Abstract
Purpose
The transition to motherhood is a time of elevated risk for clinical depression. Dispositional optimism may be protective against depressive symptoms; however the arrival of a newborn presents numerous challenges that may be at odds with initially positive expectations, and which may contribute to depressed mood. We have explored the relative contributions of antenatal and postnatal optimism regarding maternity to depressive symptoms in the postnatal period.
Methods
98 pregnant women underwent clinician interview in the third trimester to record psychiatric history, antenatal depressive symptoms, and administer a novel measure of optimism towards maternity. Measures of depressive symptoms, attitudes to maternity, and mother-to-infant bonding were obtained from 97 study completers at monthly intervals through three months postpartum.
Results
We found a positive effect of antenatal optimism, and a negative effect of postnatal disconfirmation of expectations, on depressive mood postnatally. Postnatal disconfirmation, but not antenatal optimism, was associated with more negative attitudes toward maternity postnatally. Antenatal optimism, but not postnatal disconfirmation, was associated with reduced scores on a mother-to-infant bonding measure. The relationships between antenatal optimism, postnatal disconfirmation of expectations, and postnatal depression held true among primigravidas and multigravidas, as well as among women with prior histories of mood disorders, although antenatal optimism tended to be lower among women with mental health histories.
Conclusions
We conclude that cautious antenatal optimism, rather than immoderate optimism or frank pessimism, is the approach that is most protective against postnatal depressive symptoms, and that this is true irrespective of either mood disorder history or parity. Factors predisposing to negative cognitive assessments and impaired mother-to-infant bonding may be substantially different than those associated with depressive symptoms, a finding that merits further study.
Keywords: Postpartum depression, optimism, maternal attitudes, mother-infant bonding, parenthood
Introduction
Depression manifesting in the postpartum period is common, affecting 8-19% of new mothers (Dietz et al. 2007, Banti et al. 2011, Wisner et al. 2013). Postpartum depression (hereafter PPD) carries the potential for long-term negative outcomes among mothers (Halligan et al. 2007), children (reviewed in Brand and Brennan 2009, Field 2010), the family unit (reviewed in Goodman 2003), and ultimately for society (Paulson et al. 2006, Chronis et al. 2007). Consequently, postnatal major depression is a significant public health concern.
Importantly, PPD is difficult to predict (Austin et al. 2003). It has been estimated that two-thirds of sufferers have no prior history of mood disorder (Banti et al. 2011). Other factors that have positive statistical associations with PPD, including single motherhood, young age, unsupportive partner, and poverty, are too weakly associated to function as effective predictors for the individual clinical case (Austin et al. 2005).
Furthermore, treatment of PPD is complicated by the care needs of the newborn. Optimal treatment for PPD includes frequent visits for monitoring and/or psychotherapy, and it can be difficult or impossible for a new mother to meet these requirements, especially when she is the major or sole provider of care for the newborn, with few options for child care during medical appointments. (See O'Hara and McCabe 2013 for review.)
Thus, PPD is common, entails significant negative effects in the short and long term, is difficult to predict, and is logistically complicated to treat. It would thus be of great benefit to enumerate risk factors that would have clinical utility in the prediction of PPD (Cantwell and Smith 2009). This would set the stage for clinicians to offer both preventive interventions prior to childbirth, and intensive monitoring of women at risk, in order to offer early treatment at the onset of PPD and thus mitigate the length and severity of the depressive episode.
Personality Traits and Postnatal Depression
A diverse body of work has examined the potential of personality factors to contribute to PPD. Personality traits including interpersonal sensitivity (Boyce et al. 1991), neuroticism and introversion (Verkerk et al. 2005), negative cognitive assessment style (Church et al. 2007), and attachment insecurity (Bifulco et al. 2004, Rholes et al. 2011, Monk et al. 2008) have all been implicated. This body of evidence indicates that underlying personality factors do play a role in risk for PPD, although the wide variety of traits examined and diversity of instruments used for assessment makes it difficult to discern the relationships among these traits and their relative contributions to risk for PPD.
Dispositional Optimism and Depressive Diathesis
Dispositional optimism, i.e. the tendency for a positive outlook across many situations, has been associated with protection against depressive symptoms and reduced negative affect in multiple contexts (reviewed and discussed in Taylor & Brown, 1988, 1994, and Scheier and Carver 1993). Prospective analyses have shown that dispositional optimism predicts depressive symptoms both over the short term (Vickers et al. 2000) and over many years of follow-up (Giltay et al. 2006). Twin/adoption analyses have also shown that optimism and pessimism contribute to the prediction of depression and life satisfaction (Plomin et al. 1992). Thus it could be hypothesized that dispositional optimism would also be protective against depression during the common yet major life stressor of new parenthood.
However the literature with respect to dispositional optimism and PPD specifically is scant (reviewed in Evans and Bullock 2012). Three studies have examined dispositional optimism as a predictor of postpartum depressive symptoms: two found a protective effect (Carver and Gaines 1987, n=75; Grote and Bledsoe 2006, n=179) while one found no independent effect (Fontaine and Jones 1997, n=45). All three of these used the Life Orientation Test, a six-item test of general dispositional optimism, rather than a test of optimism in cognitions specifically relating to maternity. A fourth study using a novel measure of optimism in maternity (Churchill and Davis 2010, anonymous Internet n=181 and in-person n=69) found that a realistic orientation conferred greater resilience to postnatal depressive symptoms than either an optimistic or pessimistic approach. All four studies used samples from the general population and did not explore psychiatric history as a variable in any detail.
We wished to investigate whether optimism regarding impending motherhood might be a more specific predictor of postpartum mood than general dispositional optimism, and how this relationship might differ between general and clinical samples.
Expectations and Experience of New Motherhood
A countervailing theory suggests that disconfirmation of initial positive expectations regarding maternity may contribute to depressed mood postpartum (Bouchard 2009). For example, a new mother who harbors unrealistically high expectations for joy and serenity in the postnatal period but is in fact confronted with broken sleep and inconsolable crying may find her risk for PPD increased over that of women whose initial expectations were more moderate. Indeed, it has been found that rigid maternal expectations regarding infant regulation can interact with infant feeding and sleeping problems to enhance the severity of depressive symptoms postpartum (Muscat et al. 2014). Additionally, existing studies focused specifically on the evolution of the marital relationship across the event of childbirth confirm a negative impact of disconfirmed expectations on marital satisfaction (Belsky 1985, Hackel & Ruble 1992).
Two studies have specifically examined the relationship between antenatal optimism and disconfirmed expectations with respect to postnatal depression: one found that disconfirmation of expectations increased depressive symptoms postpartum (Harwood et al. 2007, n=71) while the other found no effect (Muscat et al. 2012, n=35). As no widely accepted, validated scale is available for the measure of optimism with regard to maternity specifically, both used novel measures devised by the authors. Additionally, both studies examined community-based samples with minimal mental health histories. The authors suggested findings in clinical samples might differ.
