Abstract
Introduction
Alpha-1 antitrypsin deficiency (AATD) remains an underdiagnosed condition despite initiatives developed to increase awareness. The objective was to describe the current situation of the diagnosis of AATD in primary care (PC) in Catalonia, Spain.
Methods
We performed a population-based study with data from the Information System for Development in Research in Primary Care, a population database that contains information of 5.8 million inhabitants (80% of the population of Catalonia). We collected the number of alpha-1 antitrypsin (AAT) determinations performed in the PC in two periods (2007–2008 and 2010–2011) and described the characteristics of the individuals tested.
Results
A total of 12,409 AAT determinations were performed (5,559 in 2007–2008 and 6,850 in 2010–2011), with 10.7% of them in children. As a possible indication for AAT determination, 28.9% adults and 29.4% children had a previous diagnosis of a disease related to AATD; transaminase levels were above normal in 17.7% of children and 47.1% of adults. In total, 663 (5.3%) individuals had intermediate AATD (50–100 mg/dL), 24 (0.2%) individuals had a severe deficiency (<50 mg/dL), with a prevalence of 0.19 cases of severe deficiency per 100 determinations. Nine (41%) of the adults with severe deficiency had a previous diagnosis of COPD/emphysema, and four (16.7%) were diagnosed with COPD within 6 months.
Conclusion
The number of AAT determinations in the PC is low in relation to the prevalence of COPD but increased slightly along the study period. The indication to perform the test is not always clear, and patients detected with deficiency are not always referred to a specialist.
Keywords: alpha-1 antitrypsin deficiency, population based, diagnosis, screening, COPD
Introduction
Alpha-1 antitrypsin deficiency (AATD) is a congenital autosomical codominant condition characterized by low plasma levels of alpha-1 antitrypsin (AAT) in the blood and tissues. More than 120 genetic variants of the AAT gene have been identified and classified into three major categories: normal, with genotype M, characterized by AAT within normal ranges; deficient, characterized by reduced but detectable AAT plasma levels with genotypes Z, S, and M-like; and null, currently designated as Q0, with no detectable plasma levels.1 AATD is one of the most common congenital disorders with an estimated prevalence between one in 2,857 and one in 5,097 in USA1 and between one in 2,175 and one in 5,164 in Spain.2 AATD predisposes the development of certain diseases, especially COPD in adults and liver disease, which is more frequent in children. Other less frequent conditions associated with AATD are panniculitis, vasculitis, and fibromyalgia.1
The World Health Organization recommends the testing of all COPD patients,3 and the European Respiratory Society and American Thoracic Society guidelines recommend the testing of all symptomatic adults with persistent airway obstruction, such as COPD, emphysema, and asthma with incompletely reversible airflow obstruction, individuals with unexplained liver disease, and adults with necrotizing panniculitis or multisystemic vasculitis.1 Similarly, the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) recommends that all COPD patients should be tested at least once in their lives.4 Despite these recommendations, AATD is significantly underdiagnosed, and most of the patients are detected long after the onset of pulmonary or liver disease. Another implication of this late diagnosis is the delay in the detection of affected relatives, which hinders the implementation of measures, such as abstaining from tobacco exposure.5,6
Underdiagnosis of AATD is a challenge, particularly, for primary care (PC) physicians who attend most of the COPD patients, and this is usually the first point of contact of patients with health care providers. Computerized databases of medical records are increasingly used in clinical research to enhance the knowledge about the management and progression of this disease based on real-life data.7 Database studies help to understand real clinical practice and to design public health strategies to improve the quality of care. The objective of this study was to describe the patterns of diagnosis of AATD in PC in Catalonia, Spain.
Methods
This was an epidemiological, population-based, observational study aimed to quantify and compare the number of AAT determinations performed in the PC in Catalonia during two 2-year periods (2007–2008 and 2010–2011) and to describe the characteristics of the individuals tested and the management of those with deficient values. Data for this study were obtained from the System for the Development of Research in Primary Care (SIDIAP) database, a computerized database containing anonymized patient records for the 5.8 million people registered in the 279 PC centers of the Catalan Health Institute (>80% of Catalonia’s population). All general practitioners in the Catalan Health Institute use the same specific software called eCAP to record the clinical information of their patients. Health professionals gather this information using codes of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, and structured forms designed for the collection of variables. SIDIAP combines information from the electronic medical records with data from other databases and registers, such as laboratory test results (from the laboratory databases), the pharmacy register, and the National Mortality Register.8,9 For the purpose of the study, we checked the quality of the SIDIAP database. High-quality data were obtained from 2007 onward; however, data from 2012 were not available at the time of the initiation of the study. Therefore, to compare two periods of the same length, we used data from 2007 to 2008 and 2010 to 2011. The study was approved by IDIAP Jordi Gol Ethics Committee (Barcelona, Spain). This was a retrospective study with data from an anonymized database, so it was not necessary to request patient consent.
