Abstract
Objective
Many cardiovascular deaths can be avoided through primary prevention to address cardiovascular disease (CVD) risk factors or better access to quality medical care. In this cross-sectional study, we examined the relationship between four county-level health factors and rates of avoidable death from CVD during 2006–2010.
Methods
We defined avoidable deaths from CVD as deaths among U.S. residents younger than 75 years of age caused by the following underlying conditions, using International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes: ischemic heart disease (I20–I25), chronic rheumatic heart disease (I05–I09), hypertensive disease (I10–I15), or cerebrovascular disease (I60–I69). We stratified county-level death rates by race (non-Hispanic white or non-Hispanic black) and age-standardized them to the 2000 U.S. standard population. We used County Health Rankings data to rank county-level z scores corresponding to four health factors: health behavior, clinical care, social and economic factors, and physical environment. We used Poisson rate ratios (RRs) and 95% confidence intervals (CIs) to compare rates of avoidable death from CVD by health-factor quartile.
Results
In a comparison of worst-ranked and best-ranked counties, social and economic factors had the strongest association with rates of avoidable death per 100,000 population from CVD for the total population (RR=1.49; 95% CI 1.39, 1.60) and for each racial/ethnic group (non-Hispanic white: RR=1.37; 95% CI 1.29, 1.45; non-Hispanic black: RR=1.54; 95% CI 1.42, 1.67). Among the non-Hispanic white population, health behaviors had the next strongest association, followed by clinical care. Among the non-Hispanic black population, we observed a significant association with clinical care and physical environment in a comparison of worst-ranked and best-ranked counties.
Conclusion
Social and economic factors have the strongest association with rates of avoidable death from CVD by county, which reinforces the importance of social and economic interventions to address geographic disparities in avoidable deaths from CVD.
Avoidable death refers to deaths that could be prevented by improved public health interventions, improved medical care, or both.1–5 Studies of avoidable deaths have focused primarily on the geographic and temporal patterns of avoidable death from all causes.2,5–9 In addition, studies have reported on correlates of all-cause avoidable death rates, including community-level social, economic, and health-care characteristics.6,8,10,11 For example, studies have reported that increased health-care spending for primary care at the local level is associated with lower rates of avoidable death.3,9 One study that examined the association of several factors with avoidable death rates at the state level showed that a combination of social factors and health-care characteristics were associated with state-level variability in avoidable death rates.11
Cardiovascular disease (CVD) is the leading cause of death in the United States, and it places a huge burden on the U.S. health-care system.12,13 A U.S. study of geographic patterns of avoidable death from CVD published in 2013 reported that counties with the highest rates were concentrated primarily in the South Census Region and that non-Hispanic black people had higher rates than non-Hispanic white people.1 However, no studies have examined associations between county-level health factors and rates of avoidable death from CVD.
We examined the associations between county-level rates of avoidable death from CVD during 2006–2010 and four health factors (health behavior, clinical care, social and economic factors, and physical environment) as measured by the County Health Rankings (CHR), a publicly available county-level dataset that ranks counties on various health characteristics.14 Given the racial disparities in rates of avoidable death from CVD,1,2 we stratified the analysis by race.
METHODS
Avoidable deaths from CVD
The concept of avoidable mortality is described in previous studies1–5 and is used as a surveillance indicator15–17 to measure the number of deaths that are attributable to conditions caused by lack of primary prevention or medical care. Avoidable deaths from CVD are deaths that occur in patients younger than 75 years of age and are caused by coronary heart disease, hypertensive disease, rheumatic heart disease, or cerebrovascular disease.
We abstracted county-level death records from the National Vital Statistics System18 for 2006–2010. We obtained bridged-race19 July 1 intercensal population estimates for the years 2006–2009 and postcensal estimates for 2010 from the National Center for Health Statistics19 and the U.S. Census Bureau.20 We defined avoidable deaths from CVD as deaths that occurred from January 1, 2006, through December 31, 2010, in decedents younger than 75 years of age residing in a U.S. county from the following underlying causes, using International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes:21 ischemic heart disease (I20–I25), chronic rheumatic heart disease (I05–I09), hypertensive disease (I10–I15), or cerebrovascular disease (I60–I69). We categorized deaths for non-Hispanic black and non-Hispanic white people.1 We did not include other races or ethnicities because the number of avoidable deaths from CVD among other racial/ethnic groups was too few to categorize by county.
We calculated race-specific rates of avoidable death by county and age-standardized the rates to the 2000 U.S. standard population using the direct method. We used a local empirical Bayes algorithm22 to produce spatially smoothed rates. We suppressed rates in counties when we found the following: (1) <20 total avoidable deaths in the county of interest and its immediate neighbors, (2) <100 people in the county population, or (3) <6 avoidable deaths in each age group used for age standardization. After applying these criteria to the total population, seven counties were excluded from analysis. For analyses by race, 986 counties were excluded from analysis of the non-Hispanic black population, and 17 counties were excluded from analysis of the non-Hispanic white population.
