Abstract
Background
An unnecessary Caesarean section (CS) can cause increased maternal and perinatal morbidity and other adverse short- and long-term outcomes. However, countries worldwide have witnessed an increasing trend toward the use of CS. Our objectives were to explore the influencing factors associated with the mode of birth among childbearing women in Hunan Province and to provide evidence and suggestions for the improvement and further understanding of vaginal birth (VB) in China.
Methods
A total of 977 childbearing women (375 pregnant women and 602 mothers of infants) were enrolled in this study using a two-stage cluster sampling method, and a self-administered questionnaire was used to collect data relating to the mode of birth. A t-test and χ2-test were used to analyse the differences between groups, and logistic regression analysis was used to explore the factors that influenced the mode of birth.
Results
The VB ratio was 46.2 %, while the CS ratio was 53.8 % in Hunan Province. Among women whose preference was VB, only 69.4 % gave birth by VB. Among women whose preference was CS, 98.1 % gave birth by CS. The top four reasons for preferring CS were a lack of confidence in VB (37.3 %), an abnormality in the prenatal examination (36.6 %), the notion that the baby would suffer fewer risks (34.8 %) and the fear of pain from VB (32.7 %). Age, prenatal examination, and doctors’ suggestion were significantly associated with women’s mode of birth preference, while place of household registration, husband’s preference, prenatal examination and doctors’ suggestion had a significant influence on women who changed their choice from VB to CS.
Conclusions
The percentage of CS in Hunan was extremely high. Medical factors, such as abnormalities in prenatal examinations, and non-medical factors, such as a lack of confidence in VB, the fear of pain during VB, the desire to select the time of birth and healthy birth systems, should be seriously considered. Targeted health promotion interventions should be implemented to improve the performance of VB.
Electronic supplementary material
The online version of this article (doi:10.1186/s12884-016-0897-9) contains supplementary material, which is available to authorized users.
Keywords: Vaginal birth, Caesarean section, Mode of birth, Health promotion, China
Background
A Caesarean section (CS) can save lives and prevent injuries in circumstances such as dystocia, malpresentation and foetal distress [1, 2], which occur in approximately 5–15 % of pregnancies [3]. An unnecessary CS can cause additional maternal and perinatal morbidity in cases such as postpartum haemorrhaging, reduced fertility and placental complications in subsequent pregnancies for mothers. Additionally, there is an increased risk of postpartum respiratory morbidity, inflammatory bowel disease, obesity and Type-1 diabetes for children [4–8]. Finally, excessive unnecessary CSs are a substantial economic burden for society [9].
In the past, CS was only implemented in cases of extenuating circumstances or because of identified foetal complications. However, countries worldwide have witnessed an increasing trend toward the use of CS [10–12]. In rural China, the CS rate increased from 6 to 26 % between 1998 and 2007 [13], while in urban areas, it increased from 18.2 % in 1990-92 to 39.5 % in 1998–2002 [14]. By 2007-08, the average CS rate in China had increased to 46.2 % [15].
Studies found a disparity in the contribution of women requesting CS to the escalating CS rate in different countries, from none reported to 17 % [15–18]. It has been demonstrated that age, fear of vaginal birth (VB), issues of control, and safety of CS are the primary factors associated with women’s requests for CS [19–21]. Other researchers found that fewer interactions between the mother and practitioners [22], as well as perceived inequality and inadequacy of care [18], were also reasons that childbearing women requested CS. However, few studies exist that focus on how social and organizational factors, such as culture, hospital and family, influence women’s mode of birth preference, and a limited number of studies has focused on the change of their preference throughout the pregnancy.
Our objectives aimed to explore the influencing factors associated with mode of birth, especially women’s preference and willingness before childbirth and their actual decision, among childbearing women in Hunan Province and to provide evidence and suggestions for improvement and further understanding of VB in China.
Methods
Study population and recruitment procedures
A cross-sectional survey was conducted from August to September in 2012 in Hunan Province. A two-stage cluster sampling method was used to enrol the participants. Hospitals were divided into provincial, city and county levels, and two hospitals were randomly selected from each level. The following equation was used to calculate the sample size in each cluster: n = deff*μa2π(1-π)/δ2 [23], where μa was given a value of 1.96, δ was given a value of 0.1, and deff was given a value of 2. According to a survey conducted by the health department of Hunan Province in 2011, the average CS rate in Hunan was 53.20 % [24]; thus, π was given a value of 0.532. Considering a loss rate of 5 %, the expected sample size was 202 in each cluster.
