Abstract
A diverse 5,000-compound library was synthesized from commercially available diamines and screened for activity against Mycobacterium tuberculosis in vitro, revealing 143 hits with MIC equal to or less than 12.5 µM. New prospective scaffolds with antitubercular activity derived from homopiperazine, phenyl- and benzyl substituted piperazines, 4-aminomethylpiperidine, 4-aminophenylethylamine, 4,4'-methylenebiscyclohexylamine were identified. Compound SQ775 derived from homopiperazine, and compound SQ786 derived from benzylpiperazine had potent antimicrobial activity against M. tuberculosis in experimental animals in vivo.
Among infectious diseases, tuberculosis (TB) remains the leading single-agent killer in the world: 2 billion people are infected with latent TB and at risk for development of active disease and, annually, more than 8 million people advance to active and contagious TB. More than 2 million people die of pulmonary TB every year.1–3 Decades of misuse of existing antibiotics and poor compliance with a prolonged TB drug regimen that involves four different drugs for two months, and two drugs for an additional four months, have created an epidemic of drug-resistant TB. In countries where adequate supplies of the drugs are not readily available, the prevalence of multi-drug resistant TB (MDR-TB) is reported to be as high as 50%.4,5 In the early 1990s, New York City had one of the worst outbreaks of MDR-TB the country has ever experienced, and the city spent nearly $1 billion over two years on containment.6
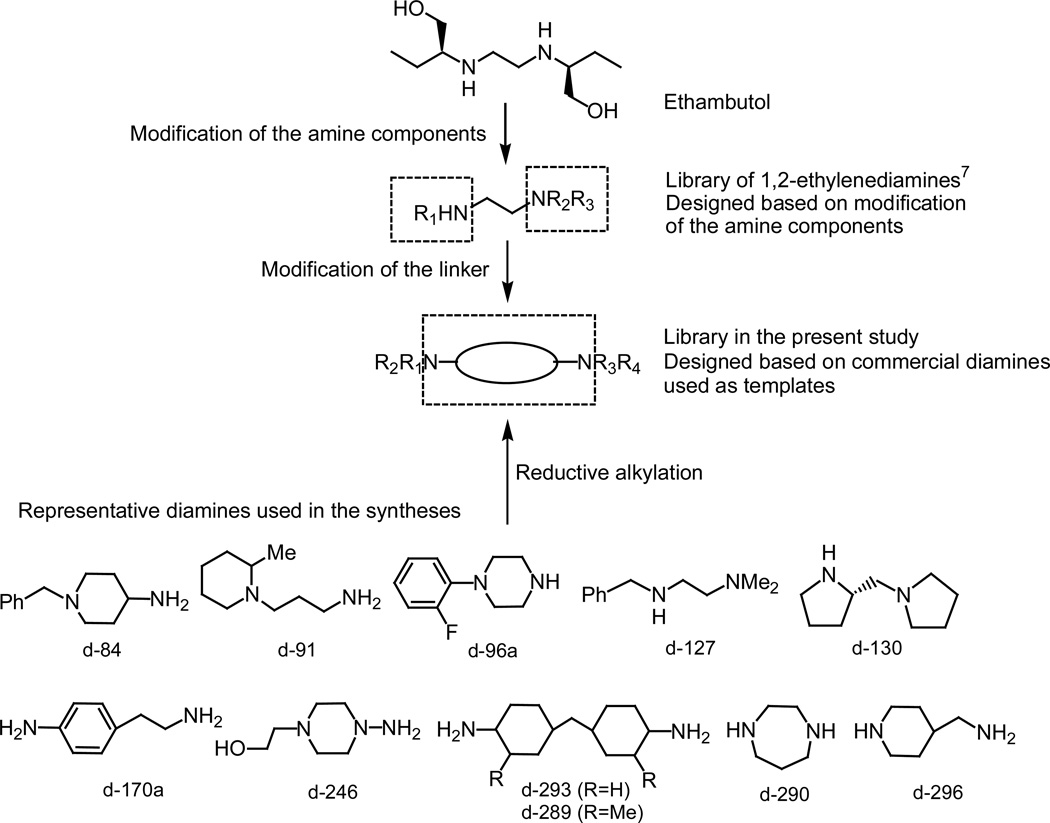
Over the last few years our research efforts have been focused on the discovery of novel scaffolds with antimycobacterial activity and the development of new anti-tubercular agents that can improve the current therapeutic regimen and be effective in treatment of MDR-TB. We synthesized several combinatorial libraries, totaling over 100K compounds, and screened them against Mycobacterum tuberculosis (M. tuberculosis). The first library of 63,238 compounds with the 1,2-ethylenediamine pharmacophore of ethambutol (EMB)7 lead to the identification of a drug candidate, SQ109 (N-Geranyl-N’-(2-adamantyl)ethane-1,2-diamine).7–9 To further enhance structural diversity, we designed, synthesized, and evaluated for antitubercular activity other diamine libraries, with an emphasis on modification of the linker between two nitrogen atoms, Figure 1. Here we present the synthesis and in vitro screening of a diverse library derived from commercially available “ready-to-use” diamine templates that led to identification of new scaffolds with activity against M. tuberculosis. Preliminary in vivo efficacy data of selected hits are also reported.
