the atlas ring hoping to maintain atlantoaxial motion, with the understanding that any possible late atlantoaxial instability would necessitate adjacent cervical fusion on a delayed basis.
Fig. 1.

Anteroposterior radiograph at 3 weeks postinjury showing widening of C1.
Fig. 2.
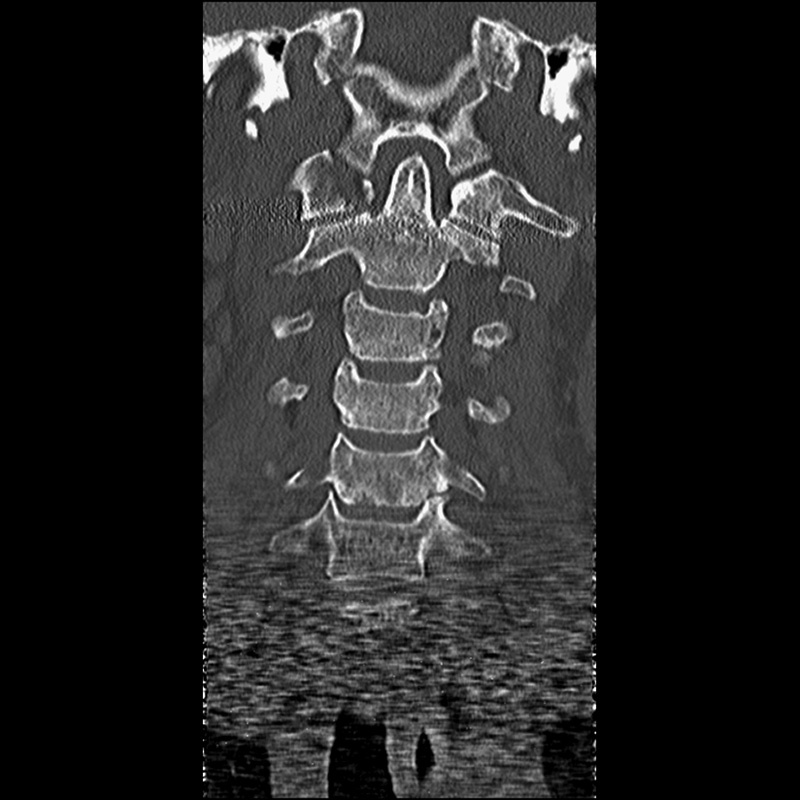
Coronal plane computed tomography scan demonstrating the displaced injury at C1.
Approximately 3 weeks after his initial injury, the patient underwent a solitary open reduction and fixation of his atlas vertebra. Cranial skeletal traction was employed to provide ligamentotaxis and help reduce the fracture fragments, and a standard open posterior midline approach was used to carefully dissect and expose the first cervical vertebra to access the lateral masses for placement of bilateral 3.5 × 32-mm Vertex Reconstruction Multi-Axial screws (Medtronic, Mississauga, Ontario, Canada). Screws were placed at C1 under fluoroscopic guidance, and compression was then applied across a titanium rod to which the screws were attached.
Postoperatively, the patient wore a rigid cervical orthosis for 6 weeks followed by a gradual return to full activities. At 6-month follow-up, he was pain-free, fully active, and working with ∼20 degrees loss of cervical rotation to the left compared with a full 90-degree arc on the right. CT scan (Fig. 3A, 3B) and dynamic radiography (Fig. 4A, 4B) demonstrated no atlantoaxial instability with good fracture alignment with preliminary osseous bridging of the fracture. The patient was allowed to resume full vocational activities with no restrictions and has not since returned to clinic.
Fig. 3.
