Abstract
Background:
Cardiovascular incidents are a common cause of death around the world. Acute myocardial infarction (AMI) poses high risks for the patient due to plaque rupture or erosion along with a superimposed non-occlusive thrombus; therefore, timely treatment with antithrombotic agents plays a key role in reducing an AMI mortality rate.
Objectives:
The present study aimed to assess the time interval between the admission of AMI-suspected patients and treatment initiation.
Patients and Methods:
This cross-sectional study was conducted on 110 patients admitted to the emergency department of Imam Hussein hospital in Tehran, Iran. Data were collected using checklists, completed by the patients’ next of kin or the emergency staff. To analyze the data, student t- test and analysis of variance were used.
Results:
In this study, 31 female and 79 male subjects were included, respectively. The mean time to receive the first dose of streptokinase was 66.39 minutes (73.74 minutes for females and 63.5 minutes for male patients), varying from 49.92 minutes in the morning to 69.78 minutes in the afternoon and 72.68 minutes during night shifts.
Conclusions:
The door-to-needle (DTN) time, in a standard setting, is recommended to be less than 30 minutes. According to the results of this study, the DTN time is comparatively two times longer in females and afternoon and night shifts. Different variables including emergency staff, physicians, patients’ characteristics, and environmental/physical factors induced this difference.
Keywords: Acute Myocardial Infarction, Emergency Service, Needle Stick Injuries, Streptokinase
1. Background
In the United States, approximately 6 - 7 million people, suspected of coronary artery diseases, are admitted to emergency departments (EDs) of hospitals each year. Around 20% - 25% of these patients are diagnosed with coronary artery diseases and should receive the required treatments.
Acute myocardial infarction (AMI) is the most common reason for many hospitalizations in developed countries. Annually, 650 thousand patients present with AMI in the United States, and 450 thousand people experience disease recurrence (1, 2).
Heart attack or AMI is also a leading cause of mortality in Iran. About 24% of Iranian people die due to AMI. These patients are mostly within the age range of 15 - 49 years, while 10.5 - 32% of the population are over 50 years of age (3). Nearly 30% of deaths among patients with AMI occur during early stages (first 30 days) of AMI development.
One of the most effective treatments for this disease is administration of a thrombolytic agent for reducing mortality rate in AMI patients (1). Administration of thrombolytic therapy within a short time period after the onset of clinical symptoms of AMI can be advantageous. The main objective of the therapy is the reduction of infarcted region following the reduced time to reperfusion (2).
Clinical studies have shown that mortality rate has decreased from 50% to 40% in patients who are treated within the first hours after AMI development. Delay in thrombolytic therapy is associated with a higher risk of death in patients (4). Generally, delay in the initiation of treatment is placed under two categories: 1) delay in hospital admission, which may occur for various reasons, e.g. long distance between the patient’s place of residence and hospital, attributing cardiac pain (heart attack) to noncardiac causes, and living alone and 2) delays at hospitals.
Time interval between a patient’s admission to ED and the initiation of thrombolytic therapy in AMI patients is of high significance; this is commonly referred to as door-to-needle (DTN) time (5); in fact, DTN time must not take longer than 30 minutes (6-8).
Door-to-needle time is divided into three intervals: 1) the first 10 minutes when the electrocardiogram (ECG) is carried out in the ED; 2) the second 10 minutes for a quick clinical evaluation and confirmation of AMI diagnosis, followed by the evaluation of contraindications to intravenous thrombolysis; and 3) the last 10 minutes when streptokinase is prepared for infusion and the required injections are made (4).
The study of Irwani et al. concluded that the median DTN time was significantly shorter in patients who were thrombolyzed in the ED by emergency physicians (EPs), compared to those who were thrombolyzed in coronary care unit (CCU) by cardiologists (29 minutes vs. 60 minutes, P < 0.001) (9). Schull et al. showed that ED crowding is associated with increased DTN time for patients with suspected AMI, and can act as a barrier to improving cardiac care in the ED (10).
