Abstract
Purpose
To compare the visual acuity (VA) and quality of vision between bilateral implantation of a trifocal intraocular lens (IOL) and blended bifocal IOLs with an intermediate add in the dominant eye and a near add in the nondominant eye.
Patients and methods
Patients with either trifocal or blended bifocal IOLs implanted were recruited after surgery. Subjects returned for a single diagnostic visit between 3 and 24 months after surgery. VA was tested at various distances, including low-contrast acuity and acuity at their preferred reading distance. A binocular defocus curve was obtained, and subjective visual function and quality of vision were evaluated.
Results
Twenty-five trifocal subjects and 30 blended bifocal subjects were enrolled. There were no significant differences in low-contrast acuity, preferred reading distance, or acuity at that reading distance. Binocular vision at 4 m, 60 cm, and 40 cm was not statistically significantly different. The trifocal provided statistically significantly better visual acuity (P<0.05) at vergences from −0.5 to −1.5 D (from 2 m to 67 cm viewing distance, P<0.05). There was no statistically significant difference in the near vision subscale scores of the 39-question National Eye Institute Visual Function Questionnaire or the overall scores of the Quality of Vision questionnaire, though significantly more trifocal subjects reported that the observed visual disturbances were “bothersome” (P<0.05).
Conclusion
Both lens modalities provided subjects with excellent binocular near and distance vision, with similar low rates of visual disturbances and good reported functional vision. The trifocal IOL provided significantly better intermediate VA in the viewing distance range of 2 m to 67 cm, corresponding to viewing things such as a car dashboard or grocery shelf. VA was similar between groups at viewing distances from 60 to 40 cm, corresponding to computer or reading distance.
Keywords: ReSTOR, At LISA tri, multifocal IOL, cataract, presbyopia
Video abstract
Introduction
Many patients presenting for cataract surgery are interested in achieving good-quality vision at distance, intermediate, and near without the use of spectacles or contact lenses. Multifocal intraocular lenses (IOLs) that can provide a wide range of clear and comfortable vision attempt to meet the objective of these patients.
Arguably, the most successful multifocal IOL design at present is a diffractive design, using a combination of refractive and diffractive technology to distribute incoming light into two (bifocal) or three (trifocal) foci. This splitting of light that occurs with all diffractive IOLs has been shown to have the potential to decrease contrast sensitivity and increase visual disturbances in some patients.1 Some surgeons are concerned that this may be worse when using trifocal IOLs, since more light is being diffracted when compared to bifocal IOLs. A bench study found that a trifocal IOL had improved intermediate visual quality at the expense of distance and near.2 Another study demonstrated increased halos with trifocal IOLs when compared to bifocal IOLs.3 The challenge in multifocal IOL design is to provide functional vision at distance, intermediate, and near, while minimizing the potential for visual disturbances.
A commonly used bifocal IOL is the AcrySof® IQ ReSTOR® lens (Alcon Laboratories, Inc., Fort Worth, TX, USA), a hydrophobic acrylic lens with central apodized diffractive surface to provide near vision and an outer refractive area for distance vision; the design premise is that low illumination with an increased pupil size will improve distance vision and reduce the potential for visual disturbances, while high illumination with a smaller pupil size will improve near vision.2 The two most commonly used ReSTOR lenses are the ReSTOR +3.0 D lens (SN6AD1) and the ReSTOR +2.5 D lens (SV25T0). The ReSTOR +2.5 D lens allows more light to distance viewing and has a lower add power than the +3.0 D lens.4 The ReSTOR +3.0 D lens has been demonstrated to provide good distance vision and good near vision at approximately 40 cm or 16 inches.5 While intermediate vision at 67 cm (−1.5 D) with this lens can be acceptable (near 20/30, or 0.2 logMAR), the +2.5 D lens has been shown to improve visual acuity (VA) at this