Abstract
Stigma has become a gendered phenomenon that affects increasing numbers of HIV-infected women worldwide. This study examined the role of age as a possible moderator of the relationship between stigma and antiretroviral therapy adherence, CD4% and viral load among 120 HIV-infected women. A secondary analysis was conducted using data from the Keeping Healthy and Active with Risk Reduction and Medication Adherence (KHARMA) Project, an National Institutes of Health (NIH) funded randomized controlled trial to improve Antiretroviral treatment (ART) adherence and reduce risky behaviors in HIV-infected women at five clinical sites in a South-eastern city from 2005 to 2008. Stigma was measured using the Perceived Personal Stigma of Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (HIV/AIDS) scale. Among participants <50 years old (n=90), age was significantly associated with viral load (rho=−.24, p=.02) and stigma was negatively associated with CD4% (r =−.26, p=.02). For the 30 participants >50 years old, age was not significantly associated with viral load, stigma or CD4%, and there was no significant association between stigma and CD4% (r=.07, p=.70). These findings indicate the need for further study regarding this potential moderating effect and possible interventions to address the susceptibility of younger women to the harmful effects of stigma.
Keywords: Adherence, Aging, Antiretroviral therapy, HIV, Stigma, Women
INTRODUCTION
HIV has become one of the most stigmatized health conditions in modern societies due to its associations with risky sexual behaviors, substance abuse and fears related to its possible contagiousness.1,2 Stigma is defined by the “co-occurrence of a label, a stereotype, separation, status loss, or discrimination in a context where power is exercised.”3 HIV-related stigma is “the collection of adverse attitudes, beliefs and actions of others against people living with or affected by HIV, which may result in deleterious internalized beliefs or actions taken by persons living with HIV infection that may result in negative health outcomes.”4
Recent shifts in the incidence of HIV infections among ethnic minorities and women parallel the increasing susceptibility of HIV-infected women to experience a stigmatizing event.5,6 Among a cohort of diverse Canadians, Loutfy and colleagues7 found that Black individuals experienced more stigma than Aboriginal, Asian, Latin and White individuals, and the highest rates of HIV-related stigma were reported by Black women and Asian men. In the United States (US), HIV-infected women often experience higher rates of “personal (internalized)” stigma than HIV-infected men.8–10 HIV-infected women may experience multiple levels of stigma due to the labels and stereotypes commonly associated with being female, HIV-infected and socially marginalized (i.e., poor, low education, substance user, or racial/ethnic minority).11,12 African American women are particularly vulnerable to experiencing a stigmatizing event due to their over-representation among women infected with HIV,13 and due in part to the double standard that “blames” a woman’s behavior for becoming infected with HIV while excusing the behaviors of HIV-infected men.14,15
The effects of HIV-related stigma may include psychological or physiological problems and suboptimal adherence to antiretroviral therapy (ART).16,17 Women who experience personal stigma may report feelings of shame, depression, and social isolation.9,18 Similarly, HIV-infected older adults report more stigma than their younger counterparts8,16,17 and they describe stigma as feeling ostracized, isolated, lonely, and rejected due to their HIV status and age.19 These feelings may contribute to increased ART avoidance behaviors that result in poor adherence to ART regimens.20,21 Suboptimal ART adherence is associated with lower CD4% and higher HIV viral loads, both of which are key health indicators for people living with HIV/AIDS.22–24 While it has been shown that HIV-related stigma adversely affects ART adherence, studies that demonstrate a direct link between stigma and clinical health outcomes such as CD4% and Viral Load (VL) remain sparse.
