Abstract
Study Design Retrospective comparative study.
Objective To evaluate the accuracy of percutaneous pedicle screw (PPS) placement and intraoperative imaging time using dual fluoroscopy units and their differences between surgeons with more versus less experience.
Methods One hundred sixty-one patients who underwent lumbar fusion surgery were divided into two groups, A (n = 74) and B (n = 87), based on the performing surgeon's experience. The accuracy of PPS placement and radiation time for PPS insertion were compared. PPSs were inserted with classic technique under the assistance of dual fluoroscopy units placed in two planes. The breach definition of PPS misplacement was based on postoperative computed tomography (grade I: no breach; grade II: <2 mm; grade III: ≤2 to <4 mm).
Results Of 658 PPSs, only 21 screws were misplaced. The breach rates of groups A and B were 3.3% (grade II: 3.4%, grade III: 0%) and 3.1% (grade II: 2.6%, grade III: 0.6%; p = 0.91). One patient in grade III misplacement had a transient symptom of leg numbness. Median radiation exposure time during PPS insertion was 25 seconds and 51 seconds, respectively (p < 0.01).
Conclusions Without using an expensive imaging support system, the classic technique of PPS insertion using dual fluoroscopy units in the lumbar and sacral spine is fairly accurate and provides good clinical outcomes, even among surgeons lacking experience.
Keywords: accuracy, percutaneous pedicle screw, dual fluoroscopy units, radiation exposure, surgeon experience
Introduction
Minimally invasive surgery of the spine provides great benefits to patients. As spinal surgery techniques and instrumentation devices develop, the demand for minimally invasive spinal fixation (MISF) grows. MISF has many advantages, including less blood loss, shorter length of hospital stay, lower rates of infection, and better relief of postoperative pain than traditional open surgery.1 2 3 The percutaneous pedicle screw (PPS) system is a basic and essential device for posterior MISF. Published research has demonstrated highly accurate PPS placement with various imaging support systems, such as computer-assisted navigation.4 5 6 7 8 9 However, such navigation systems are exceedingly expensive, and only well-funded institutions can afford such specialized equipment. Recent publications have reported the safe and accurate placement of the PPS by surgeons with different levels of experience in human cadavers.10 However, the clinical results of patients with degenerative lumbar disease in different institutions and among surgeons are not well known.
Wiesner et al reported an accurate pedicle screw insertion technique using perfect anteroposterior (AP) and lateral radiograph image guidance.11 This classic and safe technique has been used widely by spine surgeons. According to a recent report,12 Wiesner's modified method with a guidewire and cannulated screw using dual conventional fluoroscopy units achieved good results for the screw placement without specialized equipment in trauma patients. We introduced MISF using the modified PPS insertion technique with dual fluoroscopy units in 2010. Dual imaging views of two planes can simply and easily show the entry point and screw trajectory to the surgeon. We hypothesized that even less-experienced surgeons could perform safe surgeries as described in a human cadaveric report,10 if they understood the correspondence between the anatomical landmarks of the spine and the intraoperative imaging views.
Published studies reported only the degree of the PPS placement accuracy, but not the comparative clinical results among surgeons. In addition, there have been few reports about accuracy enhancement of the PPS placement with dual fluoroscopy-based techniques for degenerative lumbar disease. The accuracy of the PPS placement and the differences in the results between experienced and less-experienced surgeons in spinal surgery for degenerative lumbar spine disease were evaluated.
Methods
This retrospective, comparative study investigated the accuracy of PPS placement and the radiation time per PPS insertion between two groups of patients who underwent surgery by surgeons with less than 5 years of experience versus surgeons with more than 5 years of experience in spinal surgery. An experienced surgeon was defined as a board-certified spine surgeon and a surgeon engaged in spine surgery for over 5 years. Less-experienced surgeons included orthopedic and neurosurgical residents and fellows. The study population was selected from consecutive patients who underwent MISF with the PPS system in Fukuoka Wajiro Hospital and Shinkomonji Hospital from April 2010 to October 2013. The study protocol was approved by the Ethics Committees of the two hospitals. All patients gave their written, informed consent for this study. Patients with degenerative lumbar disease were included; cases with pedicle diameter less than 5 mm were excluded. The inclusion criterion for surgeons in both groups was based on whether they had practiced the PPS method in more than five cases.