Population
All the individuals with an AAT determination during the study period were included. Based on the levels obtained in the determination, individuals were classified as follows: no deficiency: AAT >100 mg/dL; intermediate deficiency: AAT between 50 mg/dL and 100 mg/dL; and severe deficiency: AAT <50 mg/dL.10 Since indications for AAT testing differ by age group, we classified individuals younger than 15 years as children and analyzed them separately. Demographic and clinical characteristics were recorded for all the study populations. For individuals with intermediate and severe deficiencies, we collected data on referrals to a specialist, complementary tests (spirometry and computerized tomography scans), pharmacologic treatment, and number of respiratory infections during the 6 months following the determination.
Statistical analysis
A descriptive analysis of each period (2007–2008 and 2010–2011) and of the totality of the sample was performed separately for children and adults. For qualitative variables, absolute frequencies and corresponding percentages were calculated. Quantitative variables following a normal distribution were described by mean and standard deviation, while those not following a normal distribution were described using the median and 25–75 percentiles. Differences between groups were performed using the chi-square test for categorical variables, while continuous variables were tested using the Student’s t-test (or the Mann–Whitney U-test, if the variables were not normally distributed). All tests were two-tailed, and significance was set at 5%. All statistical analyses were performed using a statistical software package (SPSS Version 20.0; IBM Corporation, Armonk, NY, USA).
Results
Frequency of AAT determinations
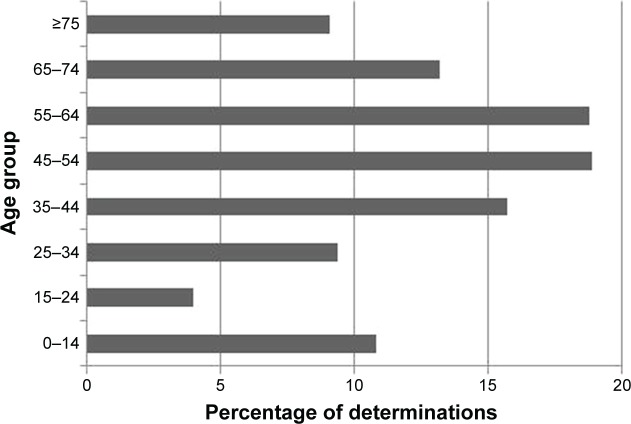
In total, 12,409 determinations of serum AAT were performed during the 4 years of the study, of which 1,335 (10.7%) were children. The number of determinations was higher in the second period (5,559 determinations in 2007–2008 and 6,850 determinations in 2011–2011) due to the low number of individuals tested in 2007. Nonetheless, the rate of individuals tested per year did not increase significantly after 2008 (Table 1). Figure 1 shows the number of determinations performed by age groups.
Table 1.
Number of AAT determinations performed by year
| Period | Children | Adults | Total | n/10,000 inhabitants |
|---|---|---|---|---|
| 2007 | 331 | 1,998 | 2,329 | 4.33 |
| 2008 | 382 | 2,848 | 3,230 | 6.85 |
| 2007–2008 | 713 | 4,846 | 5,559 | |
| 2010 | 325 | 3,351 | 3,676 | 6.77 |
| 2011 | 297 | 3,676 | 3,174 | 5.82 |
| 2010–2011 | 622 | 6,228 | 6,850 |
Abbreviation: AAT, alpha-1 antitrypsin.
Figure 1.
Distribution of percentage of AAT determinations performed by age group.
Abbreviation: AAT, alpha-1 antitrypsin.