distance.5,6 The latter lens provides good distance vision and intermediate vision at approximately 50 cm.3,4 When compared to monofocal IOLs, the ReSTOR +2.5 D lens provides better vision at 30 and 50 cm, similar vision at 70 and 100 cm, and comparable contrast acuity with and without glare.7 It has also been reported to have slightly lower higher-order aberrations and less glare symptoms when compared to the +3.0 D lens.6,8 Some surgeons attempt to take advantage of the strengths of both lenses by using a blended implantation strategy, combining a ReSTOR +2.5 D lens in the dominant eye with a ReSTOR +3.0 D lens in the nondominant eye. This strategy has been demonstrated to increase the functional range of vision for patients relative to bilateral implantation of either the +2.5 or +3.0 D lens.8
Another option for providing a greater range of vision is by implanting a trifocal IOL in both eyes. A commonly used trifocal IOL is the Carl Zeiss Meditec (CZM) AT LISA tri 839MP IOL (Carl Zeiss Meditec AG, Jena, Germany), a hydrophilic acrylate diffractive IOL with a hydrophobic surface.9,10 The AT LISA tri lens has a near power of +3.33 D and an intermediate power of +1.66 D at the IOL plane in its inner 4.34 mm trifocal area and a +3.75 D add in its outer bifocal area; this is believed to make it largely pupil independent.2,9,10 It is also believed that visual disturbances with this trifocal lens are minimized due to its smooth surface.11 The two most common visual disturbances with this trifocal IOL were halos and glare noted in 60% (15/25) and 28% (7/25) of patients, respectively.12 One study demonstrated that this trifocal lens allowed nearly 80% of patients to achieve 20/20 binocular VA at distance, intermediate, and near and 100% of patients to achieve 20/40 binocular VA at all distances.9 The defocus curve in one study demonstrated a continuum of functional vision of at least 20/32 (0.2 logMAR) from distance (0.0 D vergence) to 33 cm (3.0 D vergence).10,11
The objective of the study was to compare the postoperative near, intermediate, and distance VA, and the level of visual disturbances, provided by a ReSTOR +2.5/+3.0 “blended bifocal” modality to results obtained with bilateral implantation of the CZM AT LISA tri 839MP IOL.
Patients and methods
This noninterventional two-arm diagnostic study was designed to evaluate visual function after bilateral implantation of two different multifocal IOL modalities. The first group (blended bifocal) included subjects implanted with a ReSTOR +2.5 D IOL in the dominant eye and a ReSTOR +3.0 D IOL in the nondominant eye. The second group (trifocal) included subjects implanted with the AT LISA tri IOL in both eyes. Implanted lenses could be toric or nontoric. Regional ethics committee approval was applied for and obtained from the Regional Committees for Medical and Health Research Ethics (REK), Norway before patients were enrolled. A statistical power analysis related to the ability to detect a half-line difference in intermediate acuity indicated that 24 subjects in each group would be sufficient; the target enrollment was 30 patients in each group. Patients who had uncomplicated bilateral cataract surgery between 3 months and 2 years before their examination visit were eligible for inclusion. All patients were recruited from the files of a single surgeon (KGG) at a single site; the surgeon’s standard operating procedure was used for all patients.
The study was conducted as a postintervention diagnostic evaluation. A list of patients meeting the IOL implantation criteria above, without reported surgical complications, who were between 3 and 24 months postsurgery was prepared. Patients were called and asked to return for one diagnostic test visit. The recruiting list was updated over time, and patients were randomly called until 30 subjects in each group were scheduled. Some patients presenting for a routine postoperative follow-up visit in the appropriate time window were invited to participate immediately following their routine visit. Patients signed an informed consent form outlining the nature of the study, acknowledging their agreement to participate, and permitting use of their de-identified data for analysis. Conduct of the study was in accordance with the principles of the Declaration of Helsinki.