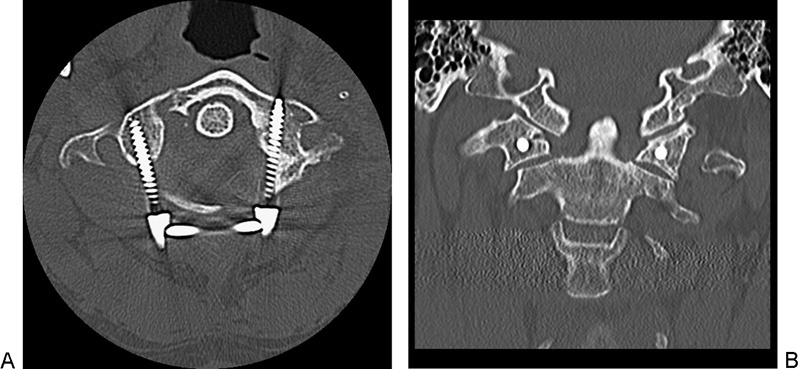
(A) Axial computed tomography (CT) at 6 months showing arch approximation and early healing. (B) Corresponding coronal CT image at 6 months.
Fig. 4.
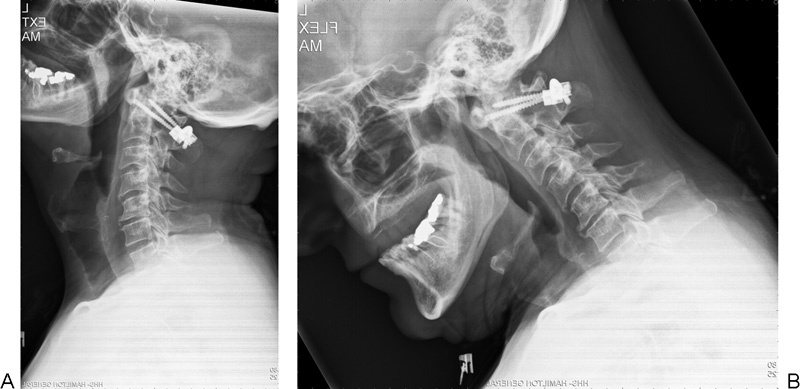
(A) Late radiograph, extension. (B) Late radiograph, flexion.
Search Methodology and Selection
We performed a structured literature search in the English language using the Medline, PubMed, Embase, and Cochrane library databases from the available periods of 1966 to 2014 using the following combinations of keyword terms: “isolated” OR “solitary,” AND “atlas,” AND “fracture” OR “fixation” OR “treatment.” The search was expanded using the “find similar” and “find citing articles” features of the Medline database and the “related articles” feature of the PubMed database. Duplicate studies were removed, leaving 491 articles, of which 292 were excluded based on their titles and 157 based on their abstracts. The remaining 42 articles were read, and we excluded 35 based on our inclusion and exclusion criteria (Fig. 5). Studies were included if they employed a single-level surgical fixation method of an isolated cervical-spine atlas fracture. Exclusion factors included studies with nonisolated atlas injuries of the cervical spine, nonoperative management of isolated atlas fractures, or operative management using adjacent-level fixation methods; studies without clinical or radiographic outcome assessments; and studies that failed to define their preoperative indications for surgical management. We were left with seven articles to include in our review. No level I or II studies have been published on isolated atlas fracture treatment, and although some case series have included in excess of 100 atlas fractures, virtually all current evidence-based surgical recommendations are generated from small observational case series (Fig. 5).
Fig. 5.
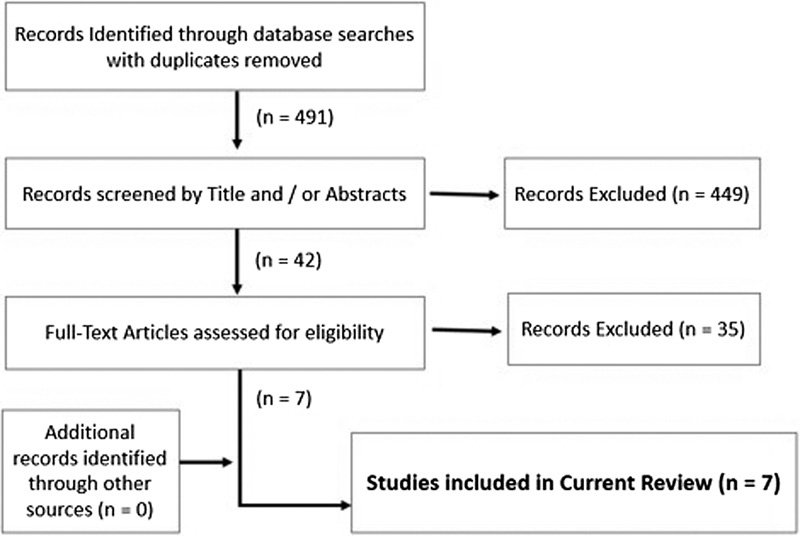
Search methodology.