County health factors
The CHR are produced annually by the University of Wisconsin Population Health Institute and the Robert Wood Johnson Foundation. The purpose of the CHR is to provide state and local organizations with a summary score for each county representing how that county ranks on various health factors in relation to other counties in the state.23 The CHR use various national data sources to rank counties, to allow a community to assess how its health profile compares with its neighbors' profiles, and to track progress over time.14,23,24 We chose the CHR because (1) they relate directly to the components of avoidable death from CVD (i.e., primary prevention and medical care), (2) they are selected carefully as direct or proxy measures of various aspects of a county's health environment,23,24 and (3) they are widely used by state and local health agencies to measure community health status.24–29 In addition to ranking overall health status, CHR also rank each county's status in four health-factor categories: health behavior, clinical care, social and economic factors, and physical environment. Individual variables are aggregated to create a health-factor summary score; all data sources used to generate the four health-factor categories and all variables are described on the CHR website.14 The data sources include national surveys such as the Behavioral Risk Factor Surveillance System. Data are also provided by national agencies and research institutions that routinely collect this information for surveillance purposes, such as the Centers for Disease Control and Prevention, U.S. Census Bureau, Dartmouth Atlas, National Center for Education Statistics, Bureau of Labor Statistics, Federal Bureau of Investigation, and Environmental Protection Agency. We used the 2010 cycle of the CHR data, which covers 2000–2008.
Although the CHR calculate county rankings for each health factor based on a weighted sum of z scores in each state, we wanted to make comparisons across all states. Therefore, we used CHR methodology to calculate weighted z scores and rankings based on all counties in the United States.14,23,30 We followed CHR methodology14,23,30 for counties that were missing data on an individual variable by giving the county the value of the state mean for that variable. The number of missing estimates for each variable varied, but for each health-factor category, no more than two variables (of ≥5 variables in each category) had more than 10% of data missing. We multiplied variables for which increases in percentages or rates correspond with favorable exposures (e.g., high school graduation rate or the percentage of ZIP codes with healthy food stores) by –1 before summing to allow for aggregation with variables for which increases in percentages or rates correspond with unfavorable exposures. We categorized county rankings for each health factor into quartiles from “best” (quartile 1) to “worst” (quartile 4).
Mapping
We mapped quintiles of spatially smoothed rates of avoidable death from CVD by county and mapped county health-factor quartiles to assess geographic distribution of health-factor rankings. We conducted all mapping using ArcMap version 10.1.31
Statistical analysis
We used generalized estimating equation Poisson regression models to evaluate the association between county health factors and rates of avoidable death from CVD. The models included the four health factors and a state term to adjust for correlated observations within states. These models estimated rate ratios (RRs) that compared rates of avoidable death between groups of counties according to rank, using the first quartile (best rankings) as the referent group. We included population counts as the offset term. We conducted all analyses using SAS® version 9.3.32
RESULTS
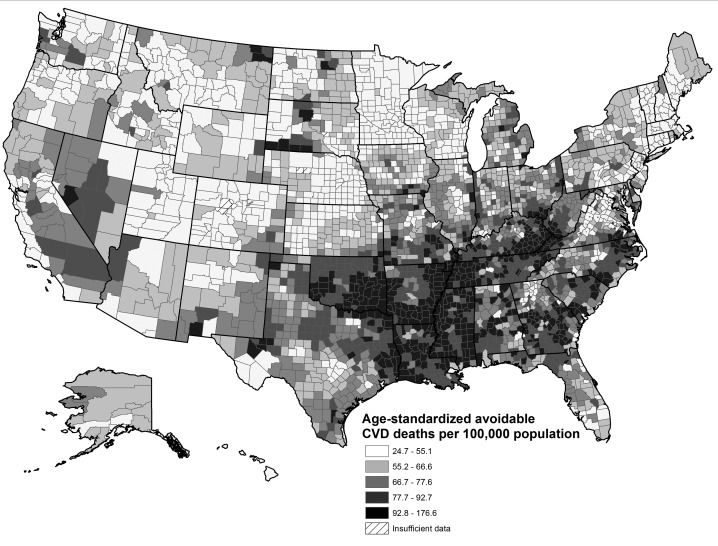
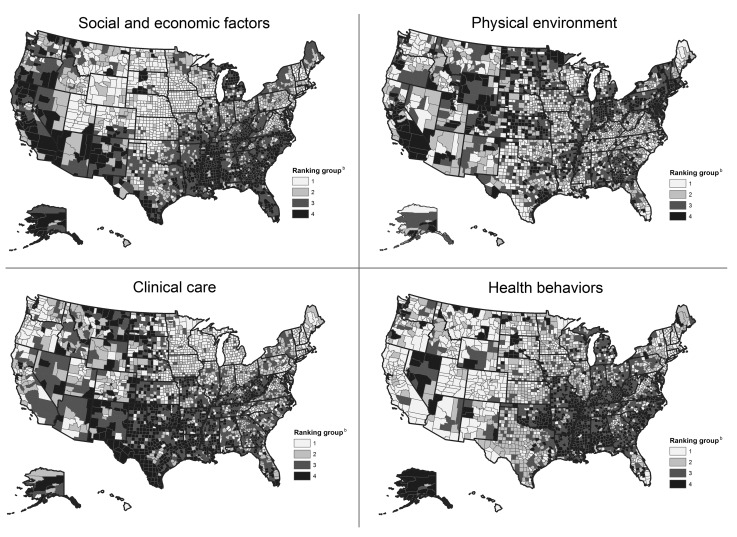
We found high rates of avoidable death from CVD throughout the central and eastern regions of the southern United States, particularly in Oklahoma, Arkansas, Tennessee, Mississippi, and Louisiana. We also found pockets of high-rate counties in parts of Texas, Missouri, North Dakota, South Dakota, and eastern Kentucky, and pockets of high rates of avoidable death from CVD in some regions of Georgia, South Carolina, and North Carolina (Figure 1). Health-factor quartiles had various geographic patterns (Figure 2). For health behaviors, the worst-ranked counties were concentrated primarily in southern states and in Nevada. Counties ranking worst in social and economic factors were found mostly in the Southeast and in the western states of Arizona, California, Nevada, New Mexico, and Oregon. Counties ranking worst in clinical care were found mostly in some southern and central parts of the United States. We found no clear geographic patterns by county for the ranking on physical environment, although pockets of low-ranking counties were located in the Northeast and California.
