Abstract
Background:
Trauma is a leading cause of morbidity and mortality among individuals under 40 and is the third main cause for death throughout the world.
Objectives:
This study was designed to compare our modified injury scoring systems with the current injury severity score (ISS) from the viewpoint of its predictive value to estimate the duration of hospitalization in trauma patients.
Patients and Methods:
This analytical cross-sectional study was performed at the general referral trauma center of Bandar-Abbas in southern Iran from March 2009 to March 2010. The study population consisted of all the trauma patients referred to the emergency department (ED). Demographic data, type and severity of injury, duration of admission, Glasgow coma scale (GCS), and revised trauma score (RTS) were recorded. The injury severity score (ISS) and NISS were calculated. The length of hospital stay was recorded during the patients follow-up and compared with ISS, NISS and modified injury scoring systems.
Results:
Five hundred eleven patients (446 males (87.3%) and 65 females (12.7%)) were enrolled in the study. The mean age was 22 ± 4.2 for males and 29.15 ± 3.8 for females. The modified NISS had a relatively strong correlation with the length of hospitalization (r = 0.79). The formula below explains the length of hospitalization according to MNISS score. Duration of hospitalization was 0.415 + (2.991) MNISS. Duration of hospitalization had a strong correlation with MISS (r = 0.805, R2: 0.65). Duration of hospitalization was 0.113 + (7.915) MISS.
Conclusions:
This new suggested scale shows a better value to predict patients’ length of hospital stay compared to ISS and NISS. However, future studies with larger sample sizes and more confounding factors such as prehospital procedures, intubation and other procedures during admission, should be designed to examine these scoring systems and confirm the results of our study.
Keywords: Multiple Trauma, Length of Stay, Injury Severity Score
1. Background
Trauma is a leading cause of morbidity and mortality among individuals under 40 and is the third main reason for death throughout the world (1, 2). The term multiple trauma is defined as trauma of multiple sites or multiple parts of the body resulting in two or more significant injuries (1). Multiple trauma usually occurs thorough falling from a height, a car accident, motorcycle accident or other motor vehicle accidents (2). Recently, numerous scoring systems have been developed to assess the severity of injury and determine patient outcome. The trauma and injury severity score (TRISS) and the injury severity score (ISS) have been widely used for estimating mortality and morbidity of patients with multiple trauma (3, 4). The abbreviated injury scale (AIS) is a scoring system for computing ISS (5). The ISS summarize the condition of patients with multiple injuries. The injury severity score considers six parts of body including head, neck, face, chest, abdomen and external areas (6). In the AIS system, each injured part of the body ranges from 1 to 6 in order to estimate the severity of trauma, in which, 1 point is allocated to a minor injury and 6 points allocated to a major and fatal injury. Other injuries are between 1 and 6 based in severity. The injury severity score is calculated by summation of squares of AIS values of the three most severely injured parts of the body. Therefore, the ISS is rated from 1 to 75 points. A fatal injury, even in a single part of the body, is equivalent to 75 in ISS. Although, ISS is widely used for trauma evaluation, it has some limitations, such as it exclusively considers the highest severe injury in a single part of the body and does not measure other milder injuries in the same body region (3, 7); thus, the new injury severity score (NISS) has been developed to overcome the limitations of ISS (8); it considers severe injuries in different body areas irrespective of affected body region (7). Many studies have been conducted to compare ISS and NISS (7, 8). The injury severity score was initially introduced to estimate the mortality of patients with trauma; however, other applications for ISS have been demonstrated in several studies (9). For example, it is estimated that, ISS can foretell the time it takes the patients to regain their health after injury (10). Also, evaluating hospital equipment and suitable care can be determined (9). Scoring systems such as ISS and NISS are the cornerstones of trauma epidemiology. Accurate assessment to manage the injury is vitally important in both clinical and research settings (11).
2. Objectives
This study was designed, for the first time, to compare our modified injury scoring systems with ISS and NISS from the point of predictive value to estimate the duration of hospitalization in trauma patients.
3. Patients and Methods
This analytical cross-sectional study was performed at the Shahid Mohammadi University Hospital of Hormozgan province in southern Iran. All of the patients referred to the emergency departments (ED) of Bandar-Abbas university hospitals with multiple trauma either, car or motorbike accident between March 2009 and March 2010 were assessed in this study; 511 patients were selected using simple sampling.
