Abstract
Background
Inflammatory bowel disease (IBD) is a heterogeneous chronic inflammatory condition requiring significant healthcare expenditure. Subgroups of individuals contribute disproportionately to spending. We aimed to determine demographic and clinical factors predictive of high healthcare expenditures for IBD patients followed over a multiyear period.
Methods
This was a registry analysis using a prospective observational, consented, natural history registry from a tertiary IBD center and associated medical charges, not including pharmacy expenses. The 100 patients with the highest medical charges (top 5%) were compared to the median 300 patients. Logistic regression determined demographic and clinical factors associated with high charge patients.
Results
IBD patients in the high charge group had significantly more unemployment (p<0.0001), black race (p=0.013), comorbid psychiatric illness (p=0.002), hypertension (p=0.01), diabetes (p=0.004), opiate use (p<0.0001), perianal involvement (p=0.002), penetrating disease (p<0.0001), and extensive colitis (p=0.01). In multivariate analysis unemployment (CD: OR 3.04; 95% CI 1.32–7.02; UC: OR 2.68; 95% CI 1.20–5.99), psychiatric illness (UC: OR 2.08; 95% CI 1.03–4.19), opiates (CD: OR 5.61; 95% CI 2.67–11.82; UC: OR 5.14; 95% CI 2.52–10.48), prior surgery (CD: OR 3.29; 95% CI 1.59–6.82; UC: OR 2.72; 95% CI 1.39–5.32), penetrating CD (OR 3.29; 95% CI 1.02–10.62), and corticosteroid requirement (CD: OR 3.78; 95% CI 1.86–7.65; UC: OR 2.98; 95% CI 1.51–5.90) remained independently associated with high charges.
Conclusion
High expenditure IBD patients were affected by more severe disease. The high prevalence of depression, anxiety, and chronic pain in these patients suggests the need for focused treatment of these comorbidities ultimately to reduce financial burden.
Keywords: inflammatory bowel disease, cost, depression, superutilizer
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic inflammatory condition affecting the gastrointestinal tract resulting from dysregulated immune response to intestinal microflora in genetically susceptible individuals. (1, 2) IBD, including Crohn’s disease (CD) and ulcerative colitis (UC), is a lifelong illness. Patients often experience a relapsing and remitting clinical course frequently causing significant morbidity and poor patient quality of life.(3)
The cost of IBD care has risen dramatically,(4) partially due to increasing prevalence of IBD,(5, 6) but also due to the necessity of invasive procedures, surgical intervention, and expensive biologic therapies.(7, 8) Recent estimates place the United States burden of CD around $10.9–15.5 billion ($25,282–$26,192 per patient)(9) and UC at $8.1–14.9 billion ($14,686–$19,946 per patient) per year.(10)
Healthcare expenditures in IBD patients are not uniform. Previous studies have suggested the upper quartile of costs accounted for 80% of total financial expenses(11) and another study reported the highest 2% of patients accrued 34% of total costs.(12) Prior to the introduction of anti-tumor necrosis factor (anti-TNF) therapy, the single largest contributor to costs was inpatient care with hospitalization accounting for 56–80% total costs in CD(11, 12) and 41–55% in UC.(4, 13) More recent studies suggest that anti-TNF therapy is now the main contributor to costs.(14) The lack of prognostic markers and inevitably variable disease courses have only exacerbated this financial situation with the ability to determine high-cost patients only after multiple years of surgeries, hospitalizations with expensive diagnostic work-ups and procedures, and expensive medications.
Recent research has focused on identifying high-utilizers of the healthcare system(15) in an effort to focus intervention and cost-reduction methods on these costly patients. Initial efforts helped identify several broad risk factors for high utilization patients: presence of comorbid medical conditions, limited access to care,(16) unstable medical relationships,(17) and coexisting mental health disorders.(18) However, this concept of high healthcare utilization patients has not been explored in depth in IBD. Ideally, these costly patients could be identified prior to years of healthcare utilization. The purpose of this study was to determine baseline patient demographic and disease factors that are associated with high healthcare utilization by IBD patients.
MATERIALS AND METHODS
Study Population
Adult (>18 years) IBD patients who were prospectively recruited to participate in a natural history research registry at a tertiary care center were used for this study. Patients were considered for inclusion if they were seen in the outpatient setting between 2009 and 2013. In order to ensure longitudinal evaluation, patients were only included if they had three or more continuous years of follow up within the UPMC Digestive Disease Center within the UPMC system (>20 hospitals, >500 outpatient sites) during the study period. Financial charges for all healthcare services from 2009–2013 were obtained for all registry patients. Financial charges included both inpatient and professional service charges. Inpatient-related charges included fees for room and board, administrative, medication, laboratory, diagnostic testing, and procedures that occurred while admitted to the hospital. Professional service fees incorporated physician or specialized personnel fees for surgery, anesthesia, endoscopy, radiology, pathology, emergency department physician services, outpatient laboratory testing, outpatient diagnostic tests or procedures (e.g. echocardiogram), gender-specific health care (e.g. mammogram), and outpatient clinic visits. Outpatient pharmacy and medication charges were not included in the charge data obtained. In order to identify high healthcare utilization patients with potentially intervenable features as opposed to stable patients being treated with expensive medications (i.e. anti-tumor necrosis factor agents) with few options for expense reduction, we elected not to impute the costs of biologic therapy. Charges were inflated to 2013 base year using Consumer Price Index adjustment rates (http://www.bls.gov/data/inflation_calculator.htm). All charges were in US dollars. Charges were totaled and organized for the years 2009–2013. Due to the extremely skewed nature of the financial charges, the highest 100 charge values (approximately top 5%) were selected and categorized as the “High Charge” patient group. The median value of total charges was then determined and the surrounding 300 patients formed the “Median Charge” category to maintain a 1:3 case to control ratio.
