Abstract
We performed a retrospective interventional case series including 80 eyes of 48 patients with keratoconus (KC) who were treated with modified corneal cross-linking (CXL) for KC (with a partial deepithelization in a pattern of stripes). The average follow-up was 5.8 years (with a minimum of 5 years). At the last follow-up visit, compared with preoperative values, there were no significant changes in spherical equivalent, average keratometry, corneal thickness, corneal hysteresis, or corneal resistance factor. The distance-corrected visual acuity was 20/39 preoperatively and 20/36 postoperatively (P = 0.3). The endothelial cell count decreased by 4.7% (P < 0.005). These findings suggest that this modified corneal CXL technique is a safe and effective alternative to halt the progression of KC up to five years after the procedure. However, some concerns remain as to whether this technique can affect in some degree the corneal endothelial cells.
Keywords: keratoconus, corneal cross-linking, corneal ectasia
Introduction
It has been more than one decade since the description of corneal collagen cross-linking (CXL) as a treatment option for corneal ectatic disease.1 Since then, multiple studies have shown that CXL has effects on slowing keratoconus (KC) progression.1–21 These results, combined with the low incidence of complications and adverse effects, have allowed an exponential increase in the implementation of CXL as a primary treatment for progressive KC, with quite favorable results, although long-term effect and more clear metrics for progression in KC are still a concern.2–7
There are few long-term studies properly assessing all the safety and efficacy variables; however, due to different inclusion criteria and surgical techniques in these studies, the evidence on this topic with regard to its long-term effects remains controversial.4–9,15,17–21 Standard corneal CXL technique includes total epithelium removal in around the central 7–9 mm in diameter, in order to increase riboflavin concentration in the corneal stroma: the so-called epithelium-off or epi-off technique.1–9 However, other alternatives have been used, including transepithelial riboflavin application: the epithelium-on or epi-on techniques.22–28
Some modifications of the standard technique, including partial corneal full-thickness deepithelization, have been also reported, including a study with a group of 40 eyes followed up for five years.14–16
The aim of the present study was to determine the safety and efficacy of CXL with partial full-thickness epithelium removal for the treatment of progressive KC at five years of follow-up in a group of 80 eyes, which is according to our knowledge the largest group of eyes with long-term results, using this modified technique, ever published.
Patients and Methods
We performed a retrospective nonrandomized study of 80 eyes of 48 patients with progressive KC who had been treated with corneal CXL between April 2007 and March 2010 at Centro Oftalmologico Virgilio Galvis – Fundacion Oftalmologica de Santander (FOSCAL, Floridablanca, Colombia). The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Ethics Committee.
Patients wearing contact lenses discontinued their use four weeks before examinations. Exclusion criteria included history of any other ocular pathology, autoimmune systemic diseases, and previous intraocular or corneal surgery.
In all cases, pilocarpine 2% was applied around one hour before the surgery to assure miosis during the procedure and proparacaine 0.5% just before the surgery. Initially, using a spatula, the corneal epithelium was removed in vertical full-thickness stripes, 1–1.5 mm wide with 1 mm distance between them, within 9 mm central corneal (Fig. 1). Afterward, riboflavin drops (0.1% in 20% dextran) were instilled onto the cornea at five-minute intervals for half an hour, within a LASEK well, which was maintained with gentle pressure on the corneal surface for a couple of minutes, so that riboflavin was kept in close contact with the deepithelized portions of the cornea. Thereafter, 3 mW/cm2 ultraviolet-A (UV-A) light (370 nm wavelength) was applied to the cornea for 30 minutes at a working distance of 5 cm, using the UV-X Illumination System (IROC). Topical riboflavin was applied every five minutes during the UV light exposure.
Figure 1.

Partial full-thickness deepithelization in a stripe pattern, used in the patients with KC. Four to five 1–1.5 mm wide vertical strips, around 1 mm apart, comprising approximately the central 9 mm of the cornea, were performed.