Given that more positive initial expectations could be expected to increase the likelihood for disconfirmation of these expectations to occur postpartum, we hypothesized that the disparity in the literature could be due to opposing causal chains, whereby baseline optimism is protective against depressive symptomatology postpartum but also increases the risk for disconfirmation of expectations postpartum, which could then increase the severity of depressive symptoms. The relationships between these quantities might also differ based on existing mental health factors. To our knowledge, no study has yet addressed the interacting and potentially opposite effects of dispositional optimism and disconfirmation of expectations on depressive symptomatology in the postpartum period among women with and without mental health histories. This information is relevant to the potential for success of the attempt to identify personality-based predictors of PPD (see Austin and Lumley 2003 for review).
Research Aims and Hypotheses
In the present study, we examined three hypotheses connecting antenatal optimism regarding maternity and the confirmation or disconfirmation of these expectations with depressive symptoms and mother-infant bonding postnatally. We examined a group of women with diverse mental health histories, in order to determine whether previous results in this area could be applicable to clinical samples and how the relationship between antenatal optimism and postnatal depression might differ among women with and without prior histories of mood disorder.
Our first aim was to explore the relationship between antenatal optimism and depressive symptoms, attitudes toward maternity, and mother-to-infant bonding postnatally. We hypothesized that antenatal optimism would be linked to reduced depressive symptoms, more positive attitudes toward maternity, and improved mother-infant bonding in the postnatal period.
Our second aim was to explore the relative contributions of antenatal optimism versus disconfirmation of positive expectations to symptoms of depression, attitudes toward maternity, and mother-to-infant bonding postpartum. We hypothesized that greater antenatal optimism would be associated with a greater degree of disconfirmation of expectations. We further hypothesized that this disconfirmation of positive expectations would independently increase the severity of depressive symptoms and would correlate with more negative attitudes towards maternity and impaired mother-to-infant bonding postpartum, and that this effect would reduce the protective effects of baseline optimism.
Secondary aims of the study included exploration of whether parity and mental health history affect maternal optimism and disconfirmation of expectations.
Methods
The study was approved by the Stanford University Institutional Review Board for Human Subjects Research, and all study participants completed informed consent prior to study participation. Participants consisted of a convenience sample of 98 women recruited sequentially from local obstetric clinics, community postings, and the Stanford Women's Wellness psychiatric clinic, between September 2011 and March 2014. Women with history of mood disorder comprised 30% of the sample, including both women who were and were not in active treatment. Inclusion criteria were age at least 18, uncomplicated singleton pregnancy, and ability to complete the interview and self-report measures in English. Exclusion criteria were active depression at intake, multiple or highly medically complicated pregnancy, and insufficient English to participate. Demographic characteristics of the sample are listed in Table 1.
Table 1.
Characteristics of the study sample.
| Mean, (SD) antenatal MMO (n=98) | Mean, (SD) 3-month MMO (n=97) | |||
|---|---|---|---|---|
| Age | Mean: 32.2 ± 4.9 years | 1.36 (2.71) | 1.33 (2.44) | |
| Marital Status | Unmarried | 7 | 1.57 (1.51) | 0.86 (1.57) |
| Married | 91 | 1.34 (2.79) | 1.37 (2.50) | |
| Parity | Primiparous | 57 | 1.32 (2.87) | 1.30 (2.23) |
| Multiparous | 41 | 1.41 (2.51) | 1.37 (2.74) | |
| Employment | Not employed | 35 | 1.66 (2.01) | 1.51 (2.09) |
| Employed | 63 | 1.19 (3.03) | 1.23 (2.63) | |
| Education | No college degree | 17 | 1.53 (2.00) | 1.29 (2.11) |
| College graduate | 24 | 0.92 (3.33) | 0.67 (2.39) | |
| Graduate schooling | 57 | 1.49 (2.61) | 1.63 (2.53) | |
| History of major mood disorder | No | 68 | 1.68(2.68) | 1.78 (2.28) |
| Yes | 30 | 0.63 (2.67) | 0.33 (2.55) | |
| Postnatal EPDS ≥12 within 2 months of birth | No | 73 | 1.85 (1.26) - | 1.74 (4.24) |
| Yes | 24 | 0.08 (3.11) | 0.08 (2.48) | |
Participants completed an initial interview between 24 and 39 weeks of gestation (mean 32.8 weeks). At one, two, and three months after delivery, participants completed follow-up surveys via the online tool SurveyMonkey. Participants who did not complete surveys received e-mail reminders and, if necessary, telephone prompts. At intake, participants completed an initial interview comprised of the following measures.
Assessment of Psychiatric History
Participants completed a modified screen for psychiatric history. The screen was administered by a trained clinician and was based on the Structured Clinical Interview for DSM Disorders (SCID, First et al. 2012). The screen consisted of ten questions intended to cover a broad base of potential psychiatric issues, including major depression. Participants who replied affirmatively to the depression screening item also completed Part A of the full SCID to clarify their mood disorder histories.
Edinburgh Postnatal Depression scale (EPDS, Cox et al. 1987)
This ten-item measure is a widely used and validated screening tool for ante- and postnatal depression, with good internal consistency (Cronbach alpha reported as 0.87 by Cox et al. 1987).
Center for Epidemiologic Studies Depression scale (CESD, Radloff 1977)
This twenty-item measure of depressive symptoms intended for the general population has been widely used and validated in large samples (Ross and Mirowsky 1983), and has good internal consistency with reported Cronbach alpha of 0.85 (Ross and Mirowsky 1983).
Measure of Maternal Optimism (MMO, Appendix)
This novel ten-item self-report measure explored maternal expectations about a range of experiences related to new motherhood. Cronbach's alpha was 0.77 at the initial administration of the measure, and 0.75 at the 3-month postpartum administration. Concurrent reliability was assessed using the Maternal Attitudes Questionnaire (MAQ, Warner et al. 1997), a measure of cognitive appraisals of maternity, administered at the 1-month postpartum timepoint. Pearson's product-moment correlation was −0.494 (p<0.001).
Follow-up assessments administered at 1, 2, and 3 months postpartum consisted of repeat administrations of the EPDS and MMO, with the addition of the MAQ and the Mother-to-Infant Bonding scale (MIB, Taylor et al. 2005). This eight-item scale is intended to assess the mother's feelings of attachment to her infant. It has an internal reliability of 0.66 and its validity has been established in postpartum samples with respect to other available bonding instruments (Wittkowski et al. 2007).
Other measures administered to this sample for concurrent studies on stress, coping, and personality factors with respect to PPD were not included in this analysis (our unpublished data). Women who scored above 12 on the EPDS were contacted by telephone and offered referral to psychiatric care and to community support resources.
