Abstract
Purpose
To determine the association between injury history at enrollment and incident lower extremity (LE) injury during cadet basic training among first-year military cadets.
Methods
Medically treated LE injuries during cadet basic training documented in the Defense Medical Surveillance System (DMSS) were ascertained in a prospective cohort study of three large U.S. military academies from 2005–2008. Both acute injuries (ICD-9 codes in the 800–900s, including fracture, dislocations, sprains/strains) and injury-related musculoskeletal injuries (ICD-9 codes in the 700s, including inflammation and pain, joint derangement, stress fracture, sprain/strain/rupture, and dislocation) were included. Risk ratios (RR) and 95% confidence intervals (CI) were computed using multivariate log-binomial models stratified by gender.
Results
During basic training there were 1,438 medically treated acute and 1,719 musculoskeletal-related LE injuries in the 9,811 cadets. The most frequent LE injuries were sprains/strains (73.6% of acute) and inflammation and pain (89.6% of musculoskeletal-related). The overall risk of incident LE injury was 23.2% [95%CI: 22.3%, 24.0%]. Cadets with a previous history of LE injury were at increased risk for incident LE injury. This association was identical in males (RR=1.74 [1.55, 1.94]) and females (RR=1.74 [1.52, 1.99]). In site-specific analyses, strong associations between injury history and incident injury were observed for hip, knee ligament, stress fracture, and ankle sprain. Injury risk was greater (p<0.01) for females (39.1%) compared to males (18.0%). The elevated injury risk in females (RR=2.19 [2.04, 2.36]) was independent of injury history (adjusted RR=2.09 [1.95, 2.24]).
Conclusion
Injury history upon entry to the military is associated with incidence of LE injuries sustained during cadet basic training. Prevention programs targeted at modifiable factors in cadets with a prior history of LE injury should be considered.
Keywords: epidemiology, lower extremity, ankle, knee, risk factors
INTRODUCTION
Non-fatal injuries are the leading cause of medical encounters in the armed services and were responsible for 1.14 million outpatient visits in 2006 (13). All four major branches of the U.S. military (Army, Navy, Marine, and Air Force) have identified physical training as a major priority for prevention efforts (27). Given the nature of military, which involves substantial stress to the lower extremity during marching, running, and jumping, it is not surprising that lower extremity injuries continue to be the most common injuries in military training, specifically overuse and sprains and strains (9, 13). Public health approaches to injury prevention include determining the incidence of injuries, identifying modifiable and non-modifiable risk factors, developing and testing prevention strategies in ideal conditions, and determining real-world effectiveness of the prevention strategies (30). Targeted injury prevention efforts have shown potential to reduce the incidence of lower extremity injuries (6); however, lower extremity injuries remain a major concern.
Upon entry into the military, all personnel undergo a rigorous basic training program generally lasting 6–8 weeks. During this period activities are standardized and, for the most part, personnel perform similar activities regardless of age or gender. Previous studies of military service members have identified several risk factors associated with lower extremity injury during basic training including: baseline fitness levels (12, 16), higher body mass index (BMI), and shorter stature (12). Investigations focused on military cadets found similar differences in injury risk among males and females for baseline fitness levels and higher BMI (4, 5). Numerous studies have noted that females experience higher rates of injury than males during basic training (3–5, 12, 16, 28). However, this finding may reflect the gender differences of other risk factors, such as baseline physical fitness, BMI, and physical stature (3), possibly in combination with gender differences in health care seeking behavior (1, 10).
In military and athlete populations, injury history is a strong and consistent predictor of incident injury (7, 8, 15). The reasons for this association remain unclear, but it is likely due to multiple factors. These may include anatomic, structural, or genetic predisposition to injury; failure to rehabilitate prior injuries adequately; alterations in movement patterns; pressure to return to duty/competition; and psychometric factors such as risk-taking behavior, psychophysics of perceived pain, and care-seeking. Basic training in the military provides an ideal setting for examining the association between injury history and incident injury, since it involves large numbers of men and women from diverse backgrounds performing demanding physical duties that are standardized and uniform. Gender differences have been documented in military training injury rates (11), however it remains unclear whether these differences simply reflect gender differences in factors such as physical condition or injury history (3). Additionally, characterizing the baseline injury profile for military cadets during the high-stress period of basic training has the potential to provide useful information for targeted prevention efforts and programs, such as exercise-based movement training programs, particularly if modifiable risk factors can be identified (16) and targeted (24).
The purpose of this study was to describe the role of injury history as a baseline risk factor for incident lower extremity (LE) injury and musculoskeletal-related conditions during the 8 week basic training period among first-year military cadets at three military service academies during 2005 to 2008. The population of interest for this analysis included first year cadets from the three largest military academies. A priori, it was hypothesized that: 1) females would be at higher risk, 2) those with a history of prior injury would be at higher risk, and 3) that some of the gender differences would be due to differences in injury history between males and females.
METHODS
Study Design and Population
Data for this secondary analysis come from the parent study, JUMP-ACL (Joint Undertaking to Monitor and Prevent ACL Injury). JUMP-ACL was a collaborative multi-site prospective cohort study of neuromuscular risk factors for anterior cruciate ligament (ACL) injury. The study was based in the 3 largest U.S. military academies: U.S. Military Academy (USMA) in West Point, NY; U.S. Naval Academy (USNA) in Annapolis, MD; and U.S. Air Force Academy (USAFA) in Colorado Springs, CO. The study was jointly coordinated by The University of North Carolina at Chapel Hill (UNC-CH) and The Uniformed Services University of the Health Sciences. All study procedures were approved by the UNC-CH Institutional Review Board and the Institutional Review Boards overseeing the three academies.