In another study, Zed et al. showed that the DTN time for patients without prior cardiology consult (prescriptions by EPs) was significantly shorter than those with cardiology consult before administration (mean 41 minutes vs. 108 minutes; P < 0.001) (11).
In one study, the researchers concluded that the DTN time was three times longer than the international standard; this is due to a number of reasons such as personnel-related factors, environmental conditions, and physical status of the patients (12).
2. Objectives
Given that every medical center may have certain shortcomings, the present study aimed to assess the time interval between hospital admission and initiation of intravenous thrombolytic therapy for patients admitted to the ED of our hospital.
3. Patients and Methods
3.1. Patients
The subjects of this cross-sectional study were AMI patients, undergoing streptokinase treatment, who referred to the Imam Hussein hospital in Tehran, Iran, in 2010. We evaluated the records of 110 patients in the current study. Data were obtained using a number of questionnaires, which were completed by patients’ next of kin or the emergency staff (11). Considering the ratio of patients treated within the ideal time (less than 30 minutes), the sampling variables were considered as d = 0.08 and P = 0.25, according to the study by Zed et al. (11).
The inclusion criteria were as follows: 1) 30 - 75 years of age; 2) AMI patients with indications for thrombolytic therapy; and 3) patient’s consent (or the consent of a relative aware of the patient’s medical condition).
The exclusion criteria were as follows: 1) lack of patient’s consent; 2) past myocardial infarction; 3) lack of indications for thrombolytic therapy or contraindications to the treatment; 4) streptokinase administration within the last 6 months; 5) warfarin therapy; 6) active peptic ulcer diseases; 7) bleeding disorders or uncontrolled hypertension; 8) moderate to severe valvular heart disease; 9) previous cardiac surgery; and 10) a cerebrovascular accident within the past 6 weeks.
3.2. Statistical Analysis
Data were analyzed using descriptive statistics with SPSS software version 15.0 (SPSS, Inc. Chicago, Illinois, USA). Descriptive statistics included mean, standard deviation and frequency distribution tables. In this study, quantitative data analysis was presented by mean and standard deviation and in order to analyze the qualitative data, the rates and ratios were closely measured.
Furthermore, the relationship between qualitative variables was reviewed by chi-square test and the association between quantitative variables was analyzed using a correlation test. Also, we used t-test and analysis of variance to obtain analytical statistics.
3.3. Ethical Considerations
Informed consents were obtained from the patients, and the subjects were ensured about the confidentiality of the data. The study was approved by the ethics committee of research at the Tehran university of medical sciences.
4. Results
Overall, 110 patients, including 31 (28.2%) females and 79 (71.8%) males, were enrolled in this study. The mean age of the subjects was 59.75 ± 8.61 years (range 36 - 85 years), and 64 patients (58.2%) were smokers, 32 patients (29.1%) had type 2 diabetes mellitus, 67 subjects (60.9%) had hypercholesterolemia, 57 patients (51.8) presented with hypertension, and 52 participants (47.3%) suffered from coronary artery diseases; only 7 patients (6.4%) had no cardiac risk factors.