The single study visit involved the subjective evaluation of VA and quality of vision. Basic demographic data were collected and enrollment qualification was confirmed as described in the protocol; subjects must have had uncomplicated bilateral surgery with one of the modalities above, with no ocular or systemic pathology that might have affected their best-corrected postoperative VA. Presenting binocular uncorrected acuity had to be 0.3 logMAR (20/40) or better, to ensure that the subjective quality of vision was not unduly affected by excessive residual refractive error. A manifest refraction was performed and VA was measured using high-contrast logMAR ETDRS charts at 4 m, 60 cm, and 40 cm under photopic conditions. VA was tested both monocularly and binocularly, uncorrected and with the best distance correction in place. A binocular defocus curve was obtained by correcting the subject for distance viewing, then introducing defocus of +1.0 D and recording the VA. The defocus was then reduced in 0.5 D increments until 0.0 D was reached, recording VA at each step. The process was repeated in the minus direction starting at −4.0 D and decreasing the defocus in 0.5 D steps until 0.0 D was reached. The preferred distance for near work and the associated logMAR VA were also measured; the patients placed the 60 cm logMAR chart at their preferred reading distance and their unadjusted logMAR VA was recorded. This was then corrected to provide the logMAR VA at the preferred reading distance. Distance low-contrast (13%) VA was also tested, both uncorrected and with the subject’s best distance correction in place. Subjective patient outcomes were characterized in two ways. The first involved having subjects complete the near vision subscale of the 39-question National Eye Institute Visual Function Questionnaire (NEI VFQ-39), a test originally developed at the RAND corporation under the sponsorship of the NEI; it provides a self-reported measure of visual function.13 The second involved measuring visual quality using the Quality of Vision questionnaire. This questionnaire asks subjects about the frequency, severity, and the degree to which visual disturbances such as glare, haloes, or starbursts are bothersome.14 Both of these subjective instruments have been validated and are scored using Rasch analysis.
This study is the first reported comparison between a blended bifocal modality and bilateral trifocal implantation. The primary measure of interest was the difference in binocular best-corrected VA at 60 cm. Other measures of interest were the differences in VA at distance and near, the binocular defocus curve, the low-contrast distance VA, the differences in the preferred reading distance and acuity at that distance, and the subjective quality of vision as reported in the questionnaires.
Clinical data were tabulated and de-identified on case report forms, along with VA data from a computerized data collection system. The data were imported into an MS Access database for data checking, collation, and preliminary analysis (Microsoft Corporation, Redmond, WA, USA). Statistical analyses were performed using the STATISTICA data analysis software system, Version 12 (StatSoft, Inc., Tulsa, OK, USA; www.statsoft.com). Statistical testing was performed using analysis of variance on continuous variables and appropriate nonparametric tests on categorical data. Statistical significance was set at P=0.05.
Results
A total of 25 bilateral trifocal subjects and 30 blended bifocal subjects were successfully recruited for the study. Table 1 contains a summary of the demographic characteristics of the subjects in the two groups. Scheduling changes resulted in several subjects being seen longer than 24 months postoperatively, but the mean difference in postoperative time between groups was not statistically significantly different. The average age in the trifocal group was statistically significantly lower than in the blended bifocal group. There was no difference in the axial length or mean keratometry between groups.
Table 1.
Demographic characteristics of subjects by group
| Trifocal (n=25, 50 eyes) | Blended bifocal (n=30, 60 eyes) | P-value | |
|---|---|---|---|
| Sex (female/male) | 9/15 | 15/15 | 0.41 |
| Age (years) | 53±8 (43, 69) | 65±9 (41, 78) | <0.01* |
| Surgery type (cataract/refractive lens exchange) | 4/21 | 5/25 | <0.01* |
| Time since surgery (days) | 433±217 (152, 729) | 411±258 (103, 792) | 0.71 |
| AL (mm) | 23.3±1.5 (20.15, 26.83) | 23.6±1.7 (20.8, 27.5) | 0.32 |
| Average K (D) | 43.6±1.3 (40.86, 46.27) | 43.8±1.7 (40.36, 47.2) | 0.50 |
Note:
Statistically significant difference (P<0.05). Continuous variables were tested with Analysis of Variance (ANOVA) while the categorical data (Sex, Surgery type) were tested with Fisher’s Exact Test (two-tailed). Data are presented as mean ± standard deviation (min, max).
Abbreviations: K, corneal power; n, number; D, diopters; AL, axial length.
Table 2 contains a summary of outcomes data for the two groups. The manifest refraction and the residual refractive cylinder were not statistically significantly different between groups. The residual astigmatism was also not statistically significantly different between the toric and spherical IOLs (P=0.66). Postoperatively, the monocular best-corrected VA at distance was also not statistically significant; the mean of both groups was slightly better than 0.0 logMAR (20/20). The preferred reading distance was around 44 cm for both study groups, with no statistically significant difference between groups; there was also no difference between groups in the adjusted VA for subjects at their preferred reading distance. Low-contrast VA was tested in the best-corrected and uncorrected states. The former is a better measure of the potential effects of the IOL, while the latter may be more relevant to the subjective responses of each subject to the questionnaires. There was a statistically significant difference between the corrected and uncorrected results for each study group, but this difference was less than two letters for both groups. There was no statistically significant difference between the study groups in either the corrected or uncorrected states. There was also no correlation between uncorrected VA and time after surgery for either IOL group.