For each military academy, cadets or midshipmen arrive in July of each year to begin their 4-year officer training. The JUMP-ACL study included a total of four classes for each of the three military academies over the 2005–2008 time period. A total of 9,811 cadets who volunteered, completed informed consent, and completed the baseline questionnaire were included in this study. On average over the 4 years, 87% of females (79% USAFA, 100% USMA, 83% USNA) and 58% of the males (51% USAFA, 87% USMA, 31% USNA) completed the baseline survey.
Baseline covariates
Cadets filled out a baseline questionnaire that included information about personal characteristics such as their age; whether they attended the preparatory academy; participation in plyometric or ACL injury prevention programs; participation in high school sports; distance running index; and LE injury history. Self-reported prior injuries to the lower extremity in the past 6 months included: ankle sprains, shin splints (medial tibial stress syndrome), lower leg stress fracture, lower leg bone fracture, knee ligament injury, patellofemoral pain, hip injury, and other lower extremity injury. Positive history of any of these injuries were categorized as “any lower extremity injury”. Positive history of an ankle sprain, shin splints, lower leg fracture or stress fracture were categorized as “any lower leg injury”. The combined effects of multiple prior LE injuries were examined for the knee and ankle. Combinations of prior LE injuries at baseline were categorized into four levels as follows: no injury history at any LE site (referent category); no injury history at same site but prior injury at other LE body site; prior injury only at same site; and prior injury at same site and other LE body site. The above prior injuries limited to those injuries that currently interfered with physical activity were also examined.
Injury events during cadet basic training
Incident lower extremity injuries were ascertained via the Defense Medical Surveillance System (DMSS) (26). The DMSS records all clinic visits of a medical nature. All injuries reported to the DMSSS during the cadet basic training period (July 1- August 31) were included. Relevant injuries to study participants during their enrollment at the academy were identified by International Classification of Disease (ICD-9) diagnosis codes. Data were provided to researchers free of personal identifiers and assigned a unique identifier for linkage with JUMP-ACL study population. Injury type categories for the injuries of the lower extremity were determined by groupings of ICD-9 codes. Acute injuries (ICD-9 diagnosis code in the 800–900s) were identified using the Barell injury diagnosis matrix (2). The Barell injury diagnosis matrix was developed by an international team of researchers as a way of summarizing medically-treated injuries in a standardized manner to enable comparisons across different populations and countries. This method was applied by researchers in surveillance of medically-treated injuries of military populations (13). Recognizing that acute injuries fail to represent comprehensively the injury experience for military personnel, injury-related musculoskeletal conditions (ICD-9 diagnosis code in the 700s) were also identified by expanding the Barell injury diagnosis matrix methodology through a review of the sports medicine literature to determine common injury-related musculoskeletal conditions (9). All acute and musculoskeletal-condition injury diagnoses were grouped by body part: hip; upper leg and thigh; knee; lower leg and ankle; foot and toes; and other or unspecified lower extremity. Acute injury type categories for the current analysis included: fracture, dislocation, and sprain/strain. Injury-related musculoskeletal conditions included: inflammation and pain (overuse); joint derangement; stress fracture; sprain/strain/rupture; and dislocation (see Table, Supplemental Digital Content 1, for ICD-9 codes by category).
Both primary and non-primary diagnosis codes were utilized. In order to minimize duplicate counting from multiple health care encounters per event, encounters for the same three-digit diagnosis code within 60 days of the first encounter were excluded. This method has been utilized in previous injury surveillance studies (9, 13). Note that using 3-digit diagnosis codes is unduly conservative as some diagnosis codes have 4th and 5th digits that identify different body part locations. For example ICD-9 diagnosis code 719 describes an overuse unspecified joint disorder, but the 4th digit determines the body part involved (i.e. ankle/foot, knee, or hip). Using 3-digit codes, the first coded encounter would be taken and subsequent encounters for other body parts would be excluded.
Data analysis
Descriptive frequencies and univariate statistics were calculated overall and by gender for cadet demographics, baseline injury history, and characteristics of incident medically-treated injuries during cadet basic training (July 1 to August 31). Incident medically-treated acute and musculoskeletal-condition injuries were combined by body part and dichotomized for analyses (e.g., incident ankle injury during basic training versus none). Statistical differences in demographic, injury history, and incident injury between males and females were determined with chi-square tests and a priori p-value <0.05. Risk ratios (RR) and 95% confidence intervals (95% CI) were calculated with multivariate general log-binomial regression models stratified by gender to examine the association between previous LE injury history and incident LE injury adjusted for the following variables: age; academy; cohort year; prep academy attendance; participation in prior injury prevention programs; participation in high school sports; and distance running index. Separate models were created for injuries to the following grouped body areas: any lower extremity injury, hip, knee ligament, lower leg, lower extremity stress fracture, and ankle sprain.
Variables associated with injury identified in previous studies (3–5, 12, 16) were initially included in multivariate models as were predictors identified in univariate analyses with a risk ratio of either 1.20 or greater or 0.80 or less. Academy and cohort year were included as adjustment variables (RRs are not reported). There were missing values for: age (n=146); prep academy attendance (n=55); participation in injury prevention programs (n=69); and running index (n=10) and multivariate models included only cadets with non-missing values (n=9,552).
RESULTS
Study participants were predominantly male (75.3%) and less than 21 years of age (97%, mean 18.8, SD=0.97, range 16–23) (Table 1), which is reflective of the enrollment at the service academies. Most entering cadets did not attend the military prep academy (81.9%), did not participate in a prior plyometric or ACL injury prevention program (67.8%), and played three or more high school sports (66.9%). Female cadets were more likely to be 18 or younger compared to male cadets (56.2% versus 43.7%, X2=120.7622 p<0.0001). No other meaningful demographic differences were observed by gender.
Table 1.
