Abstract
Objectives
Close, frequent contact between children and care providers in child-care centers presents many opportunities to spread human noroviruses. We compared state licensing regulations for child-care centers with national guidelines written to prevent human noroviruses.
Methods
We reviewed child-care licensing regulations for all 50 U.S. states and the District of Columbia in effect in June 2015 to determine if these regulations fully, partially, or did not address 14 prevention practices in four topic areas: (1) hand hygiene, (2) exclusion of ill people, (3) environmental sanitation, and (4) diapering.
Results
Approximately two-thirds (8.9) of the 14 practices across all state regulations were partially or fully addressed, with few (2.6) fully addressed. Practices related to exclusion of ill people and diapering were fully addressed most often, while practices related to hand hygiene and environmental sanitation were fully addressed least often.
Conclusion
Regulations based on guidelines for best practices are one way to prevent the spread of human noroviruses in child-care facilities, if the regulations are enforced. Our findings show that, in mid-2015, many state child-care regulations did not fully address these guidelines, suggesting the need to review these regulations to be sure they are based on best practices
In 2011, 61% of all U.S. children ≤5 years of age spent time in child care.1 The close, frequent contact between children and their care providers presents opportunities to spread enteric pathogens that cause acute gastroenteritis. Although many enteric pathogens can cause acute gastroenteritis, most cases in the United States are attributed to viruses (e.g., human noroviruses, rotaviruses, and hepatitis A virus) rather than bacteria or parasites.2 In general, these enteric viruses are highly contagious because of their low infectious dose, large number of particles shed in feces and vomitus, and resistance to environmental conditions.3,4 As such, prevention strategies (e.g., hand hygiene, environmental sanitation, and exclusion of sick people) are similar. Overall, rates of illness attributed to rotaviruses and hepatitis A virus in the United States have declined since 2006 because of the wide availability and use of vaccines.5,6 However, no vaccine is currently available for human noroviruses, so proper implementation of prevention strategies is important, especially in child-care settings, which, along with schools, accounted for 214 of 3,494 (6%) of reported outbreaks from 2009 to 2012.7
All 50 U.S. states and the District of Columbia (hereinafter “states”) have licensing regulations for child-care centers that establish minimum requirements to protect the health and safety of children, including the prevention of acute gastroenteritis.8 Multiple recommending bodies, such as the Centers for Disease Control and Prevention (CDC)9 and the American Academy of Pediatrics,10 have prepared guidelines on best practices to prevent acute gastroenteritis, but many states may not be using the guidelines to inform regulations. We compared state licensing regulations for child-care centers with national guidelines written to prevent the spread of human noroviruses, a leading cause of acute gastroenteritis, in child-care environments.11–13
METHODS
The most recent licensing regulations for child-care centers were downloaded in portable document format (PDF) from the government websites of all states in June 2015.14–71 We focused on regulations for child-care centers (i.e., nonresidential facilities providing child-care services) and did not review regulations for family or group daycare homes (i.e., facilities located in a licensee's residence).8
We identified 14 prevention practices in four topic areas: (1) hand hygiene, (2) exclusion of ill people, (3) environmental sanitation, and (4) diapering. The first three topic areas were based on CDC's human noroviruses outbreak prevention guidelines.9 CDC practices do not address diapering, but we included this topic area because of the high concentration of human noroviruses in feces72,73 and the frequency of diapering in child-care centers. To assess diapering regulations, we used standards from Caring for Our Children: National Health and Safety Performance Standards: Practices for Early Care and Education Programs (hereinafter, CFOC), which was developed jointly by the American Academy of Pediatrics, American Public Health Association, and National Resource Center for Health and Safety in Child Care and Early Education. These standards represent the best evidence, expertise, and experience on health and safety practices for child-care centers.10
We then created a system to score the 14 practices based on methods used by Cradock et al.74 (Table 1). If the state regulation fully addressed an individual practice, the practice was assigned two points. Fully addressed practices were defined as those aligned with CDC or CFOC standards. If the regulation partially addressed a practice, the practice was assigned one point. If a practice was not addressed by the regulation, the practice was assigned zero points. Two of the 14 practices (isolation of ill children and separation of diaper-changing and food areas) were scored only as fully addressed (two points) or not addressed (zero points), because it was not possible to partially address these practices. One reviewer knowledgeable about human noroviruses prevention guidelines reviewed and then assigned a score to the 14 practices in the state regulations using this system. Any uncertainties were reconciled with another expert.
Table 1.