Table 2.
Postoperative visit results
| Trifocal (n=25, 50 eyes) | Blended bifocal (n=30, 60 eyes) | P-value | |
|---|---|---|---|
| Manifest refraction, spherical equivalent (D) | 0.19±0.40 (−0.50, 1.25) | 0.18±0.32 (−0.37, 0.87) | 0.98 |
| Refractive cylinder (D) | −0.32±0.30 (−1.25, 0.00) | −0.40±0.32 (−1.25, 0.00) | 0.19 |
| Monocular corrected distance VA (logMAR) | −0.03±0.04 (−0.10, 0.10) | −0.02±0.05 (−0.16, 0.22) | 0.16 |
| Preferred reading distance (cm) | 44.2±6.3 (34, 61) | 43.4±4.0 (33, 52) | 0.53 |
| VA at preferred reading distance (logMAR) | 0.12±0.06 (0.01, 0.25) | 0.13±0.08 (0.00, 0.30) | 0.45 |
| Uncorrected low-contrast VA | 0.36±0.04 (0.28, 0.44) | 0.38±0.06 (0.24, 0.50) | 0.69 |
| Best-corrected low-contrast VA | 0.34±0.04 (0.24, 0.42) | 0.35±0.06 (0.24, 0.50) | 0.45 |
| NEI VFQ-39 near vision subset score | 94.5±5.6 (79, 100) | 92.2±8.4 (67, 100) | 0.25 |
Notes: Continuous variables were tested with Analysis of Variance (ANOVA), with statistical significance set at α 0.05. Data are presented as mean ± standard deviation (min, max).
Abbreviations: n, number; NEI VFQ, National Eye Institute Visual Function Questionnaire; VA, visual acuity; D, diopters.
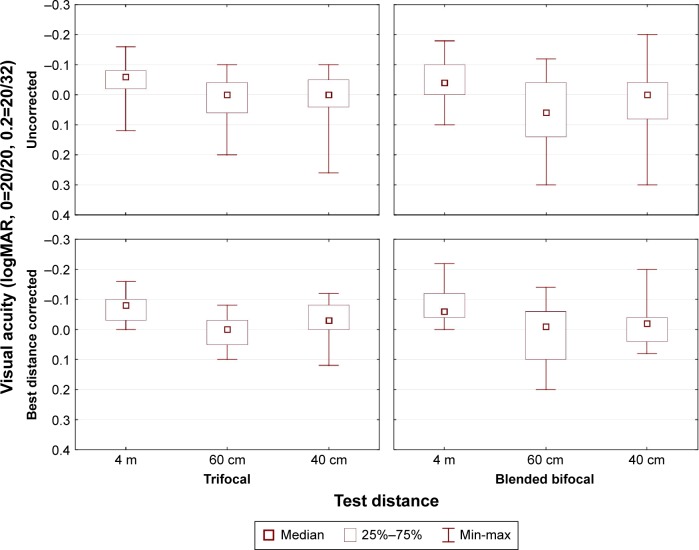
The distribution of binocular VA by distance and correction (uncorrected or with a best distance correction in place) is shown in the box–whisker plots in Figure 1. There is slightly more variability (larger “boxes”, longer “whiskers”) in the blended bifocal data, particularly at 60 cm. Note that the median value of uncorrected binocular VA achieved is better than or equal to 0.0 logMAR (20/20) for both groups at all distances, except for the uncorrected VA for the blended bifocal group at 60 cm. An analysis of variance showed a statistically significant effect of test distance (P<0.01) and correction status (P<0.01), but no statistically significant effect of IOL type.
Figure 1.
Distribution of visual acuity values by correction status, test distance, and study group.
Note: logMAR is an acuity measured using the logarithm of the minimum angle of resolution.