Demographic Characteristics of First-year Male and Female Military Cadets who Completed the Baseline JUMP-ACL Questionnaire, 2005–2008
| Males | Females | Total | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Distance running index | n | % | n | % | n | % |
| 2005 | 1558 | 21.1 | 548 | 22.6 | 2106 | 21.5 |
| 2006 | 1870 | 25.3 | 627 | 25.9 | 2497 | 25.5 |
| 2007 | 2046 | 27.7 | 660 | 27.3 | 2706 | 27.6 |
| 2008 | 1916 | 25.9 | 586 | 24.2 | 2502 | 25.5 |
| Academy1 | ||||||
| USAFA | 2175 | 29.4 | 879 | 36.3 | 3054 | 31.1 |
| USMA | 3981 | 53.9 | 758 | 31.3 | 4739 | 48.3 |
| USNA | 1234 | 16.7 | 784 | 32.4 | 2018 | 20.6 |
| Age at study entry (years)1 | ||||||
| 16 to 18 | 3182 | 43.1 | 1342 | 55.4 | 4524 | 46.1 |
| 19 to 21 | 3844 | 52.0 | 1006 | 41.6 | 4850 | 49.4 |
| 22+ | 252 | 3.4 | 39 | 1.6 | 291 | 3.0 |
| Missing | 112 | 1.5 | 34 | 1.4 | 146 | 1.5 |
| Preparatory academy attendance | ||||||
| No | 5988 | 81.0 | 1998 | 82.5 | 7986 | 81.4 |
| Yes | 1356 | 18.3 | 414 | 17.1 | 1770 | 18.0 |
| Missing | 46 | 0.6 | 9 | 0.4 | 55 | 0.6 |
|
| ||||||
| Prior participation in an injury prevention program1 | n | % | n | % | n | % |
| None | 5017 | 67.9 | 1586 | 65.5 | 6603 | 67.3 |
| Plyometric program | 2269 | 30.7 | 782 | 32.3 | 3051 | 31.1 |
| ACL prevention program | 151 | 2.0 | 93 | 3.8 | 244 | 2.5 |
| Missing | 48 | 0.6 | 21 | 0.9 | 69 | 0.7 |
| Number of high school sports played | ||||||
| 0 to 2 sports | 2437 | 33.0 | 807 | 33.3 | 3244 | 33.1 |
| 3 or more sports | 4953 | 67.0 | 1614 | 66.7 | 6567 | 66.9 |
| Distance running index1 | ||||||
| 0 to 50th percentile | 3762 | 50.9 | 1140 | 47.1 | 4902 | 50.0 |
| 51 to 100th percentile | 3619 | 49.0 | 1280 | 52.9 | 4899 | 49.9 |
| Missing | 9 | 0.1 | 1 | 0.0 | 10 | 0.1 |
| Injury history previous 6 months | ||||||
| Lower extremity injury1,2 | 4504 | 61.0 | 1716 | 70.9 | 6220 | 63.4 |
| Hip injury1 | 145 | 2.0 | 92 | 3.8 | 237 | 2.4 |
| Severe knee pain1 | 2343 | 31.7 | 957 | 39.5 | 3300 | 33.6 |
| Other leg injury1 | 390 | 5.3 | 161 | 6.7 | 551 | 5.6 |
| Lower leg injury1,3 | 3104 | 42.0 | 1218 | 50.3 | 4324 | 44.1 |
| Stress fracture1 | 148 | 2.0 | 99 | 4.1 | 247 | 2.5 |
| Bone fracture | 45 | 0.61 | 11 | 0.45 | 56 | 0.6 |
| Shin splints1 | 2307 | 31.22 | 969 | 40.02 | 3276 | 33.4 |
| Ankle sprain | 1145 | 15.5 | 385 | 15.9 | 1524 | 15.5 |
| Injury history previous 6 months interrupting physical activity | ||||||
| Lower extremity injury1,2 | 719 | 9.7 | 452 | 18.67 | 1171 | 11.9 |
| Hip injury1 | 35 | 0.5 | 33 | 1.4 | 68 | 0.7 |
| Severe knee pain1 | 168 | 2.3 | 109 | 4.5 | 277 | 2.8 |
| Knee ligament | 59 | 0.8 | 26 | 1.1 | 85 | 0.9 |
| Other leg injury1 | 57 | 0.8 | 47 | 1.9 | 104 | 1.1 |
| Lower leg injury1,3 | 429 | 5.8 | 261 | 10.8 | 690 | 7.0 |
| Stress fracture1 | 19 | 0.3 | 24 | 1.0 | 43 | 0.4 |
| Bone fracture | 5 | 0.07 | 3 | 0.12 | 8 | 0.08 |
| Shin splints1 | 316 | 4.3 | 186 | 7.7 | 502 | 5.1 |
| Ankle sprain | 124 | 1.7 | 63 | 2.6 | 187 | 1.9 |
| TOTAL CADETS | 7390 | 75.3 | 2421 | 24.7 | 9811 | 100.0 |
Statistically significant Chi-square p-value <0.05
Lower extremity injury includes history of any of the injuries listed.
Lower leg injury includes history of ankle sprain, lower leg stress fracture, lower leg bone fracture, and shin splints.
Within the 6 months prior to academy entry, 63.4% of first year cadets reported a history of injury to the lower extremity and 44.1% to the lower leg (Table 1); 11.9% and 7.0% reported that the injury currently interfered with physical activity, respectively. Shin splints (33.4%), severe knee pain (33.6%), and ankle sprains (15.5%) were the most frequently reported specific prior injuries and conditions at baseline. Females were more likely than males to have a positive history for many types of LE injury, including severe knee pain (39.5% vs. 31.7%) and shin splints (40.1% vs. 31.2%).
