Abstract
Executive dysfunction has been shown to be a promising endophenotype in neurodevelopmental disorders such as autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). This article reviewed 26 studies that examined executive function comparing ASD and/or ADHD children. In light of findings from this review, the ASD + ADHD group appears to share impairment in both flexibility and planning with the ASD group, while it shares the response inhibition deficit with the ADHD group. Conversely, deficit in attention, working memory, preparatory processes, fluency, and concept formation does not appear to be distinctive in discriminating from ASD, ADHD, or ASD + ADHD group. On the basis of neurocognitive endophenotype, the common co-occurrence of executive function deficits seems to reflect an additive comorbidity, rather than a separate condition with distinct impairments.
Keywords: executive function, autism spectrum disorder, attention-deficit/hyperactivity disorder, ASD + ADHD, neurocognitive endophenotype
Introduction
Executive function (EF) comprises a set of cognitive control processes, mainly supported by the prefrontal cortex, which regulates lower level processes (eg, perception, motor responses) and thereby enables self-regulation and self-directed behavior toward a goal, allowing us to break out habits, make decisions and evaluate risks, plan for the future, prioritize and sequence our actions, and cope with novel situations.1 Executive dysfunction has been shown to be a promising endophenotype in neurodevelopmental disorders, such as the autism spectrum disorder (ASD)2–4 and attention-deficit/hyperactivity disorder (ADHD).5–8 Although there are important differences in core symptom definition, the co-occurrence between ASD and ADHD is supported by clinical,9–11 common biological,12–14 and nonbiological risk factors15–17 and neuroimaging studies.18,19
Several authors believe that ASD and ADHD share a common genetic basis. Both family20 and twin studies21 provide support for the hypothesis that ADHD and ASD originate from partly similar familial/genetic factors. Approximately 50%–72% of the contributing genetic factors in both disorders show overlap.22 These shared genetic and neurobiological underpinnings form an explanation why both disorders occur so frequently within the same patient and family. Recent genetic evidences suggest that synaptosomal-associated protein of 25 kDa is involved in ASD and ADHD.23 In line with these observations, studies have reported significant correlations between single nucleotide polymorphisms of synaptosomal-associated protein of 25 kDa and one or more aspects of the EF.24,25 Both ADHD and ASD are childhood-onset neurodevelopmental disorders affecting key frontostriatal and frontoparietal circuits that are important for EF.8 A better understanding of the neurocognitive endophenotype of the co-occurrence of ASD + ADHD is important because it could not only provide clues for enhanced treatment options but could also highlight the existence of a combined phenotype.
EF impairments have been considered as central deficits in ADHD or ASD. It has traditionally been argued that the EF deficits, such as deficit in response inhibition or working memory (WM) and overall weakness in executive control, are related to ADHD symptoms. Pennington and Ozonoff reported minimal evidence of an association between EF and ADHD suggesting that additional research was needed to test whether the relation between ADHD and EF was significant in the general population or was a sampling artifact restricted to clinic-referred samples.26 Barkley proposed the hypothesis that ADHD symptoms may be due to EF deficits. Based on Barkley’s model, ADHD-combined (ADHD-C) subtype is related to deficits in EFs, but there is no EF deficit for ADHD-inattentive (ADHD-I) subtype.5 On the contrary, a review of differences in ADHD subtypes suggests that ADHD-C is more characterized by a lack of inhibitory control, whereas ADHD-I is more characterized by sluggish, disorganized behavior.27 Willcutt et al in a meta-analysis of 83 studies stated that ADHD children/adolescents exhibited significant deficits compared to those without ADHD in neuropsychological measures of EF, such as planning, spatial and verbal WM, response inhibition, and vigilance.8 Gargaro et al described that tasks measuring inhibition are by no means the only method for demonstrating cognitive deficits in children with ADHD.28 Consistent deficits have been reported for a number of other cognitive tasks, such as those measuring sustained attention. Furthermore, individuals with ADHD display longer reaction times and more omission and commission errors than controls. Recently, Ahmadi et al studied the possibility of iconic memory impairment in children with ADHD and found that visual memory is weaker in children with ADHD and they have weaker memory performance than normal children with both visual and auditory symbols at 50 ms and 100 ms presentation durations.29
Over time, researchers have shown an increased interest in executive dysfunction of children with ASD. Among the models that try to identify the primary deficit in ASD, a significant role is played by the assumption that a disturbance at the level of the EFs may be causing many autism symptoms.2–4 Early studies investigated the EF in high-functioning autism, especially in the domain of cognitive flexibility, planning, and WM. In all situations, both in studies with children and adolescents,2,3 people with autism have manifested constant impairments of EFs. Several studies revealed difficulties with planning, and cognitive flexibility was often observed in the form of perseverative errors in this population.30,31 In addition to perseverative errors, children with autism have also shown more deficits in shifting attention,32 sustained or selective attention,33 and response inhibition.34,35 The review by Hill et al on EF in ASD highlights impairments (vs typically developing [TD] controls) on at least two key aspects of EF: planning (eg, anticipatory grasp, Tower of Hanoi/London, detour reaching) and flexibility (eg, Wisconsin Card Sorting Test [WCST], extradimensional shift of the ID/ED task).36 In a recent review of EF in autism, O’Hearn et al37 indicated impairments in tasks requiring response inhibition, WM, planning, and attention, which appear to be present also in adulthood.
While previous studies have documented EF impairments in ADHD and ASD separately, in recent years, a considerable amount of literature has grown up around the EF deficit directly comparing ASD and ADHD. In light of such literature, the aim of this review was to examine the similarities and differences in executive functioning between ASD and ADHD in order to identify neurocognitive endo-phenotypes, which could support the eventual existence of a clinical combined phenotype (ASD + ADHD). Here we review various domains of EF through neurocognitive tasks found in both the pediatric ASD and ADHD literature. To the best of our knowledge, this is the first review on EFs comparing exclusively ASD and ADHD groups. We discuss similarities and differences in ASD and ADHD and their implications for common or differential diagnosis of these two disorders. We also analyze the executive functioning of ASD + ADHD phenotype.
Through this review, we examine different hypotheses:
ASD + ADHD is a distinct phenotype from ASD or ADHD phenotype.
ASD + ADHD phenotype represents the co-occurrence of the two disorders.
ADHD and ASD represent two separate spectrums with some overlapping.
Efforts to define the common or distinct neurocognitive endophenotype of these disorders may help to refine classification systems and enhance the assessment of these complex cases for more specific treatment strategies.