Background
The first cervical vertebra, named the atlas after the Greek mythological figure who was condemned by Zeus to hold up the celestial spheres, is a ring-shaped structure formed by an anterior and posterior ring that are joined by two lateral masses.27 This first vertebra of the spinal column lacks a vertebral body or spinous process. Its anterior arch contains a central enlargement known as the median anterior tubercle to which the longus colli muscular attaches, as well as the fovea dentis, a cartilaginous recession on its posterior surface that articulates with the odontoid process of the second vertebra to form a synovial joint. The outer half of the posterior ring contains bilateral grooves known as the sulcus arteriae, along which the vertebral artery and first spinal nerve travel, as well as a central enlargement known as the median posterior tubercle, which attaches to the nuchal ligament. The trapezoidal-shaped lateral masses have superior and inferior articular facets that communicate with the articular surfaces of the occiput and axial vertebra, respectively. The thick TAL attaches to the medial surfaces of the lateral masses and helps maintain the odontoid process in contact with the fovea dentis of the axis. The combination of these anatomic features allows the atlas to contribute to approximately half of the rotational and flexion movements of the head and neck.
Epidemiology
Fractures commonly occur at the junction of the anterior and posterior rings with the lateral masses of the atlas, accounting for ∼10 to 13% of cervical spine fractures and 1 to 2% of all acute spine injuries.1 2 3 4 5 6 10 12 13 Even though the literature reports considerable variability, the two most commonly reported injury mechanisms are motor vehicle accidents (30 to 85%) and falls (13 to 69%).
Pathophysiology
Frequently, fractures occur in combination with other spinal injuries, of which the second cervical vertebra is the most commonly associated fracture level (40 to 44%).10 12 13 Temporary quadriplegia or hemiparesis has been reported in up to 33% of patients but these injuries typically widen the spinal canal space and therefore rarely result in permanent neurologic deficits. Associated vertebral artery injuries are also rare but can present acutely in the form of dissections or occlusions or chronically as stenotic vasculopathies with variable symptom constellations including Wallenberg syndrome or “bow-hunter” syndrome, which presents as intermittent contralateral hemiparesis and hemiplegia due to vertebral artery stenosis during end-range rotational movements of the cervical spine.28 Likewise, because several cranial nerves travel within 8 mm of the transverse processes of the atlas as they exit the skull, burst-type fractures can compress these structures and typically present as Collet-Sicard syndrome,1 a unilateral palsy of the lower cranial nerves IX to XII.29 30 When associated with head injuries in this trauma population, cranial nerve deficits are often attributed to intracerebral injuries and can result in delayed diagnosis.
Most atlas fractures do not result in significant neurologic deficits. Long-term outcomes include a relatively high incidence of chronic complaints including cervical pain, greater occipital neuralgia, headaches, neck stiffness, and limited range of motion in up to 80% of patients.12 13 Most patients fail to completely return to their preinjury state of health though their functional and quality-of-life outcomes approximate those of the general population within 5 years of their injury.14
Classification
Classification systems and eponyms have played a more descriptive role in atlas fractures, with most authors recognizing that the TAL integrity is the fundamental factor guiding management.1 2 3 4 9 The term Jefferson' fracture is often used as a misnomer to specifically describe a four-part burst fracture pattern of the atlas ring, but Jefferson's original 1920 review publication included several two-, three-, and four-part burst fractures of which only 3 of the 42 cases he reviewed specifically described a four-part fracture pattern.1 Beyond the commonly used eponyms, the two most common fracture classification systems are those of Levine and Edwards9 and Landell and Van Peteghem.4 Both require CT evaluation, are generally descriptive, and fail to reliably predict fracture instability.31 As a result, most authors now consider an atlas fracture “unstable” when the TAL is completely disrupted.