Demographic and Clinical Data
Clinical and historical information was obtained from the IBD registry with manual confirmation using the electronic medical record (EMR). Demographic data collected included age, gender, race, marital and employment status, smoking status, medical insurance possession, and median household income from patient home zip code (http://www.psc.isr.umich.edu/dis/census/Features/tract2zip/). Comorbid medical conditions were retrieved from the registry and were determined by ICD-9 code as well as EMR problem list. Medications including selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and prescription opiates at initial clinic visit were recorded. IBD phenotype was determined based on endoscopic and clinical data at the initial encounter. Anatomic location and disease behavior were described using Montreal Classification(19) on initial endoscopic or radiographic evaluation. IBD-specific medical therapies including systemic corticosteroids, biology therapy (infliximab, adalimumab, certolizumab pegol), immunomodulators (azathioprine, methotrexate, 6-mercaptopurine), and 5-aminosalicylate compounds at first clinical encounter were also recorded as well as the use of total parental nutrition for IBD related indication (e.g. short bowel) at the time of enrollment. To measure disease activity over the study period, frequency of IBD-specific surgery verified by manual review of operative report and prospectively collected disease activity measures including Harvey-Bradshaw Index (HBI), Ulcerative Colitis Activity Index (UCAI), and short inflammatory bowel disease questionnaire (SIBDQ).(20–22)
Statistical Analysis
Categorical variables were expressed as percentages and continuous variables as median and interquartile range (IQR). Measures of association were performed using Fisher’s exact test for categorical variables and Wilcoxon rank-sum testing for continuous variables. Univariate logistic regression analysis of charge group membership was used to select variables for inclusion in the multivariate model. Variables with p<0.1 on univariate analysis were included in final multivariate regression model. A multivariate model was fit for each CD and UC due to the mutually exclusive nature of Montreal Classification.
ETHICAL CONSIDERATIONS
Enrollment in and use of the IBD registry (Protocol #0309054) as well as the current registry analysis (Protocol #15050062) was approved by the Institutional Review Board at the University of Pittsburgh.
RESULTS
Study Cohort
There were 2078 patients with charge data available from 2009–2013 accounting for $214,317,739 in total healthcare charges (FIGURE 1). The median charge value for all patients was $14,322 (range $76–3,835,676, IQR $84,340). The top 100 patients forming the “High Charge” group amassed $95,030,747 in charges with a median charge value of $691,081 (IQR $495,498). The 300 patients with charges closest to the median total charge formed the “Median Charge” group accounting for $4,527,035 in total charges (median $14,322, IQR $5,493). After selection for three consecutive years of follow up, 92 patients remained in the High Charge group and 246 patients in the Median Charge group.
Figure 1.
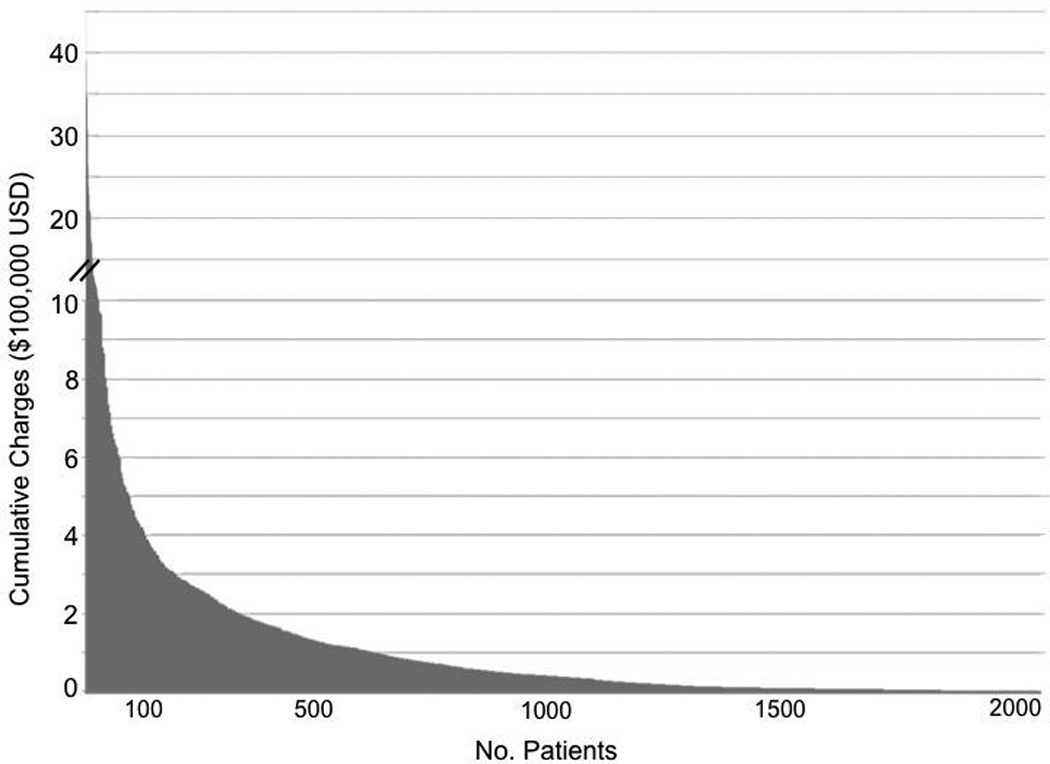
Distribution of cumulative financial charges from 2009–2013 for IBD patients enrolled in the research registry (n=2078)
There was significantly more active disease and lower quality of life in High Charge group over the study period including corticosteroid requirement (77.2% vs. 44.3%; p<0.001), IBD-surgery (80.4% vs. 14.1%; p<0.001), median HBI (7.0 vs. 2.5; p<0.001), median UCAI (5.5 vs. 2.0; p<0.001), and median SIBDQ (41.0 vs. 55.0; p<0.001) (SUPPLEMENTARY TABLE 1).