A questionnaire (or checklist) was designed to collect demographic data (age, gender) information regarding patients’ vital signs (pulse rate, respiratory rate and blood pressure), Glasgow coma scale (GCS), arrival time in ED and details about the trauma mechanism and type of injury (penetrating or blunt). The checklists were completed by an emergency specialist and a general physician. Any medical intervention or surgical procedures, morbidity or mortality during hospitalization period were recorded.
The revised trauma score, NISS and ISS were calculated for each patient using Abbreviated Injury Scale update 98 (AIS 98). Patients who had major underlying disease, those who died before arrival or those who were transferred to another medical center during the course of hospitalization were excluded.
This study was approved by the ethics committee of Hormozgan University of Medical Sciences (no. 8820). The SPSS software (Statistical Package for the Social Sciences, version 18.0, IBM company) was used to analyze data. The normality of the distribution of variables was checked by the Kolmogrov–Smirnov test. The Spearman correlation coefficient test was applied to determine the relationships and the linear regression models for the relationship between length of hospitalization and ISS or NISS. To compare the scores between patient groups, the one-way analysis of variances (ANOVA) was used. The student t-test was used to evaluate each parameter between females and males. P-values less than 0.05 were considered statistically significant.
4. Results
Five hundred eleven patients (446 males (87.3%) and 65 (12.7%) females) with a mean age of 22 ± 4.2 for males and 29.15 ± 3.8 for females were assessed.
Out of 511 patients who were followed in this study, 125 (24.5%) were admitted to the intensive care unit (ICU), 25 (4.9%) were under observation in the ED, 322 patients (63%) were admitted to other wards and 39 (7.6%) were discharged within the first hours after arrival (early discharge).
Most of the patients were scored above 13 on GCS (Table 1). Table 1 shows baseline vital features of the patients on arrival according to the RTS criteria.
Table 1. Baseline Vital Features of the Patients According to the Revised Trauma Score Criteriaa.
| Variables | Values |
|---|---|
| Respiratory Rate | |
| 6 - 14 | 5 (1) |
| 15 - 29 | 209 (40.9) |
| ≥ 30 | 297 (58.1) |
| Systolic blood pressure | |
| 50 - 74 mmHg | 5 (1) |
| 75 - 89 mmHg | 24 (4.7) |
| ≥ 90 mmHg | 482 (94.3) |
| GCS | |
| 3 | 9 (1.8) |
| 4 - 5 | 38 (7.4) |
| 5 - 8 | 31 (6.1) |
| 9 - 12 | 60 (11.7) |
| ≥ 13 | 373 (73) |
Abbreviation: GCS, Glasgow coma scale.
aValues are presented as No.(%).
Three hundred ninety-five patients (77.3%) admitted to ED underwent a surgical procedure, 248 (48.5%) orthopedic surgery, 85 (16.6%) spinal or cranial neurosurgical procedure, 21 (4.1%) general surgery and 13 (5.12%) ear nose throat (ENT) surgery were performed and 28 (5.5%) patients underwent more than a single type of operation during hospitalization.
Hospital stay ranged between 1 and 36 days (mean 6.9 ± 1.5). The mean ISS was 10.78 ± 5.5 (ranged 3 to 29) and the mean NISS was 26.74 ± 15 (4 - 81).
The mean ISS among improved patients was 9.82 ± 4.2, among patients with brain damage was 19.14 ± 4.8 and among expired patients was 23.79 ± 4.2 (P < 0.001).
The NISS score was 24.14 ± 10.8 among improved patients, 46.43 ± 17.7 among patients with brain damage and 62.3 ± 16.8 among expired patients (P < 0.001).
The mean score of ISS among patients admitted to ICU was higher than other patients. While, mean score of NISS in early discharged patients was higher than others. Table 2 shows the comparison between the mean scores of ISS and NISS among the patient groups according to admission status.
Table 2. Mean Scores of ISS and NISS in Patients According to the Admission Statusa.
| Admission Status | ISS | NISS |
|---|---|---|
| Early discharged | 4.09 ± 1.4 | 10.27 ± 2.7 |
| Under observation | 6.6 ± 5.1 | 15.16 ± 15 |
| Admitted to special wards | 9.7 ± 3.7 | 24.88 ± 9.6 |
| ICU admission | 14.06 ± 6.1 | 32.9 ± 18.1 |
| P value b | P < 0.001 c | P < 0.001 c |
Abbreviations: ICU, intensive care unit; ISS, injury severity score; NISS, new injury severity score.
adata are presented as mean ± SD.
bSignificance level less than 0.05.
cSignificant at less than 0.001.