Traditionally, “open-mouth” radiographic imaging has been used to assess whether the TAL is disrupted by the finding of a combined lateral mass displacement of greater than 6.9 mm. This criterion is based on the 1970 biomechanical study of 10 cadavers by Spence and colleagues and now often referred to as the “rule of Spence.”3 However, Dickman et al later demonstrated that a magnetic resonance imaging (MRI)-based classification system was more reliable and that simply using the rule of Spence would have missed up to 61% of unstable atlas fractures in their case series.5 In the Dickman classification, TAL injuries are separated into type I (intrasubstance injuries with permanent disruption) and type II (avulsion-type injuries with maintained TAL integrity).14 In general, poorer outcomes can be expected with type I injuries and often necessitate adjacent vertebral-level fusion to avoid chronic atlantoaxial instability.
Classical Treatment
Although the majority of isolated atlas fractures can be treated nonoperatively, indications for surgical intervention are controversial, and no definitive guidelines currently exist.12 13 32
The most commonly reported method of treatment for isolated atlas fractures is the halo orthosis,32 even though no studies have reliably compared the various external immobilization methods (e.g., rigid cervical orthosis, Minerva cast, halo, and others), and all have been shown to provide good clinical outcomes for the majority of both stable and unstable atlas fractures.22 23 Most authors recommend initial nonoperative management of isolated atlas fractures, arguing that operative intervention can be performed on a delayed basis if residual instability is present after 8 weeks of external immobilization.1 2 3 4 5 6 7 8 9 10 11 12 13
In cases of complete TAL injuries or significantly comminuted and displaced lateral mass fractures, conservative management results in elevated nonunion rates, higher risk of long-term spondylosis and instability, and greater operative complications when late repairs are performed.7 8 9 10 11 12 13 14 Specifically, type I TAL injuries may be better treated with early surgical fixation due to irreversible atlantoaxial instability and deformity once sufficient arthrosis and scarring is present.14 Several studies have shown that unstable atlas fractures that are initially reduced by traction cannot be maintained by external immobilization due to constant shifting of a patient's “shoulder buttress”; radiographic imaging demonstrates significant mobility and realignment of the atlanto-dens interval as patients reposition themselves between standing, lying, and sitting.7 Nevertheless, due to the rarity of isolated displaced atlas fractures, no adequate studies have demonstrated superiority of any treatment method and no consensus yet exists for managing these injuries.22 23
Atlantoaxial fusion is the most commonly performed procedure with the justification that when the TAL is completely disrupted (i.e., type I TAL injury) it cannot heal,10 11 12 13 15 resulting in permanent atlantoaxial instability that can only be managed by fusing these two vertebral segments.7 15 This fusion results in significant loss of cervical range of motion.
Several authors have attempted solitary atlas fixation with the consideration that adequate stabilization and healing may allow secondary stabilizers and scarring to provide sufficient translational stability to compensate for TAL dysfunction (Table 1).6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 This concept is not novel and has been substantiated by the fact that external immobilization for unstable atlas fractures has significantly high success rates without requiring surgical stabilization and fusion.31 A recent biomechanical study has shown that even in cases of unstable atlas fractures with complete disruption of the TAL and a unilateral capsule release, atlantoaxial stability is restored under physiologic loads if the atlas fractures are fixed.7 Authors who have successfully performed solitary C1 fixation have reasoned that restoration of the atlas height and alignment provides adequate stability for healing of the secondary stabilizers, including the bilateral facet capsules, alar ligaments, and tectorial membrane, to restore atlantoaxial stability. These findings have been validated in a cadaveric study of axial-load injuries to the atlas.7 The phenomenon of restoring the relationship of the occipito-atlanto-axial complex to maintain adequate ligamentous tension and stability before and after healing has been referred to as the “buoy phenomenon” by Li and colleagues.23
Table 1. Summary of reports on solitary atlas fixation for isolated atlas fractures with TAL injury.
