Abstract
Nevus sebaceous is a congenital, benign hamartomatous lesion, characterized by a yellowish to skin-colored, hairless, verrucous plaque on the head and neck region. In later life, a secondary tumor, either benign or malignant, can develop within nevus sebaceous. Eccrine poroma developing on nevus sebaceous is extremely rare. There are few case reports of eccrine poroma developing within nevus sebaceous. We report a case of a 30-year-old female who presented with a congenital, hairless, verrucous, yellowish lesion on the scalp and an erythematous nodule arising within the yellowish lesion for 8 months. Her clinical presentation and histopathological findings were compatible with nevus sebaceous and eccrine poroma.
Key Words: Adnexal neoplasm, Adnexal tumor, Eccrine poroma, Nevus sebaceous
Case Presentation
A 30-year-old female presented with a hairless, yellowish lesion on her scalp that had already been noticed at birth. Eight months earlier, she developed an asymptomatic red nodule arising on the yellowish plaque. There was no history of bleeding on the lesion. She was otherwise healthy and had no history of previous trauma of the scalp.
Physical examination revealed a solitary, slightly verrucous erythematous nodule, 3 cm in diameter and covered with scale and crust arising on a hairless, yellowish verrucous plaque measuring 3 × 6 cm, located on the left frontoparietal region of the scalp (fig. 1). There was no cervical, submandibular, and occipital lymphadenopathy. Other physical examinations were unremarkable.
Fig. 1.

Solitary erythematous, slightly verrucous nodule, 3 cm in diameter, arising on a yellowish, verrucous plaque measuring 3 × 6 cm on the left frontoparietal scalp.
Four-millimeter punch biopsies were performed on the yellowish plaque and red nodule for routine histological examination. The skin biopsy specimen obtained from the yellowish verrucous plaque showed mild epidermal papillomatosis associated with increased sebaceous gland and abortive hair follicles, consistent with nevus sebaceous (fig. 2). Another biopsy specimen obtained from the erythematous nodule revealed that the tumor consisted of uniformly small cuboidal cells, forming anastomosing bands and ductal lumen embedded in a fibrovascular stroma, compatible with eccrine poroma (fig. 3a, fig. 3b). According to the clinical and histopathologic findings, the dermatologic diagnosis was eccrine poroma arising within nevus sebaceous.
Fig. 2.
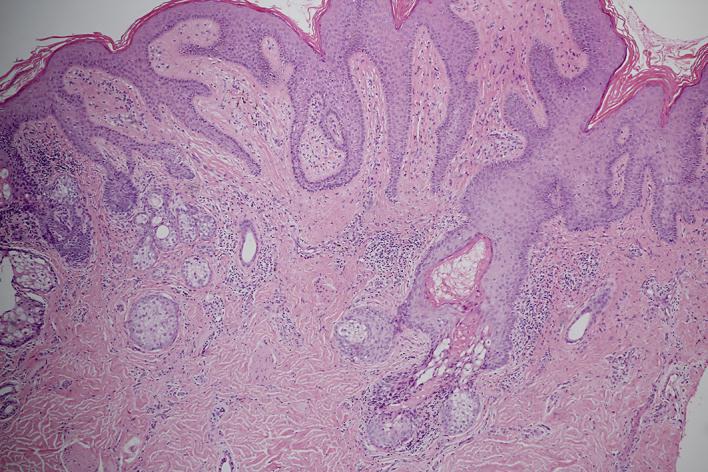
Histopathologic findings demonstrate mild epidermal papillomatosis associated with increased sebaceous gland and abortive hair follicles. HE. Original magnification ×100.
Fig. 3.
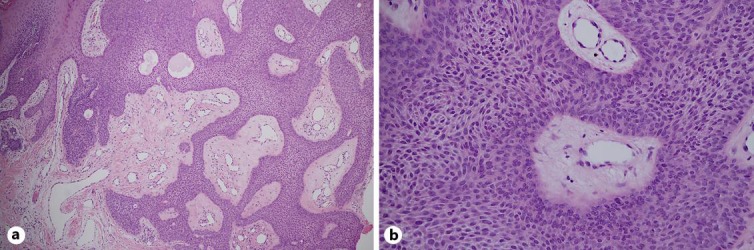
Histopathologic findings showing that the tumor consists of uniformly small cuboidal cells, forming anastomosing bands and ductal lumen emanating from the epidermis embedded in a fibrovascular stroma. a HE. Original magnification ×100. b HE. Original magnification ×400.
Our patient was referred to a plastic surgeon for wide excision of the lesion, which was completely excised with a good cosmetic result. No recurrence was observed in a 3-month follow-up.