Mean hospital stay was 9.8 days among ICU admitted patients, 2.8 days among patients under observation and 6.9 days among patients admitted to other wards (P < 0.001).
Duration of hospitalization was 3 ± 2.6 days among patients without surgery, 4.6 ± 3.6 days among patients with general surgery, 7.23 ± 3.8 days among patients with orthopedic surgery and 10.09 ± 7.56 days among patients with neurosurgical surgery. This period in patients who underwent multiple surgeries was 13.71 ± 8.77 days (P < 0.001).
Patients, who were admitted with lower GCS, had higher ISS and NISS scores. Also, the length of hospitalization was higher among patients with lower GCS. Table 3 shows the correlation between GCS and ISS, NISS and the length of hospitalization.
Table 3. Correlation Between Glasgow Coma Scale and Injury Severity Score, New Injury Severity Score and Duration of Hospitalizationa.
| Scoring Systems | GCS | P Value b | R | ||||
|---|---|---|---|---|---|---|---|
| 3 | 4 - 5 | 6 - 8 | 9 - 12 | 13 - 15 | |||
| ISS | 23.6 ± 6.1 | 15.8 ± 6.1 | 15.7 ± 5 | 11.4 ± 4.9 | 9.4 ± 4.6 | < .001 c | -0.48 |
| NISS | 65.1 ± 17.2 | 37.1 ± 17.9 | 41.1 ± 16.5 | 25.8 ± 11.2 | 23.7 ± 12.4 | < .001 c | -0.43 |
| DH, day | 11.2 ± 14.2 | 11.3 ± 9.3 | 9.4 ± 8.5 | 7.2 ± 4.2 | 6.1 ± 4.2 | < .001 c | -0.29 |
Abbreviations: DoH, duration of hospitalization. ISS, injury severity score. NISS, new injury severity score.
aData are presented as men ± SD.
bSignificance level less than 0.05.
cSignificant at less than 0.001.
Hospital stay in female patients (8.02 ± 6.7 days) was more than males (6.94 ± 5.3). However, this difference was not statistically significant (P = 0.2, 95%CI: -2.3, 0.58).
The mean score of ISS among male participants was 10.85 ± 5.5 and among females was 11.13 ± 5.86 (P = 0.9, 95% CI: -1.5, 1.37). Also, the mean score of NISS among males (26.73 ± 14.7) was lower than females (28.77 ± 16.8) (P = 0.4, 95% CI: -5.4, 2.3).The trauma scores were not significantly different between male and female patients.
The length of hospitalization had a significant correlation with the RTS criteria such as respiratory rate (P <0.001), blood pressure (P < 0.034) and GCS (P < 0.001).
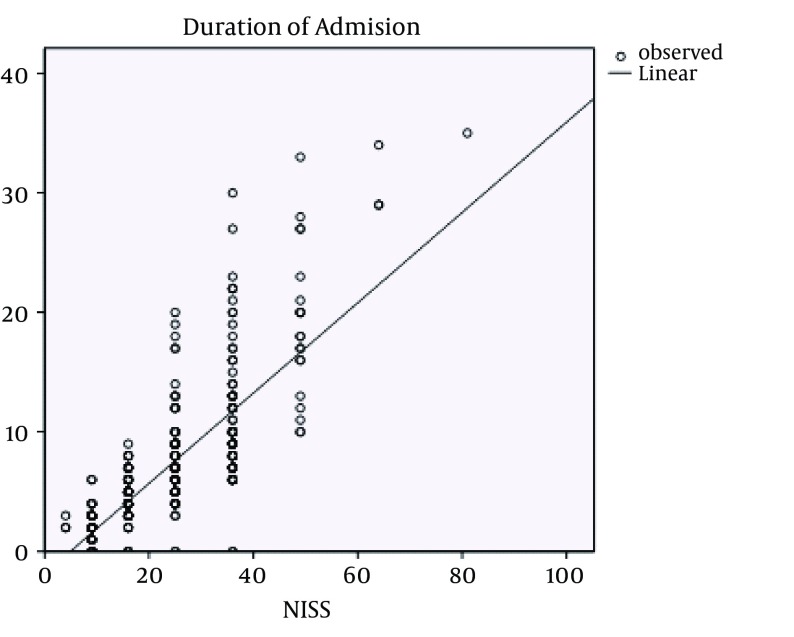
There was a poor correlation between duration of hospitalization and NISS score (r = 0.36 and R2 = 0.13%). That means NISS score could predict 13% of hospitalization period changes.