| First author and year | Study description | Indication | Evidence class | Follow-up duration (average) | Outcomes and assessment | Complications | Conclusions |
|---|---|---|---|---|---|---|---|
| Hu et al 201425 | Retrospective case series of 12 patients with isolated 3- to 4-part atlas fractures treated with posterior lateral mass screw–rod fixation | • CT and MRI confirmation of injury patterns: 7 with intact TAL, 5 with Dickman type II TAL injuries | IV | 22 mo | • CT and dynamic imaging confirmed osseous union in all patients and no evidence of atlantoaxial instability • Significant improvement of average patient pain scores |
• 3 cases of failed pedicle screw fixation converted to lateral mass fixation • One clinically insignificant partial pedicle screw breach into transverse foramen |
Atlas fractures with type II TAL injuries can be treated by solitary C1 screw–rod fixation |
| He et al 201426 | Retrospective case series of 22 patients with isolated atlas fractures treated with posterior lateral mass screw–plate fixation | • CT and MRI confirmation of injury patterns: TAL disruption in all patients • No mention of Dickman TAL injury pattern • 12 patients operated on for nonunion due to failed conservative management, 5 patients for residual atlantoaxial instability, no mention of indications for remaining 5 patients |
IV | 22.5 mo | • CT imaging confirmed osseous union in all patients • No dynamic imaging methods used to evaluate for atlantoaxial instability reported • “Good clinical” outcomes reported in all patients |
• None | Atlas fractures with TAL disruption (unknown injury pattern) and either nonunion or atlantoaxial instability can be treated with solitary C1 screw–plate fixation |
| Ma et al 201320 | Retrospective case series of 20 patients with isolated atlas fractures treated with anterior ring and lateral mass plating | • CT evaluation only, no MRIs • TAL disruption deduced from fracture characteristics • No mention of Dickman TAL injury pattern • 16 cases were nonunions after failed conservative management |
IV | 48.5 mo | • CT and dynamic imaging confirmed osseous union in all patients with no evidence of atlantoaxial instability • Significant improvement of average patient pain scores |
• Two screws breached the vertebral canal with no clinical consequences | Atlas fractures with TAL disruption (unknown injury pattern) can be treated with C1–anterior plate fixation |
| Iacoangeli et al 201219 | Retrospective case series of 2 patients with isolated atlas fracture nonunions treated with anterior ring and lateral mass fixation | • CT evaluation only, no mention of MRI • TAL disruption deduced from fracture characteristics • No mention of Dickman TAL injury pattern • Both patients developed nonunion with cranial settling after failed conservative management |
IV | 1 y | • CT imaging confirmed osseous union • No mention of atlantoaxial instability testing • Good outcomes reported in both patients |
Mild reduction in cervical rotation (∼15%) | Atlas fractures with nonunion and cranial settling (unknown TAL injury pattern) can be treated with anterior C1 ring fixation |
| Li et al 201123 | Retrospective case series of 2 patients with isolated atlas fractures treated with posterior lateral mass screw–rod fixation | • CT evaluation only, no mention of MRI • One patient with Dickman type II TAL injury, no mention of second patient TAL injury pattern |
IV | 12 mo | • CT and dynamic imaging confirmed osseous union in all patients with no evidence of atlantoaxial instability • Good outcomes reported in both patients |
None | Atlas fractures with TAL injury can be treated with direct posterior C1 lateral mass screw fixation |
| Jo et al 201124 | Retrospective case report of a patient with an isolated atlas fracture treated with posterior lateral mass screw–rod fixation | • CT and MRI confirmation of type II TAL injury pattern | IV | 8 mo | • CT and dynamic imaging confirmed osseous union with no evidence of atlantoaxial instability • Good outcomes reported in both patients |
None | Atlas fractures with type II TAL injury can be treated with solitary C1 screw–rod fixation |
| Ruf et al 200418 | Retrospective case series of 6 patients with isolated atlas fractures treated with anterior ring and lateral mass screw–rod fixation | • Plain radiography used to deduce TAL disruption based on fracture characteristics • MRI imaging available on 4 patients demonstrating a single type I TAL injury and 3 type II injuries |
IV | 6.4 y | • CT and dynamic imaging confirmed osseous union in all patients with no evidence of atlantoaxial instability • Except for a mild reduction in cervical range of motion, all patients reported good outcomes |
One patient with partial redislocation due to loosening of screw–rod connection | Transoral C1 fixation is a viable option for unstable Jefferson fractures; as long as alar ligament intact, soft tissue scarring after adequate bony realignment provides adequate atlantoaxial stability |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; TAL, transverse atlantal ligament.