Discussion
Nevus sebaceous, also known as nevus sebaceous of Jadassohn or organoid nevus, is a benign congenital hamartoma of cutaneous structures including the epidermis, sebaceous glands, sweat glands, and hair follicles [1, 2]. Nevus sebaceous was first described by Josef Jadassohn in 1895 and further divided in 3 phases (infancy, puberty and adulthood) by Mehregan and Pinkus in 1965 [3]. It usually presents at birth as skin-colored to yellowish, waxy, hairless plaques or linear lesions mainly on the head and neck and especially on the scalp. At puberty, the lesion tends to thicken and becomes papillomatous and verrucous due to androgen effects on the sebaceous glands [1, 4].
Diagnosis can be made based on the characteristic clinical finding, but skin biopsy should be performed if the diagnosis is ambiguous [5]. Histology of nevus sebaceous is characterized by papillomatous or verrucous epidermal hyperplasia and numerous, irregular sebaceous lobules opening directly into the epidermis, with heterotopic apocrine glands and abortive/immature hair follicles [4].
Nevus sebaceous is typically benign and remains unchanged throughout life. However, other tumors can develop within nevus sebaceous during adolescence and adulthood (21.4%) [1]. The majority of secondary tumors are benign. Trichoblastoma is the most common benign tumor to grow within nevus sebaceous (7.4%), followed by syringocystadenoma papilleferum (5.2%), apocrine/eccrine adenoma (2.1%), and trichilemmoma (1.1%) [1]. Basal cell carcinoma is the most common malignant tumor (1.1%) developing from nevus sebaceous [1]. Poroma arising on nevus sebaceous is extremely rare. To date, there are few case reports of poroma, including apocrine poroma and eccrine poroma developing within nevus sebaceous [2, 6, 7].
Eccrine poroma is a benign tumor originating from an intraepidermal portion of the eccrine sweat duct that was first described in 1956 by Goldman et al. [8]. It typically presents as solitary, slow-growing, bright red, skin-colored or pigmented, painful or pruritic, pedunculated, sessile papule or nodule occurring in middle-aged or elderly patients without sexual predilection [6, 9]. Eccrine poroma is commonly located on the sole (65%) and palm (10%) [6]. Interestingly it can occur on almost any cutaneous surface containing sweat glands, namely the neck, chest, nose, scalp, and ear pinna [6]. Scalp lesions are uncommon [2] and usually are asymptomatic, showing more pigmented tendency than lesions on the palm or sole [10]. The histologic features of eccrine poroma demonstrates a well-circumscribed tumor composed of proliferative, compact cuboidal keratinocytes with small monomorphic nuclei and scant eosinophilic cytoplasm (poroid cells) radiating from the basal layer of the epidermis into the dermis with highly vascularized stroma. Necrosis en masse or clear cell change may be observed [11]. The clinical course of eccrine poroma is benign, with low risk of malignant transformation into porocarcinoma or recurrence [11].
Differential diagnoses of red nodular lesions on the scalp include benign and malignant tumors commonly arising on nevus sebaceous (e.g., trichoblastoma, syringocystadenoma papilleferum, basal cell carcinoma, etc.), chronic infection (e.g. nontuberculous mycobacterium infection), and wart.
Surgical excision is the treatment of choice for nevus sebaceous. Full-thickness excision should be performed [5]. Mohs micrographic surgery may be offered in cases of nevus sebaceous with concomitant malignant tumor [12]. Timing for excision is controversy [5]. Due to the low incidence of malignant tumor arising on nevus sebaceous, prophylactic excision is unnecessary [12]. Several dermatologists suggest that it is best to perform excision when there is evidence of secondary tumor or when nevus sebaceous has a great impact on cosmetic appearance [12, 13, 14]. Alternative treatments for nevus sebaceous include fractional laser, dermabrasion, or photodynamic therapy that have variable outcomes, as nevus sebaceous may not be completely removed through these modalities [5, 15, 16, 17, 18, 19, 20]. Monitoring for malignant transformation is mandatory in all cases with incomplete removal of nevus sebaceous [4, 11].
In conclusion, we report a case of eccrine poroma arising within nevus sebaceous. Al-though poroma rarely arises on nevus sebaceous, it should be considered in the differential diagnosis of secondary neoplasm accompanying nevus sebaceous.
Statement of Ethics
The patient gave written informed consent.
Disclosure Statement
The authors declare no conflicts of interest.