During cadet basic training (July and August) there were a total of 3,157 medically treated LE injuries (Table 2): 45.5% were acute and 54.5% musculoskeletal-related conditions. The most frequent types of acute LE injuries were ankle and lower leg sprains/strains (38.7%) and unspecified LE sprains/strains (34.9%). Inflammation and pain was the most frequent type of LE musculoskeletal condition (89.6%).
Table 2.
Number and Percent of Incident Medically Treated Acute and Musculoskeletal Lower Extremity Injuries among First-year Military Cadets during Basic Training (July 1 – August 31), 2005–2008
| (a) Acute Injury (ICD-9 code 800–900 range) |
Fracture n (%) |
Dislocation n (%) |
Sprain/strain n (%) |
– | – | Total n (%) |
|---|---|---|---|---|---|---|
| Hip | 3 (0.2) | 0 (0.0) | 175 (12.2) | – | – | 178 (12.4) |
| Upper leg/thigh | 6 (0.4) | 0 (0.0) | 0 (0.0) | – | – | 6 (0.4) |
| Knee | 0 (0.0) | 29 (2.0) | 55 (3.8) | – | – | 84 (5.8) |
| Lower leg/ankle | 24 (1.7) | 1 (0.1) | 556 (38.7) | – | – | 581 (40.4) |
| Foot/toes | 26 (1.8) | 2 (0.1) | 58 (4.0) | – | – | 86 (6.0) |
| Other/unspecified lower extremity | 1 (0.1) | 0 (0.0) | 502 (34.9) | – | – | 503 (35.0) |
| Total | 60 (4.2) | 32 (2.2) | 1346 (93.6) | – | – | 1438 (100.0) |
|
| ||||||
| (b) Musculoskeletal Condition (ICD-9 code 700 range) |
Stress fracture n (%) |
Dislocation n (%) |
Sprain/strain/rupture n (%) |
Inflammation/pain (overuse)
n (%) |
Joint derangement n (%) |
Total n (%) |
|
| ||||||
| Hip/thigh | 0 (0.0) | 0 (0.0) | 1 (0.1) | 143 (8.3) | 0 (0.0) | 144 (8.4) |
| Knee | 0 (0.0) | 3 (0.2) | 34 (2.0) | 261 (15.2) | 20 (1.2) | 318 (18.5) |
| Lower leg | 54 (3.1) | 0 (0.0) | 0 (0.0) | 730 (42.5) | 0 (0.0) | 784 (45.6) |
| Ankle | 0 (0.0) | 1 (0.1) | 0 (0.0) | 312 (18.2) | 1 (0.1) | 314 (18.3) |
| Ankle/foot | 53 (3.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 12 (0.7) | 65 (3.8) |
| Foot/toes | 0 (0.0) | 0 (0.0) | 0 (0.0) | 94 (5.5) | 0 (0.0) | 94 (5.5) |
| Total | 107 (6.2) | 4 (0.2) | 35 (2.0) | 1540 (89.6) | 33 (1.9) | 1719 (100.0) |
See Supplemental Digital Content 1 Table for ICD-9 codes from Barell Matrix and Hauret et al. 2010.
Injury history as a risk factor
Cadets with a previous history of LE injury were at increased risk for a medically treated LE injury during cadet basic training (adjusted overall RR=1.72, 95% CI: 1.58, 1.88). This effect was very similar in males and females (RR of 1.74 for both), and persisted after adjusting for age, preparatory academy attendance, high school sport participation, distance running index, injury prevention program participation, academy, and cohort year (Table 3). Male cadets over 19 years of age and female cadets who attended prep academy were at increased risk of LE injury (Table 3). For both genders, playing three or more high school sports and higher distance running index were associated with lower risk of LE injury (RRs of 0.89 and 0.97 for males and females, respectively). Prior participation in injury prevention programs was not associated with LE injury risk for either gender.
Table 3.
Adjusted Risk Ratios of Incident Medically Treated Lower Extremity Injury among First-year Male (n=7187) and Female (n=2357) Military Cadets during Basic Training (July 1 – August 31), 2005–2008.
| Males | Females | |
|---|---|---|
| RR (95% CI)1 |
RR (95% CI) 1 |
|
| History of LE injury last 6 months | ||
| No | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.74 (1.55, 1.94) | 1.74 (1.52, 1.99) |
| Age | ||
| <=19 years | 1.00 (ref) | 1.00 (ref) |
| >19 | 1.29 (1.13, 1.48) | 0.89 (0.74, 1.05) |
| Attended preparatory academy | ||
| No | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.03 (0.90, 1.17) | 1.25 (1.11, 1.41) |
| Number of high school sports | ||
| Played 0 to 2 sports | 1.00 (ref) | 1.00 (ref) |
| Played 3 or more sports | 0.89 (0.81, 0.99) | 0.87 (0.79, 0.96) |
| Distance Running Index | ||
| 0 to 50th percentile | 1.00 (ref) | 1.00 (ref) |
| 51 to 100th percentile | 0.77 (0.69, 0.85) | 0.88 (0.80, 0.97) |
| Prior injury prevention program participation | ||
| No | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.06 (0.96, 1.17) | 0.93 (0.84, 1.03) |
Models adjusted for all variables in the table and cohort year and military academy; models exclude 267 cadets with missing values for age, gender, high school sports, distance index, and preparatory academy attendance.