Figure 1.
Rates of avoidable deatha from cardiovascular disease, by county,b United States, 2006–2010
aAvoidable deaths from CVD were defined by underlying causes using International Classification of Diseases, 10th Revision, Clinical Modification codes of ischemic heart disease (I20–25), chronic rheumatic heart disease (I05–09), hypertensive disease (I10–15), or cerebrovascular disease (I60–69) in decedents younger than 75 years of age residing in the United States.
bSource: National Center for Health Statistics (US). National Vital Statistics System [cited 2016 Feb 19]. Available from: http://www.cdc.gov/nchs/nvss.htm
CVD = cardiovascular disease
Figure 2.
County Health Rankings groups,a by health factor, United States, 2000–2008
aSource: Robert Wood Johnson Foundation. County Health Rankings & Roadmaps, 2010 cycle [cited 2016 Feb 23]. Available from: http://www.countyhealthrankings.org
bCounties are ranked from best (1) to worst (4) for the four health factors.
The variables used to rank counties on each health factor differed in distribution and range (Table 1). For health behaviors, clinical care, and social and economic factors, rates of avoidable death from CVD generally increased from best quartile to worst quartile among the total population and among the non-Hispanic black and non-Hispanic white populations (Table 2).
Table 1.
County-level distribution (n=3,140 counties) of variables used to generate each county health factor in the County Health Rankings, United States, 2000–2008a
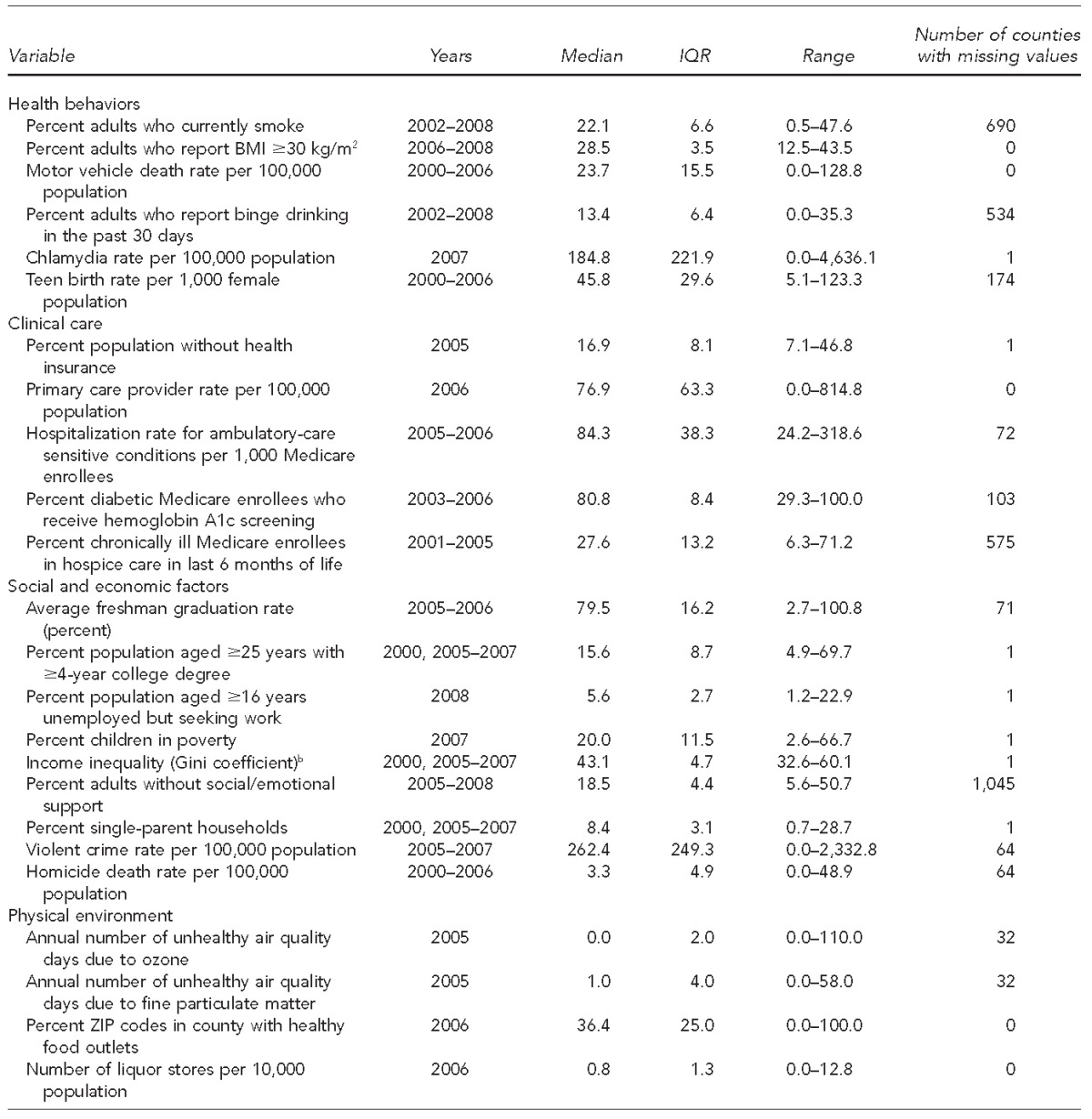