By 2015, half of those infected with HIV will be 50 years of age or older,25 and women will account for approximately 25% of those aging with HIV/AIDS in the US.26 Despite the increasing number of women aging with HIV, little is known regarding the relationships among age, HIV-related stigma, ART adherence and clinical indicators of health in HIV-infected women. Instead, many studies on HIV-related stigma have focused on (1) how stigma disrupts the psychological health of HIV-infected men and women,27,28 (2) the impact of stigma on the Quality of Life (QoL) of HIV-infected older adults,29,30 or (3) the relative rates of stigma experienced by younger versus older adults.18,31 Few women are included in these studies, and this limits generalizability to HIV infected women. To the best of our knowledge, no studies have examined the effect of age on the relationship between stigma and ART adherence. Furthermore, no studies have investigated whether age moderates the influence of stigma on HIV-related clinical outcomes such as CD4% and viral load in HIV-infected women. This is an important gap that should be addressed because women are living longer with HIV. Therefore, this study examined age as a moderator of the effect of personal stigma on ART adherence and HIV clinical markers (CD4% and viral loads). This study also examined associations between personal stigma and adherence, CD4% and HIV viral loads (VL) among HIV-infected women. The study is based on the theoretical work on personal (i.e., internalized) stigma by Goffman32 and Florom-Smith and De Santis.33
METHODS
Study Sample
This study consists of a secondary analysis of baseline data from the keeping healthy and active with risk reduction and medication adherence (KHARMA) Project.34,35 KHARMA was a randomized controlled behavioral trial that tested the efficacy of a nurse-led motivational group intervention to improve ART adherence and reduced risky behaviors in 207 HIV-infected women. Details of the study are presented elsewhere.34,35 Recruitment occurred from 2005 to 2008 at five infectious disease clinical sites in a large south-eastern city. Inclusion criteria required participants to be: (1) HIV seropositive; (2) English-speaking; (3) female by birth; (4) prescribed ART; (5) mentally stable based on a screening measure; and (6) willing to participate in all study activities. Women were assessed at baseline and then followed at 2 weeks and 3, 6, and 9 months after completion of the intervention. Data were collected using an Audio Computer-Assisted Self Interview (ACASI) on laptop computers. Laboratory data regarding CD4% and viral load were extracted from the participant’s electronic medical records. Of the 207 participants, data was available for both CD4 counts and viral load at the baseline assessment for 120 participants. These 120 participants comprise the sample for this analysis. This study was approved by the research committees at the participating recruitment sites, when required, and the University’s Institutional Review Board (IRB). Each study participant provided written, informed consent prior to participating in study activities. Participants received monetary compensation for attendance at study group sessions ($10) and study interviews ($25).
Measures
Demographic information
Information regarding participants age, race/ethnicity, income, education, etc. was collected using a sociodemographic questionnaire. For this analysis, we dichotomized age (<50 and ≥50 years old) based on widely accepted guidelines from the Centers for Disease Control and Prevention,36 which consider HIV-infected individuals aged 50 years and older as older adults.
Personal stigma
The 24-item Perceived Personal Stigma of HIV/AIDS scale37 was used to measure attitudes of self-regarding, HIV/AIDS, shame, guilt, blame and embarrassment. Participants rated each item on a four-point Likert scale from 1 (strongly agree) to 4 (strongly disagree). The possible scores ranged from 24 to 72, with higher scores indicating higher levels of perceived personal stigma. The internal reliability for this scale was α=.75.
Antiretroviral therapy adherence
Antiretroviral therapy adherence was measured in two ways. First, adherence was measured electronically using the Medication Event Monitoring System (MEMS) 6 Track Caps (Aardex Group Ltd, Sion, Switzerland). MEMS caps electronically monitor how often a participant opens a bottle of medication. The caps were placed on one bottle of each participant’s antiretroviral medication (based on protocol, usually a protease inhibitor or Non-Nucleoside Reverse Transcriptase Inhibitors [NNRTI]) approximately two weeks prior to baseline assessment to determine baseline adherence. For this analysis, MEMS adherence refers to the percent of prescribed doses (0–100%) taken during the baseline period.
Second, a self-report measure, the Antiretroviral General Adherence Scale (AGAS), was also used to assess adherence. The AGAS is composed of five items, each on a six-point Likert scale, that focus on the ease and ability to take ART in the past 30 days according to a health care provider’s recommendation.38 Higher scores indicated higher levels of adherence. There was good internal reliability for this sample with α=.85 at baseline. For this analysis, AGAS adherence refers to self-reported adherence as a percentage.34
HIV clinical indicators
CD4% and HIV viral load (VL) (log) were utilized as general indicators of immune status and HIV circulating viral activity. All of the data for the CD4 percents and the HIV viral load were abstracted from medical records using the data point nearest to the baseline assessment. Both clinical indicators were expected to improve with adherence to ART, and VL has been shown to be the most sensitive to adherence. A CD4% of ≤14 is consistent with an AIDS diagnosis, and viral load of <2.6 corresponds with a viral load of <400 copies per milliliter, which was considered undetectable at the time KHARMA was conducted.