Uncorrected and corrected distance visual acuity (UDVA and CDVA), corneal topography (Bausch and Lomb), corneal hysteresis (Ocular Response Analyzer; Reichert), corneal resistance factor (Ocular Response Analyzer, Reichert), endothelial cell count (Specular Microscope SP-3000P; Topcon), corneal pachymetry (Visante OCT; Zeiss), and a complete ophthalmic examination, including anterior segment and dilated biomicroscopic fundus examination, were recorded preoperatively and five years or longer after the surgery.
The Snellen visual acuity chart was used to determine visual acuity, which was then was converted to logarithm of the minimum angle of resolution (logMAR) units for statistical analysis.
Statistical analysis was performed with STATA 11.2 software package (Stata Corporation).
Results
A total of 80 eyes of 48 Hispanic patients with a diagnosis of KC treated with corneal CXL were included, of which 29 patients were males and 19 patients were females. The mean age of the patients was 29.3 ± 8.2 years (range 17–44 years). The mean follow-up length was 5.8 years (range 5.0–7.9 years). Stabilization of KC was achieved in all eyes after CXL treatment. On postoperative clinical examinations, mild corneal haze in an irregular pattern was observed in the anterior and mid corneal stroma in around 30% of the cases, but we did not see a clear demarcation line. Anterior segment OCT did not show the demarcation line either.
Some nonsignificant changes were observed across the follow-up period in several variables. Within one year after the procedure, refractive sphere and cylinder tended to diminish, but later both reached values similar to those in the preoperative examination (Fig. 2). A similar trend was found for keratometries: they tended to decrease at one- and two-year time points, but increased to preoperative values at the last follow-up examination (Fig. 3). There was a nonstatistically significant trend to increase in pachymetry at one-year time point (Fig. 4).
Figure 2.
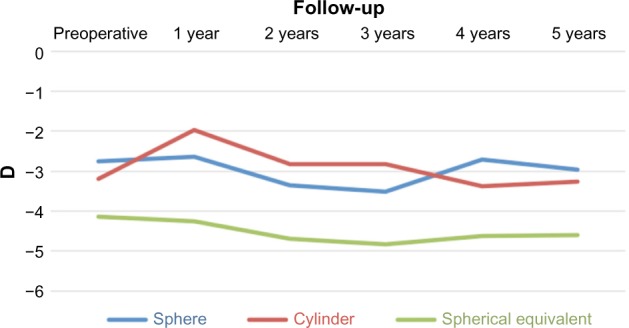
Refraction across the follow-up period.
Figure 3.
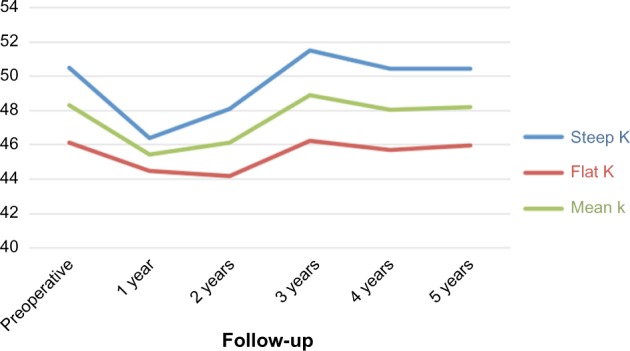
Keratometries (diopters) across the follow-up period.
Figure 4.
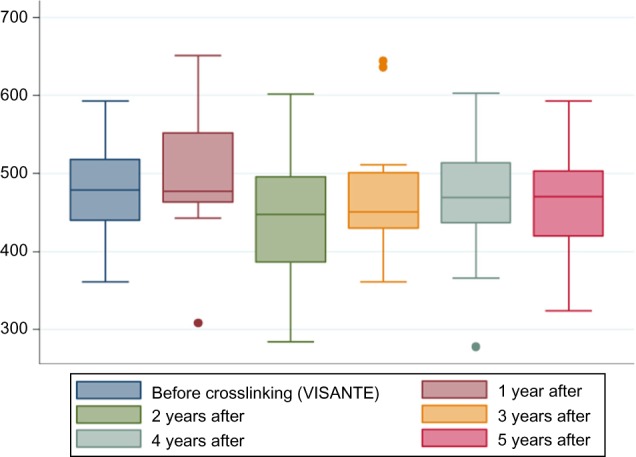
Pachymetry values (microns) across the follow-up period.