Source: Robert Wood Johnson Foundation. County Health Rankings & Roadmaps [cited 2016 Feb 23]. Available from: http://www.countyhealthrankings.org
bThe Gini coefficient of income inequality represents the inequitable distribution of income in a community by household, and can range from 0 to 1. The County Health Rankings multiplies the Gini coefficient by 100, so that the values can range from 0 to 100. A value of 100 indicates that all income in a county is concentrated in one household, while a coefficient of 0 indicates a completely equal distribution of income among households.
IQR = interquartile range
BMI = body mass index
kg/m2 = kilogram per square meter
Table 2.
Age-standardized rates of avoidable deaths caused by cardiovascular disease, by race and county health-factor quartile, United States, 2006–2010a
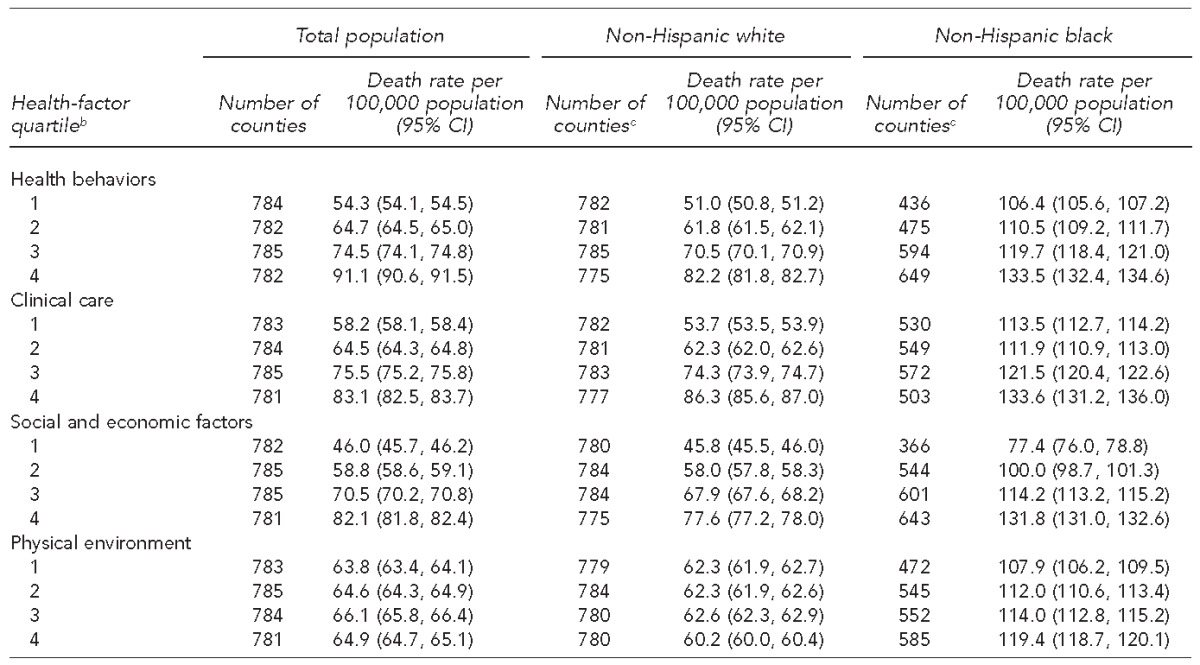
Sources: Robert Wood Johnson Foundation. County Health Rankings & Roadmaps [cited 2016 Feb 23]. Available from: http://www.countyhealthrankings.org; National Center for Health Statistics (US). National Vital Statistics System [cited 2016 Feb 19]. Available from: http://www.cdc.gov/nchs/nvss.htm
bHealth-factor quartile groups range from best (1) to worst (4) health-factor ranking.
cThe number of counties that were suppressed because of unstable rates varied by race for two reasons: (1) data on avoidable cardiovascular disease death rates considered unstable were suppressed and (2) health-factor quartile groupings were based on total population distribution.