Data Analysis
Initially, the data were analyzed using descriptive statistics including frequency distributions, means, standard deviations and ranges. Chi square tests (for categorical variables) and t-tests (for continuous and ordinal variables) were used to determine whether the independent variables were significantly related to ART adherence, CD4% and viral load. Bivariate correlations were performed using either Pearson’s r correlation (i.e., for normally distributed variables) or Spearman’s rho (i.e., for variables that were highly skewed or otherwise did not follow a normal distribution). These correlations were performed for all subjects and for the two age categories (i.e., age <50 or ≥50). Because there were only 30 subjects over the age of 50, correlations of 0.3 or higher are noted because these are considered moderate effect sizes39 and may have clinical relevance even if statistical significance was not achieved due to the small sample sizes. The Statistical Package for the Social Sciences (SPSS) for Windows version 21 (IBM Corporation, 2012) was used to perform all analysis.
RESULTS
Characteristics of the Study Population
Characteristics of the 120 participants included in these analysis are presented in Table 1. Overall, the participants ranged in age from 18 to 67 years with an average age of 43.6 years (SD=9.4); 75% were younger than age 50. The majority was African American (93.3%); heterosexual (76.7%), that had not graduated from high school, (74.2%), was unemployed (82.5%), and had annual incomes of $10,000 or less (67.2%).
Table 1.
Descriptive characteristics of the sample population at baseline (N=120).
| Characteristics | <50 years old n=90 (75.0%) |
≥50 years old n=30 (25.0%) |
Overall N=120 |
|---|---|---|---|
| Ethnicity (%) | |||
| Non-African American | 5(5.6%) | 3(10.0%) | 8(6.7%) |
| African American | 85(94.4%) | 27(90.0%) | 112(93.3%) |
| Sexual Identity | |||
| LGBT or unsure | 22(24.4%) | 6(20.0%) | 28(23.3%) |
| Heterosexual | 68(75.6%) | 24(80.0%) | 92(76.7%) |
| Single | 57(64.0%) | 29(96.7%) | 86(72.3%)** |
| Partnered | 32(36.0%) | 1(3.3%) | 33(27.7%) |
| Education Level | |||
| < High School Grad | 68(75.6%) | 21(70.0%) | 89(74.2%) |
| ≥ High School grad | 22(24.4%) | 9(30.0%) | 31(25.8%) |
| Unemployed | 74(82.2%) | 25(83.3%) | 99(82.5%) |
| Employed | 16(17.8%) | 5(16.7%) | 21(17.5%) |
| Annual Incomeb | |||
| ≤ $10,000 | 59(67.0%) | 19(67.9%) | 78(67.2%) |
| > $10,000 | 29(33.0%) | 9(32.1%) | 38(32.8%) |
| M(SD) | Range | M(SD) | Range | M(SD) | Range | ||
|---|---|---|---|---|---|---|---|
| Age, years | 39.5(6.8) | 18–49 | 55.7(4.2) | 50–67 | 43.6(9.4) | 18–67 | |
| Duration of HIVa | 8.9(5.9) | 1–26 | 9.5(5.8) | 1–22 | 9.1(5.8) | 1–26 | |
| Duration on ART | 5.2(3.9) | 0–17 | 6.3(4.8) | 0–16 | 5.5(4.2) | 0–17 | |
| (ART years >5) | 40(44.4%) | 16(53.3%) | 56(46.7%) | ||||
| Adherence: AGAS | 20.3(3.3) | 12–25 | 20.9(2.5) | 15–25 | 20.5(3.2) | 12–25 | |
| (AGAS as a%) | 81.2(13.3) | 48–100 | 83.7(10.1) | 60–100 | 81.8(12.7) | 48–100 | |
| Adherence: MEMS | 72.1(32.9) | 0–100 | 79.6(32.6) | 8.3–100 | 74.0(32.9) | 0–100 | |
| (Adherence ≥95%) | 32(35.6%) | 16(53.3%) | 48(40.0%) | ||||
| CD4 (%) | 18.6(11.2) | 1–61 | 23.3(11.0) | 7–45 | 19.7(11.3) | 1–61* | |
| Viral Load (log) | 2.6(1.1) | 1.7–5.46 | 2.3(0.8) | 1.7–4.93 | 2.5(1.0) | 1.7–5.46 | |
| V load (log) ≤2.60 | 56(62.2%) | 24(80.0%) | 80(66.7%) | ||||
| Stigma, Personalc | 45.2(10.5) | 25–72 | 45.9(11.1) | 24–68 | 45.4(10.6) | 24–72 | |
p<.05;
p< .01;
p<.001;
1 missing;
4 missing;
3 missing
For the baseline labs, the time since collection of the specimens ranged from 0 to 206 days, and the median time between baseline and collection of the specimen was approximately 27 days prior.