Methods
Search strategy
The literature search was conducted through PubMed, EBSCOhost, Elsevier, Scopus, and Web of Science using a combination of the following free-text terms: “Executive Function”, “autism spectrum disorders”, “autism”, “ASD”, “Attention Deficit Hyperactivity Disorder”, “ADHD”, and “pervasive development disorder”.
Inclusion criteria
The studies included in this review met the following five criteria: 1) compared ASD vs ADHD; 2) assessed EF skills through standardized test; 3) enrolled child and adolescent patients (from 3 years to 18 years of age); 4) were published in English; and 5) were published in peer-reviewed journals. No other restrictions (eg, date of publication) were applied. Review articles and anecdotal clinical reports were excluded.
Data extraction
Studies that met the inclusion criteria were summarized in terms of: 1) participants (sample characteristics and sample size); 2) specific EF; 3) assessment procedure; and 4) results. The first author performed data extraction from the included studies, while an independent rater checked for accuracy. In cases of disagreement on the extracted data, articles were reexamined until consensus (100% agreement) was reached.
Interobserver agreement
A total of 45 articles were identified from the initial search strategies. Each of these 45 articles was then examined, resulting in 26 articles that were retained for screening against the inclusion criteria by two independent reviewers. Agreement as to whether or not the study met the inclusion criteria was 100%.
Results
Table 1 provides a summary of the 26 studies that investigated EF deficits comparing ASD and ADHD. The studies are ordered by date of publication and are categorized by the number of participants, diagnosis-related groups, intelligence quotient (IQ), age range, and EF evaluated.
Table 1.
Features of the 26 studies reviewed
| Study | Number of participants (n) | Diagnosis-related groups | IQ | Age range, years | EF evaluated |
|---|---|---|---|---|---|
| Lawson et al42 | 125 | 70 ASD, 55 ADHD | IQ ≥70 | 6–16 | Response inhibition, flexibility |
| Samyn et al52 | 209 | 31 ASD, 30 ADHD, 148 TD | IQ ≥80 | 10–15 | Response inhibition and attention |
| Matsuura et al43 | 45 | Eleven ASD, 15 ADHD, 19 TD | IQ ≥75 | 8–13 | Attention and WM |
| Sinzig et al58 | 87 | 28 ASD, 30 ADHD, 29 TD | IQ ≥70 | 4–9 | Response inhibition, flexibility, attention |
| Hovik et al39 | 179 | 19 TS, 33 ADHD-C, 43 ADHD-I, 34 ASD, 50 TD | IQ ≥70 | 8–12 | Response inhibition, WM, planning, monitoring |
| Samyn et al62 | 65 | 24 ADHD, 20 ASD, 21 TD | IQ ≥80 | 10–15 | Attention |
| Tye et al60 | 92 | 19 ASD, 18 ADHD, 29 ASD + ADHD, 26 TD | IQ ≥70 | 8–13 | Response inhibition, attention, preparatory processing, monitoring |
| Yasumura et al55 | 36 | Ten ADHD, eleven ASD, 15 TD | IQ ≥80 | 8–13 | Response inhibition |
| Salcedo-Marin et al41 | 103 | 80 ADHD, 23 ASD | IQ ≥70 | 8–17 | Attention, WM, response inhibition, preparatory processing |
| Takeuchi et al56 | 104 | 20 ADHD, 16 ASD + ADHD, eight ASD, 60 TD | IQ ≥80 | 6–15 | Response inhibition, WM |
| Xiao et al50 | 51 | 19 ASD, 16 ADHD, 16 TD | IQ ≥80 | 8–12 | Response inhibition |
| Kado et al57 | 150 | 52 ASD, 46 ADHD, 52 TD | IQ ≥80 | 5–15 | Response inhibition, attention, WM, concept formation |
| Semrud-Clikeman et al40 | 96 | 15 ASD, 21 ADHD-C, 28 ADHD-PI, 32 TD | IQ ≥80 | 9.1–16.5 | Response inhibition, planning, WM, flexibility, monitoring |
| Corbett et al44 | 54 | 18 ASD, 18 ADHD, 18 TD | IQ ≥70 | 7–12 | Response inhibition, WM, flexibility, planning, fluency, attention |
| Gomarus et al59 | 60 | 15 ASD, 15 ADHD, 15 ASD + ADHD, 15 TD | IQ ≥70 | 8–11 | Attention, WM |
| Yang et al54 | 76 | 20 ASD, 26 ADHD, 30 TD | – | 3.7–15.8 | Response inhibition, WM, flexibility |
| Sinzig et al53 | 101 | 30 ADHD, 21 ASD + ADHD, 20 ASD, 30 TD | IQ ≥75 | 6–18 | Response inhibition, attention |
| Sinzig et al45 | 80 | 20 ADHD, 20 ASD, 20 ASD + ADHD, 20 TD | IQ ≥80 | 6–18 | Response inhibition, flexibility, WM, planning |
| Johnson et al61 | 62 | 23 ADHD, 21 ASD, 18 TD | IQ ≥70 | 8–12 | Attention |
| Happé et al46 | 94 | 32 ASD, 30 ADHD, 32 TD | IQ ≥69–70 | 8–16 | Response inhibition, flexibility, planning, WM |
| Goldberg et al47 | 70 | 17 ASD, 21 ADHD, 32 TD | IQ ≥75 | 8–12 | Response inhibition, flexibility, planning, WM |
| Tsuchiya et al49 | 59 | 17 ASD, 22 ADHD, 25 TD | IQ ≥70 | 8–16 | Response inhibition, attention, flexibility |
| Geurts et al48 | 136 | 54 ADHD, 41 ASD, 41 TD | IQ ≥80 | 6–12 | Response inhibition, WM, planning, flexibility, fluency |
| Gioia et al38 | 141 | 27 ADHD-IT, 26 ADHD-CT, 54 ASD, 34 RD, 34 TBI | IQ ≥65 | 8–15 | Response inhibition, WM, flexibility, planning, preparatory processing, monitoring |
| Nyden et al51 | 20 | Ten ASD, ten ADHD, ten TD | – | 8–11 | Response inhibition |
| Ozonoff and Jensen35 | 123 | 40 ASD, 24 ADHD, 30 TS, 29 TD | IQ ≥70 | 10–15 | Planning, flexibility, response inhibition |
Abbreviations: IQ, intelligence quotient; EF, executive function; ASD, autism spectrum disorder; ADHD, attention-deficit/hyperactivity disorder; TD, typically developing; WM, working memory; ADHD-C, ADHD-combined; ADHD-I, ADHD-inattentive; TS, tourette syndrome; ADHD-PI, ADHD-predominately inattentive; ADHD-IT, ADHD-inattentive type; ADHD-CT, ADHD-combined type; RD, reading disorders; TBI, traumatic brain injury.