Data Quality
One woman was lost to follow-up and was not included in the present analysis, resulting in a total N of 97. Rate of survey return was 90% overall (including the subject who returned no follow-up surveys). Missing surveys were replaced with data from the same subject from the previous available survey (or, in the case of a missing 1-month survey, from the next available survey). Individual missing items within a measure (<1% of total) were imputed as an average of the remainder of the items in that measure.
Scoring
A single net optimism score for each time point was derived as the sum of the scores for each optimism item, where an ‘optimistic’ response was scored as +1, a ‘flexible’ response was scored as 0, and a ‘pessimistic’ response was scored as −1. Thus optimism scores could potentially range from −10 to +10. The modal optimism score for the antenatal timepoint was +1, with a sample range of −7 to +8. The modal score for the 3-month postnatal timepoint was also +1, also with a sample range of −7 to +8. Postpartum depressive symptoms were determined as a mean of the three EPDS scores obtained over the first three postpartum months. Raw scores for disconfirmation of expectations were obtained by subtracting the antepartum MMO score from the MMO score obtained at the 3-month timepoint. In order to account for variance attributable to the antepartum MMO score itself, standardized residual scores were calculated using a regression analysis in which antenatal MMO scores served as the independent and 3-month MMO scores as the dependent variable. The difference between raw 3-month MMO score and 3-month MMO score predicted by the regression served as the residualized score for disconfirmation of expectations (Cohen & Cohen 1983).
Statistical analysis was carried out using SPSS Statistics version 22 for Windows. Pearson correlations were applied to assess potential relationships among variables of interest. Individual linear regressions were conducted with net antepartum optimism and disconfirmation of expectations as the independent variables and the EPDS, MAQ or MIB averages over the three postpartum time points as the dependent variables (Table 2). Potential confounders were added into the analysis as described in Table 2. T tests and one-way ANOVA were used to explore differences in EPDS, MAQ and MIB outcomes between groups according to parity and mental health history.
Tables 2a, 2b, and 2c.
Multiple regression analyses of depressive symptoms postpartum (2a), attitudes toward maternity (2b), and mother-infant bonding (2c) against optimism at baseline and change in optimism between the baseline and 3-month timepoints. Covariates included in all models but not listed in tables except where noted include age, marital status, parity, planned pregnancy, education, employment, ethnicity, history of mood disorder, quality of partner relationship, and baby fussiness, all nonsignificant contributors except as noted.
| Table 2a. Dependent variable: EPDS mean months 1-3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| N=97 | Model with Demographic Covariates | Model with Demographic Covariates and Baseline Optimism | Model with Demographic Covariates, Baseline Optimism and Change in Optimism | ||||||
| B | SE | Beta | B | SE | Beta | B | SE | Beta | |
| Antenatal EPDS | 0.407 | 0.09 | 0.443*** | 0.363 | 0.098 | 0.395*** | 0.342 | 0.092 | 0.373*** |
| Antenatal MMO | Not significant | −0.335 | 0.161 | −0.193* | |||||
| Residualized Change in MMO | −0.727 | 0.200 | −0.334*** | ||||||
| Adjusted R2 and SE | 0.209, 3.84 | 0.223, 3.80 | 0.323, 3.55 | ||||||
| Table 2b. Dependent variable: MAQ mean months 1-3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| N=97 | Model with Demographic Covariates | Model with Demographic Covariates and Baseline Optimism | Model with Demographic Covariates, Baseline Optimism and Change in Optimism | ||||||
| B | SE | Beta | B | SE | Beta | B | SE | Beta | |
| Antenatal EPDS | 0.177 | 0.067 | 0.282** | 0.156 | 0.070 | 0.249* | 0.139 | 0.063 | 0.221* |
| Hx Mood Disorder | 1.233 | 0.471 | 0.259* | 1.174 | 0.474 | 0.246* | 0.890 | 0.430 | 0.187* |
| Fussy baby | −1.377 | 0.491 | −0.271** | −1.407 | 0.491 | −0.277** | Not significant | ||
| Antenatal MMO | Not significant | Not significant | |||||||
| Residualized Change in MMO | −0.627 | 0.137 | −0.422*** | ||||||
| Adjusted R2 and SE | 0.160, 2.70 | 0.162, 2.70 | 0.325, 2.42 | ||||||
| Table 2c. Dependent Variable: MIB mean months 1-3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model with Demographic Covariates | Model with Demographic Covariates and Baseline Optimism | Model with Demographic Covariates, Baseline Optimism and Change in Optimism | |||||||
| N=97 | B | SE | Beta | B | SE | Beta | B | SE | Beta |
| Antenatal EPDS | 0.211 | 0.065 | 0.360** | 0.174 | 0.067 | 0.296** | 0.167 | 0.066 | 0.285* |
| Antenatal MMO | −0.233 | 0.117 | −0.210* | −0.252 | 0.116 | −0.228* | |||
| Residualized Change in MMO | Not significant | ||||||||
| Adjusted R2 and SE | 0.088, 2.63 | 0.119, 2.58 | 0.136, 2.56 | ||||||
p<0.05
p<0.01
p<0.001.
Results
Summary Statistics for the MMO
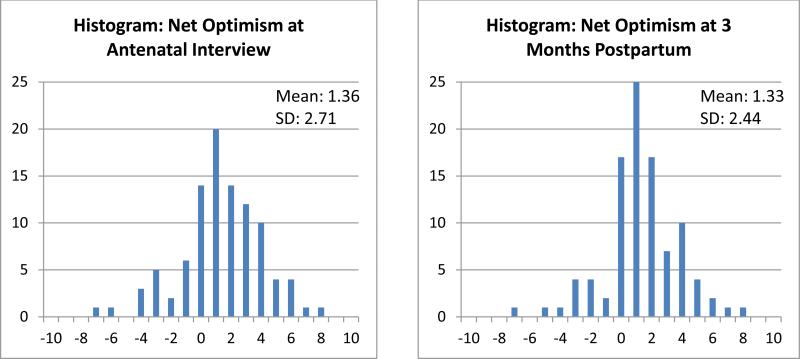
Mean MMO score for the study population was 1.36 (SD 2.71) at the initial administration of the measure, indicating slightly optimistic expectations of motherhood. At the three-month time point, mean MMO score was 1.33 (SD 2.44), not significantly different from the antepartum mean by paired-samples T test. Mean change in optimism as a raw difference between the 3-month and antenatal time points was −0.103 (SD 2.31). Mean residualized change in MMO after correction for the relationship between antenatal optimism and raw change in MMO (slope for this regression was −0.45, indicating that more antenatal optimism is associated with less likelihood of further change in the optimistic direction) was 0.00 (SD 1.98).
Notably, changes in assessments from antepartum to postpartum acted to oppose baseline displacements from the modal (+1) point of our optimism scale (Figure 1). That is, those with initially pessimistic baseline assessments were more likely to move in the optimistic direction postpartum, whereas those with initially optimistic baseline assessments were more likely to move in the pessimistic direction postpartum, creating a net convergence of the sample. Kurtosis of the MMO distribution for the antenatal time point was 0.70, whereas for the 3-month postnatal time point it was 1.41.