The results of Chi-square tests show a significant association between relationship status and age (χ2=11.914, df=1, p=.001). There was a significantly larger proportion of older women who were single (96.7%) than younger women who were single (64.0%). On average, participants had been living with HIV for 9.1 years (SD=5.8), and they were on ART for 5.5 years (SD=4.2); these rates were similar between the age groups. Electronically measured (i.e., MEMS) adherence averaged 74% (SD=32.9%) overall with 40% of the participants achieving adherence of 95% or better. Self-report (i.e., AGAS) adherence averaged 81.8% (SD=12.7%), and there were no significant differences between the two age groups. CD4% averaged 19.7(SD=11.3), and viral loads (log) averaged 2.5(SD=1.0). There were significant differences in CD4% between the age groups, with younger women having significantly lower CD4% (p=.045); however, there were no significant differences in viral loads between the age categories. The mean personal stigma score was 45.4(SD=10.6), and there were no significant differences between the age categories.
Correlations between Age, Adherence and Personal Stigma
We examined the associations between age, adherence (i.e., MEMS and AGAS), viral loads, CD4%, and personal stigma across all participants. Bivariate analysis revealed that age was significantly positively associated with MEMS adherence (rho=.20, p=.03), CD4% (r=.21, p=.02), and viral load (log) (rho=−.22, p=.02; data not shown). Bivariate analysis of correlations stratified by age group (i.e., <50 years of age and ≥50 years of age) were also conducted. Among participants less than 50 years old, lower stigma scores were significantly associated with higher CD4% (r=−.26, p=.02). In those less than 50 years old, younger age was also associated with higher viral load (log). MEMS adherence and CD4 was inversely associated with viral load (log) which is anticipated direction: as adherence increases, viral load decreases and as viral load decreases, it is expected clinically that CD4% will rise. This is in contrast to the participants aged 50 years and older among whom age was not associated with adherence (i.e., neither MEMS nor AGAS), VL (log), CD4% or stigma. Additionally, there was no significant association between personal stigma and CD4% (r=.07, p=.70; see Table 2).
Table 2.
Correlations between age, adherence, CD4%, viral load (log) and personal stigma.
| Age ≥ 50 | Age | AGAS | MEMS | CD4% | Viral Load (log) |
Personal Stigma |
|---|---|---|---|---|---|---|
| Age < 50 | ||||||
| Age | — | −0.021a | 0.140b | 0.299a | −0.098b | 0.244a |
| AGAS | 0.018a | — | 0.426b* | 0.148a | 0.045b | 0.085a |
| MEMS | 0.108b | 0.048b | — | 0.290b | −0.154b | 0.028b |
| CD4% | 0.074a | −0.057a | 0.055b | — | −0.593b ** | 0.074a |
| Viral Load (log) | −0.243b * | 0.062b | −0.275b ** | −0.380b *** | — | −0.014b |
| Personal Stigma | 0.093a | −0.147a | −0.137b | −0.256a * | 0.020b | — |
p < .05;
p < .01;
p < .001
Pearson’s r reported for normally distributed variables
Spearman’s rho reported for non-normal skewed distributed variables
Potential Moderating Effects of Age
We conducted an exploratory test of the moderation of age on the association between personal stigma and CD4%. We used stepwise linear regression to test the impact of the age-by-stigma interaction effect after adjusting for the individual main effects of age and stigma, and controlling for adherence. The moderating effect of age on the association between personal stigma and CD4% is illustrated in Figure 1. Among women less than 50 years old, higher stigma was associated with a lower CD4% whereas among older women, stigma and CD4% were not significantly related. Although a stronger association between stigma and CD4% was identified among younger women, the associations between age and stigma, age and CD4%, and viral load and CD4% were stronger for older women than for younger women (i.e., higher r values). These results suggest a possible, although not definitive, moderating effect of age for each of these associations.