Characteristics of participants
All studies involved children with ASD and children with ADHD, with a total of 646 and 789, respectively; furthermore, five studies included ASD + ADHD group in which 101 individuals met the diagnostic criteria for both ASD and ADHD. All studies have used previous versions of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, for diagnosis. TD controls were also examined in 23 studies enrolling a total of 723 children with this condition.
The age of the children ranged from 3 years to 18 years. Twenty-three studies included children between 6 years and 18 years of age, while three studies also examined children <6 years of age.
Nine studies included children with IQ scores within the normal range (≥80–85 IQ points), 14 studies also included children with IQ scores within the borderline range (≥70–75 IQ points), and only one study also involved children with IQ scores within the mild disability range (≥60–65 IQ points). Two studies did not report the IQ level.
Specific EF
Twenty-two studies examined response inhibition, fourteen studies examined the WM, thirteen studies examined flexibility, eleven studies examined different domains of attention, nine studies examined planning, four studies examined monitoring, three studies examined preparatory processing, two studies examined fluency, and one study examined concept formation (Table 1).
Procedures to assess EF deficits
Assessment of EFs involves gathering data from several sources and synthesizing the information to look for trends and patterns across time and setting. Apart from formal tests, other measures such as standardized checklists, observations, interviews, and work samples could be used. We found several different kinds of assessment tools to assess EF, which included parent/teacher reports, computerized cognitive tests, and performance-based tests measuring EFs in children with ASD and ADHD. The most common questionnaire developed for parents was the Behavior Rating Inventory of Executive Function, which was used in five studies to assess inhibition, attention, WM, flexibility/shifting, planning, preparatory processing, monitoring, and fluency.38–42 The Cambridge Neuropsychological Test Automated Battery was used in five studies to assess attention, WM, flexibility/shifting, and planning.43–47 The Go/No-Go and the Stroop tests were used in ten and seven studies, respectively, to assess inhibition response. Among the performance-based tests, five studies used the WCST in order to assess inhibition, WM, flexibility/shifting, planning, and concept formation. Table 2 reports the assessment tools used in the studies included in this review.
Table 2.
Assessment tools used in the 26 studies reviewed
| Study | Inhibition | WM | Attention | Flexibility/shifting | Planning | Monitoring | Preparatory processing | Fluency | Concept formation |
|---|---|---|---|---|---|---|---|---|---|
| Lawson et al42 | BRIEF | – | BRIEF | – | – | – | – | – | |
| Samyn et al52 | Go/No-Go task, animal ST | – | Focused and shifting attention task | – | – | – | – | – | – |
| Matsuura et al43 | – | Delayed matching to sample | RVP-CANTAB | – | – | – | – | – | – |
| Sinzig et al58 | Go/No-Go task | – | Sustained attention object | Shifting attentional set visual task | – | – | – | – | – |
| Hovik et al39 | BRIEF | BRIEF | – | – | BRIEF | BRIEF | – | – | – |
| Samyn et al62 | – | – | ACS | – | – | – | – | – | – |
| Tye et al60 | Go/No-Go task | – | Cued-CPT | – | – | Go/No-Go task | CNV | – | – |
| Yasumura et al55 | ST | – | – | – | – | – | – | – | – |
| Salcedo-Marin et al41 | ST | DS and digits forward task | BRIEF | – | – | – | Coding subtest | – | – |
| Takeuchi et al56 | Go/No-Go task, ST | WSCT | – | – | – | – | – | – | – |
| Xiao et al50 | Go/No-Go task, ST | – | – | – | – | – | – | – | – |
| Kado et al57 | WSCT | WSCT | – | WCST | – | – | – | – | WCST |
| Semrud-Clikeman et al40 | BRIEF; Color-Word Interference Test | BRIEF | – | Woodcock–Johnson Cognitive Battery III | Tower test | – | BRIEF | – | – |
| Corbett et al44 | IVA response control quotients and the D-KEFS Color Word Interference Test | CANTAB Spatial Span and Spatial WM subtests | VAQ | CANTAB | CANTAB SOC | – | – | D-KEFS Fluency test | – |
| Gomarus et al59 | – | Visual selective memory search task | Visual selective memory search task | – | – | – | – | – | – |
| Yang et al54 | ST | WCST | – | WCST | – | – | – | – | |
| Sinzig et al53 | Go/No-Go task, TAP | – | TAP | – | – | – | – | – | |
| Sinzig et al45 | Go/No-Go task | CANTAB Spatial Span and Spatial WM subtests | – | CANTAB | CANTAB SOC | – | – | – | – |
| Johnson et al61 | – | – | Sustained attention to response task | – | – | – | – | – | |
| Happé et al46 | Go/No-Go task | CANTAB Spatial Span and Spatial WM subtests | – | CANTAB | CANTAB SOC | – | – | – | – |
| Goldberg et al47 | ST | CANTAB Spatial Span and Spatial WM subtests | – | CANTAB | CANTAB SOC | – | – | – | – |
| Tsuchiya et al49 | WSCT | – | WSCT | WCST | – | – | – | – | – |
| Geurts et al48 | Change task, circle-drawing task, Opposite Worlds of the TEA-Ch | Self-ordered pointing task | – | Change task | Tower of London | – | – | – | – |
| Gioia et al38 | BRIEF | BRIEF | – | – | BRIEF | BRIEF | – | ||
| Nyden et al51 | Go/No-Go task, RIT | – | – | – | – | – | – | – | – |
| Ozonoff and Jensen35 | Go/No-Go task | – | – | WCST | Tower of Hanoi | – | – | – | – |
Abbreviations: WM, working memory; ST, Stroop test; RVP, rapid visual information processing; CANTAB, Cambridge Neuropsychological Test Automated Battery; BRIEF, Behavior Rating Inventory of Executive Function; ACS, Attention Control System; CPT, Continuous Performance Test; CNV, contingent negative variation; DS, digit span; WCST, Wisconsin Card Sorting Test; IVA, integrated visual and auditory; D-KEFS, Delis–Kaplan Executive Function System; VAQ, Visual Attention Quotient; TAP, Test of Attentional Performance; SOC, Stockings of Cambridge; TEA-Ch, Test of Everyday Attention for Children; RIT, response inhibition task.