Because the mode of birth preference changes at different stages, including pregnancy and after childbirth, we selected pregnant women and mothers of infants as study subjects. Eligible subjects were defined as follows: 1) mothers of infants who were 20–45 years old and had given birth (by VB or CS) in the past year, and 2) pregnant women who were 20–45 years old and were more than 37 weeks pregnant. Those diagnosed with pregnancy-related complications, such as pregnancy-induced hypertension, gestational diabetes, etc., were excluded from our research.
Mothers of infants were investigated at postpartum clinics where they received a health examination 42 days after birth (National Basic Public Health Service Specification 2011) and at paediatric clinics in project hospitals where new mothers brought their babies for a health examination. Pregnant women were investigated at antenatal clinics where they received prenatal examinations and pregnancy classes in project hospitals.
To analyse the influencing factors associated with changes the mode of birth, the final total sample size in each cluster was 303, of which 101 were pregnant women and 202 were mothers of infants. Finally, 984 childbearing women were surveyed, including 604 mothers of infants and 380 pregnant women.
Measures
A quantitative survey was used to conduct this research. The questionnaire content included the following (The full list of questions was provided in Additional file 1):
Demographic characteristics: age, sex, monthly income, place of household registration, educational level, and medical insurance.
History of pregnancy and self-reported health status. The women in the study were asked, “How many children have you given birth to?” and “How many times have you had an abortion?” Mothers of infant children who had only given birth to one child were considered “first childbirth”, and pregnant women who had never given birth before were considered “first childbirth”.
Prenatal examination results. The women in the study were asked, “Was any abnormality found during a prenatal examination?” If the answer was yes, then the woman was asked to identify which type(s) of abnormality: ①macrosomia; ②polyhydramnios; ③foetal growth restriction; ④pelvis stenosis; ⑤malposition; ⑥gestational hypertension; ⑦ gestational heart disease(s); ⑧gestational diabetes; ⑨multiple births; or ⑩others.
Women and their families expressed a mode of birth preference and their reasons for that preference. In this part, the preferred mode of birth was ascertained with the following question: “How would you like to give birth? 1) Vaginal birth; 2) Caesarean section.” The following question would ask why the chosen method was selected with several response options provided, each of which could be answered with yes or no.
Only mothers of infants were asked, “How did your latest birth take place?” This question was used to understand the actual mode of birth.
Data collection
The survey was conducted by investigators trained by a professor from Peking University’s School of Public Health using a structured questionnaire. After informed consent was gained from each participant, the participant was asked to complete an anonymous self-administered questionnaire. Investigators were required to check each questionnaire for logistical errors and blanks, and any errors and blanks were corrected on-site. Seven questionnaires were discarded due to substantial amounts of missing data. The validity rate of the questionnaire was 99.3 %, and among 977 qualified participants, 375 were pregnant women and 602 were mothers of infants.
Ethical statement
Before conducting the survey, written informed consent was obtained from each participant in accordance with the ethical standards of the Helsinki Declaration. The study has received approval from the Peking University Institutional Review Board, and the approval number is IRB00001052-12034.
Statistical analysis
The data were independently entered twice using Epidata 3.1, and statistical analyses were performed using SPSS 13.0. Frequencies, percentages, means and standard deviations were used to characterise the data. A t-test and χ2-test were used to analyse differences between groups. Based on the univariate analysis results shown in Table 1, logistic regression was used to explore the influencing factors associated with the mode of birth preference among mothers of infants and pregnant women (logistic regression 1), as well as the consistency between preference and actual mode of birth among infant mothers (logistic regression 2). In logistic regression 1, the mode of birth preference was set as the dependent variable (VB = 0, CS = 1); age, woman’s place of household registration, history of abortion, result of prenatal examination, doctors’ suggestion, self-assessed health status and whether the mother had health insurance were set as independent variables. In logistic regression 2, because pregnant women had not yet given birth, only data from mothers of infants could be used to determine the consistency between the preferred and the actual mode of birth. Whether mothers of infants who preferred VB during pregnancy changed their mode of birth choice was set as the dependent variable (no change = 0, changed from VB to CS = 1); age, women’s place of household registration, husbands’ preferred mode of birth, result of prenatal examination, doctors’ suggestion, whether the mother had health insurance, history of abortion, and self-assessed health status were set as independent variables. Backward LR was used to select the factors, and P < 0.05 was considered statistically significant.
Table 1.