At final follow-up, the sphere, cylinder, and spherical equivalent showed no statistically significant changes [spherical equivalent −4.41 ± 3.43 diopters (D) preoperatively and −4.6 ± 3.31 D postoperatively; P = 0.72]. The flatter, stepper, and average mean keratometry changes were not statistically significant. The distance-corrected visual acuity (DCVA) showed a mild improvement, from 20/39 preoperatively to 20/36 postoperatively, which did not reach statistical significance (P = 0.3). 81.25% of eyes did not present a decrease in DCVA. There were no significant changes in corneal thickness, corneal hysteresis, or corneal resistance factor. Table 1 summarizes the measured values at baseline and at the last follow-up visit. The endothelial cell count five years or longer after the procedure (measured in the same corneal location with the same specular microscope) decreased by 4.7% ± 7.2% (P = 0.005). No complications presented during the follow-up period.
Table 1.
Preoperative and last follow-up findings (n = 80 eyes).
| PRE QX DATA (MEAN ± SD) |
POP QX DATA (MEAN ± SD) |
P | |
|---|---|---|---|
| Sphere (D) | −2.79 ± 3.04 | −3.02 ± 3.08 | 0.64 |
| Cylinder* (D) | −3.22 ± 2.07 | −3.15 ± 1.84 | 0.82 |
| Spherical equivalent (D) | −4.41 ± 3.43 | −4.6 ± 3.31 | 0.72 |
| Flatter keratometry (D) | 46.2 ± 4.1 | 45.7 ± 4.4 | 0.46 |
| Steeper keratometry (D) | 50.5 ± 5.8 | 50.5 ± 6.14 | 1.0 |
| Mean keratometry (D) | 48.4 ± 4.8 | 48.3 ± 5.1 | 0.9 |
| Distance corrected visual acuity (LogMAR) | 0.29 ± 0.25 | 0.25 ± 0.24 | 0.3 |
| Pachymetry (microns) | 470 ± 52.2 | 471 ± 60.5 | 0.91 |
| Endothelial count (cells/mm2) | 2715 ± 317 | 2552 ± 263 | 0.005 |
| Corneal hysteresis | 8.76 ± 1.46 | 8.40 ± 1.85 | 0.17 |
| Corneal resistance factor | 7.58 ± 1.54 | 7.52 ± 2.11 | 0.39 |
Note:
Negative cylinder notation.
Discussion
CXL is currently an accepted technique in the treatment of KC. 83.3% of the members of the Group of Panelists for the Global Delphi Panel of Keratoconus and Ectatic Diseases, published in 2015, were performing the procedure, and those who did not have access to CXL were willing to use this technique once it became available in their countries.29 Since the pioneering study by Wollensak et al, the concept of including complete full-thickness corneal epithelium removal for corneal CXL was the rule (epi-off).1–3 Several studies, most of them retrospective, have shown that epi-off corneal CXL is effective in halting the progression of KC.1–21 However, over the last decade, epi-on techniques have slowly gained popularity, especially using diverse substances, such as benzalkonium chloride or ethylenediaminetetraacetic acid (EDTA), to disrupt the epithelial surface expecting to facilitate absorption of the photosensitizer.22–28 On the other hand, both experimental and clinical results have shown more CXL effect using an epi-off technique.25–27 The use of iontophoresis along with a hypoosmolar riboflavin 0.1% dextran-free solution enriched with EDTA and trometamol, to increase riboflavin uptake by the stroma through the intact epithelium, seems to improve the effect.30 Combined measures to enhance the riboflavin penetration through corneal epithelium have been used: benzalkonium chloride preoperative medication; hypotonic riboflavin solution without dextran and with increased concentration (0.5%); and prolongation of the time of application of topical riboflavin until objective verification of the stromal saturation is confirmed.31 The evidence so far is that epi-off CXL remains the most effective method of strengthening the cornea and slowing KC progression, but according to new evidence, some epi-on methods are promising.28,30–32 Other alternatives that could be considered a midpoint between the epi-off and epi-on techniques involve epithelial disruption using a specially designed metallic device (Daya Disruptor; Duckworth and Kent)33,34 or creation of microabrasions by placing a surgical sponge over the corneal surface while the patient is blinking.35 Other researcher have performed partial thickness epithelial removal using excimer laser, but it required a longer application of riboflavin to achieve corneal saturation.36