Similarities and differences in EF
The results of EF pertain to the following domains: inhibition, WM, flexibility, attention, planning, monitoring, preparatory processing, fluency, and concept formation. Table 3 reports the comparison of EF deficits between ASD, ADHD, ASD + ADHD, and TD groups.
Table 3.
Similarities and differences in EF
| Study | EF impairment
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Response inhibition | WM | Attention | Flexibility | Planning | Monitoring | Preparatory processing | Fluency | Concept formation | |
| Lawson et al42 | ADHD > ASD | – | – | ASD > ADHD | – | – | – | – | – |
| Samyn et al52 | ADHD = ASD = TD | – | ADHD = ASD = TD | – | – | – | – | – | – |
| Matsuura et al43 | – | ADHD > TD | ADHD = ASD | – | – | – | – | – | – |
| Sinzig et al58 | ASD > ADHD > TD | – | ADHD > ASD > TD | ADHD > ASD > TD | – | – | – | – | – |
| Hovik et al39 | ADHD-C > ASD; ADHD-I > TD | ADHD = ASD > TD | – | – | ADHD = ASD > TD | ADHD = ASD > TD | – | – | – |
| Samyn et al62 | – | – | ADHD + ODD > ASD, TD | – | – | – | – | – | – |
| Tye et al60 | ADHD/ASD + ADHD > ASD, TD | – | ADHD, ASD + ADHD > ASD | – | – | ASD, ASD + ADHD > ADHD, TD | ASD > ASD + ADHD, ASD, TD | – | – |
| Yasumura et al55 | ADHD > ASD, TD | – | – | – | – | – | – | – | – |
| Salcedo-Marin et al41 | ADHD = ASD | ADHD = ASD | ADHD = ASD | – | – | – | ADHD = ASD | – | – |
| Takeuchi et al56 | ADHD/ASD + ADHD > ASD, TD | ADHD, ASD + ADHD > ASD, TD (verbal); ADHD, ASD > ASD + ADHD (spatial) | – | – | – | – | – | – | – |
| Xiao et al50 | ADHD = ASD > TD | – | – | – | – | – | – | – | – |
| Kado et al57 | ASD > ADHD > TD | ADHD = ASD > TD | – | ASD > ADHD > TD | – | – | – | – | ADHD = ASD > TD |
| Semrud-Clikeman et al40 | ASD, ADHD-C, ADHD-I > TD | ASD, ADHD-C, ADHD-PI > TD | – | ADHD-C, ASD > ADHD-I, TD | ASD, ADHD-C, ADHD-PI > TD | ASD > ADHD-C; ADHD-PI > TD | – | – | – |
| Corbett et al44 | ASD > ADHD > TD | ASD > ADHD > TD | ADHD, ASD > TD | ASD > ADHD; ASD > TD | ADHD = ASD = TD | – | – | ADHD = ASD = TD | – |
| Gomarus et al59 | – | ADHD = ASD > TD | ADHD = ASD > TD | – | – | – | – | – | – |
| Yang et al54 | ADHD = ASD = TD | ADHD = ASD = TD | – | ADHD = ASD = TD | – | – | – | – | – |
| Sinzig et al53 | ADHD + ASD = ADHD = ASD = TD | – | ADHD > ASD + ADHD > ASD, TD | – | – | – | – | – | – |
| Sinzig et al45 | ADHD > ASD + ADHD > ASD, TD | ADHD > TD; ASD > ADHD | – | ADHD + ASD > ASD, TD | ASD > ADHD, TD; ASD + ADHD > TD | – | – | – | – |
| Johnson et al61 | – | – | ADHD > ASD, TD | – | – | – | – | – | – |
| Happé et al46 | ADHD > ASD > TD | ADHD > ASD, TD | – | ADHD = ASD = TD | ADHD = ASD = TD | – | – | – | – |
| Goldberg et al47 | ADHD = ASD = TD | ADHD = ASD > TD | – | ADHD = ASD = TD | ADHD = ASD = TD | – | – | – | – |
| Tsuchiya et al49 | ADHD = ASD > TD | – | ADHD = ASD > TD | ADHD > ASD | – | – | – | – | – |
| Geurts et al48 | ADHD = ASD > TD | ADHD = ASD = TD | – | ASD > ADHD = TD | ASD > ADHD = TD | – | – | ADHD = ASD, TD | – |
| Gioia et al38 | ADHD-C > ADHD-I, ASD, TD | ASD > ADHD = TD | – | ASD > ADHD-C, ADHD-I, TD | ADHD = ASD > TD | ADHD-C, ADHD-I > TD | ADHD-C, ADHD-I > TD | – | – |
| Nyden et al51 | ADHD = ASD > TD | – | – | – | – | – | – | – | – |
| Ozonoff and Jensen35 | ADHD > TD | – | – | ASD > ADHD, TD | ASD > ADHD, TD | – | – | – | – |
Abbreviations: EF, executive function; WM, working memory; ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; TD, typically developing; ADHD-C, ADHD-combined; ADHD-I, ADHD-inattentive; ADHD-PI, ADHD-predominately inattentive; ODD, oppositional defiant disorder.