Coding criteria to determine alignment of child-care center regulations with 14 practices that prevent human norovirus infections, 50 U.S. states and the District of Columbia, June 2015
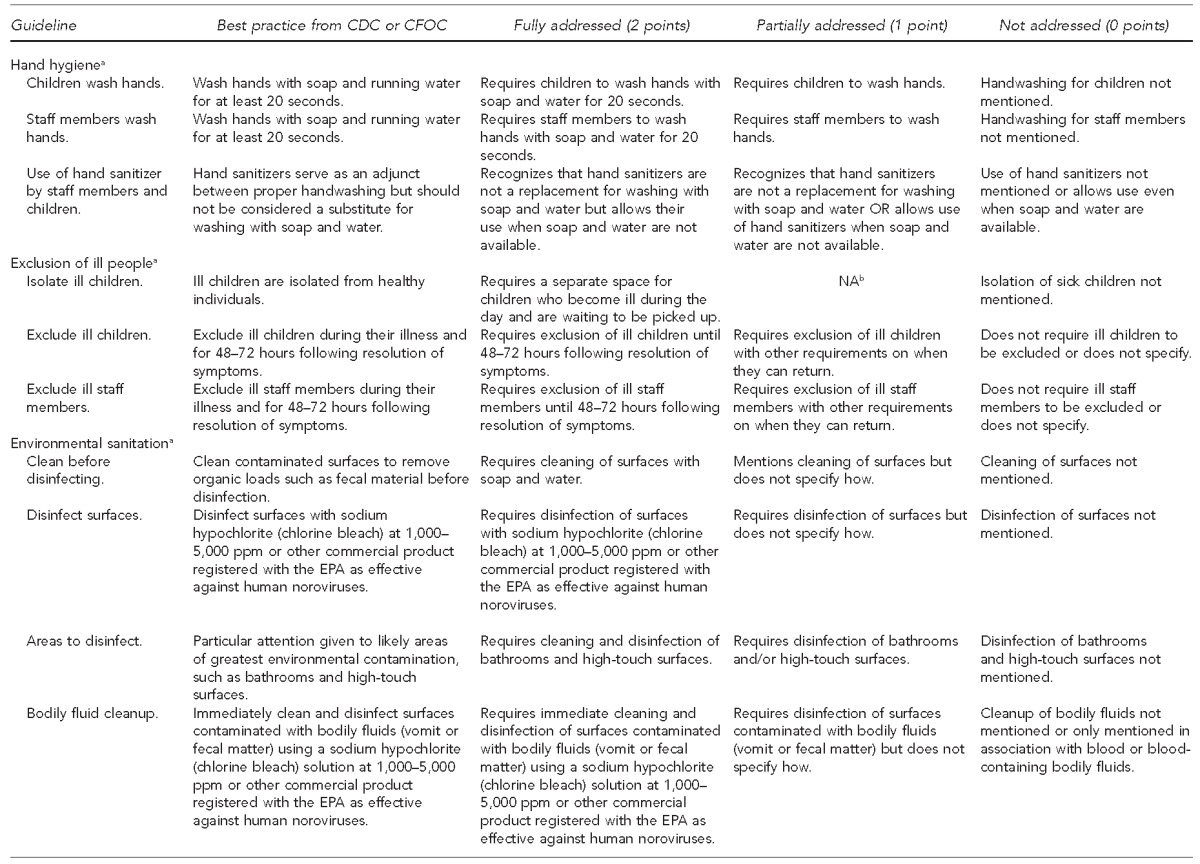

aBest practice comes from: Hall AJ, Vinje J, Lopman B, Park GW, Yen C, Gregoricus N, et al. Updated norovirus outbreak management and disease prevention guidelines [published erratum appears in MMWR Morb Mortal Wkly Rep 2011;60(20):670]. MMWR Recomm Rep 2011;60(RR3):1-15.
bNot possible to partially address this practice
cBest practice comes from: American Academy of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. Caring for our children: national health and safety performance standards: guidelines for early care and education programs. 3rd ed. Elk Grove Village (IL): American Academy of Pediatrics; 2011.
CDC = Centers for Disease Control and Prevention
CFOC = Caring for Our Children
NA = not applicable
ppm = parts per million
EPA = U.S. Environmental Protection Agency
Before coding began, each PDF of state regulations was searched by key words. For hand hygiene, key words were “hand,” “wash,” “saniti,” and “rub.” For the exclusion of ill people topic area, key words were “sick,” “ill,” “disease,” and “exclu.” For environmental sanitation, key words were “clean,” “disinfect,” “saniti,” “bodily,” “fluid,” “ppm,” “vomit,” and “bleach.” For diapering, the key word was “diaper.” Each key word was entered independently into the “find” bar of the PDF version of each state licensing regulation, and results were highlighted with a color designated for that topic area (e.g., yellow for hand hygiene or pink for exclusion of ill people). The search results were reviewed to ensure search terms encompassed all relevant data.
Next, two scores were calculated by aggregating individual state-level scores.74 The first score we calculated was a comprehensiveness score, defined as the mean number of practices across all state-level regulations that partially or fully addressed the CDC or CFOC practices (i.e., number of practices that scored one or two points). We then calculated a strength score, defined as the mean number of practices associated with each topic area across all state-level regulations that were fully addressed (i.e., number of practices that scored two points). We then calculated descriptive statistics (mean, standard deviation, and range) for practices within each topic area as well as for all 14 practices to determine how state child-care regulations as a whole addressed prevention practices.