As previously mentioned, other approaches involve full-thickness partial deepithelization.14–16 Razmjoo et al published the results of their study where in one group of 22 eyes they left untouched the central 3 mm and removed an outer ring (3 mm width) of corneal epithelium, and in another group of 22 eyes, they performed total epithelium removal over 9 mm. They found that six months after surgery, the partial deepithelization group had slightly better postoperative DCVA. No changes in sphere and cylinder were found in both groups. No significant difference was found between the groups, regarding the postoperative steeper keratometry. However, a significant improvement of that value was observed in patients treated with total removal CXL, while patients treated with partial removal of the corneal epithelium did not reveal a significant improvement. The authors concluded that there was no significant difference between these two methods, but recognized that a significant weakness of their study was the short-term follow-up.14 Recently, however, they informed that they had abandoned the partial deepithelization technique due to the presence of haze, corneal thinning, and endothelial cell damage in intact epithelial central region (Peyman A, personal communication, January 1, 2016). Hashemi et al reported results at five years after corneal CXL with partial epithelium removal in 40 eyes, showing stabilization of the disease.15 Recently, they also reported middle-term (one year) results comparing corneal CXL with partial deepithelization versus total epithelium removal. Both groups showed similar results in terms of UDVA, with small differences in DCVA, central corneal thickness, and corneal flattening.16 Some other authors have also used different variants of partial deepithelization but their reports included only very small groups of eyes.37–39
With regard to the duration of the effect of corneal CXL, a systematic review and meta-analysis published by Craig et al found statistically significant improvements in topography, visual acuity, astigmatism, and refraction at 12 months after the operation. However, they stated that uncertainty is the long-term benefit in avoiding or delaying disease progression.40 Studies showing results of CXL with a minimum follow-up of 48 months, with any technique, are scarce. We conducted a literature review and identified only six publications.15,17–21 All these six long-term studies showed stabilization or improvement of the ectatic disease in all or most of the eyes, which is consistent with our results. Only one of the long-term studies (by Hashemi et al) included a technique different to complete full-thickness corneal deepithelization.15 As already mentioned, they used a partial deepithelization of the cornea in a pattern very similar to the approach we used in our patients. The issue of whether the partial debridement may affect the effect of cross-linking is still a controversial point. Experimentally, Hayes et al performed superficial epithelial trauma by scraping of the superficial epithelium for 1015 seconds with a scalpel blade and using visual inspection to ensure that the basal layers were intact, in porcine eyes. They found normality of the transmission spectra of those corneas, which suggested the need to remove all epithelial cell layers in order to permit stromal penetration of riboflavin.41 A significant difference with the approach that we (and also Hashemi et al)15,16 used is that in the areas deepithelized, basal layers were also removed.
Ozmen et al performed partial-thickness epithelial ablation with an excimer laser in rabbit eyes, preserving one to four layers of cells, and found after CXL that no keratocyte loss occurred, which is considered a surrogate marker of successful CXL.42 Again, a critical difference with our technique is that the epithelium is completely removed in the scraped areas.
Samaras et al performed a full-thickness grid pattern removal of epithelium in porcine corneas, more similar to the approach we used in our clinical series.43 The pattern consisted of 30–40 separate abrasions placed within an area of approximately 7 mm in diameter. They observed areas of yellow coloration in the stroma in a grid pattern beneath the areas of full-thickness epithelial debridement. They considered that because of the lack of homogeneous absorption, complete removal of the corneal epithelium appeared to be necessary to permit enough riboflavin absorption into the stroma. This seems a valid argument, but when looking at the figure shown in their article, we consider that the percentage of epithelial removal in our patients was larger, and it could influence the amount of riboflavin entering into the corneal stroma (Fig. 1).