Patient Demographics
Significantly more patients in the High Charge group were black (7.6% vs. 1.6%; p=0.05), unemployed (37.0% vs. 12.2%; p<0.0001), were from lower median zip code income ($45,894 vs. $48,687; p=0.04), had comorbid psychiatric disease (35.9% vs. 19.9%; p=0.002), hypertension (33.7% vs. 19.5%; p=0.01), and diabetes (9.8% vs. 4.9%; p=0.004) (TABLE 1). Significantly more patients in the High Charge group were prescribed SSRIs (20.7% vs. 10.6%; p=0.02) and opiate medications (47.8% vs. 9.3%; p<0.0001) at the first visit than patients in the Median Charge group. There were no significant differences in gender (p=0.54), age (p=0.52), marital status (p=0.17), medical insurance (p=1.00), or smoking status (p=0.18) between High and Median Charge groups.
Table 1.
Study cohort baseline demographics, comorbidities, medications, and disease characteristics by financial charge group
| High Charge | Median Charge | p-value | |
|---|---|---|---|
| No. | 92 | 246 | -- |
| Female Gender, n(%) | 48 (52.2) | 139 (56.5) | 0.54 |
| Age, years median (IQR) | 44.0 (26.1) | 46.0 (23) | 0.52 |
| Mean Body Mass Index (± SD) | 26.7 ± 5.9 | 26.7 ± 5.6 | 0.80 |
| Race, n(%) | 0.05 | ||
| Caucasian | 85 (92.4) | 238 (96.7) | |
| Black | 7 (7.6) | 4 (1.6) | |
| Hispanic | 0 | 2 (0.8) | |
| Other/Unknown | 0 | 2 (0.8) | |
| Marital Status, n(%) | 0.17 | ||
| Single | 27 (29.3) | 61 (24.8) | |
| Married | 40 (43.5) | 121 (49.2) | |
| Divorced | 8 (8.7) | 8 (3.3) | |
| Widowed | 0 | 4 (1.6) | |
| Unknown | 17 (18.5) | 52 (21.1) | |
| Employment, n(%) | <0.0001 | ||
| Full | 31 (33.7) | 140 (56.9) | |
| Part | 1 (1.1) | 5 (2.0) | |
| Unemployed | 34 (37.0) | 30 (12.2) | |
| Retired | 10 (10.9) | 24 (9.8) | |
| Self-employed | 1 (1.1) | 10 (4.1) | |
| Student | 8 (8.7) | 16 (6.5) | |
| Unknown | 7 (7.6) | 21 (8.5) | |
| Smoking status, n(%) | 0.20 | ||
| Non-smoker | 61 (66.3) | 184 (74.8) | |
| Ex-smoker | 24 (26.1) | 50 (20.3) | |
| Current smoker | 7 (7.6) | 11 (4.5) | |
| Medical Insurance, n(%) | 75 (81.5) | 201 (81.7) | 1.00 |
| Median Annual Zipcode Income (IQR) | $45,894 ($16,875) | $48,687 ($22,644) | 0.04 |
| Comorbidities, n(%) | |||
| Psychiatric Disease | 33 (35.9) | 49 (19.9) | 0.002 |
| Hypertension | 31 (33.7) | 48 (19.5) | 0.01 |
| Diabetes Mellitus | 9 (9.8) | 12 (4.9) | 0.004 |
| Hyperlipidemia | 11 (12.0) | 19 (7.7) | 0.28 |
| Coronary Disease | 2 (2.2) | 4 (1.6) | 0.67 |
| Medication, n(%) | |||
| SSRI | 19 (20.7) | 26 (10.6) | 0.02 |
| SNRI | 8 (8.7) | 10 (4.1) | 0.11 |
| TCA | 5 (5.4) | 8 (3.3) | 0.35 |
| Opiate | 44 (47.8) | 23 (9.3) | <0.0001 |
| Disease, n(%) | 0.17 | ||
| CD | 57 (62.0) | 125 (50.8) | |
| UC | 31 (33.7) | 110 (44.7) | |
| IBD-U | 4 (4.3) | 11 (4.5) | |
| Disease Duration, years median (IQR) | 15 (15) | 15 (12) | 0.58 |
| Prior IBD Surgery, n(%) | 51 (55.4) | 68 (27.6) | <0.0001 |
| CD Location, n(%) | |||
| Ileal (L1) | 11 (19.3) | 27 (21.6) | 0.45 |
| Colonic (L2) | 15 (26.3) | 23 (18.4) | 0.19 |
| Ileocolonic (L3) | 32 (56.1) | 75 (60.0) | 0.75 |
| Upper (L4) | 4 (7.0) | 4 (3.2) | 0.26 |
| Perianal Disease (P) | 19 (33.3) | 16 (12.8) | 0.002 |
| CD Behavior, n(%) | |||
| Inflammatory (B1) | 20 (35.1) | 59 (47.2) | 0.06 |
| Stricturing (B2) | 11 (19.3) | 42 (33.6) | 0.75 |
| Penetrating (B3) | 27 (47.4) | 18 (14.4) | <0.0001 |
| UC Extent, n(%) | |||
| Proctitis (E1) | 0 | 4 (3.6) | 0.57 |
| Left-sided (E2) | 0 | 34 (30.9) | <0.0001 |
| Extensive (E3) | 28 (90.3) | 64 (58.2) | 0.01 |
| IBD Medication, n(%) | |||
| Steroids | 45 (48.9) | 61 (24.8) | <0.0001 |
| Biologics | 24 (26.1) | 27 (11.0) | 0.001 |