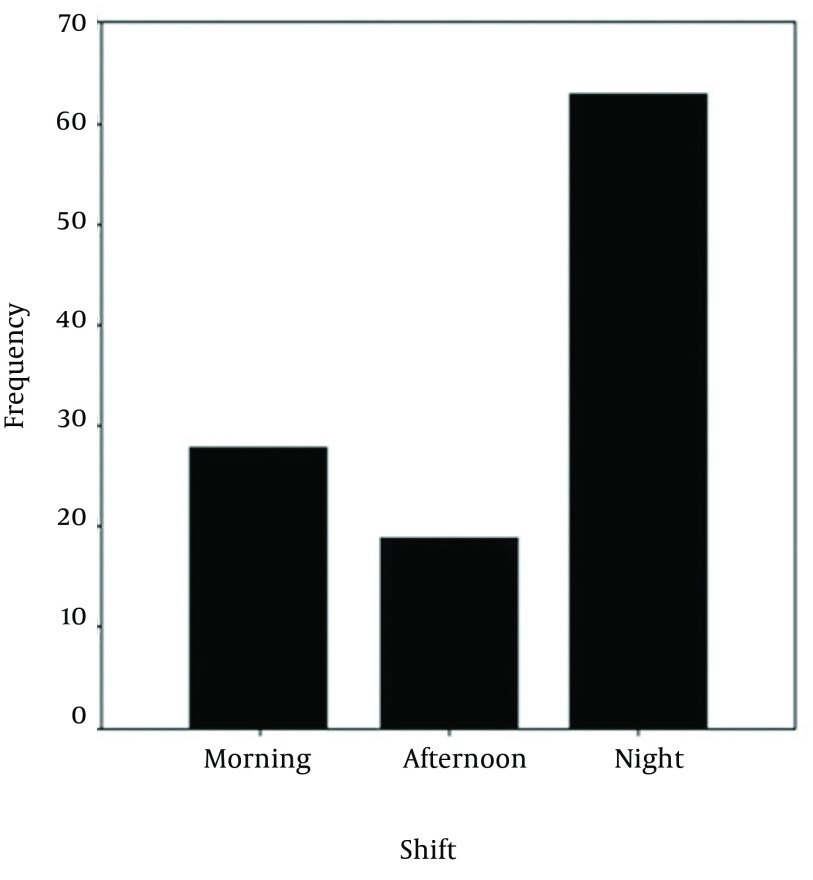
In terms of admission time to ED, 28 (25.5%), 19 (17.2%), and 63 (57.3%) patients were admitted during morning, afternoon, and night shifts, respectively. Among 63 patients, who were referred to the hospital during night shifts, 26 (41.3%) cases were admitted at 8 - 12 PM, and 37 (58.7%) patients were admitted from 12 PM to 7 AM. Also, 81 patients (73.4%) were transferred to the hospital by an ambulance, and 29 patients (26.4%) were transferred by vehicles (of their own or a taxi).
Our results indicated that the mean DTN time was 66.39 ± 29.17 (range of 20 - 185 minutes). Among patients under evaluation, the mean time interval between the onset of chest pain and admission to ED was 136.16 minutes (range of 35 - 747 minutes).
The mean time interval between ED admission and ECG performance was 17.64 minutes, with a range of 4 - 50 minutes. The mean time interval between ECG performance and thrombolytic therapy prescription was 18.91 minutes, with a range of 0 - 110 minutes. Finally, the mean time interval between the prescription of thrombolytic therapy and injection was 29.95 minutes, with a range of 5 to 140 minutes.