CXL is not a free-of-complications procedure. Microbial keratitis (including bacterial, herpetic, mycotic, and Acanthamoeba), leukomas, keratouveitis, endothelial cell failure with corneal edema, corneal melting, and corneal perforation have been reported.44–54 Partial deepithelization could allow for a faster recovery of the corneal surface, and thereby reduce the risk of infectious or inflammatory conditions.
With regard to corneal endothelial cell reduction, in our study, we found that cell count decreased by 4.7% during the five years of follow-up. Considering the physiological annual loss of 0.6%,55 we estimated an additional endothelial loss of only 1.7% in five years. It is difficult to assert whether this amount of additional cell loss is clinically significant. Factors such as the variability of endothelial cell count obtained with the specular microscopes might have influenced the result. However, close follow-up is warranted in these patients.
Conclusion
Performing cross-linking with partial corneal deepithelization provided good results in terms of long-term stabilization of KC in a group of 80 eyes followed up for at least five years, because we did not find statistically significant differences in refraction, keratometries, and pachymetries. However, further studies are warranted to determine if the loss of corneal endothelial cells that we found in this series reaches clinical significance in a larger group of eyes. Our results are consistent with the only other study published with a similar technique and a similar period of follow-up, which included 40 eyes. With regard to objective signs of corneal cross-linking, Hashemi et al did not mention the demarcation line in their study with a similar technique.15 We did not see a clear demarcation line in our cases. Further studies with a larger number of eyes and with longer follow-up times are needed to determine if the absence of this sign correlates with less cross-linking effect and to confirm if this partial deepithelization approach could be considered a good alternative to the standard total corneal deepithelization cross-linking procedure.
Footnotes
ACADEMIC EDITOR: Joshua Cameron, Editor in Chief
PEER REVIEW: Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 625 words, excluding any confidential comments to the academic editor.
FUNDING: This study was supported in part by a grant (code C34059) from Universidad Autonóma de Bucaramanga (Bucaramanga, Colombia) and in part by resources from Centro Oftalmológico Virgilio Galvis (Floridablanca, Colombia). The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE). Provenance: the authors were invited to submit this paper.
Author Contributions
Conceived and designed the experiments: VG, AT, NIC. Analyzed the data: AT, NIC, AIO, RB, CJR, MEO. Wrote the first draft of the manuscript: AIO, RB, AT. Contributed to the writing of the manuscript: CJR. Agreed with manuscript results and conclusions: VG, NIC, MEO. Jointly developed the structure and arguments for the paper: AT, AIO, CJR. Made critical revisions and approved the final version: VG, NIC. All the authors reviewed and approved the final manuscript.
REFERENCES
- 1.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen cross-linking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Chan E, Snibson GR. Current status of corneal collagen cross-linking for keratoconus: a review. Clin Exp Optom. 2013;96:155–64. doi: 10.1111/cxo.12020. [DOI] [PubMed] [Google Scholar]
- 3.Alhayek A, Lu PR. Corneal collagen crosslinking in keratoconus and other eye disease. Int J Ophthalmol. 2015;18(8):407–18. doi: 10.3980/j.issn.2222-3959.2015.02.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown SE, Simmasalam R, Antonova N, Gadaria N, Asbell PA. Progression in keratoconus and the effect of corneal cross-linking on progression. Eye Contact Lens. 2014;40:331–8. doi: 10.1097/ICL.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 5.Randleman JB, Khandelwal SS, Hafezi F. Corneal cross-linking. Surv Ophthalmol. 2015;60:509–23. doi: 10.1016/j.survophthal.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Sorkin N, Varssano D. Corneal collagen crosslinking: a systematic review. Ophthalmologica. 2014;232:10–27. doi: 10.1159/000357979. [DOI] [PubMed] [Google Scholar]