Figure 1.
Histograms of MMO scores at antenatal and three-month time points.
Because there is no available validated scale for the assessment of maternal optimism, concurrent reliability was assessed by comparison of the MMO scores from the 1-month postpartum time point to MAQ scores from the same time point. The MMO and MAQ differ on a number of key factors. The MAQ is not formulated to assess optimism; it focuses on the degree to which a woman feels satisfied and engaged versus restricted or coerced in her role as new mother. Thus the items on the MAQ focus on the mother's feelings about her relationship with, and obligations to, her baby and on the effect the baby's arrival has had on her life, whereas the MMO explores optimism with respect to a range of issues including relationship with partner, labor and delivery, changes to the mother's body, etc. Additionally, the MMO is worded generally for use at any time and by people who may or may not be parents, and thus is more suited for longitudinal investigations of changes in optimism across the event of becoming a parent. In contrast, the MAQ is specifically worded for use in mothers of young infants only. For example, while both measures include items examining the mother's feelings about the fulfillment of her infant's needs, the MMO asks, “Choose the answer that most closely describes how you feel: 1) It is a pleasure to care for a baby. 2) Babies have many tiresome needs but also offer much joy. 3) Young babies are a severe drain on the mother's resources.” The MAQ asks, “I think my baby is very demanding. (Strongly agree, agree, disagree, strongly disagree).”
Despite these important differences, Pearson product-moment correlation was 0.494 (p<0.001), indicating a moderately strong correlation.
Study Aim 1: Antenatal Optimism and Postnatal Depressive Symptoms, Attitudes Toward Maternity, and Mother-to-Infant Bonding
The first study aim was to determine whether antenatal optimism was related to depressive symptoms, attitudes toward maternity, and mother-to-infant bonding postnatally. Analysis showed that antenatal optimism regarding maternity was associated with reduced symptoms of depression (EPDS mean over 1-3 months postpartum, Pearson correlation −0.376, p<0.001), with more positive attitudes toward maternity (MAQ mean over 1-3 months postpartum, Pearson correlation −0.290, p<0.01), and with improved self-report of mother-to-infant bonding postpartum (MIB mean over 1-3 months postpartum, Pearson correlation −0.361, p<0.001).
Other characteristics associated with mean postnatal EPDS score included antenatal EPDS (Pearson correlation 0.548, p<0.001) and history of mood disorder (Pearson correlation 0.350, p<0.001). The effects of antenatal EPDS, antenatal optimism, and residualized change in optimism score, but not of history of mood disorder, remained significant after control for the potential covariates of maternal age, marital status, parity, employment, education, ethnicity, and quality of spousal relationship at intake, none of which were significant predictors of postnatal EPDS (regression analysis summarized in Table 2a).
A relative risk for caseness (defined as EPDS at or above 12 in either the first or the second postpartum month) was calculated based on antenatal optimism showed that those with antenatal MMO scores below zero (17 of 97) had a relative risk of EPDS-based caseness of 2.8 compared to those with antenatal MMO scores of zero or greater.
Study Aim 2: Disconfirmation of Expectations and Postnatal Depressive Symptoms, Attitudes Toward Maternity, and Mother-to-Infant Bonding
The second aim of the study was to elucidate any relationship between disconfirmation of antenatal expectations and depressive symptoms, attitudes toward maternity, and mother-to-infant bonding postnatally. Disconfirmation of expectations in the negative direction, indicating less optimism postnatally than antenatally (as measured by MMO residuals), was independently associated with higher postnatal mean EPDS score (Pearson correlation of MMO residuals with postnatal mean EPDS −0.378, p<0.001) and with postnatal mean MAQ score (Pearson correlation −0.491, p<0.001) but not with postnatal mean MIB score. Relative risk for EPDS-based caseness was 1.8 for women with negative MMO residuals (51 of 97) compared to women with MMO residuals of zero or greater.
These patterns held when controlling for other potential demographic and clinical covariates (Table 2). Testing for a moderator effect (Baron and Kenny 1986) did not reveal any moderation of the relationship between disconfirmation of expectations and postnatal mean EPDS by residualized MMO change score.
The major contributor to both postnatal EPDS and postnatal MIB scores was antenatal EPDS. However both baseline optimism and disconfirmation of expectations made improvements in the prediction capacity of the model for postnatal EPDS and MAQ (Tables 2a and 2b), and both baseline optimism and antenatal optimism made improvements in the prediction capacity of the model for postnatal EPDS and MIB (Tables 2a and 2c).
As hypothesized, greater antenatal optimism was associated with more negative shifts in assessment postpartum (as measured by raw MMO change scores; Pearson correlation −0.514, p<0.001), indicating a greater degree of disconfirmation of expectations in the negative direction, i.e. less optimism postnatally than antenatally.
Study Aim 3: Parity and History of Mood Disorder in Relation to Optimism and Disconfirmation of Expectations
The third aim of the study was to examine the effects of parity and history of mood disorder on antenatal optimism, disconfirmation of expectations, and the relationships of these factors to the study outcomes.
Optimism assessments at the antenatal and 3-month postnatal time points, as well as the change in optimism score between the two time points, did not differ significantly by parity for any of the three measures. The majority of the women in the sample were observed to be realistic in their expectations of motherhood. Parity did not affect either optimism regarding maternity or the degree of disconfirmation of expectations, nor did it affect mean postnatal EPDS, MAQ, or MIB. Shifts in assessment across the event of birth were small for the most part, and did not differ based on parity. Mean antenatal optimism score was 1.32 (SD 2.87) for primigravidas (n=57) and 1.41 (SD 2.51) for multigravidas (n=41), and mean optimism score at 3 months was 1.30 (SD 2.33) for primiparas (n=56) and 1.37 (SD 2.74) for multiparas (n=41).
History of major mood disorder, but not minor depression or anxiety, was associated with lower optimism scores at both the antenatal and 3-month time points. For the antenatal time point, mean optimism scores were 1.68 (SD 2.69) for women without history of major mood disorder (n=68), and 0.63 (SD 2.67) for women with history of major mood disorder (n=30), however this difference did not reach statistical significance (p=0.079). Optimism change scores also did not differ significantly between the two groups, yet at 3 months the group with history of mood disorder maintained lower optimism (mood disorder group, mean 0.33, SD 2.55; no mood history group, mean 1.78, SD 2.28; significant with t=2.78, p<0.01) and had recorded higher mean EPDS (mood disorder group, mean 8.94, SD 5.58; no mood history group, mean 6.03, SD 3.77; significant with t=3.02, p<0.01) and MAQ (mood disorder group, mean 5.88, SD 3.99; no mood history group, mean 3.62, SD 2.18; t=−2.91, p<0.01) scores. Mean MIB scores were not significantly different between these groups.