In site-specific analyses, strong associations (RRs above 3.0 for males and females) were observed between specific injury history and an incident injury of the same type, including hip injury, knee ligament injury, ankle sprain, and stress fractures (Table 4). When restricting the injury history to injuries that interrupted physical activity, the associations were at least maintained, and many became stronger. The combined effects of multiple prior LE injuries were examined for the knee and ankle, the two sites which had the greatest number of cases (Table 5). These analyses indicated that the association was specific to the body site (knee or ankle) examined, among females and males. For example, a history of knee and other LE injury was associated with incident knee injury, but a history of LE injury without knee injury was not associated with incident knee injury. The same effect was observed for ankle injury, among both males and females. Among females, history of ankle injury with or without LE injury history was associated with incident ankle injury.
Table 4.
Adjusted Risk Ratios (95% Confidence intervals) for Site-specific Associations between Injury History and Incident Medically Treated Lower Extremity Injury among First-year Male (n=7187) and Female (n=2357) Military Cadets during Basic Training (July 1 – August 31), 2005–2008.
| Males | Females | |||
|---|---|---|---|---|
| Any history of injury to that site | History of injury to that site with activity limitation | Any history of injury to that site | History of injury to that site with activity limitation | |
| Lower extremity1 | ||||
| No LE injury history | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Prior LE injury | 1.74 (1.55, 1.94) | 2.11 (1.89, 2.35) | 1.74 (1.52, 1.99) | 1.57 (1.44, 1.71) |
| Hip3 | ||||
| No hip injury history | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Prior hip injury | 4.92 (2.85, 8.50) | 8.74 (4.16, 18.37) | 7.26 (5.12, 10.30) | 10.94 (7.54, 15.86) |
| Knee2 | ||||
| No prior knee ligament injury | – | 1.00 (ref.) | – | 1.00 (ref.) |
| Prior knee ligament injury previous 6 months | – | 4.59 (2.38, 8.83) | – | 5.91 (3.40, 10.28) |
| Lower leg1 | ||||
| No lower leg injury | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Prior lower leg injury | 1.68 (1.50, 1.88) | 2.18 (1.87, 2.54) | 1.54 (1.37, 1.74) | 1.79 (1.57, 2.03) |
| Stress fracture to lower leg2 | ||||
| No stress fracture history | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Prior stress fracture | 3.58 (1.13, 11.34) | 17.03 (4.73, 61.29) | 6.06 (3.02, 12.14) | 9.68 3.91 23.95) |
| Ankle sprain2 | ||||
| No ankle sprain injury history | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Prior ankle sprain injury | 3.40 (2.72, 4.26) | 4.78 (3.25, 7.02) | 3.53 (2.79, 4.48) | 5.39 (4.05, 7.17) |
Note: Separate models created for each body area where no history of prior injury to that area (none) was the referent category; Excludes 267 cadets with missing values for age, gender, preparatory academy attendance, and high school sports.
Adjusted for age, preparatory academy attendance, military academy, cohort year, injury prevention program participation, number of high school sports, and distance running index;
Adjusted for age, injury prevention program participation, number of high school sports, and distance running index;
Adjusted for injury prevention program participation and distance running index.
Table 5.
Adjusted Risk Ratios for Incident Medically Treated Knee or Ankle Injury Associated with Different Combinations of Prior Injury Sites among First-year Male (n= 7187) and Female (n=2357) Military Cadets during Basic Training (July 1 – August 31), 2005–2008.
| Males | Females | |||
|---|---|---|---|---|
| n (%) injured with positive history | Adjusted RR for incident injury to that body site (95% CI) | n (%) injured with positive history | Adjusted RR for incident injury to that body site (95% CI) | |
| Knee | ||||
| No injury history at any LE body site | 40 (18.3) | 1.00 (ref.) | 17 (12.3) | 1.00 (ref.) |
| No injury history at knee, prior injury at other LE injury | 30 (13.7) | 1.00 (0.63, 1.61) | 19 (13.8) | 0.96 (0.50, 1.83) |
| Prior injury at knee only | 69 (31.5) | 3.58 (2.44, 5.25) | 49 (35.5) | 4.09 (2.39, 7.00) |
| Prior injury at knee and other LE body site | 80 (36.5) | 3.75 (2.57, 5.47) | 53 (38.4) | 3.00 (1.75, 5.15) |
| Total | 219 (100) | 138 (100) | ||
| Ankle | ||||
| No injury history at any LE body site | 117 (26.4) | 1.00 (ref.) | 56 (16.2) | 1.00 (ref.) |
| No injury history at ankle, prior injury at other LE injury | 176 (39.6) | 1.20 (0.95, 1.51) | 171 (49.6) | 1.43 (1.07, 1.91) |
| Prior injury only at ankle only | 46 (10.4) | 2.80 (2.02, 3.87) | 29 (8.4) | 2.83 (1.89, 4.23) |
| Prior injury at ankle and other LE body site | 105 (23.7) | 3.33 (2.58, 4.29) | 89 (25.8) | 3.98 (2.94, 5.40) |
| Total | 444 (100) | 345 (100) | ||
Separate models for knee and ankle, both models adjusted for age, preparatory academy attendance, injury prevention program participation, number of high school sports, and distance running index.
LE=lower extremity
Gender
Collectively for acute and musculoskeletal-related injuries, the overall risk of incident medically treated LE injury during the cadet basic training period (approximately 8 weeks) was 23.2% (95% CI: 22.3%, 24.0%) (Figure 1). Risk was greater for females (39.1%) compared to males (18.0%) for all LE injuries (RR=2.19 95% CI: [2.05, 2.36], X2=456.1577, p<0.0001) and specific LE injuries (Figure 1). Noting that a prior history of LE injury (Table 1) was more prevalent in females (70.9%) than males (61.0%), it was hypothesized that some of the gender effect was due to injury history. However, the elevated injury risk in females (RR=2.19 [2.04, 2.36]) persisted after controlling for injury history (adjusted RR=2.09 [1.95, 2.24]), and remained largely undiminished (adjusted RR=1.79 [1.67, 1.92]), even after controlling for injury history, age, preparatory academy attendance, high school sport participation, distance running index, injury prevention program participation, academy, and cohort year.