| IMs | 30 (32.6) | 96 (39.0) | 0.31 |
| 5-ASA | 28 (30.4) | 100 (40.7) | 0.10 |
| Total Parental Nutrition, n(%) | 1 (1.1) | 1 (0.4) | 0.47 |
| Follow-Up Duration, years mean (SD) | 4.3 (1.0) | 4.2 (1.1) | 0.91 |
SSRI: selective serotonin reuptake inhibitor; SNRI: serotonin norepinephrine reuptake inhibitor; TCA: tricyclic antidepressant; CD: Crohn’s disease; UC: ulcerative colitis; IBD-U: inflammatory bowel disease unclassified; IM: immunomodulator; ASA: aminosalicylate
Multiple logistic regression using variables from univariate analysis (TABLE 2) and controlling for both demographic and disease characteristics demonstrated that in both CD and UC, unemployment (CD: OR 3.04; 95% CI 1.32–7.02; UC: OR 2.68; 95% CI 1.20–5.99) and prescription opiate use (CD: OR 5.61; 95% CI 2.67–11.82; UC: OR 5.14; 95% CI 2.52–10.48) remained independently associated with High Charge status (TABLE 3). In UC but not CD, psychiatric disease (OR 2.08; 95% CI 1.03–4.19) and hypertension (OR 2.23; 95% CI 1.05–4.72) remained significantly associated with high charges.
Table 2.
Univariate logistic regression of charge group using demographic and disease characteristics as predictors
| OR | 95% CI | p-value | |
|---|---|---|---|
| Gender | 0.84 | 0.52–1.36 | 0.48 |
| Age | 0.99 | 0.98–1.01 | 0.51 |
| Mean Body Mass Index | 1.00 | 0.96–1.04 | 0.93 |
| Race* | |||
| Caucasian | -- | -- | -- |
| Black | 4.90 | 1.40–17.16 | 0.013 |
| Hispanic | NA | NA | NA |
| Other/Unknown | NA | NA | NA |
| Marital Status* | |||
| Single | -- | -- | -- |
| Married | 0.75 | 0.42–1.33 | 0.32 |
| Divorced | 2.26 | 0.77–6.65 | 0.14 |
| Widowed | NA | NA | NA |
| Unknown | 0.74 | 0.36–1.50 | 0.40 |
| Employment | |||
| Full | -- | -- | -- |
| Part | 0.90 | 0.10–8.01 | 0.93 |
| Unemployed | 5.12 | 2.74–9.58 | <0.0001 |
| Retired | 1.88 | 0.82–4.33 | 0.14 |
| Self-employed | 0.45 | 0.06–3.66 | 0.46 |
| Student | 2.26 | 0.89–5.74 | 0.09 |
| Unknown | 1.51 | 0.59–3.85 | 0.39 |
| Smoking status | |||
| Non-smoker | -- | -- | -- |
| Ex-smoker | 1.45 | 0.82–2.55 | 0.20 |
| Current smoker | 1.92 | 0.71–5.17 | 0.20 |
| Medical Insurance | 0.99 | 0.53–1.83 | 0.97 |
| Median Annual Zip Code Income | 1.00 | 1.00-1.00 | 0.12 |
| Comorbidities, | |||
| Psychiatric | 2.54 | 1.45–4.44 | 0.001 |
| Hypertension | 2.04 | 1.20–3.48 | 0.009 |
| Diabetes Mellitus | 3.95 | 1.60–9.72 | 0.003 |
| Hyperlipidemia | 1.62 | 0.74–3.56 | 0.23 |
| Coronary Disease | 1.34 | 0.24–7.47 | 0.74 |
| Medication | |||
| SSRI | 2.20 | 1.15–4.21 | 0.02 |
| SNRI | 2.25 | 0.86–5.88 | 0.10 |
| TCA | 1.71 | 0.54–5.37 | 0.36 |
| Opiate | 8.89 | 4.91–16.08 | <0.0001 |
| Disease | |||
| CD | -- | -- | -- |
| UC | 0.62 | 0.37–1.03 | 0.06 |
| IBD-UC | 0.80 | 0.24–2.61 | 0.71 |
| Disease Duration | 1.00 | 0.99–1.00 | 0.79 |
| Prior IBD Surgery | 3.26 | 1.98–5.35 | <0.0001 |
| CD Location | |||
| Ileal | -- | -- | -- |
| Colonic | 1.60 | 0.62–4.17 | 0.34 |
| Ileocolonic | 1.05 | 0.46–2.36 | 0.91 |
| Perianal Disease | 3.41 | 1.60–7.28 | 0.002 |
| CD Behavior | |||
| Inflammatory | -- | -- | -- |
| Stricturing | 0.77 | 0.34–1.78 | 0.55 |
| Penetrating | 4.43 | 2.02–9.68 | <0.0001 |
| UC Extent | |||
| Proctitis | -- | -- | -- |
| Left-sided | NA | NA | NA |
| Extensive | 3.19 | 1.29–7.89 | 0.01 |
| IBD Medications | |||
| Steroids | 2.90 | 1.76–4.79 | <0.0001 |
| Biologics | 2.86 | 1.55–5.29 | 0.001 |
| IMs | 0.76 | 0.46–1.25 | 0.28 |
| 5-ASA | 0.64 | 0.38–1.07 | 0.09 |
| Total Parental Nutrition | 2.69 | 0.17–43.49 | 0.49 |
Logistic regression outcomes limited by empty set input
Table 3.