References
- 1.Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332–337. doi: 10.1016/j.jaad.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Cicek AF, Aykan A, Yapici A, Gamsizkan M, Ozturk S, Demiriz M. Nevus sebaceus with basal cell carcinoma, poroma, and verruca vulgaris. Indian J Pathol Microbiol. 2015;58:534–536. doi: 10.4103/0377-4929.168885. [DOI] [PubMed] [Google Scholar]
- 3.Hsu MC, Liau JY, Hong JL, et al. Secondary neoplasms arising from nevus sebaceus: a retrospective study of 450 cases in Taiwan. J Dermatol. 2016;43:175–180. doi: 10.1111/1346-8138.13070. [DOI] [PubMed] [Google Scholar]
- 4.Alsaad KO, Obaidat NA, Ghazarian D. Skin adnexal neoplasms – part 1: an approach to tumours of the pilosebaceous unit. J Clin Pathol. 2007;60:129–144. doi: 10.1136/jcp.2006.040337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel P, Malik K, Khachemoune A. Sebaceus and Becker's nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197–204. doi: 10.1007/s40257-015-0123-y. [DOI] [PubMed] [Google Scholar]
- 6.Bae MI, Cho TH, Shin MK, Jeong KH. An unusual clinical presentation of eccrine poroma occurring on the auricle. Indian J Dermatol. 2015;60:523. doi: 10.4103/0019-5154.164446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang E, Lee JS, Kazakov DV. A rare combination of sebaceoma with carcinomatous change (sebaceous carcinoma), trichoblastoma, and poroma arising from a nevus sebaceus. J Cutan Pathol. 2013;40:676–682. doi: 10.1111/cup.12146. [DOI] [PubMed] [Google Scholar]
- 8.Goldman P, Pinkus H, Rogin JR. Eccrine poroma; tumors exhibiting features of the epidermal sweat duct unit. AMA Arch Derm. 1956;74:511–521. [PubMed] [Google Scholar]
- 9.Park E, Lee DS. Eom KS. Eccrine poroma on the scalp a case report with MR findings. Nerve. 2015;1:53–54. [Google Scholar]
- 10.Moore TO, Orman HL, Orman SK, Helm KF. Poromas of the head and neck. J Am Acad Dermatol. 2001;44:48–52. doi: 10.1067/mjd.2001.110048. [DOI] [PubMed] [Google Scholar]
- 11.Sawaya JL, Khachemoune A. Poroma: a review of eccrine, apocrine, and malignant forms. Int J Dermatol. 2014;53:1053–1061. doi: 10.1111/ijd.12448. [DOI] [PubMed] [Google Scholar]
- 12.Taher M, Feibleman C, Bennett R. Squamous cell carcinoma arising in a nevus sebaceous of Jadassohn in a 9-year-old girl treatment using Mohs micrographic surgery with literature review. Dermatol Surg. 2010;36:1203–1208. doi: 10.1111/j.1524-4725.2010.01611.x. [DOI] [PubMed] [Google Scholar]
- 13.Barkham MC, Moss C, White N, Brundler MA. Should naevus sebaceous be excised prophylactically? A clinical audit. J Plast Reconst Aesthet Surg. 2007;60:1269–1270. doi: 10.1016/j.bjps.2007.03.038. [DOI] [PubMed] [Google Scholar]
- 14.Santibanez-Gallerani A, Marshall D, Duarte AM, Melnick SJ, Thaller S. Should nevus sebaceous of Jadassohn in children be excised? A study of 757 cases, and literature review. J Craniofac Surg. 2003;14:658–660. doi: 10.1097/00001665-200309000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Ashinoff R. Linear nevus sebaceous of Jadassohn treated with the carbon dioxide laser. Pediatr Dermatol. 1993;10:189–191. doi: 10.1111/j.1525-1470.1993.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 16.Lee HE, Park SB, Lee JH, Im M. Nevus sebaceous treated with fractional carbon dioxide laser followed by pulsed dye laser. Indian J Dermatol Venereol Leprol. 2014;80:478–480. doi: 10.4103/0378-6323.140336. [DOI] [PubMed] [Google Scholar]
- 17.Chung BY, Han SS, Kim BW, Chang SE, Lee MW. Effective treatment of congenital melanocytic nevus and nevus sebaceous using pinhole method with the erbium-doped yttrium aluminium garnet laser. Anna Dermatol. 2014;26:651–653. doi: 10.5021/ad.2014.26.5.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim HS, Jun JH, Lee JY. Photodynamic therapy of facial nevus sebaceous. Photodermatol Photoimmunol Photomed. 2010;26:98–100. doi: 10.1111/j.1600-0781.2010.00489.x. [DOI] [PubMed] [Google Scholar]
- 19.In Si, Lee JY, Kim YC. Topical photodynamic therapy for nevus sebaceous on the face. Eur J Dermatol. 2010;20:590–592. doi: 10.1684/ejd.2010.1048. [DOI] [PubMed] [Google Scholar]
- 20.Beer GM, Widder W, Cierpka K, Kompatscher P, Meyer VE. Malignant tumors associated with nevus sebaceous: therapeutic consequences. Aesthetic Plast Surg. 1999;23:224–227. doi: 10.1007/s002669900272. [DOI] [PubMed] [Google Scholar]