A total of 231 consecutive patients with degenerative lumbar disease were treated by MISF with the PPS system in the two hospitals. The 161 patients satisfying the inclusion criteria were divided into two groups: group A, 74 patients (40 male and 34 female patients; average age 63 years) who were treated by four surgeons with more than 5 years of experience in lumbar surgery, and group B, 87 patients (58 male and 29 female patients; average age 60 years) who were treated by four surgeons with up to 5 years of experience.
Table 1 shows the characteristics of the patients in the two groups. The lumbar degenerative diseases included 132 cases of lumbar canal stenosis diagnosed with reference to the international classification and 29 cases with lumbar disk herniation. The range of fixation was short segment in 156 cases, 2 segments in 3 cases, and 3 segments in 2 cases. The spinal implants used were the pedicle screw and rod systems (CD HORIZON SEXTANT, Medtronic Sofamor Danek Spine, Memphis, Tennessee, United States; and VIPER, DePuy Synthes Spine, Raynham, Massachusetts, United States). The diameters of the screws ranged from 5.2 to 6.5 mm and were chosen to be within the diameter of the pedicle based on preoperative computed tomography (CT).
Table 1. Patient characteristics.
| Group A (n = 74) | Group B (n = 87) | p Value | |
|---|---|---|---|
| Male/female | 40/34 | 58/29 | 0.102a |
| Mean age (y) | 63 | 60 | 0.187b |
| LDH (n = 29) | 12 | 17 | |
| Primary | 8 | 16 | 0.178a |
| Recurrence | 4 | 1 | 0.120a |
| LCS (n = 132) | 62 | 70 | |
| Combined | 11 | 13 | 0.988a |
| Listhesis | 24 | 23 | 0.404a |
| Scoliosis | 4 | 5 | 0.925a |
| Foraminal stenosis | 15 | 22 | 0.450a |
| Segmental instability | 0 | 1 | 0.354a |
| Facet cyst | 1 | 0 | 0.276a |
| Spondylolysis | 2 | 2 | 0.869a |
| ASD | 2 | 0 | 0.122a |
| DSA | 1 | 0 | 0.276a |
Abbreviations: ASD, adjacent segmental disease; DSA, destructive spondyloarthropathy; LCS, lumbar canal stenosis; LDH, lumbar disc herniation.
Chi-square test.
Mann-Whitney U test.
All operations were performed with the patient under general anesthesia. The patient was put on the Jackson table in the prone position. The lateral fluoroscopic radiographic unit was set up at the left side of the Jackson table, and the AP unit was set up at the opposite side. This setting of the dual fluoroscopy units allowed the surgeon to view biplane images at the same time. The C-arm that had the larger diameter was set as the AP view to allow a wider working space for the operation. First, decompression and interbody fusion surgery were performed at the affected level. Subsequently, the position of the two fluoroscopy units was adjusted for the perfect AP and lateral radiographs of the target vertebra on the monitor. The following setting of the fluoroscopy units is the most important preparation for inserting PPSs. The position of the C-arm should be fine-tuned in the craniocaudal direction to align the anterior end plate of the vertebra with the posterior end plate, and it must be turned around to allow visibility of the pedicle symmetrically toward the vertebral rotation angle on the perfect AP view. On the perfect lateral view, the shaded images of the two pedicles must correspond. After setting the two fluoroscopy units, the entry point and the insertion angle of the screws were determined with dual vision (Fig. 1). A Jamshidi needle was positioned at the base of the transverse process corresponding to the lateral margin of the oval pedicle image in the perfect AP view. When the tip of the needle reached the posterior wall of the vertebra in the perfect lateral view, it was checked to be within the medial margin of the pedicle in the AP view.11 A guidewire was inserted through the cannula, and the needle was removed. The back muscles were split by a muscle dilator, a cannulated tap was inserted to make a pedicular hole, and then cannulated screws were placed into the pedicle over the guidewire. Finally, segmental fixation was completed after insertion of the screws.
Fig. 1.