FIGURE 1. Risk of Incident Medically Treated Lower Extremity Injuries during Cadet Basic Training (July 1 – August 31) among First-year Military Cadets, 2005–2008.
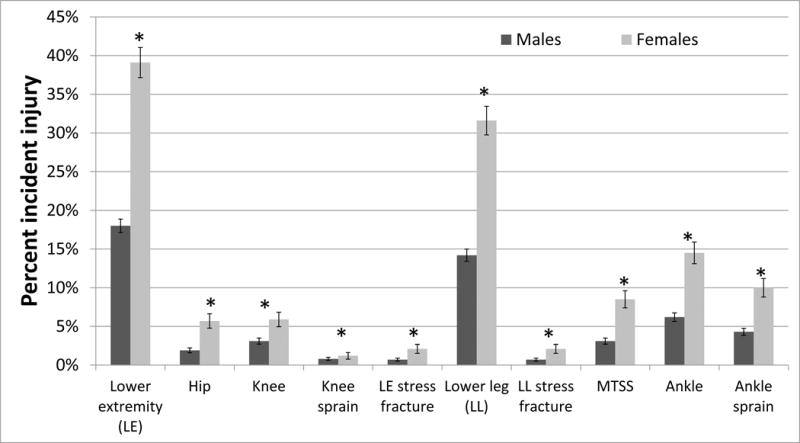
*Statistically significant Chi-square p-value <0.05
Note: Error bars represent 95% confidence intervals surrounding the risk proportions; MTSS, Medial tibial stress syndrome.
DISCUSSION
The purpose of this study was to determine the association between history of previous injury in relation to incident LE injury during cadet basic training. Previous history of prior LE injury was associated with incident lower extremity injury during cadet basic training. The association between injury history and incident LE injury was identical for males and females. The association between injury history and incident injury strengthened (RRs ranging from 3.0 to 11.0) in injury-specific analyses, in which injury history and incident injury were mutually limited to specific types of different LE injuries including hip injury, knee ligament injury, ankle sprain, and stress fractures. Previous studies in civilian athletic/active populations have found similar associations between previous lower extremity injury and subsequent lower extremity (17, 18, 25, 31) and increased incidence of recurrent ankle and knee injuries (29).
Potential reasons for these observed associations include individual-level factors such as behavioral attributes (e.g., risk-taking, overtraining, health care-seeking) and injury-specific factors. Injury-specific factors include anatomical or structural aspects (of joint, muscle, ligament, tendon, or bone), inadequate rehabilitation of previous injuries, premature return to activity, or a combination of these causal pathways (20). A third, intermediate class of factors may be individual attributes that operate at the level of the joint, such as certain types of lower extremity movement biomechanics or muscle firing patterns that predispose individuals to lower extremity injury (21, 23). In the current study, analyses of knee and ankle injuries (Table 5) indicated that ankle or knee-specific injury history was a much stronger predictor than overall lower extremity injury. In both males and females, subjects with no history of knee/ankle injury and a positive history of other LE injury were at similar risk to those with no LE injury at all.
This suggests that factors specific to that anatomic site, such as predisposing or injury-altered biomechanics (such as muscle firing patterns or inadequate proprioception), poor rehabilitation of one or more prior injuries at that anatomical site, or anatomic predisposition (such as knee ligament alignment within the joint) may be the key factors, rather than behavioral and psychological factors such as risk taking or care seeking. Behavioral and psychological factors operate at the level of the individual: if individual-level (rather than injury-specific or intermediate) factors were the main reason underlying the association between injury history and incident injury, then one would expect the RRs in Tables 4 and 5 to be distributed about (i.e. both above and below) the overall association (RR=1.74). Instead, associations strengthened considerably (i.e. above only) in these injury-specific analyses. This was true for both males and females.
From an injury prevention standpoint, these findings stress the importance of injury history identification and appropriate measures to identify the presence of any deficits that may predispose the individual to subsequent injury. For example, if there are discernable LE movement differences between those with injury history and those without injury history, then these may represent human movement “deficits” that are modifiable through neuromuscular and proprioceptive training programs. Such programs have been shown to decrease risk of new injuries (19, 22); however, the ability of these programs to reduce risk among individuals with a history of previous injuries is unknown.
Previous studies in military populations suggest that many factors may differentially affect men and women. These include current fitness levels (3, 4); previous physical activity participation (12, 16); and BMI and/or stature (12). Variation in the prevalence of these factors between men and women may account for why some specific injury types, such as stress fractures, are more frequent in females than males in military settings (4, 12). In the current study, the role of injury history was examined in considerable detail and with a large sample size. Females had a higher incidence of medically treated stress fractures and MTSS over the basic training period compared to males, consistent with the existing literature (14). Interestingly, the role of injury history was very similar for males and females. Thus, despite the higher prevalence injury history in females, injury history did not account for the observed gender differences in incident injury rates. In fact, the gender imbalance in injury incidence persisted even after adjustment for multiple factors. However, the dataset did not include markers of psychosocial factors such as propensity to seek health care for an injury. Previous studies in military populations suggest that, in general, females are more likely to report injuries and seek medical care compared to males (1, 5, 12). Both quantitative findings from surveys and qualitative studies of injured soldiers suggest that there are gender differences in health care seeking and reporting differences (10). A study of military academy cadets (5) supports the concept that reporting differences may explain the associations observed between women and men, but also indicated reporting may be strongly influenced by social context (such as the role of senior students). Such contextual effects are strongly apparent in cadet basic training, when the incoming class is being supervised by senior students being evaluated on their leadership potential and performance.