Figure 1.
Evolution of synthesized diamine-based libraries.
A targeted diamine library of approximately 5,000 compounds was synthesized in one step on 96-well plates from commercially available diamines via solution phase reductive alkylation in the presence of a polymer–bound trimethylammonium cyanoborohydride. Fifty-nine diamines that included substituted alkylenediamines, piperazines, homopiperazines, biscyclohexylamines, and pyrrolidines (Figure 2), were organized into four groups based on their structure and reactivity, and used in the syntheses as mixtures of twenty (Group 1), twelve (Group 2), fifteen (Group 3), or twelve (Group 4) compounds. We selected 64 aldehydes and 20 ketones as alkylating agents to ensure structural diversity, and also taking into consideration previously established structure-activity relationship (SAR) for 1,2-ethylenediamine series7 that warranted the use of adamantane-, cyclooctane-, and diphenylethyl-containing molecules. Prior to syntheses, the carbonyl compounds were organized in a 96-well master plate as a 1.2 M solutions of individual compounds in 1,2-dichloroethane: they were used in the reactions in 5–10 molar excess. The Supporting Information Section contains a complete list of the diamines and carbonyl compounds involved in the synthesis of the library.
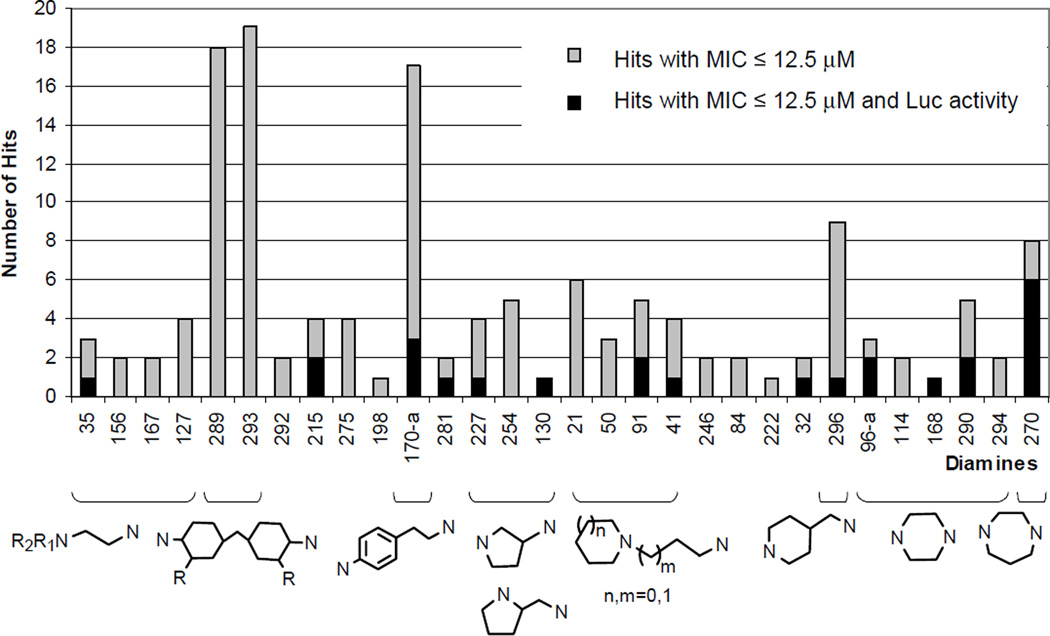
Figure 2.