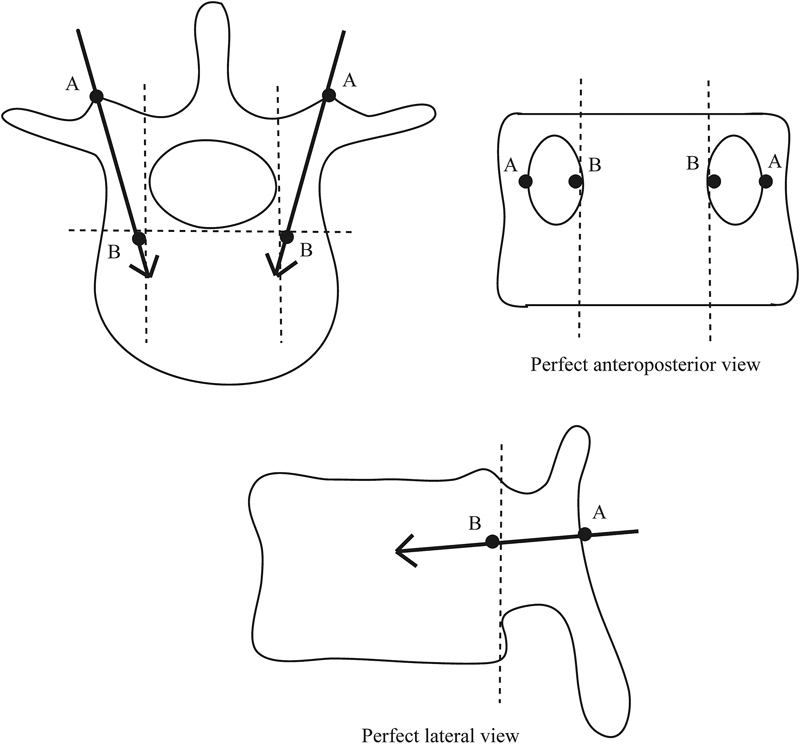
The classic technique of pedicle screw insertion using fluoroscopy. Point A is the needle insertion point, and the tip is located on the lateral margin of the pedicle on the perfect anteroposterior view. Point B shows that the tip of the needle has reached the vertebral body, and it should be within the medial margin of the pedicle on the anteroposterior view.
A CT scan was obtained to check the PPS placement 5 days after surgery. PPS misplacement was defined as breach of the pedicular wall with a grading scale of 2-mm steps (grade I: no breach; grade II: breach less than 2 mm; grade III: breach 2 to 4 mm; grade IV: breach 4 to 6 mm; grade V: breach greater than 6 mm), as described by Gertzbein and Robbins.13 The direction of pedicular wall breach in the transverse, sagittal, and coronal planes using 2-mm slice-thickness CT (Aquilion 64 TSX—101A and Aquilion ONE TSX—301A, TOSHIBA, Tokyo, Japan) was assessed by one radiologist and one spinal surgeon, and both were blinded to the patients' classification. If the CT scan interpretations disagreed, the higher grade was given priority over the lower grade. To evaluate radiation exposure, we measured the total radiation time (seconds) required for the PPS insertion in the series of operative procedures ranging from the setting of the Jamshidi needle to completion of screw insertion.
Values are shown as medians (range) for the radiation time and averages ± standard deviation for the surgical time. Statistical analyses were performed with the chi-square test for categorical data and the Mann-Whitney U test and Student t test for surgical results to compare the two groups. The differences with p < 0.05 were considered as significant.
Results
There were no significant differences in the characteristics of the patients between the two groups. A total of 658 screws were inserted in 161 patients from L2 to S1. Fig. 2 shows the distribution of the vertebral levels in which PPSs were placed and the grading of pedicular perforation.
Fig. 2.

The distribution of screw misplacement and the grading scale. Most screws are installed at L4 and L5. The highest ratio of screw deviation is seen at L2, and grade III perforations are seen only at L5 and S1.
Of the 658 screws, 637 were placed entirely in the pedicle, and only 21 screws (3.2%) were misplaced from L2 to S1. Nineteen screws (2.9%) perforated the cortex of the pedicle in grade II and 2 (0.3%) in grade III misplacement. The breach rate by lumbar level was 11% at L2, 1.9% at L3, 3.6% at L4, 2.1% at L5, and 4.5% at S1; the highest breach rate was at L2. The breach rates of groups A and B were 3.3% (10/306) and 3.1% (11/352), respectively, with no significant difference (p = 0.91). In group A, 10 screws were in grade II misplacement, with no screws in grade III misplacement. In group B, 9 screws were in grade II misplacement, and 2 screws were in grade III misplacement (Table 2). These misplacements occurred in the fourth and twelfth cases performed by different surgeons in group B.
Table 2. Comparative data of the two groups.
| Group A | Group B | p Value | |
|---|---|---|---|
| Total breach rate (%) | 3.3 | 3.1 | 0.91a |
| Grade II (%) | 3.4 | 2.6 | 0.58a |
| Grade III (%) | 0 | 0.6 | 0.18a |
| Radiation time (s) | 25 | 51 | <0.01b |
Chi-square test.
Mann-Whitney U test.