Basic characteristics of participants by mode of birth preference
| Variables | CSa (N = 287) n (%) | VBb (N = 690) n (%) | t/χ 2 value | P value |
|---|---|---|---|---|
| Age (years) | 29.4 ± 4.7 | 26.7 ± 3.9 | 8.519c | < 0.001 |
| Range | 19–42 | 18–42 | ||
| Education level | ||||
| junior middle school and below | 70 (24.6) | 158 (23.0) | 4.801d | 0.187 |
| high school/secondary school | 69 (24.0) | 199 (29.0) | ||
| junior college | 72 (25.3) | 137 (20.0) | ||
| college or above | 74 (26.0) | 192 (28.0) | ||
| Woman’s monthly income | ||||
| 0- | 89 (31.4) | 247 (36.9) | 2.661 d | 0.447 |
| 1020- | 128 (45.2) | 280 (41.8) | ||
| 3500- | 48 (17.0) | 101 (15.1) | ||
| 6000- | 18 (6.4) | 42 (6.2) | ||
| Husband’s monthly income | ||||
| 0- | 14 (4.9) | 54 (8.0) | 4.149 d | 0.246 |
| 1020- | 121 (42.8) | 287 (42.5) | ||
| 3500- | 89 (31.4) | 219 (32.4) | ||
| 6000- | 59 (20.9) | 116 (17.1) | ||
| Woman’s place of household registration | ||||
| Urban | 168 (58.5) | 357 (51.9) | 3.600 d | 0.058 |
| Rural | 119 (41.5) | 331 (48.1) | ||
| At least one type of medical insurance | ||||
| Yes | 261 (91.3) | 613 (89.1) | 1.037 d | 0.309 |
| No | 25 (8.7) | 75 (10.9) | ||
| History of abortion | ||||
| Yes | 156 (55.3) | 262 (38.6) | 22.530 d | < 0.001 |
| No | 126 (44.7) | 416 (61.4) | ||
| First childbirth | ||||
| yes | 181 (63.1) | 555 (80.4) | 32.905 d | < 0.001 |
| No | 106 (36.9) | 135 (19.6) | ||
| Result of prenatal examination | ||||
| abnormal | 126 (43.9) | 137 (20.1) | 57.725 d | < 0.001 |
| normal | 161 (56.1) | 544 (79.9) | ||
| Self-assessed health status | ||||
| good | 156 (54.9) | 415 (61.0) | 3.087 d | 0.079 |
| not good | 128 (45.1) | 265 (39.0) | ||
Note:a VB vaginal birth, b CS caesarean section
c t- test was used to compare the differences in the two groups
dA χ 2-test was used to compare the percentages in the two groups
Results
Study population
Figure 1 shows that the ratio of women who preferred CS or VB changes in our study groups; 21.3 % of pregnant women preferred CS, 34.4 % of mothers of infants preferred CS, and finally 53.8 % of mothers of infants had given birth by CS, in contrast to the decreased ratio of VB (from 78.7 to 46.2 %). These results suggested that CS may not be their first choice, and other influencing factors in the pregnancy process contributed to their mode of birth change.
Fig. 1.
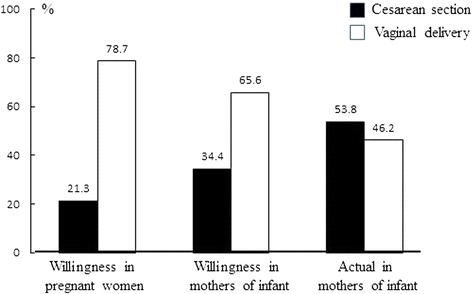
Different delivery mode choice among pregnant women and mothers of infants
The average age of pregnant women and mothers of infants was (27.38 ± 4.81) years old and (27.55 ± 4.18) years old, respectively (t = 0.586, P > 0.05). Women who preferred CS were on average approximately three years older than women who preferred VB (χ2 = 8.519, P < 0.001) (Table 1). The percentage of women with a history of abortion was significantly higher among those preferring CS than among those preferring VB (χ2 = 22.530, P < 0.001). Among women preferring CS, 43.9 % experienced an abnormality in a prenatal examination, while among women preferring VB, only 20.2 % experienced an abnormality. Among women surveyed, 63.1 % of those who preferred CS and 80.3 % of those who preferred VB were first-time mothers. The economic status and self-assessed health status of women preferring CS were slightly better than were those preferring VB, but they had no statistical significance (P > 0.05), and the percentage of urban residents among women preferring CS was higher than those preferring VB; however, these differences were also not significant (P > 0.05).
Primary reasons for mode of birth preference
Among the 676 participants who chose VB as the preferred mode of birth, the most common reason for choosing VB was that mothers would recover faster (78.7 %), and the next most common was that it was a natural process (67.2 %) (Table 2). Only 30.5 % of the participants chose VB because of its low cost. Among the 276 participants who chose CS as their preferred mode of birth, the most common reason for choosing CS was a lack of confidence in VB and concerns about VB (37.3 %), and the next most common was that an abnormality was found during a prenatal examination (36.6 %), and 10.5 % of these participants chose CS to select a fortunate time to give birth.
Table 2.