Figure 1.
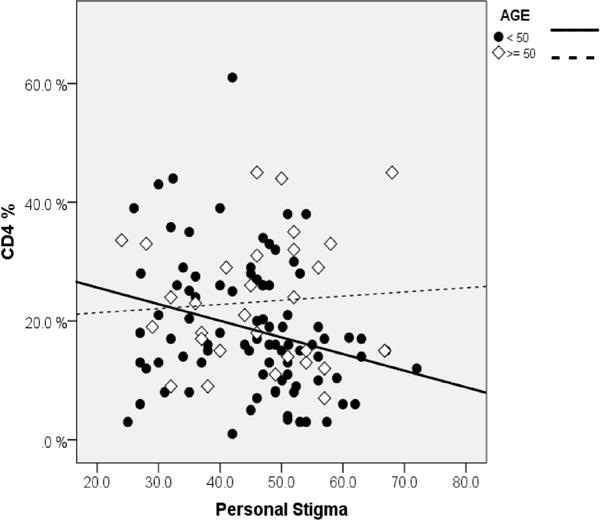
Scatterplot of CD4% by personal stigma moderated by age.
DISCUSSION
The purpose of this study was to examine the moderating effect of age on perceived personal stigma, ART adherence (i.e., MEMS and AGAS), CD4% and viral load among a group of HIV-infected women. In addition, this study also examined associations between stigma and adherence, CD4% and VLs among HIV-infected women. This study identified a significant difference in baseline CD4% between two age groups with women older than 50 years having higher CD4 percentages. Although there were no significant differences in ART adherence between the younger (i.e., age <50) and older women (i.e., age ≥50), the mean scores on both self-report and MEMS adherence were higher in the older group. Also a larger proportion of the older group achieved at least 95% or greater adherence on the MEMS report. This finding was consistent with previous reports, which indicated that older HIV-infected women were more likely to exhibit higher ART adherence compared with their younger counterparts, resulting in higher CD4%.23
Age may have a moderating effect on the relationships between stigma and ART adherence and stigma and HIV clinical health outcomes (i.e., CD4% and viral load). The younger women in this study may have been more susceptible to the negative impact of stigma on CD4 levels. However, the influence of age on the relationship between stigma, ART adherence, CD4% and viral loads could not be definitively established due to the non-significant findings.
When considering the moderating effect of age on the relationship between stigma and ART adherence, the results from the current study were inconsistent with the results from previously reported empirical and observational studies. Previous studies have shown that HIV-related stigma had a negative impact on the ART adherence practices among HIV-infected women in general and HIV-infected older women in particular.10,21 However, in contrast with other researchers, we did not find a relationship between stigma and ART adherence. Prior to analysis, we anticipated that participants aged 50 years or older would report higher levels of personal stigma that in turn would be associated with lower ART adherence compared with younger participants.40 Another expectation was that the moderating effect of age on the relationship between stigma and HIV clinical outcomes would be associated with lower CD4 percentages and higher viral loads among those aged ≥50 years. However, our study demonstrated that stigma affected women of all ages; nonetheless, younger women were more susceptible to stigma than older women. Interestingly, a significant association existed between age and ART adherence and the HIV clinical indicators (CD4% and VL). As age increased, MEMS adherence increased, CD4% increased and VL decreased among the women as a whole. Although not statistically significant, HIV-infected women ≥50 years took a higher percentage of their prescribed ART doses, as assessed by the MEMS method. In women <50 years of age, we found that higher stigma scores were associated with lower CD4%. Regression results between stigma and CD4% split by age category (controlling for adherence), showed that age may be a potential moderator of this association.