Inhibition response
Five studies detected statistical significant differences in inhibition response between ASD and ADHD groups compared to the TD group.40,48–51 No significant differences between ASD, ADHD, and TD groups on inhibit performances were found in five studies.41,47,52–54 In three studies, ADHD patients demonstrated more impairment in inhibitory control compared to the ASD patients.35,42,55 Two studies supported that children with ADHD-C tend to have more inhibition problem compared to the ADHD-I and ASD groups.38,39 Two studies reported that on the inhibition task, the ADHD group appeared more impaired than the ASD + ADHD, ASD, and TD groups, whereas the ASD + ADHD group performed worse than the TD and ASD groups.45,56 In three studies, the ASD group appeared more impaired than the ADHD and the TD groups on almost all variables that regarded the inhibition task.44,57,58
Working memory
Four studies detected more WM impairment in ASD and ADHD groups when compared with the TD group.39,40,57,59 No significant differences between the ADHD, ASD, and TD groups in WM were detected in four studies.41,48,50,54 Two studies showed that children with ASD had poor performance relative to the ADHD and TD groups in WM.38,44 The ADHD group showed striking deficits on a spatial WM task compared to ASD and TD groups in one study.46 One study found only differences between ADHD and TD groups.43 Both verbal memory and visuospatial memory were investigated in one study, finding that the ADHD and ASD + ADHD subjects had negative effects on verbal WM, while impairments in visuospatial WM were detected in the ADHD and ASD groups but not in the ASD + ADHD group.56 One study reported more WM impairment in ADHD and ASD + ADHD groups compared with ASD and TD groups.60 One study showed WM impairment in ASD and ADHD groups; however, only the ADHD group reported more deficits compared to the ASD + ADHD group.45
Flexibility
Six studies reported that ASD children have more difficulty with flexibility dimension than those with ADHD.35,38,42,44,48,57 In three studies, no significant differences in flexibility performance were observed among ASD, ADHD, and TD groups.46,47,54 Greater deficiency in flexibility in ADHD children compared to the ASD children was reported in two studies.49,58 In one study, the ASD + ADHD group appeared more impaired than the ASD and TD groups in the flexibility task.45 In one study, ADHD-C and ASD children reported more flexibility impairment compared to ADHD-I and TD children.40
Attention
Three studies reported more impairment in attention skill in ASD and ADHD children compared to the TD children.44,49,59 No significant differences between the ASD and ADHD groups on the scores of sustained and selective attention were detected in two studies.41,43 Two studies showed that ASD + ADHD and ADHD groups tend to have more attention problem compared to the ASD group.53,60 Two studies found that children with ADHD demonstrated clear deficits in sustained attention when compared to ASD and TD children.52,61 Only one study found no difference in attention performance among ASD, ADHD, and TD groups.62 On the contrary, another study showed that the ASD group had a significantly worse performance in sustained attention compared to the ADHD and TD groups.53
Planning
No significant differences on measures of planning across the ASD, ADHD, and TD groups were found in three studies.44,46,47 Three studies detected more deficit in planning skills in ASD and ADHD individuals when compared to TD individuals.38,39,60 In two studies, the ASD group showed more difficulties with cognitive planning compared to children with ADHD and the healthy control group.35,48 One study reported that ASD and ASD + ADHD groups have more planning deficit compared to TD individuals.45
Monitoring
One study found no differences in monitoring between the ASD and ADHD groups; however, both groups showed more deficit compared to the TD individuals.39 One study suggested that impaired conflict monitoring is more conspicuous in ASD and ASD + ADHD individuals than in ADHD and TD individuals.60 One study reported that ASD children have more monitoring deficit compared to ADHD and TD children.40 ADHD-I and ADHD-C children reported more impairment in monitoring than TD children in one study.38
Preparatory processing
One study showed that children with ASD had poorer performance on preparatory processing compared to ASD + ADHD, ADHD, and TD children.60 Another study showed no differences between the ASD and ADHD groups in preparatory processing.41 ADHD-I and ADHD-C children reported more impairment in preparatory processing compared to the TD children in one study.38
Fluency
No significant differences on measures of fluency across the ASD and ADHD groups were found in two studies;44,48 however, one of these48 revealed that ASD and ADHD groups were associated with more EF deficits in verbal fluency than TD counterparts.
Concept formation
Only one study examined the ability of concept formation and found that both ADHD and ASD individuals obtained lower scores using WCST compared to TD individuals, suggesting an inadequate function in these individuals concerning concept formation.57
Discussion
This systematic review identified 26 studies that compared EFs (inhibition, WM, flexibility, attention, planning, monitoring, preparatory processing, fluency, and concept formation) in ASD and ADHD children, and five of these studies also included ASD + ADHD patients. The results of these studies were not unique and often contradictory, probably due to differences in sample characteristics (number of participants, diagnosis-related groups, age, and IQ level) and assessment methodology. Nevertheless, similarities and differences between ASD, ADHD, ASD + ADHD, and TD groups were highlighted by the studies reviewed.
Overall, the similarities between neurocognitive profiles of ASD, ADHD, and ASD + ADHD individuals include several areas of EF such as attention, WM, and fluency. In most of the studies, the dysfunction in attention was frequently observed in all clinical groups (ASD, ADHD, and ASD + ADHD) compared to the TD group. Some studies reported that the severity of the attention dysfunction is greater in the ADHD and ASD + ADHD groups than the ASD and TD groups.53,60 Moreover, investigating various domains of attention, the ADHD children differed from the healthy children especially on the sustained and divided attention tasks, whereas children with ASD + ADHD had difficulties in divided attention and alertness tasks.53 Studies examining WM suggest similar performances in ASD, ADHD, and ASD + ADHD individuals.39,40,57,59 Nevertheless, both ADHD and ASD + ADHD groups needed more time to perform the WM task, while the ASD children made more errors than the healthy children.56 With regard to fluency, studies indicate that there are no significant differences across the ASD and ADHD groups, but both groups gave fewer correct responses than the TD group in this semantic category.44,48
In contrast, EF impairments, such as flexibility, planning, and response inhibition, appear to be distinctive between ASD, ADHD, and ASD + ADHD groups. Children with ASD and ASD + ADHD appear to be characterized by cognitive flexibility and planning deficits. In fact, the majority of the studies included in this review support for more deficit in cognitive flexibility in ASD than in ADHD, reporting for the ASD group a slower mean reaction time and a higher percentage of perseverative responses.42 Additionally, the ASD + ADHD group showed difficulty with test duration of flexibility task compared to the control and the ASD groups.45 With regard to planning, the ASD and ASD + ADHD groups showed more difficulties compared to the ADHD and TD children.45,48 Some authors found differences in the mean subsequent thinking time between ASD children compared to the ADHD and TD children, thus suggesting that planning difficulties, for ASD individuals, might be less a problem of comprehension than of speed (more a problem of speed rather than an issue of comprehension).35,48 Furthermore, the ASD + ADHD group was characterized by an impairment in duration of the planning task, while the ASD group showed a lower performance to initial thinking time and the mean subsequent thinking time. There are evidences showing that response inhibition appears to be more impaired in the ADHD and ASD + ADHD groups than in the ASD and TD groups.50,56,60 The ADHD and ASD + ADHD children make more errors of omission and commission compared to the ASD and healthy control children.45
Finally, there are few studies that have investigated impairment in monitoring, preparatory process, and concept formation. The results in these specific EF domains appear to be too contradictory to identify any similarities or differences between ASD, ADHD, and ASD + ADHD groups. The only common result among these studies is that the clinical groups reported greater impairment in monitoring, preparatory process, and concept formation than the group of healthy children.