Occurrence of the starting diamines in the hit molecules and scaffolds with demonstrated activity against M. tuberculosis.
Formation of the final products and composition of the product mixtures were assessed by mass spectrometry by testing two randomly selected columns per plate: 17% of the library was tested. Based on MS data, at least 4,788 of the targeted compounds (95% of the library) were formed. As expected, reductive alkylation of secondary amines yielded only mono alkylated compounds. Interpretation of the mass spectra of product mixtures derived from pooled monosubstituted piperazines, for example, was quite straightforward because every starting diamine gave only one product. For the rest of the library, derivatization of the diamines that contained a primary amino group led to the formation of mixtures of mono- and double-alkylated products, and syntheses outcomes were dependent upon the reactivity of both diamine and carbonyl compounds. Diamines with a sterically-hindered amino group (3-aminoquinonucledine, for example) formed exclusively mono alkylated products. Reductive alkylation by ketones, regardless of the nature of the starting diamines, proceeded with the sole formation of mono alkylated products. Mono alkylation of the primary amino group was also the only (or a major) process in the reactions that involved aldehydes such as 4-(dimethylamino)benzaldehyde, 2-nitrobenzaldehyde, indol-3-carboxaldehyde, 1-methyl-2-pyrrolecarboxaldehyde, 4-quinolinecarboxaldehyde, 2,3-dihydroxybenzaldehyde, or 2-hydroxy-4-methoxybenzaldehyde. Sterically hindered 5-norbornene-2-carboxaldehyde and diphenylacetaldehyde always produced a roughly equal mixture of mono- and double-alkylated products. 2-Methoxycinnamaldehyde, hydrocinnamaldehyde, citronellal, and 5-(4-chlorophenyl)furfural favored double alkylation, and in some cases the reactions with these compounds proceeded even further.
The prepared library was advanced into in vitro screening without purification, since identified hits would be later re-synthesized and purified to confirm activity. The in vitro testing against M. tuberculosis was carried out by (1) direct determination of minimum inhibitory concentration (MIC) in a broth microdilution assay and (2) a high-throughput screening bioluminescence assay (Luciferase (Luc) assay) with recombinant M. tuberculosis strain containing promoter Rv0341 fused to firefly luciferase. This promoter is activated when the bacteria encounter certain antibiotics such as EMB, isoniazid (INH), and ethionamide that act on targets involved in mycobacterial cell wall biosynthesis.7,8 The recombinant M. tuberculosis harboring the P0341-luciferase fusion produces light when the bacteria are treated with these antitubercular agents. While MIC is a direct measure of bacteria growth inhibition, the Luc assay allowed us to determine whether a compound interferes with the cell wall biosynthesis. Thus, by combining these two assays we were able to identify compounds capable of inhibiting M. tuberculosis growth in vitro presumably through damaging the bacterial cell wall components. Compounds were screened (as prepared) in pools within a range of 50 to 0.39 µM concentrations per each individual compound based on an assumption that every synthesized compound was produced with the theoretical yield of 100%; commercially available EMB (of 99% purity) was used as a positive control in each assay; the MIC of EMB ranged from 6.25 µM (1.73 µg/ml) to 3.13 µM (0.86 µg/ml). Wells with MIC equal to or less than 12.5 µM regardless the status in the Luc assay as well as the wells with MIC equal to or less than 50 µM and the Luc activity that exceeded background luminescence of untreated control by 1.5 times were considered active and were selected for deconvolution. Out of 336 synthesized compound mixtures, 176 showed antimycobacterial activity and were deconvoluted. Re-synthesized individual compounds in each active well were tested for inhibitory activity against M. tuberculosis as well as for the activation of the P0341-luciferase fusion using the same in vitro screening assays. As a result, 143 hits with MIC equal to or less than 12.5 µM were identified in the broth microdilution assay; among those, 25 compounds were also active in the Luc assay.