- 7.Mastropasqua L. Collagen cross-linking: when and how? A review of the state of the art of the technique and new perspectives. Eye Vis (Lond) 2015;29(2):19. doi: 10.1186/s40662-015-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chunyu T, Xiujun P, Zhengjun F, Xia Z, Feihu Z. Corneal collagen cross-linking in keratoconus: a systematic review and meta-analysis. Sci Rep. 2014;4:5652. doi: 10.1038/srep05652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brart DP. Corneal collagen cross-linking: a review. J Optom. 2014;7:113–24. doi: 10.1016/j.optom.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yildirim A, Cakir H, Kara N, et al. Corneal collagen crosslinking for ectasia after laser in situ keratomileusis: long-term results. J Cataract Refract Surg. 2014;40:1591–6. doi: 10.1016/j.jcrs.2014.01.042. [DOI] [PubMed] [Google Scholar]
- 11.Shetty R, Pahuja NK, Nuijts RM, et al. Current protocols of corneal collagen cross-linking: visual, refractive, and tomographic outcomes. Am J Ophthalmol. 2015;160:243–9. doi: 10.1016/j.ajo.2015.05.019. [DOI] [PubMed] [Google Scholar]
- 12.De Bernardo M, Capasso L, Lanza M, et al. Long-term results of corneal collagen crosslinking for progressive keratoconus. J Optom. 2015;8:180–6. doi: 10.1016/j.optom.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kymionis GD, Grentzelos MA, Liakopoulos DA, et al. Long-term follow-up of corneal collagen cross-linking for keratoconus-the Cretan study. Cornea. 2014;33:1071–9. doi: 10.1097/ICO.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 14.Razmjoo H, Rahimi B, Kharraji M, Koosha N, Peyman A. Corneal haze and visual outcome after collagen crosslinking for keratoconus: a comparison between total epithelium off and partial epithelial removal methods. Adv Biomed Res. 2014;3:221. doi: 10.4103/2277-9175.145677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hashemi H, Seyedian MA, Miraftab M, Fotouhi A, Asgari S. Corneal collagen cross-linking with riboflavin and ultraviolet A irradiation for keratoconus: long-term results. Ophthalmology. 2013;120:1515–20. doi: 10.1016/j.ophtha.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Hashemi H, Miraftab M, Hafezi F, Asgari S. Matched comparison study of total and partial epithelium removal in corneal cross-linking. J Refract Surg. 2015;31:110–5. doi: 10.3928/1081597X-20150122-06. [DOI] [PubMed] [Google Scholar]
- 17.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet A corneal collagen cross-linking for keratoconus in Italy: the Siena eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41:41–6. doi: 10.1016/j.jcrs.2014.09.033. [DOI] [PubMed] [Google Scholar]
- 19.Poli M, Lefevre A, Auxenfans C, Burillon C. Corneal collagen cross-linking for the treatment of progressive corneal ectasia: 6-year prospective outcome in a French population. Am J Ophthalmol. 2015;160:654–62. doi: 10.1016/j.ajo.2015.06.027. [DOI] [PubMed] [Google Scholar]
- 20.O’Brart DP, Kwong TQ, Patel P, McDonald RJ, O’Brart NA. Long-term follow-up of riboflavin/ultraviolet A (370 nm) corneal collagen cross-linking to halt the progression of keratoconus. Br J Ophthalmol. 2013;97:433–7. doi: 10.1136/bjophthalmol-2012-302556. [DOI] [PubMed] [Google Scholar]
- 21.O’Brart DP, Patel P, Lascaratos G, et al. Corneal cross-linking to halt the progression of keratoconus and corneal ectasia: seven-year follow-up. Am J Ophthalmol. 2015;160:1154–63. doi: 10.1016/j.ajo.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 22.Chan CC, Sharma M, Walcher BS. Effect of inferior-segment Intacs with and without C3-R on keratoconus. J Cataract Refract Surg. 2007;33:75–80. doi: 10.1016/j.jcrs.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Leccisotti A, Islam T. Transepithelial corneal collagen crosslinking in keratoconus. J Refract Surg. 2010;26:942–8. doi: 10.3928/1081597X-20100212-09. [DOI] [PubMed] [Google Scholar]
