Abstract
Background
Despite the ever increasing popularity of labial and clitoral surgeries, the best practices and long term effects of reconstructive procedures in these regions remain unknown. This is particularly noteworthy since the presentation of nerve related symptoms may be delayed up to a year. Despite the convention that these surgical procedures are low risk, little is known about the best practices that may reduce the postoperative complications as a result of these reconstructive surgeries. We describe a preoperative sensory mapping technique in the context of a symptomatic inclusion cyst in the clitoral region. This technique delineates anatomical and functional regions innervated by the dorsal clitoral nerve while avoiding the vascular watershed area in the midline.
Case
A prototypical case of a patient with a clitoral mass will be discussed with clinical history and surgical approach. Prior to surgical excision, the dorsal clitoral nerve distribution was mapped in order to avoid a surgical incision in this sensual zone.
Conclusions
In our practice, preoperative sensory mapping is a clinically useful planning tool that requires minimal instrumentation and no additional operating time. Sensory mapping allows identification of the functional zone innervated by the dorsal clitoral nerve so that it can be avoided.
Keywords: clitoral mass, labial surgery, dorsal clitoral nerve, sensory preservation
Introduction
Labial surgery is becoming an increasingly popular procedure in the field of plastic and reconstructive surgery.1 However, little is known about the functional implications of postoperative scarring and sensory loss after these surgeries. The few studies in the gynecological literature show that not only is there a differential innervation between the introital and external labia minora, but also that receptor density is much more condensed in the glans clitoris compared to the glans penis.2,3 Therefore, it makes sense to preserve important sensory areas during surgery. Preoperative sensory mapping of the labia and clitoral hood may prevent nociceptive injury, particularly in regions important in arousal pathways. We utilized a previously described preoperative sensory mapping technique to determine the safe zones for resection of benign cysts in the clitoral region.4 We have found this to be a useful planning tool during complex reconstructive surgeries involving genitalia.4. We demonstrated the utility and application of this minimally invasive, nerve sparing technique in a patient who underwent surgical resection of a clitoral mass.
Case Presentation
A 27-year-old female presented with a progressively enlarging clitoral mass over 18 months. She reported mild erythema surrounding the mass with cyclical increases in size during menses and increasingly limited clitoral stimulation and discomfort. Her medical history was significant for a clitoral laceration during consensual intercourse that required suturing 5 years prior. Pelvic examination revealed distention of the clitoral hood as well as fusion of the superior labia majora and minora that was deemed to be an anatomical variant. (Figure 1) The mass measured 3.0 × 2.0 cm and was mildly erythematous, non-tender, soft, and mobile; the remainder of the exam was otherwise unremarkable.
Figure 1.
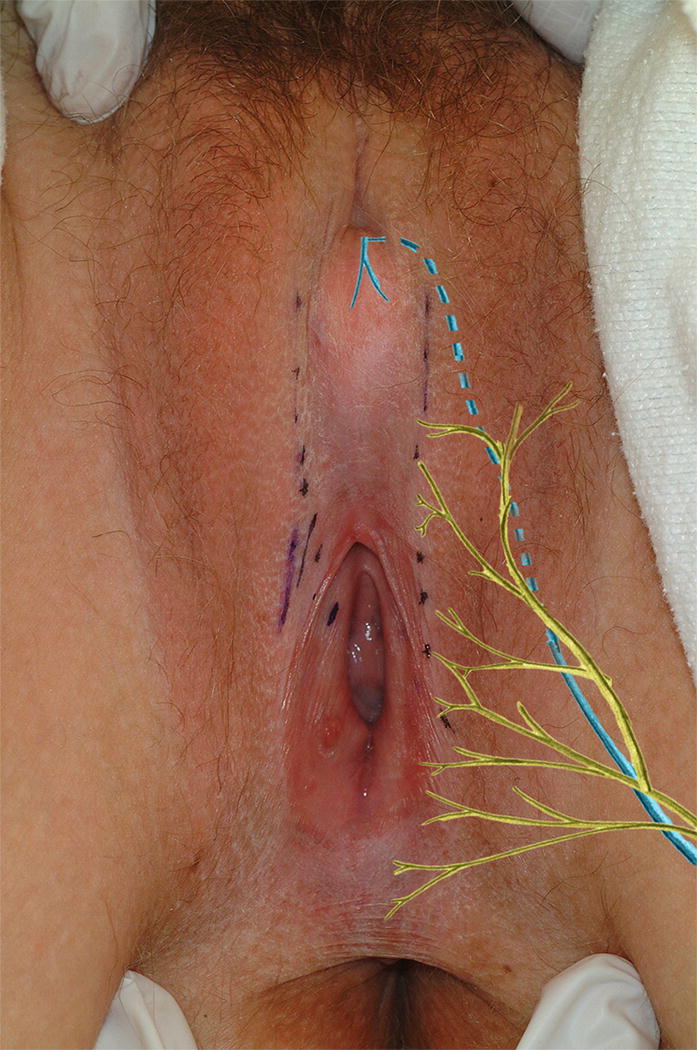
Initial appearance of the clitoral mass with superimposed sensory innervation. Branches of the pudendal nerve: dorsal clitoral nerve (dotted blue line) and perineal nerve (solid yellow lines).