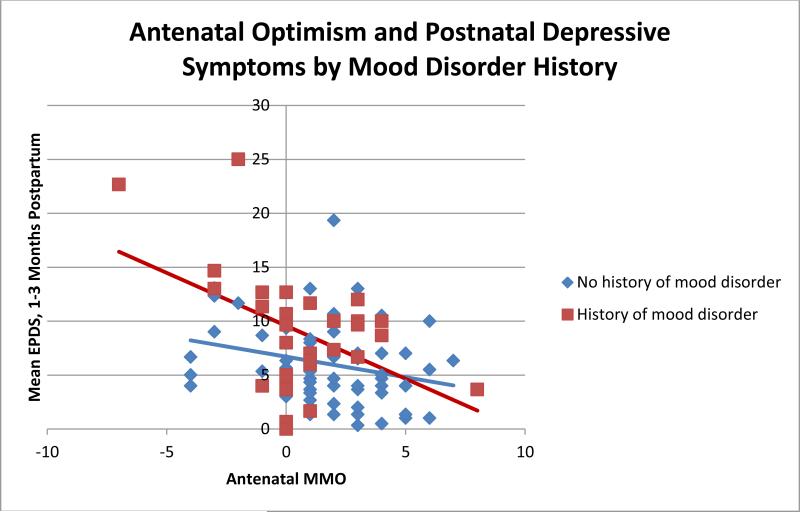
The overall relationship between increased antenatal optimism and decreased postnatal depressive symptoms held true for women with and without history of mood disorder (Figure 2).
Figure 2.
Antenatal optimism predicts reduced postnatal depressive symptoms in women with and without histories of mood disorders.
Women with history of major mood disorder were further broken down into those with history of unipolar depression (n=22) and those with history of bipolar disorder (n=8). One-way ANOVA showed a significant effect of psychiatric diagnosis on postnatal depressive symptoms. Mean postnatal EPDS scores were 5.81 (SD 3.90), 6.86 (SD 5.29), and 12.25 (SD 5.05) for women with no mood disorder history, women with history of unipolar depression, and women with history of bipolar disorder respectively. This finding was statistically significant with F=6.87 and p<0.01.
The relationship of MMO scores with diagnostic history showed a similar trend, with mean antenatal MMO score was 1.68 (SD 2.68) for women with no mood disorder history, 1.00 (SD 2.27) for women with history of unipolar depression, and −0.38 (SD 2.71) for women with history of bipolar disorder, however this difference was not statistically significant (p=0.10). No statistically significant differences among diagnostic groups were found for change in MMO between the antenatal and 3-month time points.
Postnatal MAQ scores were similarly affected by diagnosis, with mean postnatal MAQ scores being 3.62 (SD 2.18), 5.58 (SD 3.58), and 6.71 (SD 3.03) for women with no mood disorder history, women with history of unipolar depression, and women with history of bipolar disorder respectively. This finding was also statistically significant with F=6.93, p<0.01. Postnatal MIB scores did not differ significantly between groups, with the means being 2.18 (SD 1.84) for women with no mood disorder history, 3.68 (SD 4.52) for women with history of unipolar depression, and 3.57 (SD 2.80) for women with history of bipolar disorder.
Discussion
Relative Contributions of Antenatal Optimism and Disconfirmation of Expectations to Depressive Symptoms
We found that greater antenatal optimism was protective against symptoms of depression postpartum in a prospective observational study of 97 mothers, including women both with and without mental health histories. This result is concordant with previous reports on dispositional optimism and depression in the general population (Vickers et al. 2000, Giltay et al. 2006). This effect remained significant in a multiple regression when antenatal depressive symptoms and history of mood disorder were controlled, indicating that antenatal pessimism is not merely a reflection of antenatal depression or of depressive diathesis.
We also demonstrated a correlation between disconfirmation of positive expectations and lower mood and more negative maternal attitudes postpartum, but no relationship with mother-infant bonding. High antenatal optimism was correlated with a greater degree of disconfirmation of expectations in the negative direction postpartum. This implies that greater antenatal optimism is not an unmitigated good, in that excessively high antenatal expectations increase the likelihood of having these expectations fall short of reality. Thus a moderate degree of antenatal optimism, which is not so great as to contrast severely with postnatal experience, appears to be the mindset that is most protective against depressive symptoms postnatally. This is in agreement with the results of Churchill and Davis (2010), who found that a ‘realistic’ orientation was more protective than either optimism or pessimism. These results suggest that prenatal counselors would do best to promote an approach of cautious optimism, rather than either outright pessimism or unrealistically positive expectation.
The finding that antenatal optimism, but not disconfirmation of expectations, contributed to attitude toward maternity postnatally (as self-reported by the MAQ), while disconfirmation of expectations but not antenatal optimism contributed to mother-to-infant bonding (as self-reported by the MIB) is interesting. It suggests that the mother's feelings of being satisfied and engaged versus restricted or coerced in her role as new mother are most strongly related to factors that emerge postnatally. This is supported by the significant effect that maternal report of ‘fussy baby’ had on increased MAQ score. Without an independent rating of the baby's temperament it is impossible to know to what degree this judgement is related to the baby's temperament versus the mother's perception; nonetheless the fact that MAQ score is affected by both postnatal reductions in optimism score and maternal perception of fussy baby suggest that postnatal events are prominent in shaping attitudes toward maternity. Conversely, the mother's feelings of being bonded with her infant are more strongly related to her antenatal optimism, and are not related either to disconfirmation of expectations or to maternal perception of difficult temperament in the infant.
Relationship of Maternal Mental Health History to Optimism and Postnatal Depressive Symptoms
Our findings echo those of previous researchers who found that, contrary to their hypotheses, disappointment was not a common characteristic of the maternal experience, but rather that most women's experiences met or even exceeded their initially optimistic expectations (Harwood et al. 2007, Muscat et al. 2012). The inclusion in our study of women with identified mental health histories suggests that this positive result may apply more broadly across the population, even among women with previous histories of mood disorders.
While women in our study with histories of mood disorders had somewhat less optimistic antepartum assessments of motherhood than women without, they did not experience a greater or lesser degree of disconfirmation of expectations on average.
The contribution of mood disorder history to postnatal depressive symptoms, attitudes toward maternity, and mother-infant bonding was unexpectedly small, given the literature consensus that history of mood disorder increases risk for PPD (O'Hara and Swain 1996). After adjustment for confounders, prior history of any mood disorder did not reach statistical significance as a predictor of postnatal mood or mother-to-infant bonding (Table 2). However, history of bipolar disorder was strongly linked to elevated postnatal EPDS as well as postnatal MAQ scores, a finding that is consonant with an existing body of data that links bipolar disorder to postnatal mood disruptions (Freeman et al. 2002, Sharma et al. 2010).