The direction of the pedicular breach was lateral in 12, medial in 4, superior in 3, and inferior wall in 2. Malposition screws of grade III misplacement had medial and inferior positions with respect to each other in group B. No significant differences were seen in the direction of perforation between the two groups (p = 0.18, Fig. 3).
Fig. 3.

The direction of pedicular breaches is shown for the two groups. Lateral breaches are the most common in the two groups. The numbers in parentheses in group B represent grade III misplacements.
Despite the malposition of screws, all patients in grade II misplacement had no neurologic symptoms. In grade III misplacements, one group B patient (medial wall breach) had a transient symptom of nerve root irritation. As other surgical complications, another case had a deep surgical site infection unilaterally. The median fluoroscopy time for the PPS insertion was 25 (5 to 92) seconds in group A and 51 (7 to 124) seconds in group B. The radiation exposure was significantly shorter in group A than in group B (p < 0.01, Table 2). The average operative time was 132 ± 49 minutes in group A and 164 ± 46 minutes in group B (p < 0.01).
Discussion
The present study shows that PPS placement was highly accurate with the classic technique under dual fluoroscopy-based guidance, even when the surgeon lacked sufficient experience.
The technique of PPS insertion in the lumbar spine was initially introduced by Magerl in 1977.14 He described the management of spinal trauma and spondylodiscitis as temporary external fixation. Wiesner et al reported a safe technique to insert transpedicular noncannulated screws percutaneously with fluoroscopic guidance using a human cadaver model in 1999.11 The authors also reported that the results with this technique were better than those of the well-established Magerl technique. The first clinical evaluation of the tracts and PPS positions with CT scan analysis was followed by the report of an in vivo study by the same authors.15 The accuracy of fluoroscopy with computer-guided technology was assessed using cadavers by Foley et al in 2001, and computer-assisted technology has been adopted since.9 The current percutaneous insertion technique using cannulated screws with a guidewire, first described by Holly and Foley,16 has become the fundamental technique for MISF.
Breach rates of 1.1 to 23% using a percutaneous procedure with two- or three-dimensional navigation systems have been reported.5 6 7 16 The published studies including scoliosis surgery emphasize the advantages of a higher accuracy in screw placement with a navigation-assisted technique than with the conventional fluoroscopy technique.6 8 17 However, the navigation systems are very expensive and require time-consuming preregistration of anatomical landmarks. Additional CT scans are required when going beyond the imaging area for the target vertebra even with zero-preregistration mobile-type CT navigation.8 18
On the other hand, breach rates of 7.2 to 14.8% using the same procedure as ours (Wiesner's modified technique) under the assistance of fluoroscopy alone and using a postoperative grading scale of 2-mm steps on CT have been reported.4 7 18 19 Heintel et al achieved a highly satisfactory breach rate of 2% for trauma patients using dual fluoroscopy-based technique.12 However, that study did not include screw misplacement with lateral wall perforation in those that were inserted medially. In the present study, the breach rate was 1.4% (9/658) except for the lateral perforation cases. If they had used the same grading scale of screw misplacement as in the present study, the breach rate should have been higher than the result they reported.
In the present study, screw placement was better using the dual fluoroscopy-based technique than in reports of the single fluoroscopy-based technique, because the rotating single C-arm could not reflect the three-dimensional trajectory of the needle in real time during the procedure of transpedicular needle insertion into the vertebra.
Taking biplane imaging views simultaneously by dual fluoroscopy units makes it possible to identify the precise entry point and the trajectory of the PPS in real time. In addition, the use of dual fluoroscopy units has the potential to reduce the incidence of surgical site infection by saving multiple troublesome and unclean steps of C-arm control.
The cause of the high rate of lateral wall breaches at L2 is likely related to the anatomical features of the lumbar spine. The pedicle width of the lumbar vertebrae increases gradually from L1 to L5.20 When the base of the transverse process is located more on the outside than usual due to hypertrophy of a degenerative facet, an increased risk of developing a lateral wall breach is seen because the entry point of the screw is located on the outside.5 Additionally, when there is a recess in the lateral pedicular wall, a lateral pedicular breach is unavoidable based on the anatomical features (Fig. 4). The above would suggest a high rate of lateral wall breach.
Fig. 4.

The computed tomography shows lateral breach of screw due to the hypertrophy of facet and the recess in the lateral pedicular wall.