RESULTS
The overall comprehensiveness score was 8.9, indicating that 64% of the 14 practices recommended by CDC and CFOC were partially or fully addressed across all state regulations (Table 2). However, the overall strength score (2.6) showed that most practices listed in regulations were not fully addressed. When reviewing the comprehensiveness and strength scores by four topic areas, our findings showed the hand-hygiene comprehensiveness score was high (2.3 of 3.0) but the strength score was low (0.4 of 3.0). Similarly, the comprehensiveness score for exclusion of ill people was also high (2.4 of 3.0) but the strength score was low (0.9 of 3.0). The lowest comprehensiveness (1.7 of 4.0) and strength (0.2 of 4.0) scores were in the area of environmental sanitation. The comprehensiveness (2.5 of 4.0) and strength (1.1 of 4.0) scores for the four diapering practices were higher than those for environmental sanitation but were still low.
Table 2.
Comprehensivenessa and strengthb scores for alignment of child-care center regulations to prevention and control guidelines for human noroviruses, 50 U.S. states and the District of Columbia, June 2015

The comprehensiveness score was calculated as the average number of practices coded as either partially (one point) or fully (two points) addressed based on CDC guidelines (Hall AJ, Vinjé J, Lopman B, Park GW, Yen C, Gregoricus N, et al. Updated norovirus outbreak management and disease prevention guidelines [published erratum appears in MMWR Morb Mortal Wkly Rep 2011;60(02):670]. MMWR Morb Mortal Wkly Rep 2011;60(RR3):1-15.) or CFOC guidelines (American Academy of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. Caring for our children: national health and safety performance standards: guidelines for early care and education programs. 3rd ed. Elk Grove Village (IL): American Academy of Pediatrics; 2011.)
The strength score was calculated as the average number of practices coded as fully (two points) addressed based on CDC or CFOC guidelines.
SD = standard deviation
CDC = Centers for Disease Control and Prevention
CFOC = Caring for Our Children
Two of the 14 practices were fully addressed by more than half of states: isolation of ill children (45 states) and separation of diaper-changing and food areas (35 states). More than half of the states did not address five practices: bodily fluid cleanup (42 states), areas to disinfect (39 states), hand sanitizer use (35 states), disinfecting diaper-changing table (26 states), and wearing gloves when changing diapers (29 states). No state fully addressed exclusion of ill children and staff members, but most states partially addressed exclusion of ill children (45 states) and exclusion of ill staff members (32 states). Within the topic area of environmental sanitation, areas to disinfect and bodily fluid cleanup were each fully addressed by one state. Areas to disinfect were partially addressed by 11 states, and bodily fluid cleanup was addressed by eight states. Additionally, no state fully addressed disinfecting of surfaces, but 35 states partially addressed this practice (Tables 3 and 4).
Table 3.
Frequency with which practices associated with prevention of human norovirus infection were addressed in child-care center regulations, 50 U.S. states and the District of Columbia, June 2015

aThe scoring system gives two points for practices that are fully addressed in the state regulations, one point for practices that are partially addressed in the state regulations, and zero points for practices that are not addressed in the state regulations.
bNot all percentages total to 100 because of rounding.
cIt was not possible to partially address this practice.
NA = not applicable
Table 4.
Results of alignment scoringa of child-care center regulations with 14 practices that prevent human norovirus infection, 50 U.S. states and the District of Columbia, June 2015


The scoring system gives two points for practices that are fully addressed in the state regulations, one point for practices that are partially addressed in the state regulations, and zero points for practices that are not addressed in the state regulations.
bYear refers to the year that the state's child-care regulations were last updated as of June 2015.
DISCUSSION
Nearly all state regulations required children and staff members to wash their hands, but most did not fully address how children and staff members should wash their hands. For example, many state regulations either did not cite the length of time to spend in handwashing or cited varying durations. The length of time spent in handwashing is important because several studies showed that the longer the wash time, the more microorganisms are removed from hands.75–77 However, there is a lack of consensus by recommending bodies (e.g., CDC, the U.S. Food and Drug Administration, and the World Health Organization) on how long to wash hands. This lack of consensus may explain why most state regulations did not specify the length of handwashing time in their regulations. Nonetheless, the most recent CDC guidelines for preventing human norovirus infections recommend a wash time of at least 20 seconds.9
Few state regulations addressed hand sanitizer use as an adjunct to or substitute for handwashing. Evidence of hand sanitizer efficacy against human noroviruses varies.78–80 At present, alcohol-based hand rubs are the only type of hand sanitizer recommended by health organizations such as CDC and the World Health Organization (WHO).9,81 These hand rubs are effective against vegetative bacterial cells but less so against human noroviruses.78–80,82,83 Alcohol alone cannot eliminate human noroviruses from hands, but certain formulations of alcohol-based hand rubs have been shown to reduce the number of viral particles.78–80,84 Until conclusive evidence about the efficacy of hand sanitizers (alcohol-based or non-alcohol-based) against human noroviruses is available, hand sanitizers will presumably not be fully addressed in state regulations.