Main reasons for the mode of birth preference among participants
| Rank | Reasons | N (%) |
|---|---|---|
| Vaginal birth (N = 675) | ||
| 1 | The mother will recover fast | 531 (78.7) |
| 2 | Childbirth is a natural process and CS is unnecessary | 454 (67.3) |
| 3 | A baby delivered by VB is healthier | 403 (59.8) |
| 4 | VB is beneficial for breastfeeding | 352 (52.1) |
| 5 | A baby delivered by VB is smarter | 345 (51.1) |
| 6 | VB leaves no scar | 266 (39.3) |
| 7 | The mother will suffer fewer risks | 251 (37.2) |
| 8 | VB costs less | 206 (30.5) |
| Caesarean section (N = 276) | ||
| 1 | Lack of confidence and concerns about VB | 103 (37.5) |
| 2 | An abnormality was found during a prenatal examination | 101 (36.7) |
| 3 | The baby will suffer fewer risks | 96 (34.9) |
| 4 | Fear of the pain from VB | 90 (32.7) |
| 5 | Have previously had a Caesarean section | 74 (26.9) |
| 6 | The mother will suffer fewer risks | 59 (21.5) |
| 7 | To select the time of birth | 29 (10.5) |
| 8 | Less effect on sexual behaviour | 21 (7.6) |
Multivariate analysis of factors influencing mode of birth preference
The dependent variable was the mode of birth preference. Table 3 depicts the results of multivariate logistic regression analysis for the preferred mode of birth for both mothers of infants and pregnant women. Participants who found an abnormality in a prenatal examination were more likely to prefer CS (OR = 2.0, 95 % CI: 1.4–2.4), those who were advised by a doctor to have CS were five times more likely to choose VB (OR = 5.2, 95 % CI: 2.7–10.0), and older women tended to prefer CS (OR = 1.1, 95 % CI: 1.1–1.2). A woman’s abortion history and whether this was her first childbirth experience were excluded in the mode; however, further analysis showed that among women with no abortion history, 24.5 % (132/539) showed an abnormality in a prenatal examination, but among women with a history of abortion, 30.7 % (128/417) showed an abnormality (χ2 = 4.573, P = 0.032).
Table 3.
Results of multivariate logistic regression of factors influencing mode of birth preferencea
| OR | 95.0 % CI for OR | ||
|---|---|---|---|
| Lower | Upper | ||
| Age | 1.1 | 1.1 | 1.2 |
| Prenatal examination (reference: normal) | 2.0 | 1.4 | 2.4 |
| Doctors’ suggestion (reference: no suggestion) | |||
| Suggest CS | 0.8 | 0.5 | 1.2 |
| Suggest VB | 5.2 | 2.7 | 10.0 |
| No option clearly expressed | 0.8 | 0.5 | 1.6 |
| Constant | 0.01 | ||
Note: aMode of birth preference was set as the dependent variable (VB = 0, CS = 1)
Variables entered into multivariate model included age, woman’s place of household registration, history of abortion, result of prenatal examination, doctors’ suggestion, self-assessed health status and whether the mother had health insurance
Consistency between preferred and actual mode of birth
Among the 602 mothers of infants (Table 4), 395 of them preferred VB during pregnancy, and 207 of them preferred CS. Among women whose preference was VB, 274 of them actually gave birth by VB, while 121 of them actually gave birth by CS; the consistency between the preference for VB and actual childbirth by VB was 69.4 %. Among women whose preference was CS, 203 of them actually delivered by CS, and the consistency between the preference for CS and actual childbirth by CS was 98.1 %. A significant difference was found between them (χ2 = 46.120, P < 0.001).
Table 4.
Consistency between prefered and actual mode of birth (N = 602)
| Actuala | ||||
|---|---|---|---|---|
| VBc | CSd | n | ||
| Preferenceb | VB | 274 | 121 | 395 |
| CS | 4 | 203 | 207 | |
Note: aActual: mode of birth that mothers of infants finally selected during child birth; bPreference: preferred mode of birth of mothers of infants at the last week of pregnancy; c VB vaginal birth; d CS caesarean section
Analysis of influencing factors on the consistency between preferred and actual mode of birth
The dependent variable was whether mothers of infants who preferred VB during pregnancy changed their mode of birth choice. The results of a multivariate logistic regression analysis (Table 5) showed that the doctor’s suggestion influenced mothers to change from VB to CS (OR = 24.8, 95 % CI:3.8–161.9). The other influencing factors were the husband’s preferred mode of birth (OR = 4.4, 95 % CI:1.8–10.8) and a result of a prenatal examination (OR = 3.9, 95 % CI:2.2–6.9).
Table 5.