We found that the vast majority of identified hits were derived from five diamines: 4,4’-methylenebis(cyclohexylamine) (d-289) and its analogue 4,4’-methylenebis(2-methylcyclohexylamine) (d-293), 2-(4-aminophenyl)ethylamine (d-170.a), 4-(aminomethyl)piperidine (d-296), and homopiperazine (d-270), see Figures 1 and 2. Both biscyclohexylamines yielded at least thirty-seven hits with MIC equal to or less than 12.5 µM, but not a single one of them was active in the Luc assay, suggesting either that this compound class targeted different biological pathway than cell wall biosynthesis or the class represented compounds with nonspecific toxicity towards the target pathogen in the screens. Similarly, hit compounds derived from 2-(4-aminophenyl)ethylamine (d-170a) and from 4-(aminomethyl)piperidine (d-296) showed little activity in the Luc screening assay (Figure 2). Homopiperazine hits were found to be the most interesting, since they demonstrated significant activity in both bacterial growth inhibition and the Luc assay: out of 8 hits derived from homopiperazine, 6 were active in both screens. These compounds likely target mycobacterial cell wall components.
Among the new scaffolds with antitubercular activity, we also identified a series of phenyl- and benzyl substituted piperazines:10 when combined, 1-(2-fluorophenyl)piperazine (d-96.a), 1-piperonylpiperazine (d-114), 1-(4-fluorophenyl)piperazine (d-168), 1-benzylpiperazine (d-290), and 1-(4-chlorobenzhydryl)piperazine (d-294) gave 13 hits with 5 active in both screening assays.
Other identified scaffolds (Figure 2) were: 1-(2-aminoethyl)piperidine (d-21), 1-(2-aminoethyl)pyrrolidine (d-50), 1-(2-aminoethyl)piperazine (d-41), and pipecoline d-91 (total 18 hits), tryptamines d-215 and d-275 (8 hits), as well as 3-aminopyrrolidine (d-227), pyrrolidine d-130 (Figures 1), and (S)-(+)-2-(aminomethyl)pyrrolidine (d-254) that produced total 10 hits.
Within the carbonyl compounds, the most frequently occurring structural fragments in the hit molecules were contributed by 4-benzyloxybenzaldehyde (14 hits), 5-(4-chlorophenyl)furfural (11 hits), decalone (12 hits), 2-methoxy-1-naphthaldehyde (9 hits), and (S)-perillaldehyde (8 hits). We also found similarities with the 1,2-ethylenediamine series: some of the hits in this library contained earlier described7 myrtenyl, geranyl, and adamantane fragments derived from (−)-myrtenal (11 hits), (S)-citronellal (10 hits), geranylacetone (13 hits), and 2-adamantanone (8 hits).
After identification of pharmacophores with antimycobacterial activity, we focused mostly on the homopiperazine series, since these compounds were active against M. tuberculosis in both broth microdilution and Luc assays, and were easily synthesized. Eight symmetrically substituted homopiperazines SQ775-SQ782 were re-synthesized on a larger scale, purified to ensure at least 95% purity, and re-tested against M. tuberculosis. Determined by the same microdilution method, the MIC of purified hits fell within a 1.56–6.25 µM range and in most cases confirmed the previous MIC results obtained during the screening of deconvoluted plates (Table 1). INH and Rifampicin (Rif,), both commercially available from Sigma, were used as controls, with MIC of 0.46 µM (0.0625 µg/ml) and 0.03 µM (0.03 µg/ml) respectively.
Table 1.