CI = confidence interval
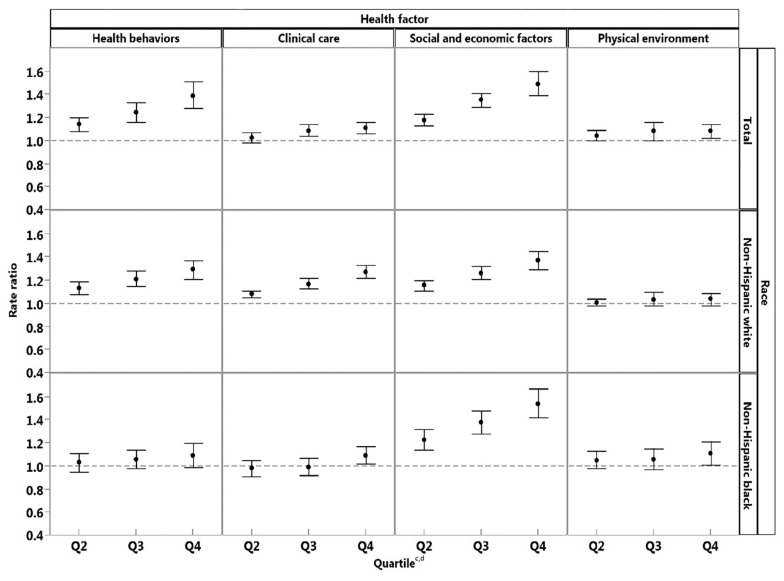
Rates increased slightly among the non-Hispanic black population from best quartile to worst quartile for physical environment factors. RRs increased substantially from the second quartile to the fourth (worst) quartile for health behaviors, clinical care, and social and economic factors among the total population. We found associations mostly when we compared worst-ranked counties with best-ranked counties in each health-factor category. Among the total population, the highest RRs for avoidable death from CVD were observed for social and economic factors (RR=1.49; 95% confidence interval [CI] 1.39, 1.60), followed by health behaviors (RR=1.39; 95% CI 1.28, 1.51), clinical care (RR=1.11; 95% CI 1.06, 1.16), and physical environment (RR=1.08; 95% CI 1.02, 1.14). Among the non-Hispanic white population, the highest RRs were observed for social and economic factors (RR=1.37; 95% CI 1.29, 1.45), health behaviors (RR=1.29; 95% CI 1.21, 1.37), and clinical care (RR=1.27; 95% CI 1.22, 1.33). The RRs for physical environment were not significant. Among the non-Hispanic black population, we found significant RRs for social and economic factors (RR=1.54; 95% CI 1.42, 1.67), physical environment (RR=1.11; 95% CI 1.01, 1.21), and clinical care (RR=1.09; 95% CI 1.02, 1.17). We found no association between health behavior rankings and avoidable CVD death rates among the non-Hispanic black population (Figure 3).
Figure 3.
Adjusted rate ratiosa of age-standardized avoidable cardiovascular disease death rates, by county health factor, United States,b 2006–2010
aRate ratios compare death rates from counties in the second-, third-, and fourth-ranking quartiles with the first-ranking quartile (the reference group) for each health factor. The rate ratio of each health-factor group is adjusted for the remaining three health factors.
bSources: Robert Wood Johnson Foundation. County Health Rankings & Roadmaps, 2010 cycle [cited 2016 Feb 23]. Available from: http://www.countyhealthrankings.org; National Center for Health Statistics (US). National Vital Statistics System, 2006–2010 [cited 2016 Feb 19]. Available from: http://www.cdc.gov/nchs/nvss.htm
cQuartiles reflect best (Q1, reference group, not shown) to worst (Q4) health-factor ranking.
dError bars represent 95% confidence intervals.
The strength of the association differed by race, particularly for health behavior and clinical care. Among the non-Hispanic white population, RRs gradually increased with worsening rank in health behavior, clinical care, and social and economic health-factor categories. Counties ranked in the second, third, and fourth quartiles in each health-factor category had higher rates of avoidable death from CVD than did counties in the first quartile. This dose–response pattern between health-factor rankings and rates of avoidable death from CVD was observed only among the non-Hispanic black population for social and economic factors. Among the non-Hispanic black population, only counties in the fourth quartile for clinical care and physical environment had substantially higher rates of avoidable death from CVD than counties in the first quartile, and the magnitude of the RRs was low. We found no association between health behavior rankings and rates of avoidable death from CVD among the non-Hispanic black population (Figure 3).