Logistic regression analysis on consistency between preferred and actual mode of birtha
| OR | 95.0 % CI for OR | ||
|---|---|---|---|
| Lower | Upper | ||
| Woman’s place of household registration (reference: urban areas) | 1.7 | 1.0 | 2.9 |
| Husband’s preferred mode of birth (reference: VB) | 4.4 | 1.8 | 10.8 |
| Prenatal examination (reference: normal) | 3.9 | 2.2 | 6.9 |
| Doctor’s suggestion (reference: no suggestion) | |||
| Suggest VB | 0.8 | 0.3 | 2.1 |
| Suggest CS | 24.8 | 3.8 | 161.9 |
| Not clearly expressed | 1.4 | 0.4 | 5.6 |
| Constant | 0.4 | ||
Note: aWhether mothers of infants who preferred VB during pregnancy changed their mode of birth choice was set as the dependent variable (no change = 0, changed from VB to CS = 1)
Variables entered into the multivariate model included age, women’s place of household registration, husbands’ preferred mode of birth, result of prenatal examination, doctor’s suggestion, whether the mother had health insurance, history of abortion and self-assessed health status
Discussion
The CS rate in Hunan Province was much higher than the overall CS rate of 27.3 % in Asia [15], and it was also much higher than the average CS rate of 36.3 % in China [25].
Among mothers of infants who preferred childbirth by CS, 98.1 % actually gave birth by CS, while only 69.4 % of mothers of infants who preferred VB actually gave birth by VB. Another study found that women’s own preferences about CS were associated with the subsequent mode of birth [26]. Thus, strategies must be implemented to increase the preference for VB.
Many non-clinical causes related to individual social psychology characteristics played important roles in the high preference of CS. In all, 37.5 % of women who preferred CS lacked confidence and were afraid that they could not successfully give birth by VB. Existing uncertainties during the process of VB can cause intense fear of giving birth vaginally; thus, some women were willing to allow doctors to have full control of their birthing process [27, 28].
In addition to the uncertainties, fear of pain during VB was also an important factor influencing women to choose CS. To avoid the risk of emergency CS in labour after a day’s pain, they chose to undergo CS directly. Our study also found that as the time of childbirth approached, the uncertainty and fear of pain about VB increased, thus raising women’s anxiety levels, and the proportion of women who preferred CS increased. This was even more pronounced when they witnessed the great pain other pregnant women experienced during childbirth, especially those pregnant women who experienced great pain and eventually failed to give birth by VB.
Culture-related social concerns also influence the mode of birth preference. Approximately 10.5 % of women preferred CS because it allowed them to select the time of birth. In China, many people believe that a person’s fate, to some extent, is determined by the day they were born. A study found that days deemed auspicious in the Chinese lunar calendar were associated with a significantly higher probability that a CS would be performed, while those days considered inauspicious were associated with a significantly lower number of CS [29]. Age was associated with the preference of CS during pregnancy but was not associated with the change in the actual mode of birth of CS from the preferred mode of birth of VB. This was consistent with previous studies that found that older women were more likely to prefer CS [20, 30].
Multivariable analysis showed that abnormalities found in prenatal examinations (AFPE) and doctor-suggested CS were the primary influencing factors that led women to prefer CS, as well as for women who preferred VB but actually gave birth by CS. AFPE was an important medical indication for women to prefer CS and for doctors to suggest CS. Among 263 women who found an abnormality in a prenatal examination, 31.2 % were suggested CS by doctors, and 47.9 % preferred CS or agreed with their doctor to have CS. Although AFPE does not mean that CS must be chosen, doctors tend to widen CS indicators, especially when women who found an abnormality in a prenatal examination requested CS because the relationship between doctors and patients has become increasingly strained in China and because CS protects doctors from the fear of malpractice and possible litigation [31, 32].
In addition, the gap between medical costs and government investment in China is covered through paid services [33], and doctors’ incomes are directly related to the hospital revenue. Revenue-related bonus systems for doctors provide strong incentives to generate demand for profitable high-tech diagnostics, surgeries and drugs, resulting in what is known as supplier-induced demand [34, 35]. CS is obviously more profitable because of its higher cost, longer hospital stay and increased drug usage; therefore, it tends to be frequently suggested by doctors. A study showed that in China, there are 2.2 obstetric staff for every 10,000 people [36]. The serious shortage of obstetric doctors spurred doctors to prefer CS because it allowed them to schedule and reduce the birth time [37]. Policy makers should comprehensively consider the effects of supplier-induced demand on CS, including how to improve doctor-patient relationships and increase patients’ confidence in the doctors. It is especially important to reform the existing health service funding arrangements and to increase the number of obstetric doctors and midwives and their salaries to encourage them to perform vaginal births.