A partial explanation for the limited correlation between mood disorder history and postnatal depressive symptoms may be that most of the women with mood disorder histories were recruited through a psychiatric clinic, and were thus receiving close monitoring and treatment throughout their pregnancies and postpartum periods. This may have mitigated the relative risk of PPD compared to women who had no mood disorder history and thus were not receiving psychiatric care.
Additionally, it is possible that PPD may represent an entity that is epidemiologically and etiologically distinct from depression manifesting at other points in the life cycle. One early investigation had suggested that recurrence risk for postpartum episodes is more strongly linked to previous postpartum episodes, and recurrence risk for non-postpartum episodes more strongly linked to previous non-postpartum episodes (Cooper and Murray 1995). To our knowledge, no more recent study has attempted to replicate this finding. Our sample contained only three women with histories of prior episodes of PPD, so we were not able to examine whether PPD history specifically could be more strongly related to risk for a second postpartum episode than general history of prior mood episodes. This would be an important point to address in future research.
Relationship of Parity to Antenatal Optimism and Disconfirmation of Expectations
The finding that parity did not affect either antenatal optimism or degree of postnatal disconfirmation of expectations was unexpected and striking. It could be expected that women with previous experience of motherhood would present smaller discrepancies between their antenatal and postnatal assessments than women with no such prior experience. However this prediction was not supported by our data. Nor were multiparas protected against postnatal depressive symptoms relative to primiparas. This finding was in agreement with the results of Muscat et al. (2012).
One possible explanation for this could be that some of the factors which affect a mother's experience of the neonatal period, such as the temperament of the baby and the presence of other children in the home, differ greatly from child to child. Thus the expectations framed by a woman's first experience of motherhood may be no better a guide to her second experience than the general knowledge about new motherhood that is available to primiparas as well.
This finding has implications for prenatal psychological counseling, which is often targeted towards primiparas under the unstated expectation that the transition to new motherhood will be more challenging for them. Our results as well as those of Muscat et al. (2012) suggest that multiparas may also benefit from psychological support as they adjust to the realities of a larger family.
Utility of the MMO as an Assessment Tool for Optimism Regarding Maternity
The MMO requires validation with larger and more heterogeneous study populations. However given its validity in this study as a predictor of postnatal EPDS and its correlation with the established MAQ scale, we regard it as a good basis for the eventual development of a reliable tool to measure optimism in attitudes toward maternity in expectant and new mothers.
The modal score on the MMO at all time points was +1, and the variance of the data decreased between the antenatal and 3-month postnatal time points, indicating a net convergence of the sample toward the +1 point of the scale (Figure 1). Importantly, this suggests that the +1 point of the MMO scale reflects a realistic approach to the experience of new motherhood. The modal score pattern was ‘flexible’ responses on items 1-9 and a ‘positive’ response on item 10. It is possible that a rewriting of the answer choices in item 10 could result in a scale where the modal response is all ‘flexible,’ which would be a more intuitive result. Future studies are needed to implement refinements of the scale and validation of revised versions.
Strengths and Weaknesses of the Current Study
A strength of this study is the inclusion of participants with mental health histories, as previous researchers in this field have suggested that negative findings may relate to the use of study populations who are generally mentally well (Muscat et al. 2012). Our results indicate that women with histories of mental illness, particularly bipolar disorder, tend to have lower levels of antenatal optimism and to be at greater risk for postpartum depressive symptoms, although they do not on average experience a greater or lesser degree of disconfirmation of expectations than do women without mental health histories. Nonetheless the relative contributions of antenatal optimism and disconfirmation of expectations to postnatal depression appear to function largely as they do in nonclinical populations (Figure 2).
Another aspect of this study which may be considered both a strength and a weakness is the homogeneity of the sample. Participants were recruited from university and private clinics servicing a relatively privileged geographical area, and this resulted in a study sample with high educational and socioeconomic attainments. This raises questions about the generalizability of our results to broader community samples. However, the socioeconomic homogeneity of the sample was useful in that it allowed the personality traits under study to become more statistically prominent, and the high socioeconomic attainment of the sample contributed to excellent follow-up rates and a low proportion of missing data. It should be noted that the expected proportion of our study participants (24 women, or 25%) developed depressive symptoms at or above the commonly used EPDS cutoff of 12, which indicates that socioeconomic privilege is not an inoculation against PPD. Future work in this area is needed to validate our novel measure with larger and more heterogeneous sample populations.
Implications for Antenatal Prediction of Postnatal Depression, and Directions for Future Research
Overall our results indicate that antenatal optimism regarding the maternal experience is a protective factor against symptoms of depression postpartum. Disconfirmation of positive expectations, which is more prominent in those with high antenatal optimism, also plays a role in increasing symptoms of depression postpartum. These results suggest that women who find a middle path of cautious optimism are less prone to postnatal depressive symptoms than either those who harbor unrealistically positive expectations or those who are initially pessimistic about motherhood. These findings apply to women with and without histories of mood disorders, and are irrespective of parity.
Effects of disconfirmation of expectations were found on attitudes toward maternity, but not on mother-to-infant bonding; conversely, antenatal optimism was related to mother-to-infant bonding but not to attitudes toward maternity. This is notable because it suggests that the trajectories leading to maternal depressive symptoms versus feelings of dissatisfaction with motherhood, versus the ability to feel warmly towards the infant may be separable, a result that is in agreement with work by other researchers as well (Tharner et al. 2012, O'Higgins et al. 2013). More work in this area is warranted to delineate the factors which predispose to maternal depression versus those that predispose to poor bonding.
The results presented herein support the importance of baseline personality traits as contributors to PPD over and above the risk represented by history of mood disorder, and thus contribute to a growing body of evidence that attributes increases in risk for PPD to premorbid personality factors more broadly (Bifulco et al. 2004, Boyce et al. 2001, Church et al. 2007, Dennis and Boyce 2004, Monk et al. 2008, Verkerk et al. 2005). These findings imply that there may be potential for fruitful research into personality-based antenatal predictors of PPD. Future work in this area should be targeted towards refinement and validation of the MMO and other scales to measure maternal optimism, and towards incorporating these assessments of optimism regarding maternity into the development of more effective tools for antenatal prediction of PPD.
Appendix: Novel Ten-Item Measure of Maternal Optimism (MMO)
For the following ten questions, please choose the answer that most closely describes how you feel. (Scoring: Answers marked ‘O’ are scored +1; answers marked ‘F’ are scored 0; answers marked ‘P’ are scored −1.)