Structures and in vitro data of homopiperazine and piperazine hit compounds
| Compd. | Structure | MIC in screen, µM1 |
MIC µM2 |
IC50, µM3 |
SI4 | Activity in the Luc assay,5 % |
LogP6 |
|---|---|---|---|---|---|---|---|
| Homopiperazines | |||||||
| SQ775 | 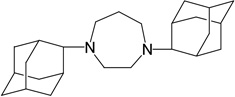 |
6.25 | 1.56 | 132 | 84.6 | 126 | 5.98 |
| SQ776 | 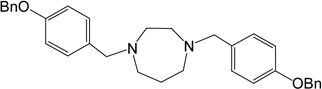 |
12.5 | 3.13 | 56 | 18 | not active | 6.29 |
| SQ777 | 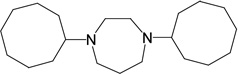 |
12.5 | 1.56 | 74 | 47 | 81 | 6.57 |
| SQ778 | 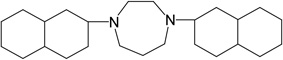 |
1.56 | 1.56 | 54 | 35 | 127 | 7.4 |
| SQ779 | 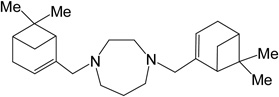 |
3.13 | 3.13 | 110 | 35 | 113 | 6.99 |
| SQ780 | 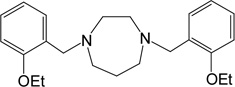 |
1.56 | 1.56 | 71 | 46 | 70 | 4.04 |
| SQ781 | 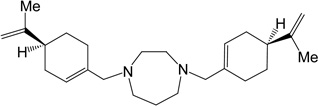 |
12.5 | 6.25 | 81 | 13 | not active | 7.14 |
| SQ782 | 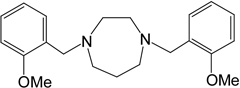 |
6.25 | 6.25 | 105 | 17 | 138 | 2.98 |
| Piperazines | |||||||
| SQ765 | 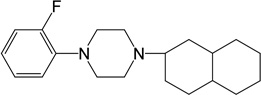 |
6.25 | 12.5 | 70 | 6 | 145 | ND7 |
| SQ774 | 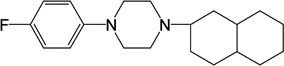 |
12.5 | 12.5 | 86 | 7 | 157 | 5.49 |
| SQ783 | 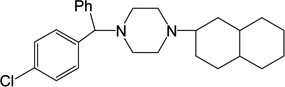 |
12.5 | 6.25 | 47 | 8 | not active | 6.01 |
| SQ784 | 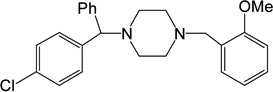 |
12.5 | 6.25 | 65 | 10 | not active | 3.85 |
| SQ786 | 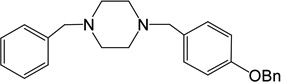 |
3.13 | 6.25 | 54 | 9 | not active | 4.02 |
| SQ788 | 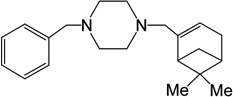 |
6.25 | 6.25 | 64 | 10 | not active | 4.36 |
| SQ789 | 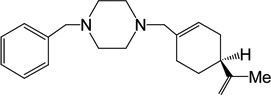 |
3.13 | 3.13 | 60 | 19 | not active | 4.44 |
Results obtained during screening of deconvoluted plates; the MICs determined by broth microdilution method. The MIC of EMB (control) ranged from 1.73 µg/ml (6.25 µM) to 0.86 µg/ml (3.13 µM).
MIC of purified compounds determined by broth microdilution method; 10 mM stock solutions in methanol were used. MIC of the controls: INH 0.0625 µg/ml (0.46 µM), RIF 0.03 µg/ml (0.03 µM).
Determined with HepG2 cell line in the MTS assay.
Selectivity Index SI (SI=IC50:MIC).
Presented as the percent of activity of a tested compound compared to the activity of EMB (100%).
Calculated using the algorithm and database statistics of the ACD.
Not determined.