On the other hand, because of limited information and knowledge in the field of healthcare services, women tend to accept doctors’ advice to avoid the unknown risks. Because abortion is associated with placenta previa, placental abruption and foetal distress [38–40], it is indirectly associated with women’s mode of birth. According to Chinese statistics, the number of abortions performed in 2012 was 6.6 million [41], and a lack of knowledge and use of contraception was strongly associated with the high abortion rate [42].
Strengths and limitations
Providing field evidence for health education and health promotion strategy development to improve natural birth in China is one of our study strengths. The data were collected from three levels of hospitals (province-city-county) so that comprehensive analysis results on the influencing factors for natural birth could be available. To reduce the bias, interviewers were trained to ensure the standardized collection of questionnaire answers, as well as to ensure standardized procedures were performed for the questionnaire survey at each hospital site.
There are some limitations of the study. First, data were collected by a questionnaire; thus, it is possible that some participants provided socially desirable responses rather than reporting their AFPE. Participants may have also over-reported their AFPE. Second, women more than 37 weeks pregnant were selected to replace the preference of mode of birth among mothers of infants in late stages of pregnancy to depict the tendency of the preferred CS rate as the pregnancy progresses. Third, the fact that only six sites were studied may limit the generalization of the findings, and the results should not be extrapolated to represent all of the pregnant women or mothers of infants in China due to important regional differences in terms of demographics and economic conditions. Fourth, there was no control group selected. Fifth, limited by resources, we only conducted a retrospective cross-sectional study, not a prospective study, to include women in earlier pregnancy stages and to follow up with them until childbirth to understand changes during the pregnancy. Finally, because of the cross-sectional nature of the data, most responses were evaluated retrospectively; therefore, recall bias was unavoidable.
Conclusion
The CS rate in Hunan was extremely high. Influencing factors, including abnormalities in prenatal examinations, lack of confidence in VB, fear of pain during VB, the desire to select time of birth and health birth systems, should be seriously considered. Measures should be taken to cultivate awareness about the adverse short- and long-term outcomes of CS and to build confidence in VB among pregnant women. A study indicated that a standard and convenient specification for a prenatal education curriculum provided by hospitals and their doctors is appropriate for providing prenatal education to pregnant women in China [43]. Additionally, continuing professional training and development in approaches for intrapartum care among doctors and midwives should be encouraged to promote natural birth, and CS should not be considered the best method to address dystocia.
Targeted health promotion intervention activities should be implemented to improve the performance of VB and reduce unnecessary CS in China. Educational programs should be provided to women of childbearing age to cultivate awareness of the harm of abortion and to instruct them to adopt safe and effective birth control methods to reduce the abortion rate, as well as to decrease abnormalities in prenatal examinations.
Proven effective measurements should be utilized and promoted to improve women’s satisfaction and confidence with childbirth and to reduce the fear of childbirth by VB so that more women would be willing to choose or attempt VB. An effective, comprehensive program to reduce unnecessary CS should be designed and studied.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its Additional files 1 and 2.
Acknowledgements
The authors would like to thank the participating investigators from Hunan Province for their contributions to the data collection. The authors would also like to thank all of the respondents enrolled in our study.
Funding
The study was funded by a grant from the UNFPA (CHN7U204).
Open access
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Additional files
A full List of Questionnaire. (DOC 67 kb)
Dataset of Survey. (XLS 1417 kb)
Footnotes
Yuhui Shi and Ying Jiang are co-first author.
Competing interests
The authors declare that they have no competing interest.
Authors’ contribution
YS, co-investigator, had primary responsibility for the conception of the analysis, oversight of the implementation of the research, analysis and preparation of the manuscript. YJ, co-investigator, performed data analyses, drafted the manuscript and incorporated critical revisions. QZ, YY, co-investigator, assisted with data acquisition, cleaning and analysis. HY contributed to the interpretation of the results and revised successive versions of the article. CC, as a co-investigator, was responsible for the management of data collection, training, oversight and interpretation of the data and critical revisions of the manuscript. RP assisted with study implementation and assisted with critical revisions of the manuscript. All of the authors provided critical revisions of the manuscript and final approval of its content.
References
- 1.Lee YM, D’Alton ME. Cesarean delivery on maternal request: maternal and neonatal complications. Curr Opin Obstet Gynecol. 2008;20(6):597–601. doi: 10.1097/GCO.0b013e328317a293. [DOI] [PubMed] [Google Scholar]
- 2.Hankins GD, Clark SM, Munn MB. Cesarean section on request at 39 weeks: impact on shoulder dystocia, fetal trauma, neonatal encephalopathy, and intrauterine fetal demise. Semin Perinatol. 2006;30(5):276–87. doi: 10.1053/j.semperi.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 3.WHO, UNFPA, UNICEF, AMMDD. Monitoring emergency obstetric care: a handbook, http://apps.who.int/iris/bitstream/10665/44121/1/9789241547734_eng.pdf Accessed 20 Aug 2014.