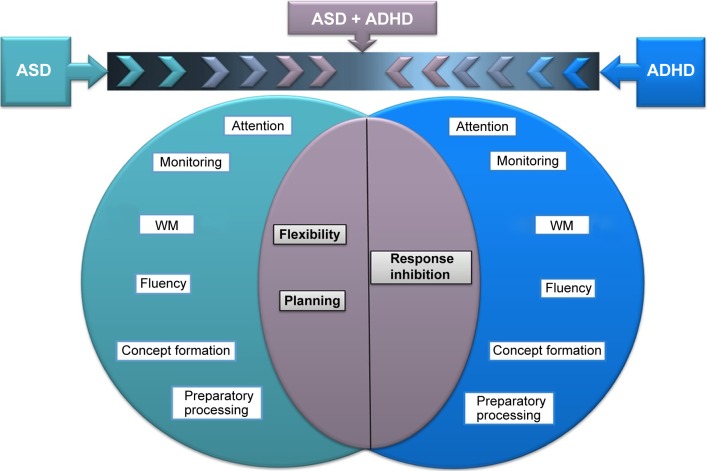
In Figure 1, we represent the similarities and differences in executive functioning between ASD, ADHD, and ASD + ADHD groups.
Figure 1.
Similarities and differences in executive functioning between ASD, ADHD, and ASD + ADHD groups.
Notes: The ASD + ADHD group appeared to share impairment in the flexibility and planning with the ASD group, while it shares the response inhibition deficit with the ADHD group. Conversely, deficit in attention, WM, preparatory processes, fluency, and concept formation does not appear to be distinctive in discriminating from ASD, ADHD, or ASD + ADHD group.
Abbreviations: ASD, autism spectrum disorder; ADHD, attention-deficit/hyperactivity disorder; WM, working memory.
Limitations
This review should be considered in the light of its limitations. The discrepancy in the results in the same EF domain could be mainly attributed to the use of different assessment tools. Many studies of EF currently use traditional neuropsychological EF measures that tap multiple aspects of EF as well as non-EF abilities. Although these tasks may be useful for screening individuals for severe EF deficits, they are too broad to answer fine-grained questions about specific aspects of EF that might be implicated in ASD or ADHD. Although there is no gold standard for the evaluation of EFs,63 the progress of theories and models of EFs, along with the new computerized assessment tests (which focus more on the theoretical account deficits below specific components), could facilitate a more accurate, sensitive, and specific performance evaluation of EF.
Conclusion
This article reviewed 26 studies that examined EF comparing ASD and ADHD children. In light of the findings set out in this review, the ASD + ADHD group appears to share impairments in flexibility and planning with the ASD group, while it shares the response inhibition deficit with the ADHD group (Figure 1). Conversely, deficit in attention, WM, preparatory processes, fluency, and concept formation does not appear to be distinctive in discriminating from ASD, ADHD, or ASD + ADHD group. These findings are in line with the new criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, where the diagnoses of ASD and ADHD are no longer mutually exclusive. In fact, on the basis of neurocognitive endophenotype, the common co-occurrence of EF deficits seems to reflect an additive comorbidity, rather than a separate condition with distinct impairments. The identification of neurocognitive endophenotype in children with ASD, ADHD or ASD + ADHD could play an important role for the treatment implication because EF cognitive training may change the underlying neural mechanisms to improve the real-world function or clinical symptoms. Nonetheless, the definition of the combined phenotype (ASD + ADHD) needs to integrate genetic, neuroimaging, neurocognitive, and clinical evidences.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Miyake A, Friedman NP. The nature and organization of individual differences in executive functions: four general conclusions. Curr Dir Psychol Sci. 2012;21(1):8–14. doi: 10.1177/0963721411429458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ozonoff S. Executive functions in autism. In: Schopler E, Mesibov G, editors. Learning and Cognition in Autism. New York: Plenum Press; 1995. pp. 199–219. [Google Scholar]
- 3.Ozonoff S, Pennington BF, Rogers SJ. Executive function deficits in high-functioning autistic individuals: relationship to theory of mind. J Child Psychol Psychiatry. 1991;32(7):1081–1105. doi: 10.1111/j.1469-7610.1991.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 4.Russell J. Autism as an Executive Disorder. Oxford: Oxford University Press; 1997. How executive disorders can bring about an inadequate “theory of mind”; pp. 256–304. [Google Scholar]
- 5.Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121(1):65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Monuteaux MC, Doyle AE, et al. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. J Consult Clin Psychol. 2004;72(5):757–766. doi: 10.1037/0022-006X.72.5.757. [DOI] [PubMed] [Google Scholar]
- 7.Nigg JT, Blaskey LG, Huang-Pollock CL, Rappley MD. Neuropsychological executive functions and DSM-IV ADHD subtypes. J Am Acad Child Adolesc Psychiatry. 2002;41(1):59–66. doi: 10.1097/00004583-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Craig F, Lamanna AL, Margari F, Matera E, Simone M, Margari L. Overlap between autism spectrum disorders and attention deficit hyperactivity disorder: searching for distinctive/common clinical features. Autism Res. 2015;8(3):328–337. doi: 10.1002/aur.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grzadzinski R, Di Martino A, Brady E, et al. Examining autistic traits in children with ADHD: does the autism spectrum extend to ADHD? J Autism Dev Disord. 2011;41(9):1178–1191. doi: 10.1007/s10803-010-1135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 12.Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK. Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. Eur Child Adolesc Psychiatry. 2010;19(3):281–295. doi: 10.1007/s00787-010-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ronald A, Simonoff E, Kuntsi J, Asherson P, Plomin R. Evidence for overlapping genetic influences on autistic and ADHD behaviours in a community twin sample. J Child Psychol Psychiatry. 2008;49(5):535–542. doi: 10.1111/j.1469-7610.2007.01857.x. [DOI] [PubMed] [Google Scholar]
- 14.Taurines R, Schwenck C, Westerwald E, Sachse M, Siniatchkin M, Freitag C. ADHD and autism: differential diagnosis or overlapping traits? A selective review. Atten Defic Hyperact Disord. 2012;4(3):115–139. doi: 10.1007/s12402-012-0086-2. [DOI] [PubMed] [Google Scholar]
- 15.Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry. 2011;68(11):1104–1112. doi: 10.1001/archgenpsychiatry.2011.73. [DOI] [PubMed] [Google Scholar]
- 16.Kroger A, Hanig S, Seitz C, Palmason H, Meyer J, Freitag CM. Risk factors of autistic symptoms in children with ADHD. Eur Child Adolesc Psychiatry. 2011;20(11–12):561–570. doi: 10.1007/s00787-011-0221-1. [DOI] [PubMed] [Google Scholar]