Characteristics of the individuals tested
The mean age of the individuals tested was 52.6 (SD 16.3) years in adults and 4.6 (SD 4.1) years in children, with an equal distribution between sexes. Among adults, 37.1% were smokers or former smokers. The most frequent comorbidities in adults were dyslipidemia (27.6%), hypertension (27.4%), diabetes mellitus (11.7%), depression (10.1%), and ischemic heart disease (4%). Up to 41% of children and 18.5% of adults were receiving treatment for a respiratory disease at the time of the determination. The majority of the determinations were performed in urban areas. Demographic characteristics are shown in Tables 2 and 3.
Table 2.
Demographic characteristics and diseases related to AATD of children tested for AAT during the study period
| Variables | Children (n=1,335) |
|---|---|
| Mean age (SD) | 4.61 (4.1) |
| Sex (males) | 769 (57.6) |
| Urban setting | 868 (65) |
| Smokers | 12 (0.9) |
| Former smokers | 2 (0.1) |
| Bronchiectasis | 2 (0.1) |
| Asthma | 298 (22.3) |
| Hepatitis | 7 (0.5) |
| Cirrhosis | 0 |
| Hepatocarcinoma | 0 |
| High transaminase levels | 236 (17.7) |
Note: Data are shown as n (%) unless specified otherwise.
Abbreviations: AAT, alpha-1 antitrypsin; AATD, alpha-1 antitrypsin deficiency.
Table 3.
Comparison of the characteristics of adult patients tested for AAT during the study period according to AAT levels
| Variable | Normal AAT levels (n=10,445) | Intermediate deficiency (n=607) | Severe deficiency (n=22) | Total (n=11,074) |
|---|---|---|---|---|
| Age, mean (SD) | 52.9 (16.3) | 48.0 (14.4)** | 42.5 (15.7)** | 52.6 (16.3) |
| Sex (males) | 5,756 (55.1) | 377 (62.1)** | 14 (63.6) | 6,147 (55.5) |
| Smoker | 2,219 (21.2) | 113 (18.6) | 7 (31.8) | 2,339 (21.1) |
| Former smoker | 1,668 (16) | 101 (16.6) | 3 (13.6) | 1,772 (16) |
| AAT (mg/dL), mean (SD) | 150.9 (34.2) | 87.6 (10.8) | 27.6 (11.6) | 147.2 (36.7) |
| Previous diseases related to AATD | ||||
| COPD | 937 (9) | 34 (5.6)* | 6 (27.3)* | 977 (8.8) |
| Emphysema | 193 (1.8) | 14 (2.3) | 4 (18.2)** | 211 (1.9) |
| Chronic bronchitis | 293 (2.8) | 14 (2.3) | 0 | 307 (2.8) |
| Bronchiectasis | 284 (2.7) | 11 (1.8) | 0 | 295 (2.7) |
| Asthma | 794 (7.6) | 45 (7.4) | 3 (13.6) | 842 (7.6) |
| Hepatitis | 768 (7.4) | 32 (5.3) | 1 (4.5) | 801 (7.2) |
| Cirrhosis | 127 (1.2) | 3 (0.5) | 0 | 130 (1.2) |
| Hepatocarcinoma | 4 (0) | 0 | 0 | 4 (0) |
| High transaminase levels | 5,430 (52) | 313 (51.6) | 8 (36.4) | 5,751 (51.9) |
| Previous respiratory infections | 3,486 (33.8) | 162 (26.6)* | 9 (40.9) | 3,657 (33.02) |
| Previous pneumonia | 136 (1.6) | 5 (0.8) | 1 (4.5) | 142 (1.3) |
| Hypertension | 2,908 (27.8) | 126 (20.8)** | 2 (9.1)* | 3,036 (27.4) |
| Dyslipidemia | 2,901 (27.8) | 158 (26) | 2 (9.1)* | 3,061 (27.6) |
| DM | 1,247 (11.9) | 44 (7.2)** | 1 (4.5) | 1,292 (11.7) |
| Depression | 1,070 (10.2) | 51 (8.4) | 2 (9.1) | 1,123 (10.1) |
| Ischemic heart disease | 428 (4.1) | 13 (2.1)** | 0 | 441 (4) |
Notes:
P<0.05 and
P<0.01 compared to individuals with normal AAT levels. Data are expressed as n (%) unless specified otherwise.
Abbreviations: AAT, alpha-1 antitrypsin; AATD, alpha-1 antitrypsin deficiency; DM, diabetes mellitus.