- 4.Gurol-Urganci I, Bou-Antoun S, Lim CP, Cromwell DA, Mahmood TA, Templeton A, van der Meulen JH. Impact of Caesarean section on subsequent fertility: a systematic review and meta-analysis. Hum Reprod. 2013;28(7):1943–52. doi: 10.1093/humrep/det130. [DOI] [PubMed] [Google Scholar]
- 5.Fawcus S, Moodley J. Postpartum haemorrhage associated with caesarean section and caesarean hysterectomy. Best Pract Res Clin Obstet Gynaecol. 2013;27(2):233–49. doi: 10.1016/j.bpobgyn.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A, Shah A, Campodonico L, Bataglia V, Faundes A. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 7.Hyde MJ, Modi N. The long-term effects of birth by caesarean section: the case for a randomised controlled trial. Early Hum Dev. 2012;88(12):943–9. doi: 10.1016/j.earlhumdev.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Bager P, Simonsen J, Nielsen NM, Frisch M. Cesarean section and offspring’s risk of inflammatory bowel disease: a national cohort study. Inflamm Bowel Dis. 2012;18(5):857–62. doi: 10.1002/ibd.21805. [DOI] [PubMed] [Google Scholar]
- 9.Khan A, Zaman S. Costs of vaginal delivery and Caesarean section at a tertiary level public hospital in Islamabad, Pakistan. BMC Pregnancy Childbirth. 2010;10:2. doi: 10.1186/1471-2393-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO Appropriate technology for birth. Lancet. 1985;2(8452):436–7. [PubMed] [Google Scholar]
- 11.Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, Wilson EC. Births: final data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70. [PubMed] [Google Scholar]
- 12.Canadian Institute for Health Information. Giving Birth in Canada: Regional Trends From 2001–2002 to 2005–2006, https://secure.cihi.ca/free_products/childbirth_aib_070725_e.pdf (2007). Accessed 20 Aug 2014.
- 13.Long Q, Zhang Y, Raven J, Wu Z, Bogg L, Tang S, Hemminki E. Giving birth at a health-care facility in rural China: is it affordable for the poor? Bull World Health Organ. 2011;89(2):144–52. doi: 10.2471/BLT.10.079434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang S, Li X, Wu Z. Rising cesarean delivery rate in primiparous women in urban China: evidence from three nationwide household health surveys. Am J Obstet Gynecol. 2006;195(6):1527–32. doi: 10.1016/j.ajog.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 15.Lumbiganon P, Laopaiboon M, Gulmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, Attygalle DE, Shrestha N, Mori R, Nguyen DH. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet. 2010;375(9713):490–9. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- 16.Robson SJ, Tan WS, Adeyemi A, Dear KB. Estimating the rate of cesarean section by maternal request: anonymous survey of obstetricians in Australia. Birth. 2009;36(3):208–12. doi: 10.1111/j.1523-536X.2009.00331.x. [DOI] [PubMed] [Google Scholar]
- 17.MacDorman MF, Menacker F, Declercq E. Cesarean birth in the United States: epidemiology, trends, and outcomes. Clin Perinatol. 2008;35(2):293–307. doi: 10.1016/j.clp.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 18.McCourt C, Weaver J, Statham H, Beake S, Gamble J, Creedy DK. Elective cesarean section and decision making: a critical review of the literature. Birth. 2007;34(1):65–79. doi: 10.1111/j.1523-536X.2006.00147.x. [DOI] [PubMed] [Google Scholar]
- 19.Dursun P, Yanik FB, Zeyneloglu HB, Baser E, Kuscu E, Ayhan A. Why women request cesarean section without medical indication? J Matern Fetal Neonatal Med. 2011;24(9):1133–7. doi: 10.3109/14767058.2010.531327. [DOI] [PubMed] [Google Scholar]
- 20.Huang K, Tao F, Faragher B, Raven J, Tolhurst R, Tang S, Broek NV. A mixed-method study of factors associated with differences in caesarean section rates at community level: The case of rural China. Midwifery. 2013;29(8):911–20. doi: 10.1016/j.midw.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 21.D’Souza R. Caesarean section on maternal request for non-medical reasons: putting the UK National Institute of Health and Clinical Excellence guidelines in perspective. Best Pract Res Clin Obstet Gynaecol. 2013;27(2):165–77. doi: 10.1016/j.bpobgyn.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Gamble J, Creedy DK, McCourt C, Weaver J, Beake S. A critique of the literature on women’s request for cesarean section. Birth. 2007;34(4):331–40. doi: 10.1111/j.1523-536X.2007.00193.x. [DOI] [PubMed] [Google Scholar]