Although most state regulations fully addressed isolation of ill children from healthy children (45 states), none fully addressed exclusion of sick children and staff members. No regulation stated how long the child or staff member should be excluded from the facility. Excluding ill people is critical because noroviruses are known to be easily transmitted from person to person (e.g., 69% of reported human norovirus outbreaks from 2009 to 2012 were transmitted from person to person7). Per current CDC guidelines, individuals who have a human norovirus infection can return to work 48–72 hours after symptoms are resolved, because they are then generally past the most infectious period of the illness.9 Some state regulations had other requirements, such as allowing children (15 states) and workers (12 states) to return to child care only after approval from a health-care provider. Six states allowed children and four states allowed staff members to return after a “recommended” period of exclusion but did not specify what recommendation was being referenced. All of the requirements given by state regulations on when children and staff can return after being ill could be problematic because sick people continue to shed virus particles at low levels for weeks after symptoms are resolved.73,85,86
Practices related to environmental sanitation were also not fully addressed by most state regulations. One common reason for this is that the terms “sanitizing” and “disinfecting” were used incorrectly or interchangeably. For example, a number of state regulations required potty chairs to be sanitized after use. However, because potty chairs come in contact with bodily fluids, they should be disinfected rather than sanitized.9 To eliminate human noroviruses from environmental surfaces contaminated with bodily fluids (e.g., vomit and fecal matter) or during an outbreak, a surface must be disinfected and not sanitized.9 In addition to not defining the proper pathogen removal treatment, most state regulations (42 states) did require surfaces to be cleaned before disinfection or sanitization. This step is critical because organic matter (e.g., filth, vomit, or fecal matter) can affect the efficacy of disinfectants.87,88 Lastly, no state regulations listed the proper disinfection concentration for noroviruses. Many disinfectants are not effective against human noroviruses at regulated concentrations and/or contact times.89–92 For example, chlorine bleach can only eliminate human noroviruses at disinfecting concentrations of 1,000–5,000 parts per million (ppm), not at sanitizing concentrations of 50–200 ppm.87–89,93 The 11 state regulations that listed a concentration for using chlorine bleach to disinfect recommended concentrations of <1,000 ppm, which would be effective against vegetative bacteria, fungi, and some viruses, but not necessarily human noroviruses.
Diapering can also contribute to the spread of human noroviruses, but state regulations only partially addressed guidelines that could prevent the spread of human noroviruses by contaminated hands and environmental surfaces. One way to minimize contamination of hands with feces during diaper changing is to wear single-use gloves, which was fully addressed by only six state regulations. Wearing gloves while changing diapers can prevent hand contamination, especially under fingernails and around nail beds, which are difficult to clean.94 However, gloves could provide workers with a false sense of security, so handwashing rather than glove use is widely recommended by public health experts.
Dirty diapers must be discarded in a sanitary manner to prevent surface contamination. The American Academy of Pediatrics et al.10 recommends using washable, plastic-lined, covered, hands-free containers to store dirty diapers. However, only four states fully addressed all four conditions for storing soiled diapers. Diaper-changing surfaces must be properly cleaned before disinfection because human noroviruses may be more resistant to disinfection when in feces.87,88 During and after diapering, human noroviruses can be transferred to surfaces and hands in the surrounding area. As such, diapering areas must be separate from food preparation and serving areas,87,95 and staff members who change diapers should never handle food. No states fully addressed all four diapering practices that could reduce the transmission of human noroviruses.
Limitations
This study was subject to several limitations. First, our findings were based on regulations that were in effect as of June 2015 and do not reflect changes made after this date. Second, noninclusion of a practice in a state's regulations does not mean that particular practice is not known or not enforced. County- or city-level regulations for child-care centers may exist, or the standard for a practice could be in a sub-regulatory guidance or policy. Third, how regulations are communicated and enforced varied by state, district, and inspector. As such, full or partial compliance with national guidelines on best practices is difficult to discern from written regulations alone. Additionally, child-care centers might pursue national accreditation from one of three national early childhood accreditation agencies: National Association for the Education of Young Children, National Accreditation Commission for Early Care and Education Programs, or National Early Childhood Program Accreditation, which might require more rigorous infectious disease control standards than are presented in state regulations.
CONCLUSIONS
Enforcing regulations based on guidelines for best practices, such as those prepared by CDC9 and CFOC,10 is one way to reduce the burden of illness from human noroviruses in child-care facilities. However, our findings indicate that many state child-care regulations have not fully addressed CDC or CFOC guidelines for prevention of human norovirus infections in child-care centers. Therefore, state child-care regulations should be reviewed and revised to be sure they are based on best practices known to prevent human norovirus infections.
Footnotes
This study was based on work supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture (USDA), under agreement #2008-51110-04335 and #2011-68003-30395. The opinions, findings, conclusions, and recommendations expressed in this article are those of the authors and do not necessarily reflect the views of the USDA. This study was exempt from institutional review board approval as no data were collected from human subjects.