1. Birth plans
O. If one prepares adequately, birth will most likely go as planned.
F. It is important to prepare, but birth is inherently unpredictable.
P. Birth is frightening and dangerous.
2. Baby needs
O. It is a pleasure to care for a baby.
F. Babies have many tiresome needs but also offer much joy.
P. Young babies are a severe drain on the mother's resources.
3. Daily routine
O. The daily tasks of baby care are manageable and mostly pleasant.
F. Baby care can be frustrating but also rewarding.
P. Baby care makes daily life more difficult and unpleasant.
4. Lifestyle
O. The changes a baby brings to the mother's lifestyle are welcome and easy to handle.
F. A baby brings both welcome and unwelcome changes to the mother's lifestyle.
P. A baby puts many unpleasant restrictions on the mother's lifestyle.
5. Parental emotional relationship
O. Having a baby brings the parents closer to each other.
F. Babies have both positive and negative effects on their parents’ relationship.
P. A new baby is a severe test of the parents’ bond with each other.
6. Parental sexual relationship
O. The parents’ sexual relationship is typically not much affected by the arrival of a baby.
F. It is difficult to predict what effect the baby may have on the parents’ sexual life, but a strong relationship will survive any changes.
P. A new baby generally has a bad effect on the parents’ sexual relationship.
7. Expectations of own needs
O. Mothers want to be with their babies all the time.
F. Mothers enjoy caring for their babies but are relieved to have breaks as well.
P. Mothers need frequent breaks in order to cope with the demands of an infant.
8. Expectations of own mood
O. Most mothers experience their babies’ first months as a joyful and rewarding time.
F. It is normal for a mother to have some emotional ups and downs during her baby's first months.
P. Most mothers find their babies’ first months are a stressful and difficult time.
9. Bodily changes after pregnancy and delivery
O. The changes to the mother's body are healthy and constructive.
F. The changes to the mother's body are unfortunate but not overly bothersome.
P. Having a baby is destructive to the mother's body.
10. Being a good parent
O. I am confident in my ability to raise a happy and healthy child.
F. I am somewhat concerned about my ability to raise a happy and healthy child.
P. It is very easy for a mother to make mistakes that will have lifelong negative consequences for the baby.
References
- 1.Affonso DD, Arizmendi TG. Disturbances in post-partum adaptation and depressive symptomatology. Journal of Psychosomatic Obstetrics & Gynecology. 1986;5(1):15–32. [Google Scholar]
- 2.Austin M, Hadzi-Pavlovic D, Saint K, Parker G. Antenatal screening for the prediction of postnatal depression: Validation of a psychosocial pregnancy risk questionnaire. Acta Psychiatrica Scandinavica. 2005;112(4):310–317. doi: 10.1111/j.1600-0447.2005.00594.x. [DOI] [PubMed] [Google Scholar]
- 3.Austin M, Lumley J. Antenatal screening for postnatal depression: A systematic review. Acta Psychiatrica Scandinavica. 2003;107(1):10–17. doi: 10.1034/j.1600-0447.2003.02024.x. [DOI] [PubMed] [Google Scholar]
- 4.Banti S, Mauri M, Oppo A, Borri C, Rambelli C, Ramacciotti D, et al. From the third month of pregnancy to 1 year postpartum. prevalence, incidence, recurrence, and new onset of depression. results from the perinatal Depression–Research & screening unit study. Comprehensive Psychiatry. 2011;52(4):343–351. doi: 10.1016/j.comppsych.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 6.Belsky J. Exploring individual differences in marital change across the transition to parenthood: The role of violated expectations. Journal of Marriage and the Family. 1985:1037–1044. [Google Scholar]
- 7.Bifulco A, Figueiredo B, Guedeney N, Gorman LL, Hayes S, Muzik M, et al. Maternal attachment style and depression associated with childbirth: Preliminary results from a european and US cross-cultural study. The British Journal of Psychiatry.Supplement. 2004;46:s31–7. doi: 10.1192/bjp.184.46.s31. [DOI] [PubMed] [Google Scholar]
- 8.Bouchard G. Parents-to-be with overly optimistic expectations of parenthood: Who are they and what should counsellors do? Canadian Journal of Counselling and Psychotherapy/Revue Canadienne De Counseling Et De Psychothérapie. 2009;43(3) [Google Scholar]
- 9.Boyce P, Hickey A, Gilchrist J, Talley N. The development of a brief personality scale to measure vulnerability to postnatal depression. Archives of Women's Mental Health. 2001;3(4):147–153. [Google Scholar]
- 10.Boyce P, Hickie I, Gordon P. Parents, partners or personality? risk factors for post-natal depression. Journal of Affective Disorders. 1991;21(4):245–255. doi: 10.1016/0165-0327(91)90004-c. [DOI] [PubMed] [Google Scholar]
- 11.Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: How are the children? Clinical Obstetrics and Gynecology. 2009;52(3):441–455. doi: 10.1097/GRF.0b013e3181b52930. [DOI] [PubMed] [Google Scholar]
- 12.Cantwell R, Smith S. Prediction and prevention of perinatal mental illness. Psychiatry. 2009;8(1):21–27. [Google Scholar]
- 13.Carver CS, Gaines JG. Optimism, pessimism, and postpartum depression. Cognitive Therapy and Research. 1987;11(4):449–462. [Google Scholar]
- 14.Chronis AM, Lahey BB, Pelham WE, Jr, Williams SH, Baumann BL, Kipp H, et al. Maternal depression and early positive parenting predict future conduct problems in young children with attention-deficit/hyperactivity disorder. Developmental Psychology. 2007;43(1):70. doi: 10.1037/0012-1649.43.1.70. [DOI] [PubMed] [Google Scholar]
- 15.Church NF, Brechman-Toussaint ML, Hine DW. Do dysfunctional cognitions mediate the relationship between risk factors and postnatal depression symptomatology? Journal of Affective Disorders. 2005;87(1):65–72. doi: 10.1016/j.jad.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 16.Churchill AC, Davis CG. Realistic orientation and the transition to motherhood. Journal of Social and Clinical Psychology. 2010;29(1):39–67. [Google Scholar]
- 17.Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- 18.Cooper PJ, Murray L. Course and recurrence of postnatal depression. evidence for the specificity of the diagnostic concept. The British Journal of Psychiatry. 1995;166(2):191–195. doi: 10.1192/bjp.166.2.191. [DOI] [PubMed] [Google Scholar]
- 19.Dennis C, Boyce P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. Journal of Psychosomatic Obstetrics & Gynecology. 2004;25(3-4):305–311. doi: 10.1080/01674820400017962. [DOI] [PubMed] [Google Scholar]
- 20.Dietz PM, Williams SB, Callaghan WM, Bachman DJ, Whitlock EP, Hornbrook MC. Clinically identified maternal depression before, during, and after pregnancies ending in live births. The American Journal of Psychiatry. 2007;164(10):1515–1520. doi: 10.1176/appi.ajp.2007.06111893. [DOI] [PubMed] [Google Scholar]