To select candidates for in vivo efficacy testing in mice, synthesized compounds were evaluated8 for (a) predicted membrane permeability based on logP values (www.acdlabs.com) (b) in vitro cytoxicity in HepG2 cells to determine IC50,11 and (c) Selectivity Index (SI), the ratio of IC50 to MIC as an estimate of a therapeutic window, see Table 1. Compounds with the best data, SQ775 (MIC 6.25 µM, SI 17, logP 5.98) and SQ780 (MIC 1.56 µM, SI 18, logP 4.04) were selected for in vivo efficacy evaluation in murine models of tuberculosis. Compound SQ782 (MIC 6.25 µM, SI 13, logP 2.98) was postponed due to structural similarities with SQ780.
We added compound SQ786 as a representative of the piperazine series to the studies with the two homopiperazines in animal models of TB. SQ786 demonstrated an MIC of 6.25 µM on M. tuberculosis, relatively low cytotoxicty (IC50 54 µM), SI of 9, and an acceptable-to-good oral bioavailability12 logP value of 4.02, Table 1. But unlike its higher homologues, SQ786 was not active in the Luc assay, implying that its target is not presumably involved in bacterial cell wall biosynthesis. Overall, out of thirteen piperazine hits, the MIC of seven compounds were re-confirmed (Table 1) and six compounds demonstrated poorer than expected activity against M.tuberculosis, with MIC values of 25–50 µM.
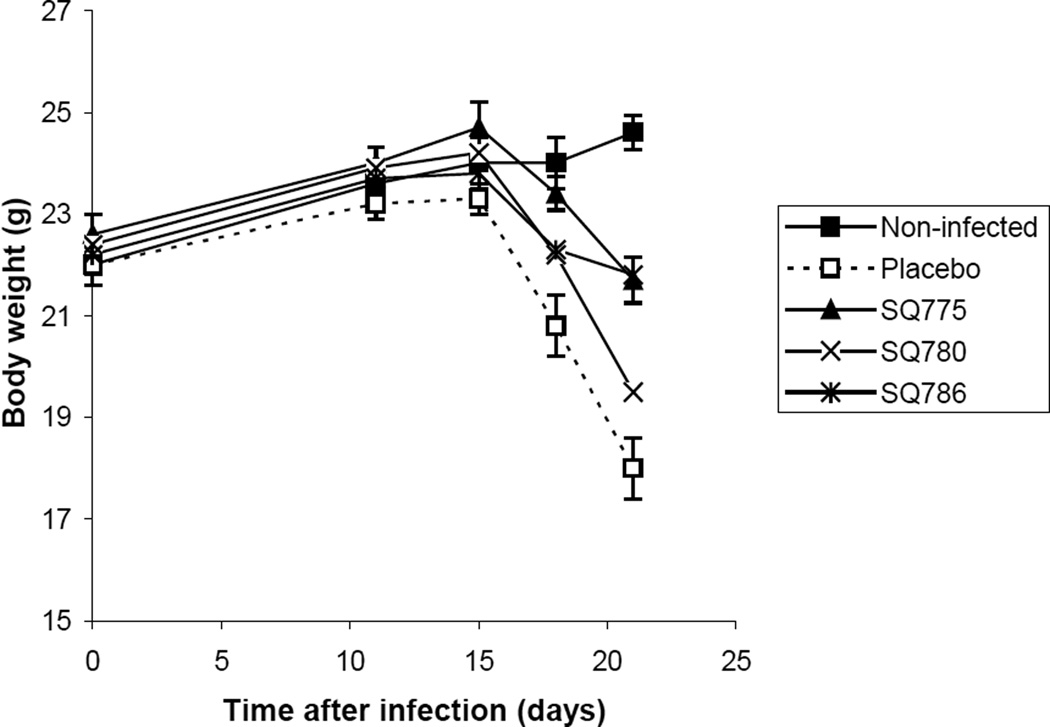
In vivo testing of SQ775, SQ780, and SQ786 was conducted using a rapid (3 wk) screening model for TB infection based on active drug prevention of infection-induced weight loss in mice.13 This screen can predict quickly and with reasonable accuracy the efficacy of both known and experimental drugs, Figure 3. Briefly, C3H mice were inoculated intravenously (iv) with 106 CFU of virulent M. tuberculosis H37Rv to develop rapid and progressive TB disease. Chemotherapy was initiated 7 days after inoculation and continued for 10 days. Experimental compounds were administrated daily by gavage at 10mg/kg (dose has not been optimized). Uninfected mice, infected untreated mice, and infected mice treated with INH at 25 mg/kg13 were used as the controls. Body weight of mice in all groups (6 per group) was monitored from day 0. By day 10, infected placebo control mice began to lose weight, and by day 20 the mice in this group lost more than 25% of their body weight (the sign of terminal illness). Treatment with SQ775 and SQ786 prevented weight loss and delayed mortality: by day 21 following challenge, the mice treated with SQ775 or SQ786 lost only 12% of their initial body weight. Compound SQ780 was ineffective in this model (21% weight loss). Preliminary results from in vivo testing of SQ775 and SQ786 in a low-dose mouse model of chronic TB infection14 suggest that these compounds might serve as leads to develop new potent antibacterial compounds.15
Figure 3.