There were several limitations to this study. First, cross-sectional design limits causal inferences that might be made related to the data. In addition, selection bias may be present because the parent study drew participants that were self-selected to be in a study to improve ART adherence. Similarly, the small sample size of participants over age 50 may have introduced further bias to the study, which limits the generalizability of the results. Second, this study was conducted in an urban setting in the south, and the findings may not be generalizable to other populations or regions. Although significant correlations were present among the variables of interest, the low magnitude of the correlations limits any attempt to generalize the findings from this study.
Third, the nature of our moderation test was underpowered for a proper test of moderation because there were only 30 participants aged 50 years or older in the sample. According to Warner,41 a regression model should have at least 15 subjects for each independent variable. More participants over the age of 50 are necessary to adequately test the potential age moderating effect at 80% power. In order to achieve 80% and 5% level of significance to detect differences in correlation for younger subjects <50 compared to older subjects (≥50), a total sample size of 200 (100 in each age group) would be needed to detect difference of 0.4 between the groups, and 352 would be needed to detect differences in correlation of 0.3 (power analysis completed using PASS 14 Power Analysis and Sample Size Software (2015; NCSS, LLC. Kaysville, Utah, USA, ncss.com/software/pass). While it is plausible that age moderates the relationship between stigma and CD4%, the moderation model presented in this study may not be generalizable to the broader population of women living with HIV due to several factors. Therefore, this study was not truly capable of determining the effect of age on the relationships among stigma, ART adherence, CD4% and viral loads. Larger studies with greater sample sizes are needed in both age categories to better test age as a moderator of stigma and CD4%.
Despite these limitations, this study is one of the first to examine relationships between age, HIV-related stigma, ART adherence and clinical indicators of health in HIV-infected women. Stigma has become a gendered phenomenon that affects increasing numbers of HIV-infected women worldwide.42,43 Women account for 25% of the people living with HIV in the United States,44 and many of these women will experience a stigmatizing event.45 The societal factors that contributed to their risk of acquiring HIV place them at higher risk for experiencing HIV-related stigma.11,12 The knowledge generated from this study may be useful in the development of gender-specific interventions that reduce the impact of stigma on the lives of HIV-infected women. By understanding the experiences of stigmatization, clinicians may be able to ask women about their experiences with stigma and provide referrals for adherence and/or mental health counseling, social services, etc to ameliorate the effects of stigma on health outcomes.
Acknowledgments
This work was supported in part by grants from The National Institutes of Health (NINR grant # R01NR008094: M. Holstad, PI; NINR grant # T32NR012715: S. Dunbar, PI), & the Emory Center for AIDS Research (P30 AI050409).
ABBREVIATIONS
- KHARMA
Keeping Healthy and Active with Risk Reduction and Medication Adherence
- NIH
National Institutes of Health
- ART
Antiretroviral therapy
- HIV/AIDS
Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome
- ACASI
Audio Computer-Assisted Self Interview
- MEMS
Medication Event Monitoring System
- AGAS
Antiretroviral General Adherence Scale
- NNRTI
Non-nucleoside reverse-transcriptase inhibitors
- VL
Viral Load
- SPSS
Statistical Package for the Social Sciences
- IRB
Institutional Review Board
- CDC
Centers for Disease Control and Prevention
Footnotes
CONFLICTS OF INTEREST
The authors report no real or perceived vested interests that relate to this article that could be construed as conflicts of interest.