No patients with grade II screw malposition had neurologic symptoms postoperatively. Screw deviation of less than 2 mm into the canal does not appear to cause adverse postoperative clinical results. In fact, the lumbar canal has a 4-mm epidural and subarachnoid space “safe zone,” and canal encroachment of the screw by less than 4 mm could be tolerated without neurologic symptoms.13
Wiesner et al reported that a major factor related to the higher misplacement rate of S1 screws with medial wall breach was the presence of the iliac crest in the vicinity.15 Ravi et al suggested that the direction of the medial or lateral breaches tended to depend on the location of the screw insertion point.5 Briefly, the medial start point due to the vicinity of the ilium resulted in a medial breach. Additionally, the AP view of the medial margin of the sacral pedicle is often poor compared with that of lumbar vertebrae. If the view is clear, a surgeon acquainted with the anatomy could anticipate the medial margin of the pedicle from the upper vertebra to some extent. The anatomical characteristics of the sacrum and a poor knowledge of anatomy resulted in the grade III screw malposition in group B.
Yang et al reported that the PPS insertion technique using the oblique visualization technique under computer-assisted fluoroscopic navigation reduced the fluoroscopy time per screw to an average of 6.6 seconds.6 With fluoroscopy guidance, Raley and Mobbs reported that of 88 cases, the first five and the last five required an average of 25.8 seconds and 6.6 seconds of fluoroscopy time per screw, respectively.19 The radiation exposure was greatly reduced by the use of computer navigation and the learning curve. A dual fluoroscopy technique similar to ours achieved a good result, with an average fluoroscopy time of 22.7 seconds per PPS and a screw breach rate of 3.3%.21 However, the surgeon had been specialized in MISF and was probably beyond the learning curve.
The present study median fluoroscopy time in group A of 25 seconds was similar to a previous report. In group B, the radiation exposure was about twice as long as in group A. The fact that the surgeons in group A were masters with knowledge of local anatomy compared with group B contributed to the lack of grade III breaches and less radiation exposure in group A. Whereas the dual fluoroscopy technique contributed to the high accuracy of screw placement on the axial plane and the optimal location of the screw top within the vertebra on lateral imaging,12 it had a disadvantage of requiring more radiation exposure.22 Without an expensive imaging support system, the technique of PPS insertion using dual fluoroscopy units is fairly accurate. However, the higher radiation exposure when using this technique compared with a navigation system is one important limitation. A larger sample size would probably have shown a significant difference between the two groups in grade III breaches.
The present study showed high accuracy of PPS placement by surgeons with a lack of experience, and experienced surgeons had shorter intraoperative radiation time. Although there was a lack of novelty, there were significant results from the perspective of a first report: the accuracy of the PPS placement for degenerative lumbar spine, not cadaveric spines, and the radiation exposure compared between surgeons with more versus less experience. An experience-dependent learning curve has the possibility of decreasing the absorbed doses of radiation. And less-experienced surgeons should insert the PPS under the technical guidance of a senior surgeon in the first 10 or more cases. The present technique using dual fluoroscopy units simultaneously resulted in favorable results achieved by the relatively less-experienced surgeons.
Conclusions
Favorable PPS placement was achieved using a conventional dual fluoroscopy-guided technique without depending on surgeon experience. The classic modified method of PPS insertion in the dual fluoroscopy technique has a risk of greater radiation exposure but provides accurate placement in any institution and by any surgeon.