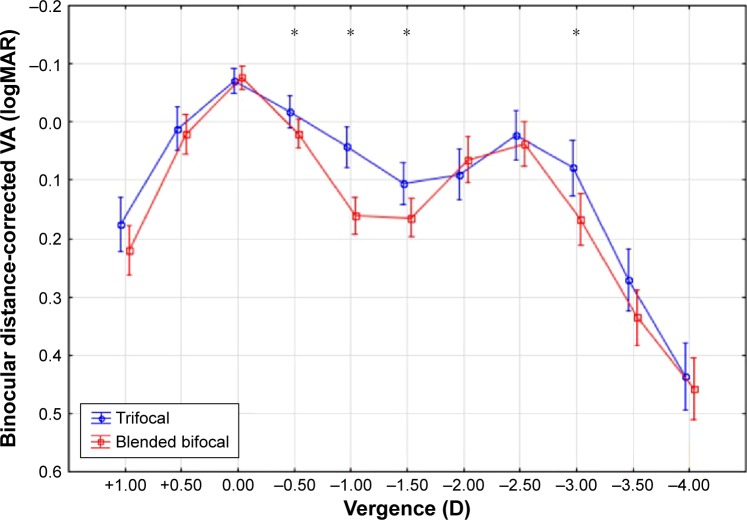
The binocular defocus curves for each study group, measured with the subject’s best distance correction in place, are shown in Figure 2. As can be seen, distance VA (vergence 0.0) and VA at a vergence of −2.5 D (the vergence equivalent to a viewing distance of 40 cm) are equivalent and near 0.0 logMAR (20/20) for both lens modalities. There are statistically significant differences in the VA at vergences of −0.5, −1.0, and −1.5 D, where the trifocal lens provided better VA (P<0.05); this corresponds to viewing distances from 2 m to 67 cm. There is also a statistically significant difference in the VA measured at −3.0 D, corresponding to a 33 cm viewing distance where the trifocal lens provided better VA. Forty percent (10/25) of trifocal subjects, versus only 3% (1/30) of blended bifocal subjects, had VA better than or equal to 0.1 logMAR (20/25) across a vergence range from +0.5 to −2.5 D; this difference was statistically significant (Fisher’s exact test, two-tailed, P<0.01).
Figure 2.
Binocular defocus curve, with distance correction in place.
Notes: *Statistically significant difference (P<0.05). Continuous variables were tested with Analysis of Variance (ANOVA). Vertical bars denote 95% confidence intervals.
Abbreviation: VA, visual acuity.
A score of 100 indicates no issues with any of the components of the near vision subscale of the NEI VFQ-39 visual function questionnaire. As shown in Table 2, both groups had mean scores over 90; there was no statistically significant difference in the scores by group (P=0.25).
There was also no statistically significant difference between groups in frequency (P=0.72), severity (P=0.51), or bothersome (P=0.26) measures of the Quality of Vision survey. A detailed distribution of the Quality of Vision survey results is shown in Figure 3; here, lower values indicate fewer issues with the quality of vision. While visual disturbances were experienced by some subjects, 68% of the trifocal subjects and 90% of the bifocal subjects rated all visual disturbances as 0, or “not at all” bothersome; the ratio was statistically significantly different (Fisher’s exact test, one-tailed, P=0.045).
Figure 3.
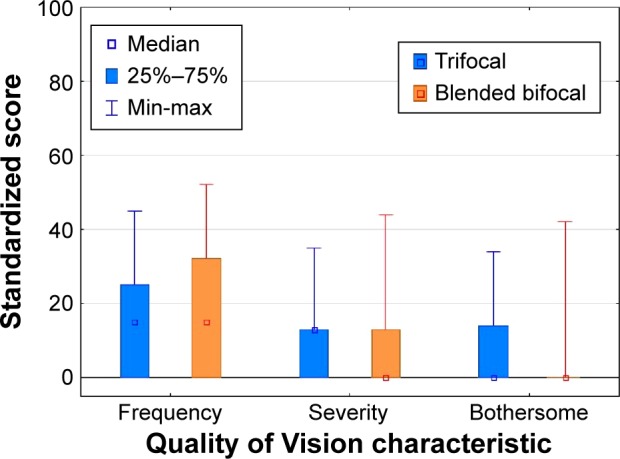
Summary scores for Quality of Vision test.