She was taken to the operative suite, where sensory mapping was performed prior to induction of anesthesia. The sensory mapping determined the anatomical region associated with sensual response. As described by Wagner et al., a lubricated cotton swab was used to stroke the clitoral hood and the medial aspect of the labia minora in a radial fashion (from the urethra outward).4 With each stroke, the patient was asked to indicate if she experienced a sensation that was “sensual” versus “neutral.” This simple distinction allowed for the identification of the functional zone of clitoral sensation, which is primarily innervated by the dorsal clitoral nerve; the non-sensual perception of the remainder of the labia and mucocutanous junction is primarily innervated by the perineal nerve. The borders were marked and a vertical incision was made at the lateral margin of the mass, which corresponded to her non-sensual region. (Figure 2) In our experience, in the vast majority of cases, the non-sensual zone is at the hairline bearing the labia majora skin, in close proximity to the clitoris.
Figure 2.

Preoperative (Left) and Postoperative (Right). The area between the dotted lines correlates to the area of sensual response. The incision was made just lateral to the dotted line on the left side.
The clitoral region was then infiltrated with injectable saline in order to hydrodissect the tissue planes, thus facilitating better visualization of this anatomically condensed region.5 The incision was taken down to the cyst capsule using bipolar cautery. Then, the tissue was undermined circumferentially with a combination of blunt and sharp dissection. The posterior wall of the mass was found to be densely adherent to the clitoral bundle. With careful dissection, the cyst was mobilized from the underlying clitoral nerve bundle. The cyst was removed intact, without compromising the clitoral nerve bundle or hood, and the incision was then closed with interrupted 4.0 Vicryl in multiple layers. (Figure 2) The pathology revealed an intact epidural inclusion cyst, measuring 2.8 × 1.8 × 1.0 cm. (Figure 3) At the patient’s eight-week postoperative evaluation, she had no residual symptoms and had resumed pain-free sexual intercourse. At 6 months, the patient noted a complete return to her baseline sexual function.
Figure 3.

Clitoral mass. Pathology revealed an intact inclusion cyst measuring 2.8 × 1.8 × 1.0 cm.
Discussion
Decreased sexual function has also been reported in association with surgical procedures of the vulva, notably labial and vulvectomy procedures. As gynecologic reconstructive and cosmetic procedures gain increasing popularity, complications such as dyspareunia, scarring, and wound healing problems may also arise. According to the ASAPS (American Society for Aesthetic Plastic Surgery) National Data Bank statistics for 2014, there was a 48.6% increase in “vaginal rejuvenation” procedures from 2013 to 2014.1 Due to the increase in these elective cosmetic procedures, the role of the surface structures (e.g. labia) of the female sexual response are being re-explored. In fact, the labia minora may have a larger role in female sexual response than previously understood. Histological examination has identified the labia minora as specialized, sexually responsive, highly vascular, folds of tissue with an abundance of neural elements.6 In addition, Schober et. al. showed a higher receptor density on the introital border compared to the external border of the labia minora.2 Shih et. al. has shown receptor density is much more condensed in the glans clitoris compared to the glans penis.3 This highlights the need for careful preoperative assessment of the neural anatomy that makes understanding the complicated nature of the female sexual response vital for the surgeon.
Understanding the neuroanatomy is important for preoperative surgical planning and in order to avoid postoperative nociceptive injury. The dorsal clitoral nerve is a terminal branch of the pudendal nerve. The pudendal nerve gives rise to the clitoral neurovascular bundle from the bilateral pelvic sidewalls as it travels beneath the ischiopubic rami towards the suspensory ligament. With respect to the suspensory ligament, the nerve innervates at the 1 o’clock and 11 o’clock positions, and it ultimately terminates within the glans of the clitoral body via attachment at the public symphysis. The perineal nerve innervates the remainder of the labia majora and minora.7,8 Therefore, knowledge of clitoral and labial innervation can greatly aid in preoperative sensory mapping.