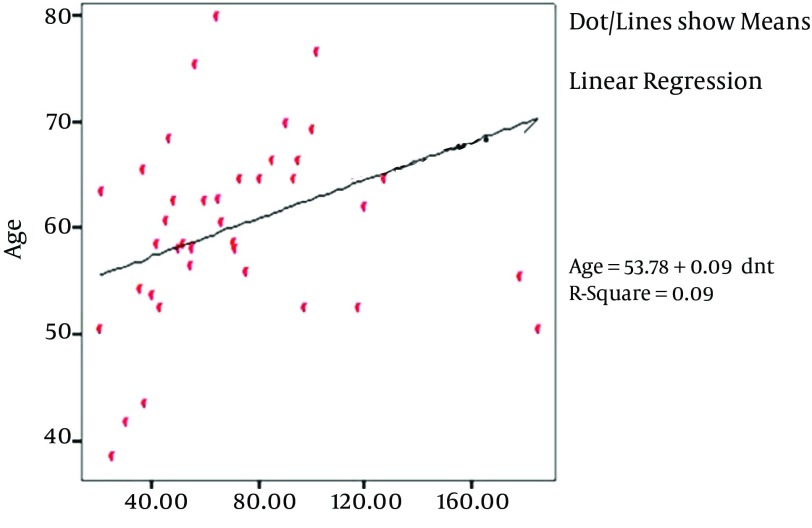
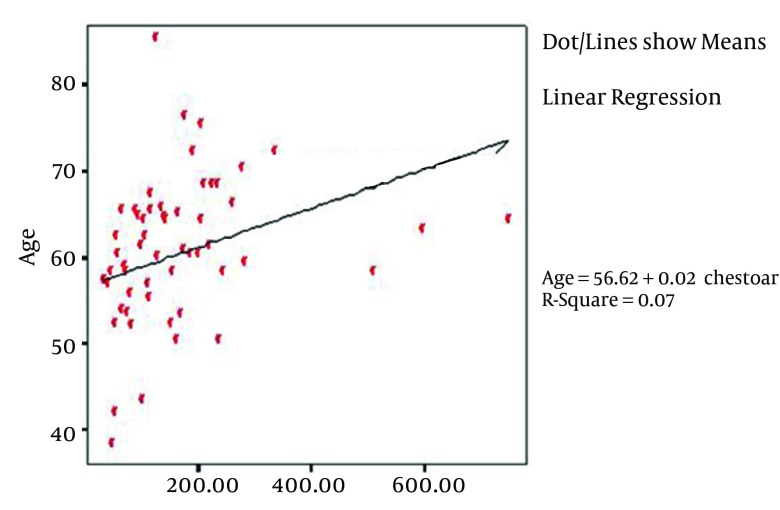
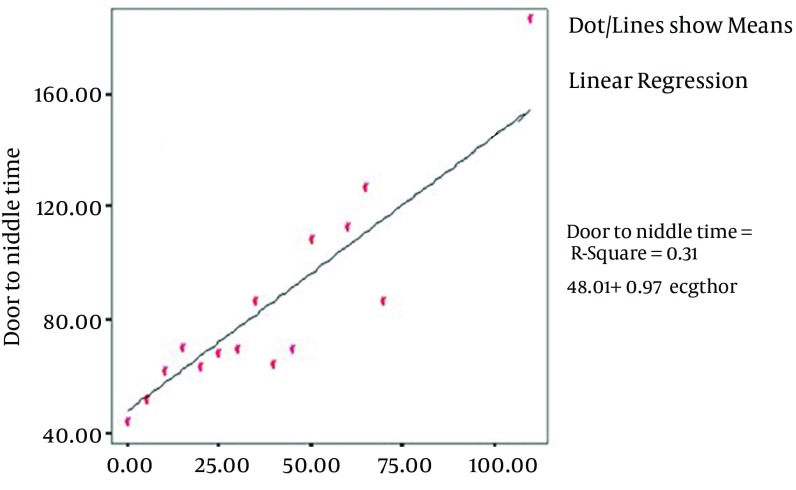
According to the results, the correlation coefficient between age and DTN time was 0.3 (P = 0.001). In addition, the correlation coefficient between age and time interval between the onset of chest pain and ED admission was 0.269 (P = 0.005). The correlation coefficient between age and time interval between ED admission and ECG was 0.85 (P = 0.381) (Figure 1). Also, the correlation coefficient between age and the interval between ECG and thrombolytic therapy prescription was 0.317 (P = 0.001) (Figure 2). The correlation coefficient between age and interval between thrombolytic therapy prescription and injection was 0.136 (P = 0.158). (Figures 3 and 4)
Figure 1. Diagram of Distribution of Admission of the Patients in Various Working Shifts.
Figure 2. The Correlation Between Age and Door-to-Needle Time in Patients.
Figure 3. The Correlation Between Age and Time to Onset of Chest Pain Until Admission in the Emergency Department.
Figure 4. The Correlation Between Age and Time of Electrocardiography to Thrombolytic Therapy.