Limitations
This study was conducted with a physically active population of military academy cadets, but there is no guarantee that the findings are applicable to other physically active populations. This study utilized medical encounter data from the DMSS and individuals could be evaluated and treated on multiple days by multiple provider types, potentially leading to over-counting of injuries. To address this, the study employed a method developed by an international group and used previously in military populations (9, 13). Another limitation of this study is that severity measures, treatment details, type of provider seen, time lost from basic training, rehabilitation of prior injuries, and human movement biomechanics were not available. There is also potential for misclassification of incident injury outcomes in this study. An outcome due to a medical encounter (or care) for a lingering baseline injury event could be incorrectly classified as care for an incident event during basic training. Models were run excluding the cadets who had a baseline LE injury in the past 6 months that limited their physical activity. Adjusted estimates remained elevated. Similarly, for this study July 1st was chosen as the start date for the basic training period and Aug 31st was the end date. Using August 31st may overlap into fall sport seasons and an injury sustained during fall sport may be attributed to basic training, and thereby potentially inflating the injury rate for basic training. These analyses do not account for attrition of cadets during basic training period.
Strengths
The study also has some strengths. These data for this study come from a prospective cohort of 9811 cadets representing all three academies over a four year period. All cadets were engaged in the same activities during this 2-month period and outside activities are unlikely to be responsible for the injury events. Medically treated injuries were ascertained using the DMSS which captures all medical encounters provided at the military academies during this two month period. In addition, injury events were identified utilizing methodology applied previously by researchers in surveillance of medically-treated injuries of military populations (9, 13). Information about cadets at baseline included injury history and multivariate analyses adjusted for potential confounders.
Conclusion
Injury history upon entry into the academy is strongly associated with medically-treated LE injuries during cadet basic training. These results support the need for future studies to examine whether there are differences in biomechanical factors, underlying predispositions, and inadequate rehabilitation of previous injuries among those with and without history of injury. Academy health care providers can use injury history information along with these other identified factors to target injury prevention efforts in incoming cadets.
Supplementary Material
Acknowledgments
JUMP-ACL Study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (R01-AR054061001). Pilot work was supported by the American Orthopedic Society for Sports Medicine. Dr. Stephen W. Marshall and the University of North Carolina Injury Prevention Research Center are partially supported by an award from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (R49/CE002479). The views and opinions expressed are those of the authors and they do not reflect the official policy of the U.S. Service Academies, the Department of Defense, or the U.S. Government. Special thanks to all the cadets who participated in this study and to service academies that supported the study. We’d also like to acknowledge the members of the JUMP-ACL study team. From the University of North Carolina at Chapel Hill: Shrikant Bangdiwala PhD, Bing Yu PhD, Michelle Boling PhD ATC, Chuck Thigpen PhD PT ATC, Lindsay Strickland PhD ATC, Ben Goeger MS ATC, Candice Goerger MS ATC, Melanie McGrath PhD ATC, David Bell MEd PhD ATC, and Kevin Guskiewicz PhD ATC. From other universities: William E. Garrett PhD MD (Duke University), COL(Ret) Dean Taylor MD (Duke University), Julie Gilchrist MD (Centers for Disease Control and Prevention), James Onate PhD ATC (Old Dominion University). From the U.S. Naval Academy: CDR Scott Pyne MD, CDR David Keblish MD, CDR Sean Kelly MD, Gregg Calhoon ATC. From the U.S. Air Force Academy: COL John Tokish MD, Barbara Coley, COL Robert Sullivan MD. From the U.S. Military Academy: Karen Y. Peck, MEd ATC, COL (Ret) Thomas M. DeBerardino MD, Sally B. Mountcastle PhD, COL (Ret) Paul D. Stoneman PT PhD, COL Steven J. Svoboda MD, and LTC(P) Brett D. Owens MD.
Footnotes
CONFLICT OF INTEREST:
The authors have no conflicts of interest to disclose. The results of the present study do not constitute endorsement by ACSM.
References
- 1.Almeida S, Trone D, Leone D, Shaffer R, Patheal S, Long K. Gender differences in musculoskeletal injury rates: a function of symptom reporting? Medicine & Science in Sports & Exercise. 1999;31(12):1807–12. doi: 10.1097/00005768-199912000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Barell V, Aharonson-Daniel L, Fingerhut LA, et al. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8(2):91–6. doi: 10.1136/ip.8.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell NS, Mangione TW, Hemenway D, Amoroso PJ, Jones BH. High injury rates among female Army trainees: A function of gender? Am J Prev Med. 2000;18(3, Supplement 1):141–6. doi: 10.1016/s0749-3797(99)00173-7. [DOI] [PubMed] [Google Scholar]
- 4.Bijur PE, Horodyski M, Egerton W, Kurzon M, Lifrak S, Friedman S. Comparison of Injury During Cadet Basic Training by Gender. Arch Pediatr Adolesc Med. 1997;151(5):456–61. doi: 10.1001/archpedi.1997.02170420026004. [DOI] [PubMed] [Google Scholar]
- 5.Billings CE. Epidemiology of Injuries and Illness during the United States Air Force Academy 2002 Basic Cadet Training Program: Documenting the Need for Prevention. Mil Med. 2004;169(8):664–70. doi: 10.7205/milmed.169.8.664. [DOI] [PubMed] [Google Scholar]