Discussion
Trifocal IOLs were designed to address the perceived deficiency in intermediate vision reported by some patients when they were implanted with a bifocal IOL that provided good near and distance vision.15 The potential concern with providing a third focal point was the possibility that visual disturbances would be increased, as there would be two out-of-focus images with one in-focus image at any viewing distance. Diffractive trifocal designs attempt to reduce this potential issue by having an intermediate focus that contributes some of the unfocused light to “near”, a scenario that requires the near vergence to be twice the intermediate vergence (eg, 3.50 D near, 1.75 D intermediate).16
The results of the present study indicate that significantly better intermediate vision can be achieved with use of binocular trifocal IOL implantation when compared to the implantation of the blended bifocal IOLs, as demonstrated by the defocus curve in Figure 2. The differences between study groups was highest at a vergence of −1.0 D, equivalent to a viewing distance of 1 m, where the mean VA in the trifocal group was just over one line better. Interestingly, the VA was also statistically significantly better at 33 cm. This may be because only the nondominant eye of the blended IOL group provides a near focus, and because the near focal point of the trifocal is slightly higher than that of the “near” bifocal (+3.33 D for the trifocal vs +3.00 D for the bifocal, both at the IOL plane). The diffractive bifocal segment of the trifocal at the periphery of the lens has a +3.75 D add, which would also be a contributing factor. It is also important to note that the VA was not statistically significantly different at vergences of −2.0 or −2.5 D, corresponding to viewing distances of 50 and 40 cm, respectively.
The defocus curves for the blended bifocal group and the trifocal IOL group provided in the present study are reasonably consistent with previous reports, though we observed less drop-off of distance VA in the blended bifocal group and less drop-off of near VA in the trifocal group than has been previously reported.8,10 The significant differences observed in the defocus curve corresponded to viewing distances from 2 m (−0.5 D) to 67 cm (−1.5 D), with a mean difference at the latter defocus of 3 logMAR letters, or about a half line of acuity. While no comparative blended bifocal data were available in the literature, these differences are consistent with results observed between the same trifocal IOL and a bilateral near bifocal (AT LISA 801, Carl Zeiss Meditec).17 At 50 cm (−2.0 D), the mean difference was less than a letter, and not statistically significant. The statistically significantly better VA at intermediate observed for the trifocal IOL is at a distance that would matter more for activities at arm’s length or longer, and would be less important for intermediate viewing activities such as computer use.
While the defocus curve suggests significantly better intermediate vision with the trifocal IOL, a test of binocular VA at near, intermediate (60 cm), and distance revealed no significant differences between IOL groups. This is likely a function of the intermediate test distance. The intermediate test distance used was 60 cm (with a corresponding vergence of −1.67 D), near midway between the two points (−1.5 and −2.0 D) on the defocus curve in Figure 2. The difference in binocular VA between the two groups at 60 cm was 0.02 logMAR, or one letter. This indicates that the results from the VA testing and defocus curve are consistent.
There were neither any differences in the low-contrast acuity between the lens groups nor between the preferred reading distance and the VA at that reading distance. The reading results are similar to those that have been reported for a trifocal versus bifocal IOL comparison.18
Both the NEI VFQ-39 near vision subscale and the Quality of Vision questionnaire suggest that the visual quality and effect of visual disturbances are similar between the two study groups,2,3 though there was an indication that fewer subjects with the blended bifocal found visual disturbances bothersome. One should note that more subjects in the trifocal group were younger when compared to the blended bifocal group; this may at least partly explain the greater bother reported in the trifocal group, as these younger subjects may have had relatively higher visual demands/expectations. Results in the blended bifocal group were remarkably similar to the results obtained for a single-vision IOL implanted in a previous study at the same site.4 It is possible that placing the ReSTOR +2.5 D lens in the dominant eye allows for visual performance similar to a monofocal IOL, as suggested in one study where both eyes were implanted with this bifocal IOL.7
Conclusion
In summary, this is the first reported comparison between a blended bifocal modality and bilateral trifocal implantation. Both the trifocal and blended bifocal modalities used in the present study provided subjects with excellent binocular near and distance vision, with similar low rates of visual disturbances and good reported functional vision. The trifocal IOL provided significantly better intermediate VA at vergences corresponding to viewing distances from 2 m to 67 cm, with similar VA between groups at vergences corresponding to viewing distances from 50 to 40 cm. The differences are likely to be appreciated more for arms’ length viewing (eg, car dashboard, grocery shelf) than for closer activities such as computer use.