- 17.Lyall K, Pauls DL, Spiegelman D, Ascherio A, Santangelo SL. Pregnancy complications and obstetric suboptimality in association with autism spectrum disorders in children of the Nurses’ Health Study II. Autism Res. 2012;5(1):21–30. doi: 10.1002/aur.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brieber S, Neufang S, Bruning N, et al. Structural brain abnormalities in adolescents with autism spectrum disorder and patients with attention deficit/hyperactivity disorder. J Child Psychol Psychiatry. 2007;48(12):1251–1258. doi: 10.1111/j.1469-7610.2007.01799.x. [DOI] [PubMed] [Google Scholar]
- 19.Christakou A, Murphy CM, Chantiluke K, et al. Disorder-specific functional abnormalities during sustained attention in youth with Attention Deficit Hyperactivity Disorder (ADHD) and with autism. Mol Psychiatry. 2013;18(2):236–244. doi: 10.1038/mp.2011.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holtmann M, Bolte S, Poustka F. Attention deficit hyperactivity disorder symptoms in pervasive developmental disorders: association with autistic behavior domains and coexisting psychopathology. Psychopathology. 2007;40(3):172–177. doi: 10.1159/000100007. [DOI] [PubMed] [Google Scholar]
- 21.Ronald A, Edelson LR, Asherson P, Saudino KJ. Exploring the relationship between autistic-like traits and ADHD behaviors in early childhood: findings from a community twin study of 2-year-olds. J Abnorm Child Psychol. 2010;38(2):185–196. doi: 10.1007/s10802-009-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children – what do we know? Front Hum Neurosci. 2014;8:268. doi: 10.3389/fnhum.2014.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghezzo A, Guerini FR, Bolognesi E, et al. Neuropsycological gender differences in healthy individuals and in pediatric neurodevelopmental disorders. A role for SNAP-25. Med Hypotheses. 2009;73(6):978–980. doi: 10.1016/j.mehy.2009.05.045. [DOI] [PubMed] [Google Scholar]
- 24.Braida D, Guerini FR, Ponzoni L, et al. Association between SNAP-25 gene polymorphisms and cognition in autism: functional consequences and potential therapeutic strategies. Transl Psychiatry. 2015;5:e500. doi: 10.1038/tp.2014.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guerini FR, Bolognesi E, Chiappedi M, et al. SNAP-25 single nucleotide polymorphisms are associated with hyperactivity in autism spectrum disorders. Pharmacol Res. 2011;64(3):283–288. doi: 10.1016/j.phrs.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 26.Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. J Child Psychol Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- 27.Milich RB, Balentine AC, Lynam DR. ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology: Science and Practice. 2001;8:463–488. [Google Scholar]
- 28.Gargaro BA, Rinehart NJ, Bradshaw JL, Tonge BJ, Sheppard DM. Autism and ADHD: how far have we come in the comorbidity debate? Neurosci Biobehav Rev. 2011;35(5):1081–1088. doi: 10.1016/j.neubiorev.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Ahmadi N, Goodarzi MA, Hadianfard H, et al. Comparing iconic memory in children with and without attention deficit hyperactivity disorder. Iran J Psychiatry. 2013;8(3):131–137. [PMC free article] [PubMed] [Google Scholar]
- 30.Hughes C, Russell J, Robbins TW. Evidence for executive dysfunction in autism. Neuropsychologia. 1994;32(4):477–492. doi: 10.1016/0028-3932(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 31.Pascualvaca DM, Fantie BD, Papageorgiou M, Mirsky AF. Attentional capacities in children with autism: is there a general deficit in shifting focus? J Autism Dev Disord. 1998;28(6):467–478. doi: 10.1023/a:1026091809650. [DOI] [PubMed] [Google Scholar]
- 32.Courchesne E, Townsend J, Akshoomoff NA, et al. Impairment in shifting attention in autistic and cerebellar patients. Behav Neurosci. 1994;108(5):848–865. doi: 10.1037//0735-7044.108.5.848. [DOI] [PubMed] [Google Scholar]
- 33.Noterdaeme M, Mildenberger K, Minow F, Amorosa H. Evaluation of neuromotor deficits in children with autism and children with a specific speech and language disorder. Eur Child Adolesc Psychiatry. 2002;11(5):219–225. doi: 10.1007/s00787-002-0285-z. [DOI] [PubMed] [Google Scholar]
- 34.Brian JA, Tipper SP, Weaver B, Bryson SE. Inhibitory mechanisms in autism spectrum disorders: typical selective inhibition of location versus facilitated perceptual processing. J Child Psychol Psychiatry. 2003;44(4):552–560. doi: 10.1111/1469-7610.00144. [DOI] [PubMed] [Google Scholar]
- 35.Ozonoff S, Jensen J. Brief report: specific executive function profiles in three neurodevelopmental disorders. J Autism Dev Disord. 1999;29(2):171–177. doi: 10.1023/a:1023052913110. [DOI] [PubMed] [Google Scholar]
- 36.Hill E, Berthoz S, Frith U. Brief report: cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. J Autism Dev Disord. 2004;34(2):229–235. doi: 10.1023/b:jadd.0000022613.41399.14. [DOI] [PubMed] [Google Scholar]
- 37.O’Hearn K, Asato M, Ordaz S, Luna B. Neurodevelopment and executive function in autism. Dev Psychopathol. 2008;20(4):1103–1132. doi: 10.1017/S0954579408000527. [DOI] [PubMed] [Google Scholar]
- 38.Gioia GA, Isquith PK, Kenworthy L, Barton RM. Profiles of everyday executive function in acquired and developmental disorders. Child Neuropsychol. 2002;8(2):121–137. doi: 10.1076/chin.8.2.121.8727. [DOI] [PubMed] [Google Scholar]
- 39.Hovik KT, Egeland J, Isquith PK, et al. Distinct patterns of everyday executive function problems distinguish children with Tourette syndrome from children with ADHD or autism spectrum disorders. J Atten Disord. 2014 Sep 24; doi: 10.1177/1087054714550336. Epub. [DOI] [PubMed] [Google Scholar]
- 40.Semrud-Clikeman M, Walkowiak J, Wilkinson A, Butcher B. Executive functioning in children with Asperger syndrome, ADHD-combined type, ADHD-predominately inattentive type, and controls. J Autism Dev Disord. 2010;40(8):1017–1027. doi: 10.1007/s10803-010-0951-9. [DOI] [PubMed] [Google Scholar]
- 41.Salcedo-Marin MD, Moreno-Granados JM, Ruiz-Veguilla M, Ferrin M. Evaluation of planning dysfunction in attention deficit hyperactivity disorder and autistic spectrum disorders using the zoo map task. Child Psychiatry Hum Dev. 2013;44(1):166–185. doi: 10.1007/s10578-012-0317-y. [DOI] [PubMed] [Google Scholar]