The application of sensory nerve mapping prior to surgical resection of a clitoral mass or reconstructive procedures may prevent compromising sensory function of the area. The surgeon can also avoid unnecessary dissection of the labia minora. The typical midline incision risks disruption of the densely innervated clitoris and the labia minora. The sensory mapping technique leads to a lateral approach, minimizing this risk. Based on our experience to date, in most instances, the safe zone falls at the junction of the labia majora and minora (the “inter-labial sulcus”), which is generally immediately before the transition to hairy skin. Given the superficial and central location of this patient’s clitoral mass, the surgeon is tempted to make a midline incision; however, this can be dangerous since the incision will fall in the central distribution of the clitoral sensation. Furthermore, a midline incision falls within the water shed area for blood supply and may cause delayed healing and scar formation. Given the condensed neuroanatomy of this region, we routinely use saline hydrodissection to facilitate dissection between fascial planes. The concept of preoperative sensory mapping has applications not only in labial surgery, but in other female external genitalia surgeries as well.
This case highlights the importance of preoperative assessment using a sensory mapping technique in order to distinguish areas innervated by the dorsal clitoral nerve that are important for arousal. The technique we propose is simple to use and cost-effective. In other instances of clitoral cyst removal, magnetic resonance imaging is used to identify the location of a patient’s neurovascular structures with relation to the cyst. This imaging technique can be cost prohibitive, especially since many individuals requiring surgery to excise clitoral cysts are victims of Female Genital Mutilation and may have limited access to healthcare resources.9,10 Nevertheless, knowledge of clitoral and labial neurovascular anatomy may decrease the risk of nerve injury and improve postoperative outcomes. Future studies comparing immediate and longer term functional outcomes of reconstructive and cosmetic surgeries are needed in order to better understand the clinical implications of nerve sparing techniques in gynecological procedures.
Conclusion
Preoperative sensory mapping is a clinically useful planning tool that requires minimal instrumentation and no additional operating time. Sensory mapping identifies critical sensory arousal regions innervated by the dorsal clitoral nerve. Avoiding incision in this functional zone may prevent long term postoperative functional complications.
Acknowledgments
Conflicts of Interest and Sources of Funding: This report is independent research supported, in part by the National Institute of Health (P01 NS045685, Zolnoun)
References
- 1.Cosmetic surgery national data bank statistics. Aesthet Surg J. 2014;34(Suppl 1):1–20. doi: 10.1093/asj/34.Supplement_1.1. [DOI] [PubMed] [Google Scholar]
- 2.Schober J, Cooney T, Pfaff D, et al. Innervation of the labia minora of prepubertal girls. J Pediatr Adolesc Gynecol. 2010;23(6):352–357. doi: 10.1016/j.jpag.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Shih C, Cold CJ, Yang CC. Cutaneous corpuscular receptors of the human glans clitoris: descriptive characteristics and comparison with the glans penis. J Sex Med. 2013;10(7):1783–1789. doi: 10.1111/jsm.12191. [DOI] [PubMed] [Google Scholar]
- 4.Wagner IJ, Damitz LA, Carey E, Zolnoun D. Bilateral accessory breast tissue of the vulva: a case report introducing a novel labiaplasty technique. Ann Plastic Surg. 2013;70(5):549–552. doi: 10.1097/SAP.0b013e31827ead39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malone DG, Clark TB, Wei N. Ultrasound-guided percutaneous injection, hydrodissection, and fenestration for carpal tunnel syndrome: description of a new technique. Journal of Applied Research. 2011;11(1):1. [Google Scholar]
- 6.Ginger VA, Cold CJ, Yang CC. Structure and innervation of the labia minora: more than minor skin folds. Female pelvic medicine & reconstructive surgery. 2011;17(4):180–183. doi: 10.1097/SPV.0b013e318221f835. [DOI] [PubMed] [Google Scholar]
- 7.Pauls RN. Anatomy of the clitoris and the female sexual response. Clin Anat. 2015;28(3):376–384. doi: 10.1002/ca.22524. [DOI] [PubMed] [Google Scholar]
- 8.Furtenmuller G, McKenna C, Ebmer J, et al. Pudenal Nerve 3-Dimensional Illustration Gives Insight Intro Surgical Approaches. Ann Plastic Surg. 2013 doi: 10.1097/SAP.0000000000000169. [DOI] [PubMed] [Google Scholar]
- 9.Johnson LT, Lara-Torre E, Murchison A, et al. Large Epidermal Cyst of the Clitoris: A Novel Diagnostic Approach to Assist in Surgical Removal. Journal of Pediatric and Adolescent Gynecology. 2013;26(2):e33–e35. doi: 10.1016/j.jpag.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Rouzi AA, Alturki F. Female genital mutilation/cutting: an update. Clinical and experimental obstetrics & gynecology. 2015;42(3):300–303. [PubMed] [Google Scholar]