Using the linear regression model analysis, duration of hospitalization was calculated by the following equation:
| (1) |
Figure 1 shows the direct linear correlation between NISS score and duration of hospital stay.
Figure 1. Correlation Between New Injury Severity Score and Duration of Hospitalization.
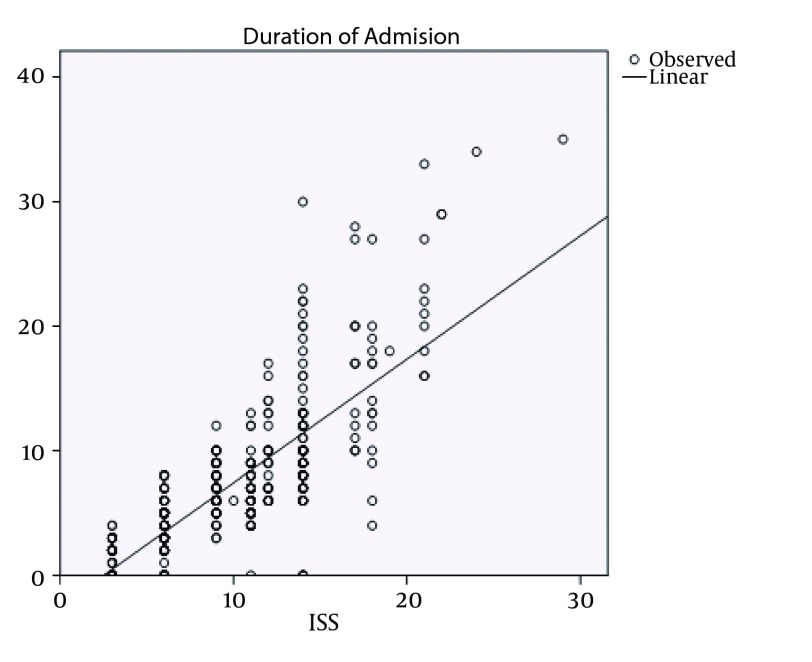
The results showed that, duration of hospitalization had a relatively strong correlation with ISS score (r = 0.78), and approximately 0.62% of hospitalization period could be explained by ISS score (R square = 0.619).
Below is the linear equation according to regression analysis:
| (2) |
In Figure 2, the correlation of ISS scores and duration of hospitalization are displayed.
Figure 2. Correlation Between Injury Severity Score and Duration of Hospitalization.
The results showed a moderate correlation between the length of hospitalization and RTS score (r = 0.56, R2: 0.31).
The length of hospitalization according to RTS score are demonstrated in the formula below:
| (3) |
In this study we examined a new scoring system, in which, ISS score was divided by RTS score (ISS/RTS). Also, the NISS score was divided by RTS (NISS/RTS), and we called these systems modified ISS (MISS) and modified NISS (MNISS), respectively.
The modified NISS had a relatively strong correlation with the length of hospitalization (r = 0.79).
The formula below explains the length of hospitalization according to MNISS score.
Duration of hospitalization = 0.415 + (2.991) modified NISS. Duration of hospitalization had a strong correlation with MISS (r = 0.805, R2: 0.65).
| (4) |
5. Discussion
This study was performed to assess the correlation between duration of hospital stay and injury severity scoring systems including ISS, NISS, MISS and MNISS in trauma patients. The results showed that, most of the patients with multiple trauma were male. This finding was consistent with the studies conducted by George et al. (12), Dongel et al. (13) and Brongel (14). Some studies have examined the length of hospitalization in trauma patients and indicated that prehospital interventions such as endotracheal intubation and other procedures performed by EMS teams at the trauma field can be associated with other complications such as pneumonia and higher mortality rates (15, 16). For example, in a prospective review of 191 patients, Bochicchio and colleagues (17) compared outcomes between the field intubated patients and hospital intubated patients. The authors concluded that the frequency of ICU admission and hospital stay duration are more in pre-hospital intubated patients (17). Also, in another study, prehospital intubation performed by EMS, increased the risk of pneumonia more than four times (16). Our results showed that hospitalization length in patients transported to ED by EMS was higher than those who transported by personal vehicle. This may be due to ventilation associated pneumonia or other complications, which are induced by paramedics in the trauma field.