Indications for AAT determinations, AAT concentrations, and follow-up
As a possible indication for AAT determination, 3,195 (28.9%) adults and 393 (29.4%) children had a previous diagnosis of a disease related to AATD. Up to 17.7% of children and 47.1% of adults had transaminase levels above normal (Tables 2 and 3). Nine percent of children were between the age 0 year and 1 year, suggesting neonatal jaundice as the most likely indication. During the previous year, 31.3% of individuals had had at least one respiratory infection and 1.3% had had pneumonia.
The mean AAT plasma level was 147.2 (36.7) mg/dL in adults and 154.1 (37.2) mg/dL in children. In total, 663 (5.3%) individuals (56 children) had an intermediate AAT deficiency, while 24 (0.2%) individuals (two children) had a severe deficiency, with a prevalence of 0.19 cases of severe deficiency per 100 determinations. Patients with severe deficiency were younger than individuals with normal AAT levels (42.5 years vs 52.9 years, P=0.003) and were more likely to have a previous diagnosis of COPD or emphysema (45.5% vs 10.8%, P<0.05) (Table 3).
During the 6-month follow-up, four of the patients with severe deficiency (18.1%) were newly diagnosed with COPD or emphysema, two (9.1%) following diagnostic spirometry and one (4.2%) after a computerized tomography scan. Only three patients (13.6%) were referred to a pneumologist and another patient was referred to internal medicine (Table 4).
Table 4.
Six-month follow-up of adults tested for AATD according to AAT levels
| Diagnosis after AAT determination | Normal AAT levels (n=10,445) | Intermediate deficiency (n=607) | Severe deficiency (n=22) |
|---|---|---|---|
| COPD | 106 (1) | 5 (0.8) | 2 (9.1)* |
| Emphysema | 36 (0.3) | 1 (0.2) | 2 (9.1)** |
| Chronic bronchitis | 18 (0.2) | 2 (0.3) | 0 |
| Respiratory infections | 3,090 (29.5) | 148 (24.4)** | 10 (45.5)* |
| Pneumonia | 58 (0.6) | 3 (0.5) | 0 |
| Spirometry | 407 (2.9) | 24 (4) | 2 (9.1) |
| Referrals | |||
| Pneumology | 229 (2.2) | 22 (3.6)* | 3 (13.6)* |
| Gastroenterology | 489 (4.7) | 42 (6.9)* | 0 |
| Internal medicine | 73 (0.7) | 2 (0.3) | 1 (4.5) |
Notes:
P<0.05 and
P<0.01 compared to individuals with normal levels of AAT. Data are expressed as n (%).
Abbreviations: AAT, alpha-1 antitrypsin; AATD, alpha-1 antitrypsin deficiency.
Discussion
The results of this study show that the number of AAT determinations performed in the PC in Catalonia, Spain, is low and has not increased after 2008. In addition, in most cases, we could not identify the reason for requesting the test, and after detection of a severe deficiency, some individuals were not tested further or referred to a specialist.
AATD is one of the most common congenital disorders but remains significantly underdiagnosed despite the recommendations of national and international guidelines.1,2 Moreover, there is still a large delay between the onset of symptoms and diagnosis,11 with no significant improvement in this delay during the last decades.12 In Spain, it is estimated that 12,026 patients have a severe deficiency,13 witĥ1,700 of these cases corresponding to Catalonia alone.14 Nonetheless, only 511 cases from all over the country are diagnosed and included in the Spanish registry for AATD.15
Possible explanations for the underdiagnosis of AATD have been addressed in previous studies. Knowledge of AATD is generally poor even for trainees who declared a special interest in respiratory medicine.16 Among nonpulmonologists, awareness of AATD is low in comparison with other respiratory diseases,17 with the consequent low rate of testing for AATD.11,12,18 A survey carried out in Spain and Portugal showed that the main reasons for not testing for AATD are the referral of patients to other specialists for testing or the erroneous perception of the high cost of the test.19
Despite the current recommendations of testing symptomatic adults with persistent airway obstruction and individuals with unexplained liver disease,1,2 the rate of AAT determinations observed in our study along the years varied from 4.33 determinations per 10,000 inhabitants in 2007 to 6.85 determinations per 10,000 inhabitants in 2008, with intermediate values for 2010 and 2011. Data from a recent study performed with data from SIDIAP indicated that a mean of 6,932 new patients were diagnosed with COPD per year between 2007 and 2012, a figure well above the 375 mean number of COPD patients tested yearly for AATD during the 4 years of our study.9 Although underdiagnosis of the deficiency has been reported in many countries, to our knowledge, this low rate of AAT determinations in the general population and in COPD patients has not been previously reported, thereby not allowing comparison of our findings with data from other countries or geographical areas.