DISCUSSION
We found that three of the four county health-factor rankings (health behavior, clinical care, and social and economic factors) were associated with county-level rates of avoidable death from CVD for the total population; therefore, counties in the second, third, and fourth quartiles (i.e., those with the worst health-factor scores) had higher rates of avoidable death from CVD than counties in the first quartile (i.e., those with the best health-factor scores). The strongest associations with rates of avoidable death from CVD were observed for social and economic factors, followed by health behavior and clinical care factors. The physical environment factor showed a significant association only when we compared the fourth and first quartile; the RR observed was low in magnitude. Among the non-Hispanic white population, the association between county health factors and rates of avoidable death from CVD was similar to that of the total population. However, among the non-Hispanic black population, only social and economic factors showed a strong association with rates of avoidable death from CVD; no association was observed between health behaviors and rates of avoidable death from CVD. Only in a comparison of the fourth and first quartiles were significant associations observed for clinical care and physical environment among the non-Hispanic black population, and the RRs were low in magnitude.
Social and economic factors consistently showed the strongest association with rates of avoidable death from CVD among the total population, the non-Hispanic black population, and the non-Hispanic white population. Social and economic factors include -characteristics such as educational attainment, percentage of children living below the federal poverty level, unemployment rates, and violent crime rates. Our findings are consistent with those of several studies that examined local characteristics in association with avoidable deaths from all causes. For example, in a U.S. study that examined the association of county-level characteristics with changes in rates of avoidable death from 1999 to 2006, having a higher proportion of college graduates in the county was associated with lower rates of avoidable death.8 Similarly, another study found that state-level social factors, such as the percentage of the population living below the federal poverty level and the percentage of the population that was non-Hispanic black, demonstrated strong positive associations with rates of avoidable death; moreover, when they were accounted for in a multivariate model, these factors diminished the magnitude of the association between avoidable death and health-care indicators, such as the rate of preventable hospitalization and the percentage of the population that was uninsured.11 Living in environments characterized by low educational attainment, economic instability, and poor access to health care, healthy foods, or safe physical environments is associated with poor cardiovascular health.33,34 Lack of educational and economic resources is associated with unhealthy lifestyle behaviors, such as having a poor diet, smoking cigarettes, and being physically inactive—all risk factors for CVD.35 Social and economic deprivation may also limit access to physical resources such as healthy foods. For example, neighborhoods that have a high percentage of low-income residents typically have fewer full-service supermarkets.36 Finally, chronic exposure to stress from living in these deprived environments can alter biological processes (e.g., allostatic load or physiological wear-and-tear that results from chronic stress) and over time lead to adverse cardiovascular outcomes.34,37 Thus, lack of social and economic opportunity may shape or limit certain health behaviors.
Our findings support the need to increase healthy behaviors and access to quality health care. These -factors could be improved by reducing the prevalence of smoking and unhealthy weight, increasing the percentage of the population with health insurance, increasing the number of primary care physicians per 1,000 population, and decreasing rates of preventable hospitalizations. Similarly, access to timely and effective medical care is an important contributor to reducing rates of avoidable death from CVD. In a study that compared the health systems of the United States and United Kingdom, the authors proposed that increasing the proportion of U.S. adults who receive regular primary care in the United States would reduce the number of unnecessary hospital admissions and improve overall health outcomes among adults younger than 65 years of age.5 Our findings also suggest that clinical care factors may not be as strongly associated with avoidable heart disease death rates among the non-Hispanic black population. The difference in the magnitude of association could reflect the presence of disparities between non-Hispanic black and non-Hispanic white populations in access to or quality of care.38
We did not find an association between the physical environment and rates of avoidable death from CVD among the non-Hispanic white population; we found an association among the total -population and the non-Hispanic black population only when we compared the worst quartile with the best quartile. This observation could signify that the indicators used in 2010 by the CHR to rank the physical environment do not capture all of the physical environment elements that are pertinent to CVD health.39 For example, the indicators included in the physical environment factor are the annual number of unhealthy air quality days due to ozone and fine particulate matter, the percentage of ZIP codes in the county with healthy food outlets, and the number of liquor stores per 10,000 population. These indicators, although important, may not fully account for all pertinent environmental elements, such as housing conditions, safe places for physical activity, and access to smoke-free public places.
The associations between county health factors and rates of avoidable death from CVD were maintained regardless of county racial composition. We repeated the analysis controlling for percentage non-Hispanic black population and found similar results in the total population and among the non-Hispanic black and non-Hispanic white populations. The results among the non-Hispanic white population were also maintained even after limiting the analysis to counties with a predominantly non-Hispanic white population (≥90%). This finding supports the conclusion that the association between health factors and rates of avoidable death from CVD is not a function of the higher percentages of non-Hispanic black people (who have higher overall rates of avoidable death from CVD) living in those counties.
Limitations
The strength of association between county health factors and rates of avoidable death from CVD could have differed by race because the CHR comprise non-race–specific measures. County health-factor data are provided for a county's entire population, not for each race/ethnicity; therefore, both the non-Hispanic white and non-Hispanic black populations are assigned the same value, regardless of any disparities between the two groups in a county. This drawback potentially limited the study's ability to identify county-level associations between health factors and race-specific rates of avoidable death from CVD, especially in communities where disparities exist and the racial group with the less desirable health factor comprises a small percentage of the county's population. For example, previous studies documented differences by race in the proportion of the population that is uninsured—a variable that is included in the clinical care factor ranking—and these differences can account for access to quality health care that can affect health outcomes.40,41 Because we were unable to identify variables such as racial/ethnic disparities in insurance coverage in CHR data, we were unable to examine the relationship between these disparities and rates of avoidable death from CVD.