Footnotes
Disclosures Masayuki Nakahara, none Takao Yasuhara, none Takafumi Inoue, none Yuichi Takahashi, none Shinji Kumamoto, none Yasukazu Hijikata, none Akira Kusumegi, none Yushi Sakamoto, none Koichi Ogawa, none Kenki Nishida, none
References
- 1.Grass R, Biewener A, Dickopf A, Rammelt S, Heineck J, Zwipp H. [Percutaneous dorsal versus open instrumentation for fractures of the thoracolumbar border. A comparative, prospective study] Unfallchirurg. 2006;109(4):297–305. doi: 10.1007/s00113-005-1037-6. [DOI] [PubMed] [Google Scholar]
- 2.Kim D Y, Lee S H, Chung S K, Lee H Y. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 2005;30(1):123–129. [PubMed] [Google Scholar]
- 3.Isaacs R E Hyde J Goodrich J A Rodgers W B Phillips F M A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications Spine (Phila Pa 1976) 201035(26, Suppl):S322–S330. [DOI] [PubMed] [Google Scholar]
- 4.Schwarzenbach O, Berlemann U, Jost B. et al. Accuracy of computer-assisted pedicle screw placement. An in vivo computed tomography analysis. Spine (Phila Pa 1976) 1997;22(4):452–458. doi: 10.1097/00007632-199702150-00020. [DOI] [PubMed] [Google Scholar]
- 5.Ravi B, Zahrai A, Rampersaud R. Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine (Phila Pa 1976) 2011;36(1):84–91. doi: 10.1097/BRS.0b013e3181cbfd09. [DOI] [PubMed] [Google Scholar]
- 6.Yang B P, Wahl M M, Idler C S. Percutaneous lumbar pedicle screw placement aided by computer-assisted fluoroscopy-based navigation: perioperative results of a prospective, comparative, multicenter study. Spine (Phila Pa 1976) 2012;37(24):2055–2060. doi: 10.1097/BRS.0b013e31825c05cd. [DOI] [PubMed] [Google Scholar]
- 7.Villavicencio A T, Burneikiene S, Bulsara K R, Thramann J J. Utility of computerized isocentric fluoroscopy for minimally invasive spinal surgical techniques. J Spinal Disord Tech. 2005;18(4):369–375. doi: 10.1097/01.bsd.0000168511.67189.64. [DOI] [PubMed] [Google Scholar]
- 8.Nakashima H, Sato K, Ando T, Inoh H, Nakamura H. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. J Spinal Disord Tech. 2009;22(7):468–472. doi: 10.1097/BSD.0b013e31819877c8. [DOI] [PubMed] [Google Scholar]
- 9.Foley K T, Simon D A, Rampersaud Y R. Virtual fluoroscopy: computer-assisted fluoroscopic navigation. Spine (Phila Pa 1976) 2001;26(4):347–351. doi: 10.1097/00007632-200102150-00009. [DOI] [PubMed] [Google Scholar]
- 10.Baird E O McAnany S J Overley S Skovrlj B Guzman J Z Qureshi S A Accuracy of percutaneous pedicle screw placement: does training level matter? J Spinal Disord Tech 2015; April 3 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 11.Wiesner L, Kothe R, Rüther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 1999;24(15):1599–1603. doi: 10.1097/00007632-199908010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Heintel T M, Berglehner A, Meffert R. Accuracy of percutaneous pedicle screws for thoracic and lumbar spine fractures: a prospective trial. Eur Spine J. 2013;22(3):495–502. doi: 10.1007/s00586-012-2476-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gertzbein S D, Robbins S E. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15(1):11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Magerl F P. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;(189):125–141. [PubMed] [Google Scholar]
- 15.Wiesner L, Kothe R, Schulitz K P, Rüther W. Clinical evaluation and computed tomography scan analysis of screw tracts after percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 2000;25(5):615–621. doi: 10.1097/00007632-200003010-00013. [DOI] [PubMed] [Google Scholar]
- 16.Holly L T Foley K T Three-dimensional fluoroscopy-guided percutaneous thoracolumbar pedicle screw placement. Technical note J Neurosurg 200399(3, Suppl):324–329. [DOI] [PubMed] [Google Scholar]
- 17.Kotani Y, Abumi K, Ito M. et al. Accuracy analysis of pedicle screw placement in posterior scoliosis surgery: comparison between conventional fluoroscopic and computer-assisted technique. Spine (Phila Pa 1976) 2007;32(14):1543–1550. doi: 10.1097/BRS.0b013e318068661e. [DOI] [PubMed] [Google Scholar]
- 18.Gu G Zhang H He S et al. Percutaneous pedicle screw placement in lumbar spine: a comparison study between the novel guidance system and the conventional fluoroscopy method J Spinal Disord Tech 2013; September 27 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 19.Raley D A, Mobbs R J. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: accuracy and complication rates. Spine (Phila Pa 1976) 2012;37(12):1092–1100. doi: 10.1097/BRS.0b013e31823c80d8. [DOI] [PubMed] [Google Scholar]
- 20.Lien S B, Liou N H, Wu S S. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16(8):1215–1222. doi: 10.1007/s00586-006-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitz S M, Sandhu F A, Voyadzis J M. Percutaneous “K-wireless” pedicle screw fixation technique: an evaluation of the initial experience of 100 screws with assessment of accuracy, radiation exposure, and procedure time. J Neurosurg Spine. 2015;22(4):422–431. doi: 10.3171/2014.11.SPINE14181. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad F U, Wang M Y. Use of anteroposterior view fluoroscopy for targeting percutaneous pedicle screws in cases of spinal deformity with axial rotation. J Neurosurg Spine. 2014;21(5):826–832. doi: 10.3171/2014.7.SPINE13846. [DOI] [PubMed] [Google Scholar]