- 24.Boxer Wachler BS, Pinelli R, Ertan A, Chan CC. Safety and efficacy of transepithelial crosslinking (C3-R/CXL) J Cataract Refract Surg. 2010;36:186–8. doi: 10.1016/j.jcrs.2009.08.019. author rely 188–9. [DOI] [PubMed] [Google Scholar]
- 25.Buzzonetti L, Petrocelli G. Transepithelial corneal cross-linking in pediatric patients: early results. J Refract Surg. 2012;28:763–7. doi: 10.3928/1081597X-20121011-03. [DOI] [PubMed] [Google Scholar]
- 26.Tao X, Yu H, Zhang Y, et al. Role of corneal epithelium in riboflavin/ultraviolet-A mediated corneal cross-linking treatment in rabbit eyes. Biomed Res Int. 2013;2013:624563. doi: 10.1155/2013/624563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caporossi A, Mazzotta C, Paradiso AL, Baiocchi S, Marigliani D, Caporossi T. Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results. J Cataract Refract Surg. 2013;39:1157–63. doi: 10.1016/j.jcrs.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 28.Raiskup F, Veliká V, Veselá M, Spörl E. Cross-linking in keratoconus: “Epi-off” or “Epi-on”? Klin Monbl Augenheilkd. 2015;232:1392–6. doi: 10.1055/s-0035-1546155. [DOI] [PubMed] [Google Scholar]
- 29.Gomes JA, Tan D, Rapuano CJ, et al. Group of panelists for the global delphi panel of keratoconus and ectatic diseases. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34:359–69. doi: 10.1097/ICO.0000000000000408. [DOI] [PubMed] [Google Scholar]
- 30.Buzzonetti L, Petrocelli G, Valente P, Iarossi G, Ardia R, Petroni S. Iontophoretic transepithelial corneal cross-linking to halt keratoconus in pediatric cases: 15-month follow-up. Cornea. 2015;34:512–5. doi: 10.1097/ICO.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 31.Stojanovic A, Zhou W, Utheim TP. Corneal collagen cross-linking with and without epithelial removal: a contralateral study with 0.5% hypotonic riboflavin solution. Biomed Res Int. 2014;2014:619398. doi: 10.1155/2014/619398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shalchi Z, Wang X, Nanavaty MA. Safety and efficacy of epithelium removal and transepithelial corneal collagen crosslinking for keratoconus. Eye (Lond) 2015;29:15–29. doi: 10.1038/eye.2014.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rechichi M, Daya S, Scorcia V, Meduri A, Scorcia G. Epithelial-disruption collagen crosslinking for keratoconus: one-year results. J Cataract Refract Surg. 2013;39:1171–8. doi: 10.1016/j.jcrs.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 34.Samaras KE, Lake DB. Corneal collagen cross linking (CXL): a review. Int Ophthalmol Clin. 2010;50:89–100. doi: 10.1097/IIO.0b013e3181e20df6. [DOI] [PubMed] [Google Scholar]
- 35.Stojanovic A, Chen X, Jin N, et al. Safety and efficacy of epithelium-on corneal collagen cross-linking using a multifactorial approach to achieve proper stromal riboflavin saturation. J Ophthalmol. 2012;2012:498435. doi: 10.1155/2012/498435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bakke EF, Stojanovic A, Chen X, Drolsum L. Penetration of riboflavin and postoperative pain in corneal collagen crosslinking: excimer laser superficial versus mechanical full-thickness epithelial removal. J Cataract Refract Surg. 2009;35:1363–6. doi: 10.1016/j.jcrs.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 37.Kymionis GD, Diakonis VF, Coskunseven E, Jankov M, Yoo SH, Pallikaris IG. Customized pachymetric guided epithelial debridement for corneal collagen cross linking. BMC Ophthalmol. 2009;9:10. doi: 10.1186/1471-2415-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaya V, Utine CA, Yilmaz OF. Efficacy of corneal collagen cross-linking using a custom epithelial debridement technique in thin corneas: a confocal microscopy study. J Refract Surg. 2011;27:444–50. doi: 10.3928/1081597X-20101201-01. [DOI] [PubMed] [Google Scholar]