References
- 1.Drewes J, Kleiber D. Contagiousness under antiretroviral therapy and stigmatization towards people with HIV. AIDS Care. 2014;26:1383–1386. doi: 10.1080/09540121.2014.913768. [DOI] [PubMed] [Google Scholar]
- 2.Sayles JN, Ryan GW, Silver JS, et al. Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. J Urban Health. 2007;84:814–828. doi: 10.1007/s11524-007-9220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebied EME. Factors contributing to HIV/AIDS-related stigma and discrimination attitude in Egypt: Suggested stigma reduction guide for nurses in family health centers. J Educ and Pract. 2014;5:35–46. [Google Scholar]
- 5.Bunting SM. Sources of stigma associated with women with HIV. Adv Nurs Sci. 1996;19:64–73. doi: 10.1097/00012272-199612000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Quinn SC. AIDS and the African American Women: the triple burden of race, class, and gender. Health Educ Q. 1993;20:305–320. doi: 10.1177/109019819302000303. [DOI] [PubMed] [Google Scholar]
- 7.Loutfy MR, Logie CH, Zhang Y, et al. Gender and ethnicity differences in HIV-related stigma experienced by people living with HIV in Ontario, Canada. PLoS One. 2012;7:e48168. doi: 10.1371/journal.pone.0048168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bogart LM, Cowgill BO, Kennedy D, et al. HIV-related stigma among people with HIV and their families: a qualitative analysis. AIDS Behav. 2008;12:244–254. doi: 10.1007/s10461-007-9231-x. [DOI] [PubMed] [Google Scholar]
- 9.Colbert AM, Kim KH, Serika SM, et al. An examination of the relationships among gender, health status, social support, and HIV-related stigma. J Assoc Nurses AIDS Care. 2010;21:302–313. doi: 10.1016/j.jana.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolitski RJ, Pals SL, Kidder DP, et al. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS Behav. 2009;12:1222–1232. doi: 10.1007/s10461-008-9455-4. [DOI] [PubMed] [Google Scholar]
- 11.Logie CH, James L, Tharao W, et al. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8:E1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Storholm ED, Halkitis PN, Kupprat SA, et al. HIV-related stigma as a mediator of the relation between multiple-minority status and mental health burden in an aging HIV-positive population. J HIV/AIDS and Social Services. 2013;12:9–25. doi: 10.1080/15381501.2013.767557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone VE. HIV/AIDS in women and racial/ethnic minorities in the U.S. Curr Infect Dis Rep. 2012;14:53–60. doi: 10.1007/s11908-011-0226-4. [DOI] [PubMed] [Google Scholar]
- 14.Asiedu GB, Myers-Bowman KS. Gender differences in the experiences of HIV/AIDS-related stigma. A qualitative study in Ghana. Health Care Women Int. 2014;35:703–727. doi: 10.1080/07399332.2014.895367. [DOI] [PubMed] [Google Scholar]
- 15.Pannetier J, Lelièvre E, Le Cœur S. HIV-related stigma experiences: understanding gender disparities in Thailand. AIDS Care. 2015;19:1–9. doi: 10.1080/09540121.2015.1096888. [DOI] [PubMed] [Google Scholar]
- 16.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21:742–753. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 17.Vyavaharkar M, Moneyham L, Corwin S, et al. Relationships between stigma, social support and depression in HIV-infected African American women living in the rural southeastern United States. J Assoc Nurses AIDS Care. 2010;21:144–152. doi: 10.1016/j.jana.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a southern minority population with HIV disease. J Assoc Nurses AIDS Care. 2008;19:98–104. doi: 10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Emlet CA. A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care STDs. 2006;20:350–358. doi: 10.1089/apc.2006.20.350. [DOI] [PubMed] [Google Scholar]
- 20.Langebeek N, Gisolf EH, Reiss P, et al. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med. 2014;12:142. doi: 10.1186/PREACCEPT-1453408941291432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rintamaki LS, Davis TC, Skripkauskauskas S, et al. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDs. 2006;20:359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 22.Earnshaw VA, Smith LR, Chaudoir SR, et al. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17:1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tyer-Viola LA, Corless IB, Webel A, et al. Predictors of medication adherence among HIV-positive women in North America. Journal Obstet Gynecol Neonatal Nurs. 2014;43:168–178. doi: 10.1111/1552-6909.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangsberg DR, Perry S, Charlebois ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 25.High KP, Brennan-Ing M, Clifford DB, et al. HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and aging working group. J of Acquir Immune Defic Syndr. 2012;60(Suppl 1):S1–S18. doi: 10.1097/QAI.0b013e31825a3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Diagnoses of HIV infection among adults aged 50 years and older in the United States and Dependent areas, 2007–2010. 2013 Website: http://www.cdc.gov/hiv/library/reports/surveillance/2010/surveillance_Report_vol_18_no_3.html. Accessed 2015.