In vivo efficacy testing of SQ775, SQ780, and SQ786 in the rapid mouse model of TB. Dynamics of body weight of mice infected with M.tuberculosis and treated with SQ775, SQ780, and SQ786 at 10 mg/kg by oral administration. In this model, isoniazid at a dose of 25 mg/kg (used as a positive control) fully prevented body weight loss (data are not shown; the dynamics of body weight were identical to those of uninfected control mice).
In conclusion, we identified new prospective scaffolds with activity against M. tuberculosis in vitro and in vivo. Synthesis of new compounds based on these potentially valuable scaffolds is in progress.
Acknowledgement
This work was supported by the Challenge Grant (UC1A149514) of the National Institute of Allergic and Infectious Diseases (NIAID) of the NIH. The Inter-Institute Program of the NIAID for the Development of AIDS-Related Therapeutics provided MS support for the project. We would like to thank Dr. Charles Sparacino and Dr. Michael Gardner of the Research Triangle Institute International for mass spectra data and Dr. Yiu-fai Lam of the University of Maryland, College Park, for acquiring NMR spectra.
Footnotes
Supporting Information Available: complete list of diamines and carbonyl compounds used in the library preparation, detailed experimental procedures, 1H NMR and MS spectra for individual compounds. This material is available free of charge via the Internet at http://pubs.acs.org.
References
- 1.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Global burden of tuberculosis. JAMA. 1999;282:677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 2.Bass JB, Farer LS, Hopewell PC, O’Brein R, Jacob RF, Ruben F, Snider DE, Jr, Thornton G. Treatment of tuberculosis and tuberculosis infection in adults and children. Am. J. Respir. Crit. Care Med. 1994;149:1359–1374. doi: 10.1164/ajrccm.149.5.8173779. [DOI] [PubMed] [Google Scholar]
- 3.Farmer P, Bayona J, Becerra M, Furin J, Henry C, Hiatt H, Kim JY, Mitnick C, Nardell E, Shin S. The dilemma of MDR-TB in the global era. Int. J. Tuberc. Lung. Dis. 1998;2:869–876. [PubMed] [Google Scholar]
- 4.Cohn DL, Bustreo F, Raviglione MC. Drug-resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD Global Surveillance Project. International Union Against Tuberculosis and Lung Disease. Clin. Infect. Dis. 1997;24(Suppl 1):S121–S130. doi: 10.1093/clinids/24.supplement_1.s121. [DOI] [PubMed] [Google Scholar]
- 5.Espinal MA, Laslo A, Simonsen L, Boulahbal F, Kim SJ, Reniero A, Hoffner S, Reider HL, Binkin N, Dye C, Williams R, Raviglione MC. Global trends in resistance to antituberculosis drugs (For the World Health Organization–International Union against Tuberculosis and Lung Disease Working Group on Anti-Tuberculosis Drug Resistance Surveillance) N. Engl. J. Med. 2001;343:1294–1303. doi: 10.1056/NEJM200104263441706. [DOI] [PubMed] [Google Scholar]
- 6.Stokstad E. Drug-resistant TB on the rise. Science. 2000;287:2391. doi: 10.1126/science.287.5462.2391a. [DOI] [PubMed] [Google Scholar]
- 7.Lee RE, Protopopova M, Crooks E, Slayden RA, Terrot M, Barry CE., III Combinatorial lead optimization of [1,2]-diamines based on Ethambutol as potential antituberculosis preclinical candidates. J. Comb. Chem. 2003;5:172–187. doi: 10.1021/cc020071p. 2003. [DOI] [PubMed] [Google Scholar]