Multiple logistic regression of charge group using demographic and disease characteristics as predictors
| Crohn’s Disease (n=182) |
Ulcerative Colitis (n=141) |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Race | ||||||
| Caucasian | -- | -- | -- | -- | -- | -- |
| Black | 2.7 | 0.52–13.93 | 0.24 | 3.57 | 0.63–20.16 | 0.15 |
| Employment | ||||||
| Full | -- | -- | -- | -- | -- | -- |
| Part | 0.41 | 0.02–10.84 | 0.59 | 0.64 | 0.04–9.23 | 0.75 |
| Unemployed | 3.04 | 1.32–7.02 | 0.009 | 2.68 | 1.20–5.99 | 0.02 |
| Retired | 1.79 | 0.60–5.33 | 0.30 | 1.57 | 0.52–4.73 | 0.42 |
| Self-employed | 0.52 | 0.05–5.01 | 0.57 | 0.53 | 0.06–4.97 | 0.58 |
| Student | 1.62 | 0.43–6.07 | 0.47 | 1.37 | 0.39–4.77 | 0.62 |
| Unknown | 0.94 | 0.30–2.96 | 0.91 | 1.05 | 0.32–3.46 | 0.94 |
| Comorbidities | ||||||
| Psychiatric | 1.73 | 0.86–3.46 | 0.12 | 2.08 | 1.03–4.19 | 0.04 |
| HTN | 1.97 | 0.94–4.15 | 0.07 | 2.23 | 1.05–4.72 | 0.04 |
| DM | 2.98 | 0.92–9.68 | 0.07 | 2.61 | 0.79–8.68 | 0.12 |
| Medication | ||||||
| SSRI | 1.35 | 0.55–3.34 | 0.52 | 1.12 | 0.47–2.66 | 0.79 |
| SNRI | 0.64 | 0.16–2.56 | 0.52 | 0.62 | 0.17–2.24 | 0.47 |
| Opiate | 5.61 | 2.67–11.82 | <0.0001 | 5.14 | 2.52–10.48 | <0.0001 |
| Prior IBD Surgery | 3.29 | 1.59–6.82 | 0.001 | 2.72 | 1.39–5.32 | 0.003 |
| CD Behavior | -- | -- | -- | |||
| Inflammatory | -- | -- | -- | |||
| Stricturing | 0.35 | 0.11–1.05 | 0.06 | |||
| Penetrating | 3.29 | 1.02–10.62 | 0.047 | |||
| Perianal Disease | 0.94 | 0.23–3.76 | 0.93 | -- | -- | -- |
| UC Extent* | -- | -- | -- | |||
| Proctitis | NA | NA | NA | |||
| Left-sided | NA | NA | NA | |||
| Extensive | 1.75 | 0.86–3.55 | 0.12 | |||
| IBD Medications | ||||||
| Steroids | 3.78 | 1.86–7.65 | <0.0001 | 2.98 | 1.51–5.90 | 0.002 |
| Biologics | 1.83 | 0.73–4.61 | 0.20 | 2.04 | 0.89–4.69 | 0.09 |
Logistic regression outcomes limited by empty set input
HTN: hypertension; DM: diabetes mellitus; OR: odds ratio
Disease Characteristics
There was no significant difference in IBD type (CD, UC, or IBD-U) between High Charge and Median Charge groups (p=0.17) (TABLE 1). Significantly more patients in the High Charge groups had a history of prior IBD surgery (55.4% vs. 27.6%; p<0.0001), had perianal disease (33.3% vs. 12.8%; p=0.002), penetrating CD (47.4% vs. 14.4%; p<0.0001), and extensive UC (90.3% vs. 58.2%; p=0.01) compared to Median Charge patients. There were significantly more patients receiving systemic steroids (48.9% vs. 24.8%; p<0.0001) and biologic therapy (26.1% vs. 11.0%; p=0.001) at initial visit in the High Charge group. There was no difference in disease duration (p=0.58) between the two groups and there was one CD patient in each group receiving total parental nutrition at initial visit (p=0.47) due to short bowel syndrome (High Charge) and post-colectomy malnutrition (Median Charge).
Multiple logistic regression controlling for both demographic and disease characteristics revealed in both CD and UC, a history of prior IBD surgery (CD: OR 3.29; 95% CI 1.59–6.82; UC: OR 2.72; 95% CI 1.39–5.32) and steroid requirement at initial encounter (CD: OR 3.78; 95% CI 1.86–7.65; UC: OR 2.98; 95% CI 1.51–5.90) were independently associated with high charges (TABLE 3). In CD, penetrating behavior (OR 3.29; 95% CI 1.02–10.62) remained significantly associated with charge status while perianal disease failed to reach significance (p=0.93). In UC, extensive colonic involvement failed to reach significance (p=0.12).