According to our study, ISS is a better scoring system as a predictor of hospitalization length compared to NISS, and ISS should not be replaced with NISS. Also, MISS and MNISS are better predictors of hospitalization length compared with ISS and NISS. Our results showed that MISS was the best predictor among the scoring systems. In a prospective review of 891 trauma patients in Beirut, Hala Tamim and colleagues compared the predictive power of ISS and NISS for mortality, ICU admission and the length of hospital stay for 2 years. The authors concluded that, ISS is a better predictor for ICU admission and hospitalization length than NISS, but that was not a good predictor of patient survival (18).
Another study, which is inconsistent with our study, conducted in Canada compared the NISS and ISS among 23,909 patients. The authors concluded that, the length of hospital stay and ICU admission could be better predicted by NISS than ISS (19). Many studies have been conducted to compare the ISS and NISS value to predict the length of hospital stay of patients (18-20). The results of these studies are conflicting. Some studies have shown that, the predicting power of ISS and NISS are generally equivalent in in patients with minor injury. While, some others demonstrated that, the NISS is a better predictor than ISS in patients with moderate to severe injury (19).
The MISS is not only an anatomical scoring system, but also is a system that takes physiologic status, and vital features of patients into account. On the other hand, many limitations have been reported for ISS and NISS. The injury severity score considers only a single injury for each region and may underestimate the severity of damages, while NISS is possible to overestimate each region’s injury (20). Accordingly, as indicated in our study, MISS and MNISS seem to be more appropriate for predicting the duration of hospital stay in patients with multiple trauma. This study did not consider the effect of some confounding factors such as patients’ age and its’ role has been confirmed in other studies and may affect study results (19, 21).
In this study we recommended a modified scoring system (MISS and MNISS) in order to predict the length of hospitalization in multiple trauma patients. This new suggested scale showed a better value to predict patients’ length of hospital stay compared to ISS and NISS. However, future studies with larger sample sizes and consideration of more confounding factors are needed to examine these scoring systems and confirm the results of our study.
Acknowledgments
We thank the Hormozgan University of Medical Sciences and the emergency medical service teams for their valuable help and all who patiently cooperated in this study.
Footnotes
Authors’ Contribution:Seyed Ashkan Tabibzadeh Dezfuli: Study concept and design, acquisition and, Analysis of data, interpretation and making final conclusion of the results, writing and editing the article; Seyed Shojaeddin Namazi: Edition of the article; Oveis Salehi: Study design, acquisition of data, and study supervision, analysis of data, interpretation and making final conclusion of the results, writing and editing the article; Morteza Saeedi: Critical revision of the manuscript for important intellectual content.