- 39.Mazzotta C, Ramovecchi V. Customized epithelial debridement for thin ectatic corneas undergoing corneal cross-linking: epithelial island cross-linking technique. Clin Ophthalmol. 2014;8:1337–43. doi: 10.2147/OPTH.S66372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Craig JA, Mahon J, Yellowlees A, et al. Epithelium-off photochemical corneal collagen cross-linkage using riboflavin and ultraviolet A for keratoconus and keratectasia: a systematic review and meta-analysis. Ocul Surf. 2014;12:202–14. doi: 10.1016/j.jtos.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 41.Hayes S, O’Brart DP, Lamdin LS, et al. Effect of complete epithelial debridement before riboflavin-ultraviolet-A corneal collagen crosslinking therapy. J Cataract Refract Surg. 2008;34:657–61. doi: 10.1016/j.jcrs.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Ozmen MC, Hondur A, Yilmaz G, Bilgihan K, Hasanreisoglu B. A histological study of rabbit corneas after transepithelial corneal crosslinking using partial epithelial photoablation or ethanol treatment. Int J Ophthalmol. 2014;7:959–63. doi: 10.3980/j.issn.2222-3959.2014.06.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Samaras K, O’Brart DP, Doutch J, Hayes S, Marshall J, Meek KM. Effect of epithelial retention and removal on riboflavin absorption in porcine corneas. J Refract Surg. 2009;25:771–5. doi: 10.3928/1081597X-20090813-03. [DOI] [PubMed] [Google Scholar]
- 44.Rana M, Lau A, Aralikatti A, Shah S. Severe microbial keratitis and associated perforation after corneal crosslinking for keratoconus. Cont Lens Anterior Eye. 2015;38:134–7. doi: 10.1016/j.clae.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 45.Abbouda A, Abicca I, Alio JL. Infectious keratitis following corneal crosslinking: a systematic review of reported cases: management, visual outcome, and treatment proposed. Semin Ophthalmol. 2015;21:1–7. doi: 10.3109/08820538.2014.962176. [DOI] [PubMed] [Google Scholar]
- 46.Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35:1358–62. doi: 10.1016/j.jcrs.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 47.Kymionis GD, Portaliou DM, Pallikaris IG. Additional complications of corneal crosslinking. J Cataract Refract Surg. 2010;36:185. doi: 10.1016/j.jcrs.2009.07.028. author reply 186. [DOI] [PubMed] [Google Scholar]
- 48.Kymionis GD, Portaliou DM, Bouzoukis DI, et al. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg. 2007;33:1982–4. doi: 10.1016/j.jcrs.2007.06.036. [DOI] [PubMed] [Google Scholar]
- 49.Seiler TG, Schmidinger G, Fischinger I, Koller T, Seiler T. Complications of corneal cross-linking. Ophthalmologe. 2013;110:639–44. doi: 10.1007/s00347-012-2682-0. [DOI] [PubMed] [Google Scholar]
- 50.Gokhale NS. Corneal endothelial damage after collagen cross-linking treatment. Cornea. 2011;30:1495–8. doi: 10.1097/ICO.0b013e31820687f7. [DOI] [PubMed] [Google Scholar]
- 51.Sharma A, Nottage JM, Mirchia K, Sharma R, Mohan K, Nirankari VS. Persistent corneal edema after collagen cross-linking for keratoconus. Am J Ophthalmol. 2012;154:922–6. doi: 10.1016/j.ajo.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 52.Bagga B, Pahuja S, Murthy S, Sangwan VS. Endothelial failure after collagen cross-linking with riboflavin and UV-A: case report with literature review. Cornea. 2012;31:1197–200. doi: 10.1097/ICO.0b013e31823cbeb1. [DOI] [PubMed] [Google Scholar]
- 53.Labiris G, Kaloghianni E, Koukoula S, Zissimopoulos A, Kozobolis VP. Corneal melting after collagen cross-linking for keratoconus: a case report. J Med Case Rep. 2011;5:152. doi: 10.1186/1752-1947-5-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rama P, Di Matteo F, Matuska S, Paganoni G, Spinelli A. Acanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens use. J Cataract Refract Surg. 2009;35:788–91. doi: 10.1016/j.jcrs.2008.09.035. [DOI] [PubMed] [Google Scholar]
- 55.Bourne WM, Nelson LR, Hodge DO. Central corneal endothelial cell changes over a ten-year period. Invest Ophthalmol Vis Sci. 1997;38(3):779–82. [PubMed] [Google Scholar]