Regarding the reasons for requesting AAT determination, we observed that only 13% of the adults tested had COPD, chronic bronchitis, or emphysema and half had high transaminase levels, which could justify the request for AAT determination. These results concur with the observation that >70% of PC physicians in Spain were aware of liver complications of AATD, but very few decided to test all COPD patients.19 Similarly, only 0.5% of children had a codified liver disease at the time of AAT determination, and interestingly, the number of children tested for transaminitis and asthma was similar, although AATD is not a recognized cause of respiratory diseases in childhood.20
In an attempt to improve the rate of diagnosis of AATD in COPD, several screening initiatives or case findings have been developed,21–25 some being carried out in the PC.22,23 In the IDDEA project of case finding of AATD in COPD patients, volunteer PC physicians were provided with filter paper to collect dried blood spots, together with information about AATD and a Web tool. The ratio of recruitment only reached 6.6 patients per participant over the 9-month collection period, being somewhat low considering that the estimated prevalence of COPD in Spain is 10.2% of adults older than 40 years.26 However, among the individuals tested, 4% were carriers of the severe deficient allele Z, and 0.34% were diagnosed with severe homozygous PiZZ deficiency.23 Jain et al24 implemented an electronic alert to encourage guideline-based testing for AATD. This alert was displayed for patients with obstructive spirometry results, and this tool was associated with an increase in the frequency of testing.
Other strategies, such as programs to educate respiratory physicians27 and the combination of an awareness program with the offer of free diagnostic testing,28 resulted in high rates of detection of individuals with severe AATD. Population screening programs in areas of high prevalence or protocols to measure and phenotype AAT in selected patients were found to be effective at detecting AATD patients.29–31
Our study has some limitations. First, the reason to request a complementary test is not recorded in the SIDIAP database, and we cannot be completely certain of the indication leading to the AAT determination. We can only assume the reason based on the codified diagnosis or the results of liver function tests. Second, databases are also subject to possible diagnostic and miscoding biases.32 However, considering that our main objective was to quantify the number of AAT determinations performed, we believe that this possible bias had little impact, if any, on the main objective of the study. On the other hand, the SIDIAP database includes data from >80% of the population of our area, thereby ensuring the representativeness of the results for the whole population of Catalonia.
Conclusion
Our study shows that the rate of testing for AAT in PC is still low, and the reasons for requesting the determination often remain unclear. These results should help to design interventions to increase the awareness and the diagnosis of AAT in selected individuals or populations according to the current guidelines for the diagnosis and management of AATD.
Acknowledgments
This study was funded by unrestricted grants from Grifols, Fundació Catalana de Pneumologia, and the Spanish Society of Pneumology and Thoracic Surgery.
Footnotes
Disclosure
Marc Miravitlles has received speaker fees from Almirall, Boehringer Ingelheim, Pfizer, AstraZeneca, Chiesi, Esteve, GlaxoSmithKline, Menarini, Grifols, Nycomed, and Novartis and consulting fees from Almirall, Boehringer Ingelheim, Pfizer, GlaxoSmithKline, GebroPharma, CSL Behring, MediImmune, Novartis, Grifols, and Nycomed. Carl Llor received a grant from the Fundació Jordi Gol I Gurina for research at the University of Cardiff in 2013. He has also received research grants from the European Commission (Sixth and Seventh Programme Frameworks), the Catalan Society of Family Medicine, and Instituto de Salud Carlos III. Pere Simonet has received speaker fees from Chiesi, Gebro Pharma, Menarini, and TEVA. Miriam Barrecheguren has received speaker fees from Menarini, GlaxoSmithKline, and GebroPharma and consulting fees from Novartis. The other authors report no conflicts of interest in this work.