References
- 1.Karakus A, Kekec Z, Akcan R, Seydaoglu G. The relationship of trauma severity and mortality with cardiac enzymes and cytokines at multiple trauma patients. Ulus Travma Acil Cerrahi Derg. 2012;18(4):289–95. doi: 10.5505/tjtes.2012.81488. [DOI] [PubMed] [Google Scholar]
- 2.Hodgson NF, Stewart TC, Girotti MJ. Autopsies and death certification in deaths due to blunt trauma: what are we missing? Can J Surg. 2000;43(2):130–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Tohira H, Jacobs I, Mountain D, Gibson N, Yeo A. Comparisons of the Outcome Prediction Performance of Injury Severity Scoring Tools Using the Abbreviated Injury Scale 90 Update 98 (AIS 98) and 2005 Update 2008 (AIS 2008). Ann Adv Automot Med. 2011;55:255–65. [PMC free article] [PubMed] [Google Scholar]
- 4.Kuhls DA, Malone DL, McCarter RJ, Napolitano LM. Predictors of mortality in adult trauma patients: the physiologic trauma score is equivalent to the Trauma and Injury Severity Score. J Am Coll Surg. 2002;194(6):695–704. doi: 10.1016/s1072-7515(02)01211-5. [DOI] [PubMed] [Google Scholar]
- 5.Lesko MM, Woodford M, White L, O'Brien SJ, Childs C, Lecky FE. Using Abbreviated Injury Scale (AIS) codes to classify Computed Tomography (CT) features in the Marshall System. BMC Med Res Methodol. 2010;10:72. doi: 10.1186/1471-2288-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehsaei MR, Sarreshtedar A, Ashraf H, Karimiani EG. Trauma Mortality: Using Injury Severity Score (ISS) for Survival Prediction in East of Iran. Razavi Int J Med . 2014;2(1):15189. [Google Scholar]
- 7.Whitaker IY, Gennari TD, Whitaker AL. The difference between ISS and NISS in a series of trauma patients in Brazil. Annu Proc Assoc Adv Automot Med. 2003;47:301–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Jamulitrat S, Sangkerd P, Thongpiyapoom S, Na Narong M. A comparison of mortality predictive abilities between NISS and ISS in trauma patients. J Med Assoc Thai. 2001;84(10):1416–21. [PubMed] [Google Scholar]
- 9.Stevenson M, Segui-Gomez M, Lescohier I, Di Scala C, McDonald-Smith G. An overview of the injury severity score and the new injury severity score. Inj Prev. 2001;7(1):10–3. doi: 10.1136/ip.7.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glancy KE, Glancy CJ, Lucke JF, Mahurin K, Rhodes M, Tinkoff GH. A study of recovery in trauma patients. J Trauma. 1992;33(4):602–9. doi: 10.1097/00005373-199210000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Emircan S, Ozguc H, Akkose Aydin S, Ozdemir F, Koksal O, Bulut M. Factors affecting mortality in patients with thorax trauma. Ulus Travma Acil Cerrahi Derg. 2011;17(4):329–33. [PubMed] [Google Scholar]
- 12.George RL, McGwin Jr G, Windham ST, Melton SM, Metzger J, Chaudry IH, et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock. 2003;19(1):28–32. doi: 10.1097/00024382-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Dongel I, Coskun A, Ozbay S, Bayram M, Atli B. Management of thoracic trauma in emergency service: Analysis of 1139 cases. Pak J Med Sci. 2013;29(1):58–63. doi: 10.12669/pjms.291.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brongel L. One-day surgery in multiple trauma patients. Przegl Lek. 2000;57 Suppl 5:133–5. [PubMed] [Google Scholar]
- 15.Murray JA, Demetriades D, Berne TV, Stratton SJ, Cryer HG, Bongard F, et al. Prehospital intubation in patients with severe head injury. J Trauma. 2000;49(6):1065–70. doi: 10.1097/00005373-200012000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Sloane C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19(3):259–64. doi: 10.1016/s0736-4679(00)00235-3. [DOI] [PubMed] [Google Scholar]
- 17.Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, Scalea TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J Trauma. 2003;54(2):307–11. doi: 10.1097/01.TA.0000046252.97590.BE. [DOI] [PubMed] [Google Scholar]
- 18.Tamim H, Al Hazzouri AZ, Mahfoud Z, Atoui M, El-Chemaly S. The injury severity score or the new injury severity score for predicting mortality, intensive care unit admission and length of hospital stay: experience from a university hospital in a developing country. Injury. 2008;39(1):115–20. doi: 10.1016/j.injury.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The Injury Severity Score or the New Injury Severity Score for predicting intensive care unit admission and hospital length of stay? Injury. 2005;36(4):477–83. doi: 10.1016/j.injury.2004.09.039. [DOI] [PubMed] [Google Scholar]
- 20.Balogh ZJ, Varga E, Tomka J, Suveges G, Toth L, Simonka JA. The new injury severity score is a better predictor of extended hospitalization and intensive care unit admission than the injury severity score in patients with multiple orthopaedic injuries. J Orthop Trauma. 2003;17(7):508–12. doi: 10.1097/00005131-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Koksal O, Ozdemir F, Bulut M, Aydin S, Almacioglu ML, Ozguc H. Comparison of trauma scoring systems for predicting mortality in firearm injuries. Ulus Travma Acil Cerrahi Derg. 2009;15(6):559–64. [PubMed] [Google Scholar]