Acknowledgments
IFocus Øyeklinikk AS received an investigator-initiated study grant from Alcon to conduct this research (IIT proposal #15446521). IFocus Øyeklinikk AS provided funding to Science in Vision to assist with data analysis and preparation of this manuscript. Sarah Y Makari, OD, a consultant to Science in Vision, received compensation for providing writing assistance to the authors in preparation of the manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;9:CD003169. doi: 10.1002/14651858.CD003169.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, García-Lázaro S, Montés-Micó R. Optical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocal. J Refract Surg. 2013;29(11):749–754. doi: 10.3928/1081597X-20131021-04. [DOI] [PubMed] [Google Scholar]
- 3.Carson D, Hill WE, Hong X, Karakelle M. Optical bench performance of AcrySof(®) IQ ReSTOR(®), AT LISA(®) tri, and FineVision(®) intraocular lenses. Clin Ophthalmol. 2014;8:2105–2113. doi: 10.2147/OPTH.S66760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol. 2013;7:1979–1985. doi: 10.2147/OPTH.S52922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kohnen T, Nuijts R, Levy P, Haefliger E, Alfonso JF. Visual function after bilateral implantation of apodized diffractive aspheric multifocal intraocular lenses with a +3.0 D addition. J Cataract Refract Surg. 2009;35(12):2062–2069. doi: 10.1016/j.jcrs.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Pedrotti E, Mastropasqua R, Passilongo M, Parisi G, Marchesoni I, Marchini G. Comparison of two multifocal intraocular lens designs that differ only in near add. J Refract Surg. 2014;30(11):754–760. doi: 10.3928/1081597X-20141021-07. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi K, Ogawa S, Manabe S, Hirata A. Visual outcomes in eyes with a distance-dominant diffractive multifocal intraocular lens with low near addition power. Br J Ophthalmol. 2015;99(11):1466–1470. doi: 10.1136/bjophthalmol-2014-306476. [DOI] [PubMed] [Google Scholar]
- 8.Mastropasqua R, Pedrotti E, Passilongo M, Parisi G, Marchesoni I, Marchini G. Long-term visual function and patient satisfaction after bilateral implantation and combination of two similar multifocal IOLs. J Refract Surg. 2015;31(5):308–314. doi: 10.3928/1081597X-20150423-04. [DOI] [PubMed] [Google Scholar]
- 9.Kretz FT, Müller M, Gerl M, Gerl RH, Auffarth GU. Binocular function to increase visual outcome in patients implanted with a diffractive trifocal intraocular lens. BMC Ophthalmol. 2015;15:110. doi: 10.1186/s12886-015-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mojzis P, Majerova K, Hrckova L, Piñero DP. Implantation of a diffractive trifocal intraocular lens: one-year follow-up. J Cataract Refract Surg. 2015;41(8):1623–1630. doi: 10.1016/j.jcrs.2014.11.050. [DOI] [PubMed] [Google Scholar]
- 11.Marques EF, Ferreira TB. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 2015;41(2):354–363. doi: 10.1016/j.jcrs.2014.05.048. [DOI] [PubMed] [Google Scholar]
- 12.Kohnen T, Titke C, Böhm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016;161:71–77.e1. doi: 10.1016/j.ajo.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, National Eye Institute Visual Function Questionnaire Field Test Investigators Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 14.McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–5545. doi: 10.1167/iovs.10-5341. [DOI] [PubMed] [Google Scholar]
- 15.Alfonso JF, Fernández-Vega L, Amhaz H, Montés-Micó R, Valcárcel B, Ferrer-Blasco T. Visual function after implantation of an aspheric bifocal intraocular lens. J Cataract Refract Surg. 2009;35(5):885–892. doi: 10.1016/j.jcrs.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37(11):2060–2067. doi: 10.1016/j.jcrs.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 17.Mojzis P, Kukuckova L, Majerova K, Liehneova K, Piñero DP. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014;30(10):666–672. doi: 10.3928/1081597X-20140903-06. [DOI] [PubMed] [Google Scholar]
- 18.Jonker SM, Bauer NJ, Makhotkina NY, Berendschot TT, van den Biggelaar FJ, Nuijts RM. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015;41(8):1631–1640. doi: 10.1016/j.jcrs.2015.08.011. [DOI] [PubMed] [Google Scholar]