REFERENCES
- 1.Laughlin L. Washington: Census Bureau (US), Department of Commerce, Economics and Statistics Administration; 2013. Who's minding the kids? Child care arrangements: spring 2011. [Google Scholar]
- 2.Hall AJ, Lopman BA, Payne DC, Patel MM, Gastañaduy PA, Vinjé J, et al. Norovirus disease in the United States. Emerg Infect Dis. 2013;19:1198–205. doi: 10.3201/eid1908.130465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desselberger U. Rotaviruses. Virus Res. 2014;190:75–96. doi: 10.1016/j.virusres.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Robilotti E, Deresinski S, Pinsky BA. Norovirus. Clin Microbiol Rev. 2015;28:134–64. doi: 10.1128/CMR.00075-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leshem E, Lopman B, Glass R, Gentsch J, Bányai K, Parashar U, et al. Distribution of rotavirus strains and strain-specific effectiveness of the rotavirus vaccine after its introduction: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:847–56. doi: 10.1016/S1473-3099(14)70832-1. [DOI] [PubMed] [Google Scholar]
- 6.Ly KN, Klevens RM. Trends in disease and complications of hepatitis A virus infection in the United States, 1999–2011: a new concern for adults. J Infect Dis. 2015;212:176–82. doi: 10.1093/infdis/jiu834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall AJ, Wikswo ME, Pringle K, Gould LH, Parashar UD. Vital signs: foodborne norovirus outbreaks—United States, 2009–2012. MMWR Morb Mortal Wkly Rep. 2014;63(22):491–5. [PMC free article] [PubMed] [Google Scholar]
- 8.National Child Care Information and Technical Assistance Center, Department of Health and Human Services (US), National Association for Regulatory Administration. Ann Arbor (MI): Inter-university Consortium for Political and Social Research; 2009. Child care licensing study, 2007. [Google Scholar]
- 9.Hall AJ, Vinjé J, Lopman B, Park GW, Yen C, Gregoricus N, et al. Updated norovirus outbreak management and disease prevention guidelines [published erratum appears in MMWR Morb Mortal Wkly Rep 2011;60(02):670] MMWR Morb Mortal Wkly Rep. 2011;60(RR3):1–15. [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. 3rd ed. Elk Grove Village (IL): American Academy of Pediatrics; 2011. Caring for our children: national health and safety performance standards: guidelines for early care and education programs. [Google Scholar]
- 11.Lee MB, Greig JD. A review of enteric outbreaks in child care centers: effective infection control recommendations. J Environ Health. 2008;71:24–32. [PubMed] [Google Scholar]
- 12.Lyman WH, Walsh JF, Kotch JB, Weber DJ, Gunn E, Vinjé J. Prospective study of etiologic agents of acute gastroenteritis outbreaks in child care centers. J Pediatr. 2009;154:253–7. doi: 10.1016/j.jpeds.2008.07.057. [DOI] [PubMed] [Google Scholar]
- 13.Ferreira MSR, Xavier Mda P, Tinga AC, Rose TL, Fumian TM, Fialho AM, et al. Assessment of gastroenteric viruses frequency in a children's day care center in Rio De Janeiro, Brazil: a fifteen year study (1994–2008) PLoS One. 2012;7:e33754. doi: 10.1371/journal.pone.0033754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.State of Alabama Department of Human Resources. Minimum standards for day care centers and nighttime centers: regulations and procedures. 2001 [cited 2015 Dec 10] Available from: http://www.dhr.alabama.gov/documents/minimumstandards_daycare.pdf.
- 15. Title 7 Alaska Adm. Code §57 (2007)
- 16. Title 7 Alaska Adm. Code §10 (2007)
- 17.Arizona Department of Health Services. Arizona administrative code and Arizona revised statutes for child care facilities. 2010 [cited 2015 Dec 11] Available from: http://www.azdhs.gov/documents/licensing/childcare-facilities/rules/bccl-child-care-facility-rules.pdf.
- 18.Arkansas Department of Human Services. Minimum licensing requirements for child care centers. 2015 [cited 2015 Dec 11] Available from: http://humanservices.arkansas.gov/dccece/licensing_docs/2014%20A1%20CCC%20clean%20copy%20final%20filing.pdf.
- 19.California Department of Social Services. Child care center regulations [cited 2015 Dec 11] Available from: http://www.cdss.ca.gov/ord/PG587.htm.
- 20. 12 Code of Colorado Regulations §2509-8 (2012)
- 21. 6 Code of Colorado Regulations §1010-7.
- 22.State of Connecticut, Office of Early Childhood, Division of Licensing. Statutes and regulations for licensing child day care centers and group day care homes. 2015 [cited 2015 Dec 11] Available from: http://www.ct.gov/oec/lib/oec/licensing/childcare/centers_statsregs.pdf.
- 23.Delaware Department of Services for Children, Youth and Their Families. 101 DELACARE: regulations for early care and education and school-age centers. 2015 [cited 2015 Dec 11] Available from: http://kids.delaware.gov/occl/announcements/Center-Regulations-2015.pdf.
- 24.District of Columbia Department of Health, District of Columbia Department of Human Services. Notice of final rulemaking. 2007 [cited 2015 Dec 11] Available from: http://osse.dc.gov/sites/default/files/dc/sites/osse/publication/attachments/Licensing_Regulations_29_DCMR_3.pdf.
- 25. 65C Florida Adm. Code §22 (2013)
- 26.Georgia Department of Early Care and Learning. Rules for child care learning centers. Chapter 591-1-1. Updated 2016 Jan 1 [cited 2016 Jan 21] Available from: http://decal.ga.gov/documents/attachments/CCLCrulesandregulations.pdf.