This study had three additional limitations. First, the cross-sectional design did not allow for examination of the association between health factors and avoidable death risk across the lifespan. We assumed that (1) populations living in these counties lived in these counties for long periods of time, (2) each county's health-factor rankings were stable, and (3) the time frame was long enough to observe the influence of individual metrics on population death rates. Nonetheless, some indicators may affect rates of avoidable death from CVD during a relatively short time frame; one study showed that increases in public health spending can be associated with reductions in rates of avoidable death within a similar number of years as our study.9 Second, some metrics included in the CHR were based on estimates that had significant statistical variance and missing values. However, the variables with >10% missing values represented a small proportion of all the variables used to create each health-factor ranking and likely had little influence on the overall associations we observed. The use of multiple variables aggregated in each health-factor category also improved the reliability of the rankings.23 Third, because CHR data are at the county level, the results can be interpreted only at the county level and do not reflect individual-level associations; however, these results are important for understanding factors that may be beneficial for understanding and addressing population-based policies or programs to reduce geographic disparities in rates of avoidable death from CVD.
Strengths
This study also had several strengths. It examined commonly used indices of county-level contextual variables to help determine factors that could have the greatest impact on reducing geographic disparities in rates of avoidable death from CVD. Health factors developed by the CHR standardize and summarize multiple variables that are commonly analyzed individually. The use of the CHR allowed the variables to be integrated into four summary metrics that characterize various aspects of community health (health behavior, clinical care, social and economic factors, and physical environment). In addition, we calculated the rankings on the basis of the entire distribution of counties, which allowed us to compare ranking across states instead of comparing only rankings within each state. Finally, our modeling approach also accounted for potentially correlated observations within each state.
CONCLUSION
Our findings support the recommendations of the Framework for Public Health Action, a five-tier pyramid depicting the impact of various types of public health interventions. The framework emphasizes that interventions aimed at improving the social determinants of health have the greatest potential to improve health outcomes.42 Our findings support the need for prevention strategies that recognize the importance of a multipronged approach to reducing avoidable CVD deaths, with an emphasis on the role of underlying social and economic conditions.
Footnotes
The authors acknowledge Tiffany Chang, MPH, for her assistance with map creation. The findings and conclusions of this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Institutional review board approval was not necessary because secondary data were used for this analysis.
REFERENCES
- 1.Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61:2249–52. doi: 10.1016/j.jacc.2013.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macinko J, Elo IT. Black-white differences in avoidable mortality in the USA, 1980–2005. J Epidemiol Community Health. 2009;63:715–21. doi: 10.1136/jech.2008.081141. [DOI] [PubMed] [Google Scholar]
- 3.Heijink R, Koolman X, Westert GP. Spending more money, saving more lives? The relationship between avoidable mortality and healthcare spending in 14 countries. Eur J Health Econ. 2013;14:527–38. doi: 10.1007/s10198-012-0398-3. [DOI] [PubMed] [Google Scholar]
- 4.James PD, Wilkins R, Detsky AS, Tugwell P, Manuel DG. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J Epidemiol Community Health. 2007;61:287–96. doi: 10.1136/jech.2006.047092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nolte E, McKee CM. In amenable mortality—deaths avoidable through health care—progress in the US lags that of three European countries. Health Aff (Millwood) 2012;31:2114–22. doi: 10.1377/hlthaff.2011.0851. [DOI] [PubMed] [Google Scholar]
- 6.Cheng ER, Kindig DA. Disparities in premature mortality between high- and low-income US counties. Prev Chronic Dis. 2012;9:E75. [PMC free article] [PubMed] [Google Scholar]
- 7.Elo IT, Beltran-Sanchez H, Macinko J. The contribution of health care and other interventions to black-white disparities in life expectancy, 1980–2007. Popul Res Policy Rev. 2014;33:97–126. doi: 10.1007/s11113-013-9309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kindig DA, Cheng ER. Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood) 2013;32:451–8. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- 9.Mays GP, Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Aff (Millwood) 2011;30:1585–93. doi: 10.1377/hlthaff.2011.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ronzio CR, Pamuk E, Squires GD. The politics of preventable deaths: local spending, income inequality, and premature mortality in US cities. J Epidemiol Community Health. 2004;58:175–9. doi: 10.1136/jech.2003.008672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoenbaum SC, Schoen C, Nicholson JL, Cantor JC. Mortality amenable to health care in the United States: the roles of demographics and health systems performance. J Public Health Policy. 2011;32:407–29. doi: 10.1057/jphp.2011.42. [DOI] [PubMed] [Google Scholar]
- 12.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heron M. Deaths: leading causes for 2010. Natl Vital Stat Rep. 2013 Dec 20;62:1–96. [PubMed] [Google Scholar]
- 14.Robert Wood Johnson Foundation. County health rankings & roadmaps [cited 2016 Feb 23] Available from: http://www.countyhealthrankings.org.