The findings indicated no relationship between gender and the mentioned time intervals (P > 0.5). Our findings revealed that the mean DTN time in patients who were admitted during night shifts, was 23 minutes longer (mean) than the DTN time in patients who were admitted during morning shifts (P = 0.002). In addition, our results showed that the mean DTN time was 78.88 ± 26.91 min at the beginning of night shifts (8 - 12 PM) and 68.32 ± 35.12 minutes at the end of night shifts (12 PM to 7 AM) (P = 0.202).
Also, we assessed the mean DTN time in terms of means of transfer. The mean DTN time in patients, who were transferred to the hospital by an ambulance, was 4 min longer than those who were transferred by private vehicles (P = 0.532).
Our findings indicated that the correlation between DTN time and the time interval between the onset of chest pain and admission was 0.149 (P = 0.122). Moreover, the relation between DTN time and interval between ED admission and ECG performance was significant (P < 0.001, r = 684). Likewise, the association between DTN time and interval between ECG and thrombolytic therapy prescription was noticeable (P = 0.001, r = 0.560). Also, the time interval between therapy prescription and injection was significant (P = 0.001, r = 0.560).
5. Discussion
Many institutions have established strict strategies to decrease the DTN time for fibrinolytic administration. It has been demonstrated that a diligent team, who follow clear protocols, can effectively reduce the DTN time in one hospital (13-15).
In our study, the mean DTN time for all patients was estimated to be 66.39 minutes, which is nearly twice as long as the standard time. In a study performed in Israel, this duration was around 54 minutes (16). Also, in a study performed in Vancouver, Canada, the mean time of DTN was estimated about 43 minutes (11). At the national university of Singapore hospital, DTN time was reported to be 60 minutes for patients who were administered streptokinase at the CCU (9); also, this time was reported to be 64 minutes in a study in Glasgow (17).
In a similar research, performed in Urmia, Iran, the mean DTN time for patients, who had received streptokinase in CCU, was 89.25 minutes (12). However, DTN time in a cohort study by Kelly et al. was approximately 46.5 minutes (18). In this regard, O’Rourke et al. suggested that the availability of ECG equipment in ED might significantly reduce the DTN time. Subsequently, such equipment are now easily accessible and have proven to be effective in many centers (5).
The comparison between the current study and previous research indicated a noticeable prolongation of DTN time in the present study. Also, the results of several studies indicate that one of the most important strategies for reducing DTN time is performing intravenous thrombolytic therapy in the EDs rather than CCUs; fortunately, this strategy has been implemented at our center.
Another considered factor in our study was the DTN time in female patients, which was longer than that of male patients; this is consistent with the report of the royal hospital in the United Kingdom, where the mean DTN time was 90 minutes for women (60 to 143.5) and 78 minutes (50 to 131 minutes) for men (19). It should be also noted that the study in Urmia, Iran, showed that DTN took longer for women than men (109.2 vs. 86.5 minutes) (11). This difference could be due to the misconception that acute coronary syndrome is less prevalent in women compared to men; therefore, women are highly neglected in terms of symptoms.
Another factor investigated in this study was the difference in DTN time during various work shifts. In this study, DTN time in morning shift was significantly different from that of afternoon and night shifts. The patients, who were admitted during morning hours, had drastically shorter DTN time compared to those who were admitted during afternoon or night shifts. Conversely, in the study in Vancouver, Canada, the DTN time during night shifts appeared to be significantly shorter than those of morning and evening work shifts (11). However, in one study, no significant difference was observed among different work shifts (12).
We found out that ED crowding is associated with increased DTN time for patients, and this correlation was of statistical importance. This finding was, to some extent, aligned with the finding of a study in Toronto, Canada, in which the mean DTN times were 40, 45, and 47 minutes in conditions of none, moderate, and high ED crowding, respectively (10). In our analyses, we noted that the heavy workload of ED personnel is associated with an increased DTN time, which proves to be a barrier to improving cardiac care at EDs for patients with suspected AMI.