- 27.Hawaii Department of Human Services. Licensing for infant and toddler child care centers. 2002 [cited 2015 Dec 11] Available from: http://humanservices.hawaii.gov/bessd/files/2013/11/HAR_17-895-infant-and-toddler-child-care-center-rules.pdf.
- 28.Idaho Department of Health and Welfare. Basic day care license. 2011 [cited 2015 Dec 11] Available from: http://www.legislature.idaho.gov/idstat/title39/T39CH11.htm.
- 29.Illinois Department of Children and Family Services. Licensing standards for day care centers. 2014 [cited 2015 Dec 11] Available from: http://www.ilga.gov/commission/jcar/admincode/089/08900407sections.html.
- 30.Indiana Family and Social Services Administration. Interpretative guide for child care center rules. 2013 [cited 2015 Dec 11] Available from: www.in.gov/fssa/files/BCC_Centers_Interpretive_Guide.pdf.
- 31.Iowa Department of Human Services. Child care centers. 2015 [cited 2015 Dec 11] Available from: https://ccmis.dhs.state.ia.us/providerportal/documentviewer.aspx?ID=8.
- 32. 28 Kansas Adm. Reg. §4-122 (2008)
- 33. 28 Kansas Adm. Reg. §4-420 (2012)
- 34.Kentucky Department for Community Based Services. Child-care center health and safety standards. 2013 [cited 2015 Dec 11] Available from: http://www.lrc.ky.gov/kar/922/002/120.htm.
- 35.Louisiana Department of Education. Louisiana early learning center licensing regulations. 2015 [cited 2015 Dec 11] Available from: http://www.louisianabelieves.com/docs/default-source/early-childhood/ccdf-bulletin-137-early-learning-center-licensing-regulations.pdf?sfvrsn=4.
- 36.Louisiana Department of Children and Family Services. Licensing class “A” regulations for child care centers. 2014 [cited 2015 Dec 14] Available from: http://www.louisianabelieves.com/docs/default-source/child-care-providers/2014-child-care-updates-(9).pdf?sfvrsn=2.
- 37.Maine Department of Health and Human Services. Rules for the licensing of child care facilities. 2008 [cited 2015 Dec 11] Available from: http://maine.gov/dhhs/ocfs/ec/occhs/cclicensing.htm.
- 38. Code of Maryland Regulations 13A, §16.01-19 (2014)
- 39.Massachusetts Department of Early Education and Care. Standards for the licensure or approval of family child care; small group and school age and large group and school age child care programs. 2010 [cited 2015 Dec 11] Available from: http://www.mass.gov/edu/docs/eec/licensing/regulations/2010-reg-family-group-school-age-child-care-programs.pdf.
- 40.Michigan Department of Human Services. Licensing rules for child care centers. 2014 [cited 2015 Dec 11] Available from: http://michigan.gov/documents/dhs/Child_Care_Center_Rules_419095_7.pdf.
- 41.Minnesota Department of Human Services. Child care center licensing. 2013 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/MN/2_9503-MN.pdf.
- 42. 15 Mississippi Adm. Code §55 (2013)
- 43.Missouri Department of Health and Senior Services. Licensing rules for group child care homes and child care centers. 2011 [cited 2015 Dec 11] Available from: http://s1.sos.mo.gov/cmsimages/adrules/csr/current/19csr/19c30-62.pdf.
- 44.Montana Department of Public Health and Human Services. Licensing requirements for child day care centers. 2012 [cited 2015 Dec 11] Available from: https://dphhs.mt.gov/Portals/85/qad/documents/licensurebureau/child%20care/DCC%20regulation%20book%20july%202012.pdf.
- 45.Nebraska Department of Health and Human Services. Child care centers. 2013 [cited 2015 Dec 11] Available from: http://www.sos.ne.gov/rules-and-regs/regsearch/Rules/Health_and_Human_Services_System/Title-391/Chapter-3.pdf.
- 46. Nevada Adm. Code Ch. 432A (2012)
- 47.New Hampshire Department of Health and Human Services. Child care program licensing rules. 2008 [cited 2015 Dec 11] Available from: http://www.dhhs.nh.gov/oos/cclu/documents/finalrules.pdf.
- 48.New Jersey Department of Children and Families. Manual of requirements for child care centers. 2013 [cited 2015 Dec 11] Available from: http://www.state.nj.us/dcf/providers/licensing/laws/CCCmanual.pdf.
- 49.New Mexico Kids. Child care centers, out of school time programs, family child care homes, and other early care and education programs. 2012 [cited 2015 Dec 11] Available from: http://164.64.110.239/nmac/parts/title08/08.016.0002.pdf.
- 50.New York Office of Children and Family Services. Child day care centers. 2015 [cited 2015 Dec 11] Available from: http://ocfs.ny.gov/main/childcare/regs/418-1%20DCC%20effective%206.1.15.pdf.
- 51. 10A North Carolina Adm. Code, Ch. 9 (2015)
- 52.North Carolina Department of Environment and Natural Resources. Sanitation of child care centers. 2007 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/NC/nc_2800.pdf.
- 53.North Dakota Department of Human Services. Child care center early childhood services. 2014 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/ND/75-03-10.pdf.