References
- 1.American Thoracic Society. European Respiratory Society American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2003;168(7):818–900. doi: 10.1164/rccm.168.7.818. [DOI] [PubMed] [Google Scholar]
- 2.Blanco I, de Serres FJ, Fernández-Bustillo E, et al. Estimates of the prevalence of alpha-1-antitrypsin deficiency PI*S and PI*Z alleles and the numbers at risk in Europe countries. Eur Respir J. 2006;27(1):77–84. doi: 10.1183/09031936.06.00062305. [DOI] [PubMed] [Google Scholar]
- 3.Alpha 1-antitrypsin deficiency: memorandum from a WHO meeting. Bull World Health Organ. 1997;75(5):397–415. No authors listed. [PMC free article] [PubMed] [Google Scholar]
- 4.Casas F, Blanco I, Martinez MT, et al. Indications for active case searches and intravenous alpha-1 antitrypsin treatment for patients with alpha-1 antitrypsin deficiency chronic pulmonary obstructive disease: an update. Arch Bronconeumol. 2015;51(4):185–192. doi: 10.1016/j.arbres.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Strange C, Monk R, Schwarz L, Walker D, Kumbhare S, Bieko T. The United States alpha-1 foundation research registry: genesis, impact and future. COPD. 2015;12(Suppl 1):42–45. doi: 10.3109/15412555.2015.1021914. [DOI] [PubMed] [Google Scholar]
- 6.Hogarth K, Rachelefsky G. Screening and familial testing of patients for alpha-1 antitrypsin deficiency. Chest. 2008;133(4):981–988. doi: 10.1378/chest.07-1001. [DOI] [PubMed] [Google Scholar]
- 7.Bellón Saameño JÁ. Large population data bases for primary care research: “we have the advantage”. Aten Primaria. 2010;42(11):549–551. doi: 10.1016/j.aprim.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolíbar B, Avilés F, Morros R, et al. SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. Med Clin (Barc) 2012;138(14):617–621. doi: 10.1016/j.medcli.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Barrecheguren M, Monteagudo M, Ferrer J, et al. Treatment patterns in COPD patients newly diagnosed in primary care. A population-based study. Respir Med. 2016;111:47–53. doi: 10.1016/j.rmed.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Miravitlles M, Herr C, Ferrarotti I, et al. Laboratory testing of individuals with severe AAT deficiency in three European centres. Eur Respir J. 2010;35(5):960–968. doi: 10.1183/09031936.00069709. [DOI] [PubMed] [Google Scholar]
- 11.Kohnlein T, Janciauskiene S, Welte T. Diagnostic delay and clinical modifiers in alpha-1 antitrypsin deficiency. Ther Adv Respir Dis. 2010;4(5):279–287. doi: 10.1177/1753465810376407. [DOI] [PubMed] [Google Scholar]
- 12.Campos M, Wanner A, Zhang G, et al. Trends in the diagnosis of symptomatic patients with alpha1 antitrypsin deficiency. Chest. 2005;128(3):1179–1186. doi: 10.1378/chest.128.3.1179. [DOI] [PubMed] [Google Scholar]
- 13.Vidal R, Blanco I, Casas F, et al. Diagnostic and treatment of alpha one antitrypsin deficiency. Arch Bronconeumol. 2006;42(12):645–659. doi: 10.1016/s1579-2129(07)60007-x. [DOI] [PubMed] [Google Scholar]
- 14.Vidal R, Miravitlles M, Jardi R, et al. Study of the frequency of different alpha-one antitrypsin phenotypes in a population in Barcelona. Med Clin (Barc) 1996;107(6):211–214. [PubMed] [Google Scholar]
- 15.Lara B, Miravitlles M. Spanish registry of patients with alpha-1 antitrypsin deficiency; comparison of the characteristics of PiSZ and PiZZ individuals. COPD. 2015;12(Suppl 1):27–31. doi: 10.3109/15412555.2015.1021912. [DOI] [PubMed] [Google Scholar]
- 16.Taliercio RM, Chatburn RL, Stoller JK. Knowledge of alpha 1 antitrypsin deficiency among internal medicine house officers and respiratory therapists: results of a survey. Respir Care. 2010;55(3):322–327. [PubMed] [Google Scholar]