In the current study, another challenging issue was the role of EPs in the administration of intravenous thrombolysis. The findings of Zed et al. suggested that cardiology consult leads to prolonged DTN time. This time prolongation could be attributable to the delay inherent in waiting for a consultation before fibrinolytic prescription and subsequent administration. Thus, the DTN time was significantly shorter when the fibrinolytic agent was prescribed by an EP (without prior cardiology consult), compared to the time when cardiology consult was requested before administration (35 vs. 90 minutes) (11).
The mean DTN time in the report of Irwani was significantly shorter in patients who were thrombolyzed in ED by an emergency physician, compared to those who were thrombolyzed in CCU by cardiologists (29 vs. 60 minutes, P < 0.001) (9). A number of studies in Australia and UK reported similar results in terms of DTN time (20, 21).
Patient evaluation by cardiologists at ED leads to longer DTN times. The main reasons for cardiology consult were lack of confidence in ECG diagnosis, probable contraindications to thrombolytic therapy, and unstable hemodynamic patients. However, intravenous thrombolytic therapy by EPs is of great significance and reflects their medical skills. We presume that by placing more confidence in thrombolytic therapy, we might no longer need cardiology consult. This possibility may be associated with improved care of patients with AMI.
Considering the provided information in the current study and the importance of reducing DTN time for AMI mortality reduction, the following recommendations seem practical: 1) streptokinase administration in the ED instead of CCU; 2) accelerating the admission process of AMI-suspected patients; 3) sufficient training and awareness of emergency staff to better understand the importance of time in treatment; and 4) prescription of intravenous thrombolytic therapy by EPs at EDs.
Acknowledgments
We would like to thank the vice-chancellor for research at Imam Hussein hospital, affiliated to Tehran university of medical sciences, for funding and supporting the current study. The help of all colleagues, who participated in the preparation of this manuscript, are highly appreciated. We also thank Zamen Salamati Co. for English proofreading of the manuscript.
Footnotes
Authors’ Contribution:Study concept and design: Ali Omraninava; data analysis and interpretation: Amir Masoud Hashemian; drafting of the manuscript: Babak Masoumi and Ali Omraninava; and statistical analysis: Amir Masoud Hashemian.
Funding/Support:This study was financially supported by vice-chancellor of research of Imam Hussein hospital in Tehran university of medical sciences.
References
- 1.Zeraati F, Homayounfar S, Esna-Ashari F, Khalili M. Fibrinolytic Therapy in CCU Instead of Emergency Ward: How It Affects Door to Needle Time? Int J Prev Med. 2014;5(3):308–12. [PMC free article] [PubMed] [Google Scholar]
- 2.Atzema CL, Austin PC, Tu JV, Schull MJ. Emergency department triage of acute myocardial infarction patients and the effect on outcomes. Ann Emerg Med. 2009;53(6):736–45. doi: 10.1016/j.annemergmed.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Maleki A, Shariari A, Sadeghi M, Rashidi N, Alyari F, Forughi S, et al. Evaluation of fibrinolytic medical therapy for patients with acute myocardial infarction. ARYA Atheroscler. 2012;8(1):46–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Kloner RA, Dai W, Hale SL, Shi J. Approaches to Improving Cardiac Structure and Function During and After an Acute Myocardial Infarction: Acute and Chronic Phases. J Cardiovasc Pharmacol Ther. 2015 Nov 25; doi: 10.1177/1074248415616187. pii: 1074248415616187. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.O'Rourke MF, Cook A, Carroll G, Gallagher D, Hall J. Accuracy of a portable interpretive ECG machine in diagnosis of acute evolving myocardial infarction. Aust N Z J Med. 1992;22(1):9–13. doi: 10.1111/j.1445-5994.1992.tb01701.x. [DOI] [PubMed] [Google Scholar]