- 54. 5101 Ohio Adm. Code §2-12 (2011)
- 55.Oklahoma Department of Human Services. Licensing requirements for child care centers. 2013 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/OK/OK_2013%20Child%20Care%20Centers.pdf.
- 56. 414 Oregon Adm. Rules §300 (2013)
- 57. 55 Pennsylvania Code §3270 (2010)
- 58.Rhode Island Department of Children, Youth and Families. Child care program regulations for licensure. 2013 [cited 2015 Dec 11] Available from: http://www.dcyf.ri.gov/docs/center_regs.pdf.
- 59.South Carolina Department of Social Services. Regulations for the licensing of child care centers. 2005 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/SC/sc_centers.pdf.
- 60.South Dakota Department of Social Services. Licensed day care programs. 2013 [cited 2015 Dec 11] Available from: http://legis.sd.gov/Rules/DisplayRule.aspx?Rule=67:42:10.
- 61.Tennessee Department of Human Services. Licensure rules for child care centers. 2009 [cited 2015 Dec 11] Available from: http://share.tn.gov/sos/rules/1240/1240-04/1240-04-03.20090314.pdf.
- 62.Texas Department of Family and Protective Services. Minimum standards for child-care centers. 2015 [cited 2015 Dec 11] Available from: https://www.dfps.state.tx.us/documents/Child_Care/Child_Care_Standards_and_Regulations/746_Centers.pdf.
- 63. 430 Utah Adm. Code §100 (2013)
- 64. 33 Vermont Statutes Annotated §306(b) (2013)
- 65. 63.2 Virginia Adm. Code §17 (2013)
- 66.Virginia Department of Social Services. Standards for licensed child day centers. 2012 [cited 2015 Dec 11] Available from: http://www.dss.virginia.gov/files/division/licensing/cdc/intro_page/code_regulations/regulations/standards.pdf.
- 67. 170 Washington Adm. Code §170-295 (2014)
- 68.West Virginia Department of Human Services. Child care centers licensing. 2014 [cited 2015 Dec 11] Available from: http://www.dhhr.wv.gov/bcf/Childcare/Documents/ChildCareCenterRegulationWeb.pdf.
- 69.Wisconsin Department of Children and Families. Group child care centers. 2014 [cited 2015 Dec 11] Available from: http://docs.legis.wisconsin.gov/code/admin_code/dcf/201_252/251.pdf.
- 70.Wyoming Department of Family Services. Administrative rules for certification of child care facilities: certification of child caring acilities. 2013 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/WY/2013_Chapter%203%20Administrative%20Rules%20for%20Certification%20of%20 Child%20Care%20Facilities%20Certification%20of%20Child%20Caring%20Facilities.pdf.
- 71.Wyoming Department of Family Services. Administrative rules for certification of child care facilities: health and sanitation. 2012 [cited 2015 Dec 11] Available from: http://nrckids.org/default/assets/File/StateRegs/WY/wy_chapter9.pdf.
- 72.Barreira DM, Ferreira MS, Fumian TM, Checon R, de Sadovsky AD, Leite JP, et al. Viral load and genotypes of noroviruses in symptomatic and asymptomatic children in southeastern Brazil. J Clin Virol. 2010;47:60–4. doi: 10.1016/j.jcv.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 73.Atmar RL, Opekun AR, Gilger MA, Estes MK, Crawford SE, Neill FH, et al. Determination of the 50% human infectious dose for Norwalk virus. J Infect Dis. 2014;209:1016–22. doi: 10.1093/infdis/jit620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cradock AL, O'Donnell EM, Benjamin SE, Walker E, Slining M. A review of state regulations to promote physical activity and safety on playgrounds in child care centers and family child care homes. J Phys Act Health. 2010;7(Suppl 1):S108–19. doi: 10.1123/jpah.7.s1.s108. [DOI] [PubMed] [Google Scholar]
- 75.Fischler GE, Fuls JL, Dail EW, Duran MH, Rodgers ND, Waggoner AL. Effect of hand wash agents on controlling the transmission of pathogenic bacteria from hands to food. J Food Prot. 2007;70:2873–7. doi: 10.4315/0362-028x-70.12.2873. [DOI] [PubMed] [Google Scholar]
- 76.Fuls JL, Rodgers ND, Fischler GE, Howard JM, Patel M, Weidner PL, et al. Alternative hand contamination technique to compare the activities of antimicrobial and nonantimicrobial soaps under different test conditions. Appl Environ Microbiol. 2008;74:3739–44. doi: 10.1128/AEM.02405-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jensen DA, Danyluk MD, Harris LJ, Schaffner DW. Quantifying the effect of hand wash duration, soap use, ground beef debris, and drying methods on the removal of Enterobacter aerogenes on hands. J Food Prot. 2015;78:685–90. doi: 10.4315/0362-028X.JFP-14-245. [DOI] [PubMed] [Google Scholar]