- 27.Foster PP, Gaskins SW. Older African Americans management of HIV/AIDS stigma. AIDS Care. 2009;21:1306–1312. doi: 10.1080/09540120902803141. [DOI] [PubMed] [Google Scholar]
- 28.Herek GM, Saha S, Burak J. Stigma and psychological distress in people with HIV/AIDS. Basic and Applied Social Psychology. 2013;35:41–54. doi: 10.1080/01973533.2012.746606. [DOI] [Google Scholar]
- 29.Emlet CA. Experiences of stigma in older adults living with HIV/AIDS: a mixed-methods analysis. AIDS Patient Care STDs. 2007;21:740–752. doi: 10.1089/apc.2007.0010. [DOI] [PubMed] [Google Scholar]
- 30.Grov C, Golub SA, Parsons JT, et al. Loneliness and HIV-related stigma explain depression among older HIVpositive adults. AIDS Care. 2010;22:630–639. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDoom MM, Bokhour B, Sullivan B, et al. How older black women perceive the effects of stigma and social support on engagement in HIV care. AIDS Patient Care STDs. 2015;29:95–101. doi: 10.1089/apc.2014.0184. [DOI] [PubMed] [Google Scholar]
- 32.Goffman E. Stigma: Notes on the management of a spoiled identity. New York, NY, USA: Simon & Schuster; 1963. [Google Scholar]
- 33.Florom-Smith AL, De Santis JP. Exploring the concept of HV-related stigma. Nurs Forum. 2012;47:153–165. doi: 10.1111/j.1744-6198.2011.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holstad MM, Dilorio C, Magowe MK. Motivating HIV positive women to adhere to antiretroviral therapy and risk reduction behavior: The KHARMA Project. Online J Issues Nurs. 2006;11:78–94. [PubMed] [Google Scholar]
- 35.Holstad MM, DiIorio C, Kelley ME, et al. Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS Behav. 2011;15:885–896. doi: 10.1007/s10461-010-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Reports. 1992;41:1–19. [PubMed] [Google Scholar]
- 37.Westbrook L, Bauman L. Perceived stigma of HIV/AIDS Scale. Bronx, NY, USA: Albert Einstein College of Medicine; 1996. [Google Scholar]
- 38.Holstad MM, Foster V, DiIorio C, et al. An examination of the psychometric properties of the antiretroviral general adherence scale (AGAS) in two samples of HIV-Infected individuals. J Assoc Nurses AIDS Care. 2010;21:162–172. doi: 10.1016/j.jana.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ, USA: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 40.Brown RL. Perceived stigma among people with chronic health conditions: the influence of age, stressor exposure, and psychosocial resources. Res Aging. 2014;37(4):335–360. doi: 10.1177/0164027514533133. [DOI] [PubMed] [Google Scholar]
- 41.Warner RM. Applied Statistics. Los Angeles, CA, USA: SAGE Publications, Inc; 2013. [Google Scholar]
- 42.Asiedu GB, Myers-Bowman KS. Gender differences in the experiences of HIV/AIDS-related stigma. A qualitative study in Ghana. Health Care Women Int. 2014;35:703–727. doi: 10.1080/07399332.2014.895367. [DOI] [PubMed] [Google Scholar]
- 43.Van Hollen C. HIV/AIDS and the gendering of stigma in Tamil Nadu, South India. Cult Med Psychiatry. 2010;34:633–657. doi: 10.1007/s11013-010-9192-9. [DOI] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Fact Sheet: HIV among women. 2014 Website: http://www.cdc.gov/hiv/risk/gender/women/facts/index.html. Accessed 2015.
- 45.Sandelowski M, Lambe C, Barroso J. Stigma in HIVpositive women. J Nurs Scholarsh. 2004;36:122–128. doi: 10.1111/j.1547-5069.2004.04024.x. [DOI] [PubMed] [Google Scholar]