- 6.Bullock SH, Jones BH, Gilchrist J, Marshall SW. Prevention of Physical Training-Related Injuries: Recommendations for the Military and Other Active Populations Based on Expedited Systematic Reviews. Am J Prev Med. 2010;38(1, Supplement 1):S156–S81. doi: 10.1016/j.amepre.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Gilchrist J, H JB, Sleet DA, Kimsey CD. Exercise-related injuries among women: strategies for prevention from civilian and military studies. MMWR Recommendations and Reports. 2000;49(RR-2):13–33. [PubMed] [Google Scholar]
- 8.Grier T, Morrison S, Knapik J, Canham-Chervak M, Jones B. Risk factors for injuries in the U.S. Army Ordnance School. Mil Med. 2011;176(11):1292–9. doi: 10.7205/milmed-d-11-00215. [DOI] [PubMed] [Google Scholar]
- 9.Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. Musculoskeletal Injuries: Description of an Under-Recognized Injury Problem Among Military Personnel. Am J Prev Med. 2010;38(1, Supplement 1):S61–S70. doi: 10.1016/j.amepre.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 10.Jennings BM, Yoder LH, Heiner SL, Loan LA, Bingham MO. Soldiers With Musculoskeletal Injuries. Journal of Nursing Scholarship. 2008;40(3):268–74. doi: 10.1111/j.1547-5069.2008.00237.x. [DOI] [PubMed] [Google Scholar]
- 11.Jones B, Knapik J. Physical training and exercise-related injuries. Surveillance, research and injury prevention in military populations. Sports Med. 1999;27(2):111–25. doi: 10.2165/00007256-199927020-00004. [DOI] [PubMed] [Google Scholar]
- 12.Jones BH, Bovee MW, Harris JM, Cowan DN. Intrinsic risk factors for exercise-related injuries among male and female army trainees. Am J Sports Med. 1993;21(5):705–10. doi: 10.1177/036354659302100512. [DOI] [PubMed] [Google Scholar]
- 13.Jones BH, Canham-Chervak M, Canada S, Mitchener TA, Moore S. Medical Surveillance of Injuries in the U.S. Military: Descriptive Epidemiology and Recommendations for Improvement. Am J Prev Med. 2010;38(1, Supplement 1):S42–S60. doi: 10.1016/j.amepre.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 14.Jones BH, Thacker SB, Gilchrist J, Kimsey CD, Sosin DM. Prevention of Lower Extremity Stress Fractures in Athletes and Soldiers: A Systematic Review. Epidemiol Rev. 2002;24(2):228–47. doi: 10.1093/epirev/mxf011. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman KR, Brodine S, Shaffer R. Military training-related injuries: Surveillance, research, and prevention. Am J Prev Med. 2000;18(3, Supplement 1):54–63. doi: 10.1016/s0749-3797(00)00114-8. [DOI] [PubMed] [Google Scholar]
- 16.Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. Risk factors for training-related injuries among men and women in basic combat training. Medicine & Science in Sports & Exercise. 2001;33(6):946–54. doi: 10.1097/00005768-200106000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Knowles SB, Marshall SW, Bowling JM, et al. A Prospective Study of Injury Incidence among North Carolina High School Athletes. Am J Epidemiol. 2006:kwj337. doi: 10.1093/aje/kwj337. [DOI] [PubMed] [Google Scholar]
- 18.Kucera KL, Marshall SW, Kirkendall DT, Marchak PM, Garrett WE. Injury history as a risk factor for incident injury in youth soccer. Br J Sports Med. 2005;39(7):462. doi: 10.1136/bjsm.2004.013672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a Neuromuscular and Proprioceptive Training Program in Preventing Anterior Cruciate Ligament Injuries in Female Athletes: 2-Year Follow-up. Am J Sports Med. 2005;33(7):1003–10. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 20.Murphy D, Connolly D, Beynnon B. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37(1):13–29. doi: 10.1136/bjsm.37.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myer G, Ford K, Di Stasi S, Foss K, Micheli L, Hewett T. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49(2):118–22. doi: 10.1136/bjsports-2013-092536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olsen O-E, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. Br Med J. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Padua D, DiStefano L, Beutler A, de la Motte S, DiStefano M, Marshall S. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury-Prevention Program in Elite-Youth Soccer Athletes. Journal of Athletic Training. 2015;50(6):589–95. doi: 10.4085/1062-6050-50.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padua D, Frank B, Donaldson A, et al. Seven steps for developing and implementing a preventive training program: lessons learned from JUMP-ACL and beyond. Clin Sports Med. 2014;33(4):615–32. doi: 10.1016/j.csm.2014.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rauh M, Macera C, Wiksten D. Subsequent Injury Patterns in Girls’ High School Sports. Journal of Athletic Training. 2007;42(4):486–94. [PMC free article] [PubMed] [Google Scholar]
- 26.Rubertone M, Brundage J. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002;92(12):1900–4. doi: 10.2105/ajph.92.12.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruscio B, Jones B, Bullock S, et al. A process to identify military injury prevention priorities based on injury type and limited duty days. Am J Prev Med. 2010;38(1 Suppl):S19–33. doi: 10.1016/j.amepre.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Snedecor MR, Boudreau CF, Ellis BE, Schulman J, Hite M, Chambers B. U.S. Air Force recruit injury and health study. Am J Prev Med. 2000;18(3, Supplement 1):129–40. doi: 10.1016/s0749-3797(00)00109-4. [DOI] [PubMed] [Google Scholar]
- 29.Swensen D, Yard E, Fields S, Comstock RD. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009;37(8):1586–93. doi: 10.1177/0363546509332500. [DOI] [PubMed] [Google Scholar]
- 30.Van Mechelen W, Hlobil H, Kemper H. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med. 1992;14(2):82–99. doi: 10.2165/00007256-199214020-00002. [DOI] [PubMed] [Google Scholar]
- 31.Yang J, Bowling JM, Lewis MA, Marshall SW, Runyan CW, Mueller FO. Use of Discretionary Protective Equipment in High School Athletes: Prevalence and Determinants. Am J Public Health. 2005;95(11):1996–2002. doi: 10.2105/AJPH.2004.050807. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