- 21.Evans EC, Bullock LF. Optimism and other psychosocial influences on antenatal depression: A systematic review. Nursing & Health Sciences. 2012;14(3):352–361. doi: 10.1111/j.1442-2018.2012.00700.x. [DOI] [PubMed] [Google Scholar]
- 22.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior & Development. 2010;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fontaine KR, Jones LC. Self-esteem, optimism, and postpartum depression. Journal of Clinical Psychology. 1997;53(1):59–63. doi: 10.1002/(sici)1097-4679(199701)53:1<59::aid-jclp8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 24.Freeman MP, Smith KW, Freeman SA, McElroy SL, Kmetz G, Wright R, et al. The impact of reproductive events on the course of bipolar disorder in women. The Journal of Clinical Psychiatry. 2002;63(4):284–287. doi: 10.4088/jcp.v63n0403. [DOI] [PubMed] [Google Scholar]
- 25.Giltay EJ, Zitman FG, Kromhout D. Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: The zutphen elderly study. Journal of Affective Disorders. 2006;91(1):45–52. doi: 10.1016/j.jad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 26.Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. Journal of Advanced Nursing. 2004;45(1):26–35. doi: 10.1046/j.1365-2648.2003.02857.x. [DOI] [PubMed] [Google Scholar]
- 27.Grote NK, Bledsoe SE. Predicting postpartum depressive symptoms in new mothers: The role of optimism and stress frequency during pregnancy. Health & Social Work. 2007;32(2):107–118. doi: 10.1093/hsw/32.2.107. [DOI] [PubMed] [Google Scholar]
- 28.Hackel LS, Ruble DN. Changes in the marital relationship after the first baby is born: Predicting the impact of expectancy disconfirmation. Journal of Personality and Social Psychology. 1992;62(6):944. doi: 10.1037//0022-3514.62.6.944. [DOI] [PubMed] [Google Scholar]
- 29.Halligan SL, Murray L, Martins C, Cooper PJ. Maternal depression and psychiatric outcomes in adolescent offspring: A 13-year longitudinal study. Journal of Affective Disorders. 2007;97(1):145–154. doi: 10.1016/j.jad.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 30.Harwood K, McLean N, Durkin K. First-time mothers' expectations of parenthood: What happens when optimistic expectations are not matched by later experiences? Developmental Psychology. 2007;43(1):1. doi: 10.1037/0012-1649.43.1.1. [DOI] [PubMed] [Google Scholar]
- 31.Monk C, Leight KL, Fang Y. The relationship between women’s attachment style and perinatal mood disturbance: Implications for screening and treatment. Archives of Women's Mental Health. 2008;11(2):117–129. doi: 10.1007/s00737-008-0005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muscat T, Obst P, Cockshaw W, Thorpe K. Beliefs about infant regulation, early infant behaviors and maternal postnatal depressive symptoms. Birth. 2014;41(2):206–213. doi: 10.1111/birt.12107. [DOI] [PubMed] [Google Scholar]
- 33.Muscat T, Thorpe K, Obst P. Disconfirmed expectations of infant behaviours and postnatal depressive symptoms among parents. Journal of Reproductive and Infant Psychology. 2012;30(1):51–61. [Google Scholar]
- 34.O'Higgins M, Roberts ISJ, Glover V, Taylor A. Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Archives of Women's Mental Health. 2013:1–9. doi: 10.1007/s00737-013-0354-y. [DOI] [PubMed] [Google Scholar]
- 35.O'Hara MW, McCabe JE. Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- 36.O'Hara MW, Swain AM. Rates and risk of postpartum depression-a meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- 37.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 38.Plomin R, Scheier MF, Bergeman CS, Pedersen NL, Nesselroade JR, McClearn GE. Optimism, pessimism and mental health: A twin/adoption analysis. Personality and Individual Differences. 1992;13(8):921–930. [Google Scholar]
- 39.Rholes WS, Simpson JA, Kohn JL, Wilson CL, Martin AM, III, Tran S, et al. Attachment orientations and depression: A longitudinal study of new parents. Journal of Personality and Social Psychology. 2011;100(4):567. doi: 10.1037/a0022802. [DOI] [PubMed] [Google Scholar]
- 40.Ross CE, Mirowsky J. Components of depressed mood in married men and women the center for epidemiologic studies'depression scale. American Journal of Epidemiology. 1984;119(6):997–1004. doi: 10.1093/oxfordjournals.aje.a113819. [DOI] [PubMed] [Google Scholar]
- 41.Scheier MF, Carver CS. On the power of positive thinking: The benefits of being optimistic. Current Directions in Psychological Science. 1993:26–30. [Google Scholar]
- 42.Sharma V, Khan M. Identification of bipolar disorder in women with postpartum depression. Bipolar Disorders. 2010;12(3):335–340. doi: 10.1111/j.1399-5618.2010.00809.x. [DOI] [PubMed] [Google Scholar]
- 43.Taylor A, Atkins R, Kumar R, Adams D, Glover V. A new mother-to-infant bonding scale: Links with early maternal mood. Archives of Women's Mental Health. 2005;8(1):45–51. doi: 10.1007/s00737-005-0074-z. [DOI] [PubMed] [Google Scholar]
- 44.Taylor SE, Brown JD. Illusion and well-being: A social psychological perspective on mental health. Psychological Bulletin. 1988;103(2):193. [PubMed] [Google Scholar]
- 45.Taylor SE, Brown JD. Positive illusions and well-being revisited: Separating fact from fiction. 1994 doi: 10.1037/0033-2909.116.1.21. [DOI] [PubMed] [Google Scholar]
- 46.Tharner A, Luijk MP, Van IJzendoorn MH, Bakermans-Kranenburg MJ, Jaddoe VW, Hofman A, et al. Maternal lifetime history of depression and depressive symptoms in the prenatal and early postnatal period do not predict infant–mother attachment quality in a large, population-based dutch cohort study. Attachment & Human Development. 2012;14(1):63–81. doi: 10.1080/14616734.2012.636659. [DOI] [PubMed] [Google Scholar]
- 47.Verkerk GJ, Denollet J, Van Heck GL, Van Son MJ, Pop VJ. Personality factors as determinants of depression in postpartum women: A prospective 1-year follow-up study. Psychosomatic Medicine. 2005;67(4):632–637. doi: 10.1097/01.psy.0000170832.14718.98. [DOI] [PubMed] [Google Scholar]
- 48.Vickers KS, Vogeltanz ND. Dispositional optimism as a predictor of depressive symptoms over time. Personality and Individual Differences. 2000;28(2):259–272. [Google Scholar]
- 49.Warner R, Appleby L, Whitton A, Faragher B. Attitudes toward motherhood in postnatal depression: Development of the maternal attitudes questionnaire. Journal of Psychosomatic Research. 1997;43(4):351–358. doi: 10.1016/s0022-3999(97)00128-1. [DOI] [PubMed] [Google Scholar]
- 50.Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression FindingsDepression screening in postpartum women. JAMA Psychiatry. 2013;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wittkowski A, Wieck A, Mann S. An evaluation of two bonding questionnaires: A comparison of the mother-to-infant bonding scale with the postpartum bonding questionnaire in a sample of primiparous mothers. Archives of Women's Mental Health. 2007;10(4):171–175. doi: 10.1007/s00737-007-0191-y. [DOI] [PubMed] [Google Scholar]