DISCUSSION
In this registry analysis of a longitudinal, prospective, observational IBD patient cohort, we have identified that there are several patient characteristics and baseline disease features significantly associated with future high healthcare utilization IBD patients. Patient characteristics including black race, unemployment, multiple comorbidities, and prescription pain medications were associated with future high utilization. Furthermore, penetrating CD and the use of more aggressive medical therapy at first visit were associated with increased healthcare utilization over the next five years. This study identifies several baseline characteristics that may place patients at increased risk of accumulating large healthcare expenditures over the following several years.
In this study patient unemployment was independently significantly associated with the high charge group. This characteristic may reflect socioeconomic disadvantages and barriers to care impeding efficient longitudinal outpatient care.(15) This claim in strengthened by the fact that high utilization patients had significantly lower zip code median income compared to median utilization patients on association analysis. Conversely, one may interpret the association of unemployment as a reflection of disability secondary to debilitating severe IBD. Unfortunately, we could not determine which patients were on disability in this study. While failing to reach statistical significance in multivariate analysis likely due to limited sample size, black race was associated with high charges in association and univariate analysis. The combination of racial and socioeconomic disparities has been previously identified as a detriment to adequate healthcare and a risk factor for high healthcare utilization.(23, 24)
Comorbid medical conditions significantly associated with higher healthcare expenditures in univariate analysis included diabetes and hypertension with hypertension retaining significance in multivariate modeling. While these comorbidities carry intrinsic healthcare costs, they are also harbinger comorbidities that can cause multi-organ dysfunction over time. The contribution of multiple comorbidities to complex medical patients and “superutilizer” patients has been well documented identifying these at-risk patients worthy of personal intervention with associated future healthcare cost reduction.(16, 18) In IBD specifically, medical comorbidities have also been associated with increased rates of post-operative complications(25) as well as increased mortality.(26, 27)
Furthermore psychiatric diseases (depression and/or anxiety) and increased SSRI prescription were also significantly associated with high healthcare utilization in this study. This may represent a patient subgroup with psychosomatic overlap, increased risk for surgery(28) and a cognitive inability to cope with their disease and the intense medical/surgical therapies required.(29, 30) Unfortunately, outcomes on mental health interventions in IBD have been mixed. A Cochrane Review of 21 studies found little to no evidence for psychological interventions in the adult IBD population;(31) however, subsequent adult studies targeting “in need” patients with severe disease and poor mental health demonstrated improved mental quality of life through the use of cognitive behavior therapy.(32) Moreover, recent studies in pediatric CD exhibited improved disease activity indices in children receiving cognitive behavior therapy compared to supportive nondirective therapy.(33) Together, these recent studies endorse the use of specific therapies in targeted populations.
Prescription opiates at the time of the initial visit were similarly associated with future increased healthcare utilization. Prescription opiate use likely identifies a patient subgroup of more severe cases with intense abdominal pain as a result of uncontrolled inflammation, refractory pain from nerve damage, coexisting functional abdominal pain, or narcotic bowel.
It is perhaps unsurprising that disease characteristics defining “severe” disease such a penetrating CD and requiring steroids or biologics, were associated with high utilization patients as these patients require the most intense follow up with invasive monitoring, aggressive medical management, and often require surgical intervention. In this study, High Charge patients had significantly more active disease over the five-year time period measured by corticosteroid requirement, IBD surgery, and disease activity indices. It should be noted that as outpatient pharmacy charges were not included in this study, the association of severe disease and high cost would likely have been even stronger given the increased biologic agent requirement in the High Charge group.
Severe disease contributing disproportionally to healthcare expenditures has been explored in several studies. Silverstein et al used a Markov model for CD to assess disease states over a lifetime and demonstrated that compared to patients with mild CD, patients who required surgery had average monthly charges nearly nine times higher than patients who did not require surgery.(8) Furthermore, Feagan et al demonstrated that the average annual cost of patients requiring chronic steroid or immunosuppressive drug therapy were 45% higher than the remaining CD patient majority.(11) The study also reported that CD patients requiring hospitalization were 6.1 times more costly on average than the remaining majority. These findings hold true in UC as well. Hillson et al found that patients with UC requiring hospital admission amassed direct medical cost more than three times higher than patients who did not require hospitalization.(34)
With the rising cost of healthcare in the US, there is an important push to identify potential strategies for cost reduction. Evidence is mounting that high utilizer patients are receiving inadequate coordination of care, preventative care, or care in the most appropriate settings.(35) Several of the patient characteristics identified in this study are potentially amenable to multidisciplinary intervention including social workers for socioeconomic challenges, case workers to address barriers to care, chronic pain management, mental health care, internal medicine and subspecialty collaboration for complex patients with multiple comorbidities, all with coordinated care plans developed in conjunction with the patient.(36) Recent intervention studies on this multidisciplinary care approach in a non-IBD patient population demonstrated reductions in healthcare utilization and improvement in patient social and clinical outcomes.(37)
There are several limitations to this study. Level of education data of patients was not available. Higher patient education correlates with reduction in health care costs.(38) Similarly, patient attitudes towards their healthcare were not assessed. A collaborative relationship is important point of breakdown in care relationships in superutilizer patients.(17, 18) Alcohol and other substances of abuse data was not available and have been shown to contribute to high utilization.(39) There was little race variation in our study due to the prevalence of these minorities in the City of Pittsburgh. While black race was shown to be associated with higher healthcare expenditures on univariate association, other minorities were unable to be compared. Furthermore, race was not significantly independently associated in multivariate analysis, likely due to limited number of minorities and sample size. Regardless, other studies have shown that other minorities including Hispanics have limited access to care and are associated with higher utilization patients in a variety of diseases.(23) While this study defines conditions associated with high expenditures, it does not define the directionality of the relationship. Further studies are needed to determine the cause and effect. Outpatient pharmacy charge data was not available in this study. Thus, the absolute charge totals from a societal perspective is underestimated. Rather the totals described in the current study represent pure utilization burden from a healthcare system perspective. The differences in financial burden between High Charge and Median Charge groups would likely only be further exaggerated by inclusion of pharmacy charges as High Charge patients were more than two times likely to require biologic agents in this study. Lastly, financial charges vary between institutions and along with the single center nature of the study, limits the generalizability of the results.