- 8.Protopopova M, Hanrahan C, Nikonenko B, Samala R, Chen P, Gearhart J, Einck L, Nacy CA. Identification of a new antitubercular drug candidate SQ109 from a combinatorial library of 1,2-ethylenediamines. J. Antimicrob. Chemother. 2005;56:968–974. doi: 10.1093/jac/dki319. [DOI] [PubMed] [Google Scholar]
- 9.Jia L, Tomaszewski JE, Hanrahan C, L. Coward L, P. Noker P, G. Gorman G, Nikonenko B, Protopopova M. Pharmacodynamics and pharmacokinetics of SQ109, a new diamine-based antitubercular drug. Br. J. Pharmacol. 2005;144:80–87. doi: 10.1038/sj.bjp.0705984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.For antitubercular activity of some compound classes enhanced by the piperazine mojety, see the following. Renau TE, Sanchez JP, Gage JW, Dever JA, Shapiro MA, Gracheck SJ, Domagala JM. J. Med. Chem. 1996;39:729–735. doi: 10.1021/jm9507082. Foroumadi A, Soltani F, Moshafi MH. Boll. Chim. Farm. 2002;141:394–396. Tangallapally RP, Yendapally R, Lee RE, Hevener K, Jones VC, Lenaerts AJM, McNeil MR, Wang Y, Franzblau S, Lee RE. J. Med. Chem. 2004;47:5276–5283. doi: 10.1021/jm049972y. Kuo MR, Morbidoni HR, Alland D, Sneddon SF, Gourlie BB, Staveski MM, Leonard M, Gregory JS, Janjigian AD, Yee C, Musser JM, Kreiswirth B, Iwamoto H, Perozzo R, Jacobs WR, Jr, Sacchettini JC, Fidock DA. J. Biol. Chem. 2003;278:20851–20859. doi: 10.1074/jbc.M211968200. Foks H, Pancechowska-Ksepko D, Janowiec M, Zwolska Z, Augustynowicz-Kopec E. Acta Pol. Pharm. 2004;61:473–476.
- 11.Cory AH, Owen TC, Barltrop JA, Cory JG. Use of an aqueous tetrazolium/formazan assay for cell growth assay in culture. Cancer Commun. 1991;3:207–212. doi: 10.3727/095535491820873191. [DOI] [PubMed] [Google Scholar]; CellTiter 96 AQueous Non-Radioactive Cell Proliferation Assay Technical Bulletin. Promega Corporation; Rev 04/05. [Google Scholar]
- 12.Lipinskii CA, Lombardo F, B.W. Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug. Delivery Rev. 1997;23:3–25. doi: 10.1016/s0169-409x(00)00129-0. [DOI] [PubMed] [Google Scholar]
- 13.Nikonenko BV, Samala R, Einck L, Nacy CA. Rapid, simple in vivo screen for new drugs active against Mycobacterium tuberculosis. Antimocrob. Agents Chemother. 2004;48:4550–4555. doi: 10.1128/AAC.48.12.4550-4555.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly BP, Furney SK, Jessen MT, Orme IM. Low-dose aerosol infection model for testing drugs for efficacy against. Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 1996;40:2809–2812. doi: 10.1128/aac.40.12.2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.In the chronic mouse model, female C57BL/6 mice were infected iv with virulent 105 CFU M. tuberculosis H37Rv; chemotherapy was initiated 20 days following infection. SQ775 and SQ786 (at 10 mg/kg), and isoniazid (at 25 mg/kg, used as a positive control) were administered daily by gavage for four weeks, 5 days/week. The cfu in organs were determined as described.13 Following reduction in the CFUs was observed (compared to a group of infected non-treated mice); 3.5 log (isoniazid), 0.7 log (SQ775), 1.0 log (SQ786).