- 42.Lawson RA, Papadakis AA, Higginson CI, et al. Everyday executive function impairments predict comorbid psychopathology in autism spectrum and attention deficit hyperactivity disorders. Neuropsychology. 2015;29(3):445–453. doi: 10.1037/neu0000145. [DOI] [PubMed] [Google Scholar]
- 43.Matsuura N, Ishitobi M, Arai S, et al. Distinguishing between autism spectrum disorder and attention deficit hyperactivity disorder by using behavioral checklists, cognitive assessments, and neuropsychological test battery. Asian J Psychiatr. 2014;12:50–57. doi: 10.1016/j.ajp.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 44.Corbett BA, Constantine LJ, Hendren R, Rocke D, Ozonoff S. Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Res. 2009;166(2–3):210–222. doi: 10.1016/j.psychres.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sinzig J, Morsch D, Bruning N, Schmidt MH, Lehmkuhl G. Inhibition, flexibility, working memory and planning in autism spectrum disorders with and without comorbid ADHD-symptoms. Child Adolesc Psychiatry Ment Health. 2008;2(1):4. doi: 10.1186/1753-2000-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Happé F, Booth R, Charlton R, Hughes C. Executive function deficits in autism spectrum disorders and attention-deficit/hyperactivity disorder: examining profiles across domains and ages. Brain Cogn. 2006;61(1):25–39. doi: 10.1016/j.bandc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 47.Goldberg MC, Mostofsky SH, Cutting LE, et al. Subtle executive impairment in children with autism and children with ADHD. J Autism Dev Disord. 2005;35(3):279–293. doi: 10.1007/s10803-005-3291-4. [DOI] [PubMed] [Google Scholar]
- 48.Geurts HM, Verte S, Oosterlaan J, Roeyers H, Sergeant JA. How specific are executive functioning deficits in attention deficit hyperactivity disorder and autism? J Child Psychol Psychiatry. 2004;45(4):836–854. doi: 10.1111/j.1469-7610.2004.00276.x. [DOI] [PubMed] [Google Scholar]
- 49.Tsuchiya E, Oki J, Yahara N, Fujieda K. Computerized version of the Wisconsin card sorting test in children with high-functioning autistic disorder or attention-deficit/hyperactivity disorder. Brain Dev. 2005;27(3):233–236. doi: 10.1016/j.braindev.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 50.Xiao T, Xiao Z, Ke X, et al. Response inhibition impairment in high functioning autism and attention deficit hyperactivity disorder: evidence from near-infrared spectroscopy data. PLoS One. 2012;7(10):e46569. doi: 10.1371/journal.pone.0046569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nyden A, Gillberg C, Hjelmquist E, Heiman M. Executive function/attention deficits in boys with Asperger syndrome, attention disorder and reading/writing disorder. Autism. 1999;3:213–228. [Google Scholar]
- 52.Samyn V, Roeyers H, Bijttebier P, Rosseel Y, Wiersema JR. Assessing effortful control in typical and atypical development: are questionnaires and neuropsychological measures interchangeable? A latent-variable analysis. Res Dev Disabil. 2014;36C:587–599. doi: 10.1016/j.ridd.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 53.Sinzig J, Bruning N, Morsch D, Lehmkuhl G. Attention profiles in autistic children with and without comorbid hyperactivity and attention problems. Acta Neuropsychiatr. 2008;20(4):207–215. doi: 10.1111/j.1601-5215.2008.00292.x. [DOI] [PubMed] [Google Scholar]
- 54.Yang J, Zhou S, Yao S, Su L, McWhinnie C. The relationship between theory of mind and executive function in a sample of children from mainland China. Child Psychiatry Hum Dev. 2009;40(2):169–182. doi: 10.1007/s10578-008-0119-4. [DOI] [PubMed] [Google Scholar]
- 55.Yasumura A, Kokubo N, Yamamoto H, et al. Neurobehavioral and hemodynamic evaluation of Stroop and reverse Stroop interference in children with attention-deficit/hyperactivity disorder. Brain Dev. 2014;36(2):97–106. doi: 10.1016/j.braindev.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 56.Takeuchi A, Ogino T, Hanafusa K, et al. Inhibitory function and working memory in attention deficit/hyperactivity disorder and pervasive developmental disorders: does a continuous cognitive gradient explain ADHD and PDD traits? Acta Med Okayama. 2013;67(5):293–303. doi: 10.18926/AMO/51865. [DOI] [PubMed] [Google Scholar]
- 57.Kado Y, Sanada S, Yanagihara M, et al. Executive function in children with pervasive developmental disorder and attention-deficit/hyperactivity disorder assessed by the Keio version of the Wisconsin card sorting test. Brain Dev. 2012;34(5):354–359. doi: 10.1016/j.braindev.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 58.Sinzig J, Vinzelberg I, Evers D, Lehmkuhl G. Executive function and attention profiles in preschool and elementary school children with autism spectrum disorders or ADHD. Int J Dev Disabil. 2014;60(3):144–154. [Google Scholar]
- 59.Gomarus HK, Wijers AA, Minderaa RB, Althaus M. ERP correlates of selective attention and working memory capacities in children with ADHD and/or PDD-NOS. Clin Neurophysiol. 2009;120(1):60–72. doi: 10.1016/j.clinph.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 60.Tye C, Asherson P, Ashwood KL, Azadi B, Bolton P, McLoughlin G. Attention and inhibition in children with ASD, ADHD and co-morbid ASD + ADHD: an event-related potential study. Psychol Med. 2014;44(5):1101–1116. doi: 10.1017/S0033291713001049. [DOI] [PubMed] [Google Scholar]
- 61.Johnson KA, Robertson IH, Kelly SP, et al. Dissociation in performance of children with ADHD and high-functioning autism on a task of sustained attention. Neuropsychologia. 2007;45(10):2234–2245. doi: 10.1016/j.neuropsychologia.2007.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Samyn V, Wiersema JR, Bijttebier P, Roeyers H. Effortful control and executive attention in typical and atypical development: an event-related potential study. Biol Psychol. 2014;99:160–171. doi: 10.1016/j.biopsycho.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 63.Chan RC, Shum D, Toulopoulou T, Chen EY. Assessment of executive functions: review of instruments and identification of critical issues. Arch Clin Neuropsychol. 2008;23(2):201–216. doi: 10.1016/j.acn.2007.08.010. [DOI] [PubMed] [Google Scholar]