- 15.Canadian Institute for Health Information (CA) Ottawa (ON): Canadian Institute for Health Information; 2014. Health indicators 2013. Also available from: https://secure.cihi.ca/free_products/HI2013_Jan30_EN.pdf [cited 2016 Feb 23] [Google Scholar]
- 16.Office for National Statistics (UK) Newport, Wales (UK): Office for National Statistics; 2015. Avoidable mortality in England and Wales, 2013. Also available from: http://www.ons.gov.uk/ons/dcp171778_404337.pdf [cited 2016 Feb 23] [Google Scholar]
- 17.Rotterdam (NL): AMIEHS; 2011. Avoidable mortality in the European Union: towards better indicators for the effectiveness of health systems (AMIEHS) Also available from: http://amiehs.lshtm.ac.uk/publications/reports/amiehs%20final%20report%20vol%20i.pdf [cited 2016 Feb 23] [Google Scholar]
- 18.National Center for Health Statistics (US) National Vital Statistics System [cited 2016 Feb 19] Available from: http://www.cdc.gov/nchs/nvss.htm.
- 19.National Center for Health Statistics (US) U.S. census populations with bridged race categories. Updated 2015 Jun 30 [cited 2015 Oct 26] Available from: http://www.cdc.gov/nchs/nvss/bridged_race.htm.
- 20.Census Bureau (UYS) 2010 population estimates [cited 2016 Feb 19] Available from: https://www.census.gov/popest/data/datasets.html.
- 21.Centers for Medicare & Medicaid Services (US) International classification of diseases, tenth revision, clinical modification. 2015 [cited 2016 Feb 23] Available from: https://www.cms.gov/Medicare/Coding/ICD10/index.html.
- 22.Marshall RJ. Mapping disease and mortality rates using empirical Bayes estimators. J R Stat Soc Ser C Appl Stat. 1991;40:283–94. [PubMed] [Google Scholar]
- 23.Remington PL, Catlin BB, Gennuso KP. The County Health Rankings: rationale and methods. Popul Health Metr. 2015;13:11. doi: 10.1186/s12963-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peppard PE, Kindig DA, Dranger E, Jovaag A, Remington PL. Ranking community health status to stimulate discussion of local public health issues: the Wisconsin County Health Rankings. Am J Public Health. 2008;98:209–12. doi: 10.2105/AJPH.2006.092981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nayar P, Yu F, Apenteng BA. Frontier America's health system challenges and population health outcomes. J Rural Health. 2013;29:258–65. doi: 10.1111/j.1748-0361.2012.00451.x. [DOI] [PubMed] [Google Scholar]
- 26.Rappold AG, Cascio WE, Kilaru VJ, Stone SL, Neas LM, Devlin RB, et al. Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ Health. 2012;11:71. doi: 10.1186/1476-069X-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rohan AM, Booske BC, Remington PL. Using the Wisconsin County Health Rankings to catalyze community health improvement. J Public Health Manag Pract. 2009;15:24–32. doi: 10.1097/PHH.0b013e3181903bf8. [DOI] [PubMed] [Google Scholar]
- 28.Wagner SE, Hurley DM, Hebert JR, McNamara C, Bayakly AR, Vena JE. Cancer mortality-to-incidence ratios in Georgia: describing racial cancer disparities and potential geographic determinants. Cancer. 2012;118:4032–45. doi: 10.1002/cncr.26728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yeager VA, Menachemi N, Ginter PM, Sen BP, Savage GT, Beitsch LM. Environmental factors and quality improvement in county and local health departments. J Public Health Manag Pract. 2013;19:240–9. doi: 10.1097/PHH.0b013e31825f74b2. [DOI] [PubMed] [Google Scholar]
- 30.Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Madison (WI): University of Wisconsin, Population Health Institute; 2010. County Health Rankings working paper: different perspectives for assigning weights to determinants of health. [Google Scholar]
- 31.Environmental Systems Research Institute. Redlands (CA): ESRI; 2011. ArcMap: Version 10.1. [Google Scholar]
- 32.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2012. SAS®: Version 9.3. [Google Scholar]
- 33.Diez Roux A. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–89. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24:325–34. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 35.Kilander L, Berglund L, Boberg M, Vessby B, Lithell H. Education, lifestyle factors and mortality from cardiovascular disease and cancer. A 25-year follow-up of Swedish 50-year-old men. Int J Epidemiol. 2001;30:1119–26. doi: 10.1093/ije/30.5.1119. [DOI] [PubMed] [Google Scholar]
- 36.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95:660–7. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 38.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3 Pt 2):1278–99. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hendryx M, Ahern MM, Zullig KJ. Improving the environmental quality component of the County Health Rankings model. Am J Public Health. 2013;103:727–32. doi: 10.2105/AJPH.2012.301016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menlo Park (CA): Henry J. Kaiser Family Foundation; 2013. Health coverage by race and ethnicity: the potential impact of the Affordable Care Act. [Google Scholar]
- 41.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff (Millwood) 2005;24:398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 42.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]