- 78.Macinga DR, Sattar SA, Jaykus LA, Arbogast JW. Improved inactivation of nonenveloped enteric viruses and their surrogates by a novel alcohol-based hand sanitizer. Appl Environ Microbiol. 2008;74:5047–52. doi: 10.1128/AEM.00487-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu P, Yuen Y, Hsiao HM, Jaykus LA, Moe C. Effectiveness of liquid soap and hand sanitizer against Norwalk virus on contaminated hands. Appl Environ Microbiol. 2010;76:394–9. doi: 10.1128/AEM.01729-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Park GW, Barclay L, Macinga D, Charbonneau D, Pettigrew CA, Vinjé J. Comparative efficacy of seven hand sanitizers against murine norovirus, feline calicivirus, and GII.4 norovirus. J Food Prot. 2010;73:2232–8. doi: 10.4315/0362-028x-73.12.2232. [DOI] [PubMed] [Google Scholar]
- 81.World Health Organization. Geneva: WHO Press; 2009. WHO guidelines on hand hygiene in health care: first global patient safety challenge: clean care is safe care. [PubMed] [Google Scholar]
- 82.Kampf G, Grotheer D, Steinmann J. Efficacy of three ethanol-based hand rubs against feline calicivirus, a surrogate virus for norovirus. J Hosp Infect. 2005;60:144–9. doi: 10.1016/j.jhin.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 83.Lages SL, Ramakrishnan MA, Goyal SM. In-vivo efficacy of hand sanitisers against feline calicivirus: a surrogate for norovirus. J Hosp Infect. 2008;68:159–63. doi: 10.1016/j.jhin.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 84.Tung G, Macinga D, Arbogast J, Jaykus LA. Efficacy of commonly used disinfectants for inactivation of human noroviruses and their surrogates. J Food Prot. 2013;76:1210–7. doi: 10.4315/0362-028X.JFP-12-532. [DOI] [PubMed] [Google Scholar]
- 85.Murata T, Katsushima N, Mizuta K, Muraki Y, Hongo S, Matsuzaki Y. Prolonged norovirus shedding in infants ≤6 months of age with gastroenteritis. Pediatr Infect Dis J. 2007;26:46–9. doi: 10.1097/01.inf.0000247102.04997.e0. [DOI] [PubMed] [Google Scholar]
- 86.Kirkwood CD, Streitberg R. Calicivirus shedding in children after recovery from diarrhoeal disease. J Clin Virol. 2008;43:346–8. doi: 10.1016/j.jcv.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 87.Barker J, Vipond IB, Bloomfield SF. Effects of cleaning and disinfection in reducing the spread of norovirus contamination via environmental surfaces. J Hosp Infect. 2004;58:42–9. doi: 10.1016/j.jhin.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 88.Park GW, Sobsey MD. Simultaneous comparison of murine norovirus, feline calicivirus, coliphage MS2, and GII.4 norovirus to evaluate the efficacy of sodium hypochlorite against human norovirus on a fecally soiled stainless steel surface. Foodborne Pathog Dis. 2011;8:1005–10. doi: 10.1089/fpd.2010.0782. [DOI] [PubMed] [Google Scholar]
- 89.Doultree JC, Druce JD, Birch CJ, Bowden DS, Marshall JA. Inactivation of feline calicivirus, a Norwalk virus surrogate. J Hosp Infect. 1999;41:51–7. doi: 10.1016/s0195-6701(99)90037-3. [DOI] [PubMed] [Google Scholar]
- 90.Gulati BR, Allwood PB, Hedberg CW, Goyal SM. Efficacy of commonly used disinfectants for the inactivation of calicivirus on strawberry, lettuce, and a food-contact surface. J Food Prot. 2001;64:1430–4. doi: 10.4315/0362-028x-64.9.1430. [DOI] [PubMed] [Google Scholar]
- 91.Jimenez L, Chiang M. Virucidal activity of a quaternary ammonium compound disinfectant against feline calicivirus: a surrogate for norovirus. Am J Infect Control. 2006;34:269–73. doi: 10.1016/j.ajic.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 92.Belliot G, Lavaux A, Souihel D, Agnello D, Pothier P. Use of murine norovirus as a surrogate to evaluate resistance of human norovirus to disinfectants. Appl Environ Microbiol. 2008;74:3315–8. doi: 10.1128/AEM.02148-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Girard M, Ngazoa S, Mattison K, Jean J. Attachment of noroviruses to stainless steel and their inactivation, using household disinfectants. J Food Prot. 2010;73:400–4. doi: 10.4315/0362-028x-73.2.400. [DOI] [PubMed] [Google Scholar]
- 94.Lin CM, Wu FM, Kim HK, Doyle MP, Michael BS, Williams LK. A comparison of hand washing techniques to remove Escherichia coli and caliciviruses under natural or artificial fingernails [published erratum appears in J Food Prot 2004;67] J Food Prot. 2003;66:2296–301. doi: 10.4315/0362-028x-66.12.2296. [DOI] [PubMed] [Google Scholar]
- 95.Jiang X, Dai X, Goldblatt S, Buescher C, Cusack TM, Matson DO, Pickering LK. Pathogen transmission in child care settings studied by using a cauliflower virus DNA as a surrogate marker. J Infect Dis. 1998;177:881–8. doi: 10.1086/515253. [DOI] [PubMed] [Google Scholar]