Techniques of Direct C1 Fracture Stabilization
A review of the published techniques for solitary C1 fixation described two main approaches: an anterior transoral or transnasal approach and a posterior midline approach.18 19 20 21
The anterior approach to the atlantoaxial spine may be challenged by wound complication rates of up to 75%, dehiscence rates of 22%, and a lack of familiarity with these approaches among many spine surgeons,1 30 but the two largest series of anterior approaches specific to atlas fracture fixation did not report any significant postoperative complications, suggesting that the approach is a viable technique in experienced hands.18 20
Posterior approaches include lateral mass screw–rod or screw–plate constructs.22 23 24 25 Although virtually all solitary atlas fixation studies provide reliable postoperative documentation of atlantoaxial stability and clinical outcomes, standardized preoperative injury classification is often lacking. Unstable atlas fracture is typically defined as a ring fracture in combination with radiographic evidence of TAL disruption; however, the TAL injury pattern is rarely defined and most studies fail to obtain preoperative MRIs. Review of the reported clinical outcomes all suggest that solitary C1 fixation is a viable surgical option for most unstable atlas fractures with successful restoration of atlantoaxial stability on short-term follow-up. However, larger long-term cohort studies with MRI-confirmed type I injuries of the TAL will be necessary before traditional C1–C2 fusion techniques are superseded.
Conclusions
Isolated unstable atlas fractures are relatively rare and no consensus is available to definitely guide management. Although stable fractures without TAL injury can be confidently treated conservatively with external immobilization, unstable fractures with complete TAL disruption remain controversial. The 65 cases of solitary atlas fixation reported in the literature to date indicate that solitary C1 fixation is a viable operative technique with generally good outcomes and reliable restoration of atlantoaxial stability.18 19 20 21 22 23 24 25
We suggest that the best surgical indication for direct atlas fracture repair would be complete TAL insufficiency. This diagnosis could be made acutely by the observation of combined coronal plane atlas displacement greater than 7 mm or subacutely with progressive coronal plane displacement under conservative care. After fracture healing, translational C1–C2 stability should always be confirmed with flexion–extension radiographs as are routinely indicated after successful nonoperative care.
With increasingly supportive biomechanical and clinical evidence supporting restoration of surrounding secondary stabilizers, solitary atlas fixation may eventually provide an alternative approach for managing unstable atlas fractures with complete TAL disruption. Nevertheless, at this time no conclusions can be definitively drawn and traditional atlantoaxial fixation should remain the standard until better evidence from future anticipated progressive randomized trials becomes available.