This study has several strengths. First the use of a prospective observational data set allows for a real-world collection of a multiyear period of patients allowing for temporal variation in disease course and to minimize the signal of patients with a single acute deterioration. This study utilized a unique measure of healthcare utilization to define high cost patients in charge data. Other studies to date of financial outcomes have largely relied on claims data and ICD codes which can bias results against certain patient populations (e.g. uninsured) and can be inappropriately labeled or entirely missing. While this study is not meant to grossly categorize all high utilization patients as having the same high-risk features, this study helps to identify common themes in IBD patients associated with disproportionately increased future expenditures.
In conclusion, this study identifies several baseline patient demographic characteristics, comorbidities and disease-related risk factors for future high healthcare utilization within an IBD patient cohort. These factors may represent potential targets for cost reduction interventions in conjunction with coordinated care models.
Supplementary Material
Acknowledgments
Grant Support: Benjamin Click reports support from National Institute of Health training grant 5T32DK063922-12 (PI: David Whitcomb, MD PhD). Ioannis Koutroubakis reports support by a sabbatical salary of Medical Faculty University of Crete, Greece. Alyce M. Anderson reports support from University of Pittsburgh Clinical and Translational Science Institute grant 5TL1TR000145-09 (PI: Steven Reiss, MD). David G. Binion and Michael A. Dunn report support from Grant W81XWH-11-2-0133 from the US Army Medical Research and Materiel Command.
Footnotes
Disclosures: None of the authors have any potential conflicts (financial, professional, or personal) related to this manuscript to disclose.
References
- 1.Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abraham C, Cho JH. Inflammatory bowel disease. The New England journal of medicine. 2009;361:2066–2078. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ananthakrishnan AN, Weber LR, Knox JF, et al. Permanent work disability in Crohn's disease. The American journal of gastroenterology. 2008;103:154–161. doi: 10.1111/j.1572-0241.2007.01561.x. [DOI] [PubMed] [Google Scholar]
- 4.Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn's disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135:1907–1913. doi: 10.1053/j.gastro.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42. doi: 10.1053/j.gastro.2011.10.001. quiz e30. [DOI] [PubMed] [Google Scholar]
- 6.Kappelman MD, Moore KR, Allen JK, et al. Recent trends in the prevalence of Crohn's disease and ulcerative colitis in a commercially insured US population. Digestive diseases and sciences. 2013;58:519–525. doi: 10.1007/s10620-012-2371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen RD, Larson LR, Roth JM, et al. The cost of hospitalization in Crohn's disease. The American journal of gastroenterology. 2000;95:524–530. doi: 10.1111/j.1572-0241.2000.01779.x. [DOI] [PubMed] [Google Scholar]
- 8.Silverstein MD, Loftus EV, Sandborn WJ, et al. Clinical course and costs of care for Crohn's disease: Markov model analysis of a population-based cohort. Gastroenterology. 1999;117:49–57. doi: 10.1016/s0016-5085(99)70549-4. [DOI] [PubMed] [Google Scholar]
- 9.Yu AP, Cabanilla LA, Wu EQ, et al. The costs of Crohn's disease in the United States and other Western countries: a systematic review. Current medical research and opinion. 2008;24:319–328. doi: 10.1185/030079908x260790. [DOI] [PubMed] [Google Scholar]
- 10.Cohen RD, Yu AP, Wu EQ, et al. Systematic review: the costs of ulcerative colitis in Western countries. Alimentary pharmacology & therapeutics. 2010;31:693–707. doi: 10.1111/j.1365-2036.2010.04234.x. [DOI] [PubMed] [Google Scholar]
- 11.Feagan BG, Vreeland MG, Larson LR, et al. Annual cost of care for Crohn's disease: a payor perspective. The American journal of gastroenterology. 2000;95:1955–1960. doi: 10.1111/j.1572-0241.2000.02261.x. [DOI] [PubMed] [Google Scholar]
- 12.Hay JW, Hay AR. Inflammatory bowel disease: costs-of-illness. Journal of clinical gastroenterology. 1992;14:309–317. doi: 10.1097/00004836-199206000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Gibson TB, Ng E, Ozminkowski RJ, et al. The direct and indirect cost burden of Crohn's disease and ulcerative colitis. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2008;50:1261–1272. doi: 10.1097/JOM.0b013e318181b8ca. [DOI] [PubMed] [Google Scholar]
- 14.van der Valk ME, Mangen MJ, Leenders M, et al. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFalpha therapy: results from the COIN study. Gut. 2014;63:72–79. doi: 10.1136/gutjnl-2012-303376. [DOI] [PubMed] [Google Scholar]
- 15.Foundation. RWJ. Super-utilizer summit: common themes from innovative complex care management programs. Available at: http://wwwrwjforg/en/library/research/2013/10/super-utilizer-summithtml. [Google Scholar]
- 16.Hempstead K, Delia D, Cantor JC, et al. The fragmentation of hospital use among a cohort of high utilizers: implications for emerging care coordination strategies for patients with multiple chronic conditions. Medical care. 2014;52(Suppl 3):S67–S74. doi: 10.1097/MLR.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 17.Mautner DB, Pang H, Brenner JC, et al. Generating hypotheses about care needs of high utilizers: lessons from patient interviews. Population health management. 2013;16(Suppl 1):S26–S33. doi: 10.1089/pop.2013.0033. [DOI] [PubMed] [Google Scholar]