- 6.Khalili H, Talasaz AH, Jenab Y, Salarifar M. Clinical characteristics and risk assessment of ST-segment elevation myocardial infarction patients of an Iranian referral center. J Cardiovasc Med (Hagerstown). 2012;13(11):708–15. doi: 10.2459/JCM.0b013e328356a3c6. [DOI] [PubMed] [Google Scholar]
- 7.Yaylali YT. Door-to-needle times in acute myocardial infarction. Asian Cardiovasc Thorac Ann. 2010;18(2):122–6. doi: 10.1177/0218492309338130. [DOI] [PubMed] [Google Scholar]
- 8.Vlahaki D, Fiaani M, Milne WK. A door-to-needle time of 30 minutes or less for myocardial infarction thrombolysis is possible in rural emergency departments. CJEM. 2008;10(5):429–33. doi: 10.1017/s1481803500010502. [DOI] [PubMed] [Google Scholar]
- 9.Irwani I, Seet CM, Manning PG. Emergency physician versus cardiologist-initiated thrombolysis for acute myocardial infarction: a Singapore experience. Singapore Med J. 2004;45(7):313–7. [PubMed] [Google Scholar]
- 10.Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44(6):577–85. doi: 10.1016/S0196064404005232. [DOI] [PubMed] [Google Scholar]
- 11.Zed PJ, Abu-Laban RB, Cadieu TM, Purssell RA, Filiatrault L. Fibrinolytic administration for acute myocardial infarction in a tertiary ED: factors associated with an increased door-to-needle time. Am J Emerg Med. 2004;22(3):192–6. doi: 10.1016/j.ajem.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Khadem VK, Rostamzadeh A, Mohammadzadeh H. Assessment of Door to Needle Time for Initiation of Streptokinase Infusion in Patients With Acute Myocardial Infarction. J Urmia Univ med sci. 2005;16(3):152–8. [Google Scholar]
- 13.Kelion AD, Banning AP, Shahi M, Bell JA. The effect of reduction of door-to-needle times on the administration of thrombolytic therapy for acute myocardial infarction. Postgrad Med J. 1998;74(875):533–6. doi: 10.1136/pgmj.74.875.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knox I. Door to needle times of 12 minutes are possible in one emergency department. Bmj. 1999;319(7210):643. doi: 10.1136/bmj.319.7210.643b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Millar-Craig MW, Joy AV, Adamowicz M, Furber R, Thomas B. Reduction in treatment delay by paramedic ECG diagnosis of myocardial infarction with direct CCU admission. Heart. 1997;78(5):456–61. doi: 10.1136/hrt.78.5.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolak A, Gilutz H, Amit G, Cafri C, Ilia R, Zahger D. Door to balloon and door to needle: temporal trends in delays to reperfusion. Isr Med Assoc J. 2003;5(12):852–5. [PubMed] [Google Scholar]
- 17.Corfield AR, Graham CA, Adams JN, Booth I, McGuffie AC. Emergency department thrombolysis improves door to needle times. Emerg Med J. 2004;21(6):676–80. doi: 10.1136/emj.2004.014449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly AM, Kerr D, Patrick I, Walker T. Call-to-needle times for thrombolysis in acute myocardial infarction in Victoria. Med J Aust. 2003;178(8):381–5. doi: 10.5694/j.1326-5377.2003.tb05255.x. [DOI] [PubMed] [Google Scholar]
- 19.Hourigan CT, Mountain D, Langton PE, Jacobs IG, Rogers IR, Jelinek GA, et al. Changing the site of delivery of thrombolytic treatment for acute myocardial infarction from the coronary care unit to the emergency department greatly reduces door to needle time. Heart. 2000;84(2):157–63. doi: 10.1136/heart.84.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edhouse JA, Sakr M, Wardrope J, Morris FP. Thrombolysis in acute myocardial infarction: the safety and efficiency of treatment in the accident and emergency department. J Accid Emerg Med. 1999;16(5):325–30. doi: 10.1136/emj.16.5.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barakat K, Wilkinson P, Suliman A, Ranjadayalan K, Timmis A. Acute myocardial infarction in women: contribution of treatment variables to adverse outcome. Am Heart J. 2000;140(5):740–6. doi: 10.1067/mhj.2000.110089. [DOI] [PubMed] [Google Scholar]