- 17.Greulich T, Ottaviani S, Bals R, et al. Alpha1 antitrypsin deficiency. Diagnostic testing and disease awareness in Germany and Italy. Respir Med. 2013;107(9):1400–1408. doi: 10.1016/j.rmed.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 18.Stoller JK, Sandhaus RA, Turino G, et al. Delay in diagnosis of alpha 1 antitrypsin deficiency. Chest. 2005;128(4):1989–1994. doi: 10.1378/chest.128.4.1989. [DOI] [PubMed] [Google Scholar]
- 19.Esquinas C, Barrecheguren M, Sucena M, Rodríguez E, Fernandez S, Miravitlles M. Practice and knowledge about diagnosis and treatment of alpha-1 antitrypsin deficiency in Spain and Portugal. BMC Pulm Med. 2016;16:64. [Google Scholar]
- 20.Svegen T, Piitulainen E, Arborelius M. Clinical features and lung function in 18-year-old adolescents with alpha 1-antitrypsin deficiency. Acta Paediatr. 1995;84(7):815–816. doi: 10.1111/j.1651-2227.1995.tb13765.x. [DOI] [PubMed] [Google Scholar]
- 21.Sorroche PB, Fernández-Acquier M, López O, et al. Alpha-1 antitrypsin deficiency in COPD: a cross-sectional study. Arch Bronconeumol. 2015;51(11):539–543. doi: 10.1016/j.arbres.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Wencker M, Marx A, Konietzko N, et al. Screening for alpha-1 Pi deficiency in patients with lung diseases. Eur Respir J. 2002;20(2):319–324. doi: 10.1183/09031936.02.02012001. [DOI] [PubMed] [Google Scholar]
- 23.Molina J, Flor X, García R, Timiraos R, Tirado-Conde G, Miravitlles M. The IDDEA project: a strategy for the detection of alpha-1 antitrypsin deficiency in COPD patients in the primary care setting. Ther Adv Respir Dis. 2011;5(4):237–243. doi: 10.1177/1753465811404919. [DOI] [PubMed] [Google Scholar]
- 24.Jain A, McCarthy K, Xu M, et al. Impact of a clinical decision support system in an electronic health record to enhance detection of alpha 1 antitrypsin deficiency. Chest. 2011;140(1):198–204. doi: 10.1378/chest.10-1658. [DOI] [PubMed] [Google Scholar]
- 25.De la Roza C, Rodríguez-Frías F, Lara B, et al. Results of a case-detection programme for alpha-1-antitrypsin deficiency in COPD patients. Eur Respir J. 2005;26(4):616–622. doi: 10.1183/09031936.05.00007305. [DOI] [PubMed] [Google Scholar]
- 26.Miravitlles M, Soriano JB, García-Río F, et al. Prevalence of COPD in Spain: impact of undiagnosed COPD on quality of life and daily life activities. Thorax. 2009;64(10):863–868. doi: 10.1136/thx.2009.115725. [DOI] [PubMed] [Google Scholar]
- 27.Stoller JK, Strange C, Schwarz L, et al. Detections of alpha 1 antitrypsin deficiency by respiratory therapists: experience with an educational program. Respir Care. 2014;59(5):667–672. doi: 10.4187/respcare.02817. [DOI] [PubMed] [Google Scholar]
- 28.Bals R, Koczulla R, Kotke V, et al. Identification of individuals with alpha-1 antitrypsin deficiency by a targeted screening program. Respir Med. 2007;101(8):1708–1714. doi: 10.1016/j.rmed.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 29.Corda L, Medicina D, La Piana GE, et al. Population genetic screening for alpha one antitrypsin deficiency in a high prevalence area. Respiration. 2011;82(5):418–425. doi: 10.1159/000325067. [DOI] [PubMed] [Google Scholar]
- 30.Corda L, Bertella E, Pini L, et al. Diagnostic flow chart for targeted detection of alpha1- antitrypsin deficiency. Respir Med. 2006;100(3):463–470. doi: 10.1016/j.rmed.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 31.Greulich T, Vogelmeier CF. Alpha-1-antitrypsin deficiency: increasing awareness and improving diagnosis. Ther Adv Respir Dis. 2016;10(1):72–84. doi: 10.1177/1753465815602162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roche N, Reddel H, Martin R, et al. Quality standards for real-world research. Ann Am Thorac Soc. 2014;11(Suppl 2):S99–S104. doi: 10.1513/AnnalsATS.201309-300RM. [DOI] [PubMed] [Google Scholar]