- 18.Gawande A. Medical Report: The hot spotters—can we lower medical costs by giving the neediest patients better care? Available at: http://wwwnewyorkercom/magazine/2011/01/24/the-hot-spotters Published January 24, 2011. [PubMed] [Google Scholar]
- 19.Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2005;19(Suppl A):5a–36a. doi: 10.1155/2005/269076. [DOI] [PubMed] [Google Scholar]
- 20.Harvey RF, Bradshaw JM. A simple index of Crohn's-disease activity. Lancet. 1980;1:514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- 21.Kozarek RA, Patterson DJ, Gelfand MD, et al. Methotrexate induces clinical and histologic remission in patients with refractory inflammatory bowel disease. Annals of internal medicine. 1989;110:353–356. doi: 10.7326/0003-4819-110-5-353. [DOI] [PubMed] [Google Scholar]
- 22.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn's Relapse Prevention Trial. The American journal of gastroenterology. 1996;91:1571–1578. [PubMed] [Google Scholar]
- 23.Kaufman S, Ali N, DeFiglio V, et al. Early efforts to target and enroll high-risk diabetic patients into urban community-based programs. Health promotion practice. 2014;15:62s–70s. doi: 10.1177/1524839914535776. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen GC, Chong CA, Chong RY. National estimates of the burden of inflammatory bowel disease among racial and ethnic groups in the United States. Journal of Crohn's & colitis. 2014;8:288–295. doi: 10.1016/j.crohns.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 25.De Silva SCM, Ma C, Prusinkiewicz M, Panaccione R, Ghosh S, Mac Lean A, Buie D, Devlin S, Seow D, Leung Y, Hubbard J, Kaplan GG. Predictors of complications following a colectomy for ulcerative colitis patients: A population-based study. Gut. 2009;58:A457. [Google Scholar]
- 26.Winther KV, Jess T, Langholz E, et al. Survival and cause-specific mortality in ulcerative colitis: follow-up of a population-based cohort in Copenhagen County. Gastroenterology. 2003;125:1576–1582. doi: 10.1053/j.gastro.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 27.Roman AL, Munoz F. Comorbidity in inflammatory bowel disease. World journal of gastroenterology : WJG. 2011;17:2723–2733. doi: 10.3748/wjg.v17.i22.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ananthakrishnan AN, Gainer VS, Perez RG, et al. Psychiatric co-morbidity is associated with increased risk of surgery in Crohn's disease. Alimentary pharmacology & therapeutics. 2013;37:445–454. doi: 10.1111/apt.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faust AH, Halpern LF, Danoff-Burg S, et al. Psychosocial factors contributing to inflammatory bowel disease activity and health-related quality of life. Gastroenterology & hepatology. 2012;8:173–181. [PMC free article] [PubMed] [Google Scholar]
- 30.Gandhi S, Jedel S, Hood MM, et al. The relationship between coping, health competence and patient participation among patients with inactive inflammatory bowel disease. Journal of Crohn's & colitis. 2014;8:401–408. doi: 10.1016/j.crohns.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Timmer A, Preiss JC, Motschall E, et al. Psychological interventions for treatment of inflammatory bowel disease. The Cochrane database of systematic reviews. 2011 doi: 10.1002/14651858.CD006913.pub2. Cd006913. [DOI] [PubMed] [Google Scholar]
- 32.Mikocka-Walus A, Bampton P, Hetzel D, et al. Cognitive-behavioural therapy has no effect on disease activity but improves quality of life in subgroups of patients with inflammatory bowel disease: a pilot randomised controlled trial. BMC gastroenterology. 2015;15:54. doi: 10.1186/s12876-015-0278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Szigethy E, Youk AO, Gonzalez-Heydrich J, et al. Effect of 2 psychotherapies on depression and disease activity in pediatric Crohn's disease. Inflammatory bowel diseases. 2015;21:1321–1328. doi: 10.1097/MIB.0000000000000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hillson E, Dybicz S, Waters HC, et al. Health care expenditures in ulcerative colitis: the perspective of a self-insured employer. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2008;50:969–977. doi: 10.1097/JOM.0b013e31816fd663. [DOI] [PubMed] [Google Scholar]
- 35.Mulder BJ, Tzeng HM, Vecchioni ND. Preventing avoidable rehospitalizations by understanding the characteristics of "frequent fliers". Journal of nursing care quality. 2012;27:77–82. doi: 10.1097/NCQ.0b013e318229fddc. [DOI] [PubMed] [Google Scholar]
- 36.Li J, Williams MV. Managing superutilizers-staying patient centered is the solution. Journal of hospital medicine. 2015 doi: 10.1002/jhm.2357. [DOI] [PubMed] [Google Scholar]
- 37.Althaus F, Paroz S, Hugli O, et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Annals of emergency medicine. 2011;58:41–52.e42. doi: 10.1016/j.annemergmed.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Colombara F, Martinato M, Girardin G, et al. Higher levels of knowledge reduce health care costs in patients with inflammatory bowel disease. Inflammatory bowel diseases. 2015;21:615–622. doi: 10.1097/MIB.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 39.Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. The Journal of emergency medicine. 2013;44:717–729. doi: 10.1016/j.jemermed.2012.08.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