- 23.Huang Y. Clinical epidemiology (second version) Beijing: People’s medical publishing house; 2008. p. 85. [Google Scholar]
- 24.Ye D, Li M, Xie D, Zhao L, Wu N, Fu C, Sun Z. Study on the factors related to Cesarean Section(CS) in Hu-nan Province by two-level models analysis. Chin J Health Stat. 2010;27(4):341–4. [Google Scholar]
- 25.Meng Q, Xu L, Zhang Y, Qian J, Cai M, Xin Y, Gao J, Xu K, Boerma JT, Barber SL. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–14. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 26.Hildingsson I. How much influence do women in Sweden have on caesarean section? A follow-up study of women’s preferences in early pregnancy. Midwifery. 2008;24(1):46–54. doi: 10.1016/j.midw.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Fenwick J, Staff L, Gamble J, Creedy DK, Bayes S. Why do women request caesarean section in a normal, healthy first pregnancy? Midwifery. 2010;26(4):394–400. doi: 10.1016/j.midw.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 28.Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86(4):451–6. doi: 10.1080/00016340701217913. [DOI] [PubMed] [Google Scholar]
- 29.Lo JC. Patients’ attitudes vs. physicians’ determination: implications for cesarean sections. Soc Sci Med. 2003;57(1):91–6. doi: 10.1016/S0277-9536(02)00301-5. [DOI] [PubMed] [Google Scholar]
- 30.Tollanes MC. Increased rate of Caesarean sections--causes and consequences. Tidsskr Nor Laegeforen. 2009;129(13):1329–31. doi: 10.4045/tidsskr.08.0453. [DOI] [PubMed] [Google Scholar]
- 31.Ji H. A study on associated factors related to high cesarean section rate and future intervention strategies from perspectives of both clients and providers in one district of Shangha. Shanghai: Fudan University; 2012. [Google Scholar]
- 32.Minkoff H. Fear of litigation and cesarean section rates. Semin Perinatol. 2012;36(5):390–4. doi: 10.1053/j.semperi.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 33.Yip W, Hsiao WC. The Chinese health system at a crossroads. Health Aff (Millwood) 2008;27(2):460–8. doi: 10.1377/hlthaff.27.2.460. [DOI] [PubMed] [Google Scholar]
- 34.Eggleston K, Li L, Meng Q, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Econ. 2008;17(2):149–65. doi: 10.1002/hec.1306. [DOI] [PubMed] [Google Scholar]
- 35.Bogg L, Huang K, Long Q, Shen Y, Hemminki E. Dramatic increase of Cesarean deliveries in the midst of health reforms in rural China. Soc Sci Med. 2010;70(10):1544–9. doi: 10.1016/j.socscimed.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 36.Hu W, Jin X, Du L, Luo R. The current status and equity of human resources allocation in obstetric healthcare of china. Chin J Women Child Health. 2013;4(1):1–3. [Google Scholar]
- 37.Lin HC, Xirasagar S. Institutional factors in cesarean delivery rates: policy and research implications. Obstet Gynecol. 2004;103(1):128–36. doi: 10.1097/01.AOG.0000102935.91389.53. [DOI] [PubMed] [Google Scholar]
- 38.Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol. 1997;177(5):1071–8. doi: 10.1016/S0002-9378(97)70017-6. [DOI] [PubMed] [Google Scholar]
- 39.Koifman A, Levy A, Zaulan Y, Harlev A, Mazor M, Wiznitzer A, Sheiner E. The clinical significance of bleeding during the second trimester of pregnancy. Arch Gynecol Obstet. 2008;278(1):47–51. doi: 10.1007/s00404-007-0530-2. [DOI] [PubMed] [Google Scholar]
- 40.Song W, Jin Z. The effect of ante- primiparous artificial abortion to pregnancy and parturition. Sh J Prev Med. 2001;13(4):184–5. [Google Scholar]
- 41.MOH . Chinese health year book 2012. Beijing: Chinese Peking Union Medical university press; 2012. p. 201. [Google Scholar]
- 42.Xu J, Cheng L. Awareness and usage of emergency contraception among teenagers seeking abortion: a Shanghai survey. Eur J Obstet Gynecol Reprod Biol. 2008;141(2):143–6. doi: 10.1016/j.ejogrb.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Shi Y, Wang D, Yuan Y, Jiang Y, Zeng Q, Chang C. The effect of prenatal education curriculum on mother’s prenatal examination utilization, delivery mode and recovery status: a cross-sectional survey in China. Environ Health Prev Med. 2015;20(6):397–403. doi: 10.1007/s12199-015-0480-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article and its Additional files 1 and 2.