Footnotes
Disclosures Drew A. Bednar, none Khaled A. Almansoori, none
References
- 1.Jefferson G. Fractures of the atlas vertebra. Report of four cases and a review of those previously recorded. Br J Surg. 1919;7(27):407–422. [Google Scholar]
- 2.Jefferson G. Remarks on fractures of the first cervical vertebra. BMJ. 1927;2(3473):153–157. doi: 10.1136/bmj.2.3473.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spence K F Jr, Decker S, Sell K W. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am. 1970;52(3):543–549. [PubMed] [Google Scholar]
- 4.Landells C D, Van Peteghem P K. Fractures of the atlas: classification, treatment and morbidity. Spine (Phila Pa 1976) 1988;13(5):450–452. doi: 10.1097/00007632-198805000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Dickman C A, Greene K A, Sonntag V K. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38(1):44–50. doi: 10.1097/00006123-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Dickman C A, Sonntag V K. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1997;40(4):886–887. doi: 10.1097/00006123-199704000-00061. [DOI] [PubMed] [Google Scholar]
- 7.Koller H, Resch H, Tauber M. et al. A biomechanical rationale for C1-ring osteosynthesis as treatment for displaced Jefferson burst fractures with incompetency of the transverse atlantal ligament. Eur Spine J. 2010;19(8):1288–1298. doi: 10.1007/s00586-010-1380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sonntag V K, Hadley M N, Dickman C A, Browner C M. Atlas fractures: treatment and long-term results. Acta Neurochir Suppl (Wien) 1988;43:63–68. doi: 10.1007/978-3-7091-8978-8_15. [DOI] [PubMed] [Google Scholar]
- 9.Levine A M, Edwards C C. Fractures of the atlas. J Bone Joint Surg Am. 1991;73(5):680–691. [PubMed] [Google Scholar]
- 10.Hadley M N Dickman C A Browner C M Sonntag V K Isolated fractures of the atlas in adults Neurosurgery 200250(3, Suppl):S120–S124. [DOI] [PubMed] [Google Scholar]
- 11.Kontautas E, Ambrozaitis K V, Kalesinskas R J, Spakauskas B. Management of acute traumatic atlas fractures. J Spinal Disord Tech. 2005;18(5):402–405. doi: 10.1097/01.bsd.0000177959.49721.3b. [DOI] [PubMed] [Google Scholar]
- 12.Kakarla U K Chang S W Theodore N Sonntag V KH Atlas fractures Neurosurgery 201066(3, Suppl):60–67. [DOI] [PubMed] [Google Scholar]
- 13.Ryken T C, Aarabi B, Dhall S S. et al. Management of isolated fractures of the atlas in adults. Neurosurgery. 2013;72 02:127–131. doi: 10.1227/NEU.0b013e318276ee2a. [DOI] [PubMed] [Google Scholar]
- 14.Dvorak M F, Johnson M G, Boyd M, Johnson G, Kwon B K, Fisher C G. Long-term health-related quality of life outcomes following Jefferson-type burst fractures of the atlas. J Neurosurg Spine. 2005;2(4):411–417. doi: 10.3171/spi.2005.2.4.0411. [DOI] [PubMed] [Google Scholar]
- 15.Hein C, Richter H-P, Rath S A. Atlantoaxial screw fixation for the treatment of isolated and combined unstable Jefferson fractures—experiences with 8 patients. Acta Neurochir (Wien) 2002;144(11):1187–1192. doi: 10.1007/s00701-002-0998-2. [DOI] [PubMed] [Google Scholar]
- 16.Dickman C Re: Ruf M, Melcher R, Harms J. Transoral reduction and osteosynthesis C1 as a function-preserving option in the treatment of unstable Jefferson fractures. Spine 2004;29:823–7 Spine (Phila Pa 1976) 200429192196, author reply 2197 [DOI] [PubMed] [Google Scholar]
- 17.Fiore A J, Haid R W, Rodts G E. et al. Atlantal lateral mass screws for posterior spinal reconstruction: technical note and case series. Neurosurg Focus. 2002;12(1):E5. doi: 10.3171/foc.2002.12.1.6. [DOI] [PubMed] [Google Scholar]
- 18.Ruf M, Melcher R, Harms J. Transoral reduction and osteosynthesis C1 as a function-preserving option in the treatment of unstable Jefferson fractures. Spine (Phila Pa 1976) 2004;29(7):823–827. doi: 10.1097/01.brs.0000116984.42466.7e. [DOI] [PubMed] [Google Scholar]
- 19.Iacoangeli M, Di Rienzo A, Alvaro L, Scerrati M. Fully endoscopic endonasal anterior C1 arch reconstruction as a function preserving surgical option for unstable atlas fractures. Acta Neurochir (Wien) 2012;154(10):1825–1826. doi: 10.1007/s00701-012-1471-5. [DOI] [PubMed] [Google Scholar]
- 20.Ma W, Xu N, Hu Y. et al. Unstable atlas fracture treatment by anterior plate C1-ring osteosynthesis using a transoral approach. Eur Spine J. 2013;22(10):2232–2239. doi: 10.1007/s00586-013-2870-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joaquim A F, Ghizoni E, Rubino P A. et al. Lateral mass screw fixation of the atlas: surgical technique and anatomy. World Neurosurg. 2010;74(2–3):359–362. doi: 10.1016/j.wneu.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Abeloos L, De Witte O, Walsdorff M, Delpierre I, Bruneau M. Posterior osteosynthesis of the atlas for nonconsolidated Jefferson fractures: a new surgical technique. Spine (Phila Pa 1976) 2011;36(20):E1360–E1363. doi: 10.1097/BRS.0b013e318206cf63. [DOI] [PubMed] [Google Scholar]
- 23.Li L, Teng H, Pan J. et al. Direct posterior C1 lateral mass screws compression reduction and osteosynthesis in the treatment of unstable Jefferson fractures. Spine (Phila Pa 1976) 2011;36(15):E1046–E1051. doi: 10.1097/BRS.0b013e3181fef78c. [DOI] [PubMed] [Google Scholar]
- 24.Jo K-W, Park I-S, Hong J T. Motion-preserving reduction and fixation of C1 Jefferson fracture using a C1 lateral mass screw construct. J Clin Neurosci. 2011;18(5):695–698. doi: 10.1016/j.jocn.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 25.Hu Y, Xu R-M, Albert T J. et al. Function-preserving reduction and fixation of unstable Jefferson fractures using a C1 posterior limited construct. J Spinal Disord Tech. 2014;27(6):E219–E225. doi: 10.1097/BSD.0b013e31829a36c5. [DOI] [PubMed] [Google Scholar]
- 26.He B, Yan L, Zhao Q, Chang Z, Hao D. Self-designed posterior atlas polyaxial lateral mass screw-plate fixation for unstable atlas fracture. Spine J. 2014;14(12):2892–2896. doi: 10.1016/j.spinee.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 27.Levine A M. Philadelphia, PA: Saunders; 1998. Fractures of the atlas: pathoanatomy; pp. 209–211. [Google Scholar]
- 28.Sorensen B F. Bow hunter's stroke. Neurosurgery. 1978;2(3):259–261. doi: 10.1227/00006123-197805000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Dettling S D, Morscher M A, Masin J S, Adamczyk M J. Cranial nerve IX and X impairment after a sports-related Jefferson (C1) fracture in a 16-year-old male: a case report. J Pediatr Orthop. 2013;33(3):e23–e27. doi: 10.1097/BPO.0b013e3182746bc1. [DOI] [PubMed] [Google Scholar]
- 30.Connolly B, Turner C, DeVine J, Gerlinger T. Jefferson fracture resulting in Collet-Sicard syndrome. Spine (Phila Pa 1976) 2000;25(3):395–398. doi: 10.1097/00007632-200002010-00023. [DOI] [PubMed] [Google Scholar]
- 31.Radcliff K E, Sonagli M A, Rodrigues L M, Sidhu G S, Albert T J, Vaccaro A R. Does C1 fracture displacement correlate with transverse ligament integrity? Orthop Surg. 2013;5(2):94–99. doi: 10.1111/os.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001;121(1–2):50–55. doi: 10.1007/s004020000182. [DOI] [PubMed] [Google Scholar]


